Breast cancer remains the most common cancer that affects women in the United States with over 200,000 women diagnosed each year1,2; approximately 60,000 of these patients undergo mastectomy.2 Breast reconstruction has been shown to provide profound psychological and quality-of-life benefits to the cancer patient.3–7 Unfortunately, in spite of the Women’s Health and Cancer Rights Act requiring insurance coverage for all breast reconstruction after mastectomy, fewer than 25% of patients receive reconstruction annually.8–11 Studies have however shown a steady rise in reconstruction rates in recent years.10,11 Barriers to breast reconstruction exist and variability with reconstruction rates and techniques occur based on geographic region, age, ethnicity and socioeconomic status.11–13 Low utilization has been attributed to non-uniform insurance coverage and variations in referral patterns. 14–16
With a changing healthcare system, the financial landscape for plastic surgeons is likely to evolve. These changes are certain to affect reimbursement for breast reconstruction which will likely contribute to existing concerns among plastic surgeons over declining reimbursement.17–19 A recent national survey of plastic surgeons in the United States showed that nearly 50% of plastic surgeons decreased their breast reconstruction volume due to poor reimbursement.20 Additionally, the shift toward increasing implant-based reconstructions over autologous free-flap reconstruction is likely partly due to a more favorable reimbursement-to-operative time ratio.19 Several studies have examined the cost and profitability of breast reconstruction for select procedures.18,21–30 Our group previously found breast reconstruction fiscally advantageous for the surgical practice when offering tissue expander, and pedicled transverse rectus abdominis myocutaneous (TRAM) flap breast reconstruction; however, reimbursement for autologous reconstructions was poor.18
The aim of this study is to perform an in-depth and updated financial analysis of all breast reconstruction procedure-types to examine the financial implications that breast reconstruction has on both the surgical practice and health care institution, particularly after the introduction of abdominal-based free flap procedures into the practice.
METHODS
Study Population
The authors examined the inpatient billing records of all patients who underwent breast reconstruction at the University of Michigan Health System during the 2011 fiscal year. From these records, we collected data on the Current Procedural Terminology (CPT) code, timing of surgery (immediate or delayed after mastectomy), unilateral or bilateral procedure, operative time, length of stay, insurance provider, charges incurred, and payments received. Procedures performed over the study time period include single and staged implant reconstructions, latissimus dorsi myocutaneous flaps with tissue expanders (TE), transverse rectus abdominis myocutaneous (TRAM) flaps, deep inferior epigastric perforator (DIEP) flaps, and superficial inferior epigastric artery (SIEA) flaps. Data regarding charges for each case included plastic surgery professional charges and hospital (facility) charges. Professional and facility revenue generated included income from all operative procedures performed. Data regarding expenses incurred by the academic practice and facility was collected as well. International Classification of Diseases, Ninth Revision (ICD-9) codes 174.0 to 174.9 and v10.3 were used to identify breast cancer patients. CPT codes 19340 and 19342 (implant), 19357 (tissue expander), 19361 (latissimus dorsi flap), 19367 (pedicled TRAM flap), 19364 (free TRAM, Muscle sparing TRAM), and S2068 (DIEP and SIEA flap) were used to identify patients with breast reconstructive procedures. Institutional review board approval was not needed for this study as the data collected and reported did not include any personal identifiable information.
Professional costs, revenues, and earnings
Professional costs were defined as expenses incurred by plastic surgeons while providing reconstructive services to post mastectomy patients. These costs included the portion of each physician’s salary, benefits, and malpractice allowance allotted to post mastectomy breast reconstruction. The costs also included department and health system taxes for the fiscal year 2011.
Professional revenue was defined as dollars received by the health care providers (physicians) for the services rendered. Net professional revenue was calculated as the difference between the total professional revenue and the total professional costs or expenses. Physician reimbursement per operating room hour was calculated by dividing the average reimbursement per procedure by average operating room time utilized.
Facility costs, revenues, and earnings
Facility or hospital costs for the year 2011 were provided by the hospital billing department. The costs included direct fixed costs, direct variable costs, and indirect costs allotted to the billing system and payroll system. Variable costs included the supplies utilized by each individual patient whereas fixed costs are permanent costs. Indirect costs comprised of health system administrator salaries.
Facility revenues were calculated taking into account the amount billed for providing inpatient, operating room services (nursing, anesthesia), clinic, and pharmacy services. Operating income (profit) was defined as the difference between total facility revenue and total facility costs.
In addition, professional earnings for a subset of patients who proceeded to complete reconstruction were calculated. Completion of reconstruction in this study was defined at the point of having nipple areola reconstruction because this typically represents the final procedure performed prior to nipple tattooing in our practice. We calculated the average number of procedures required to reach the completed stage for each reconstruction type and computed the revenue per reconstruction for each completed reconstruction type.
RESULTS
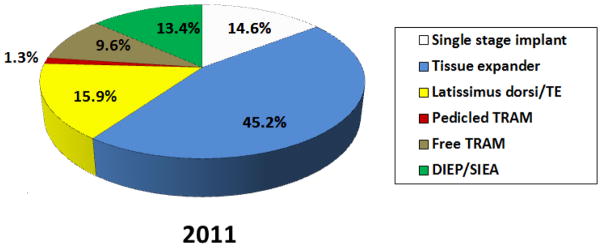
One hundred and fifty two breast reconstructions were performed over a 12 month period by four plastic surgeons at the University of Michigan who dedicated at least a proportion of their practice to breast reconstruction. The distribution of reconstructions based on procedure-type is provided in Figure 1. With the introduction of abdominal perforator flap breast reconstruction, the percentage of pedicled TRAM flap reconstructions decreased from observed percentages (39.6% to 1.3%) reported in 2007.18 Tissue expander and latissimus dorsi/expander-based breast reconstruction percentages remained relatively stable. Free abdominal flap reconstructions comprised 23% of all reconstructions.
Figure 1.
Distribution of breast reconstruction types
The payer mix and collection rates for the patient sample in 2011 were compared to those from 2007 (Table 1). In 2011, 87.3% of patients treated had private insurance, 8.9% were Medicare patients, 3.2% were Medicaid patients, and 0.6% were self-pay. While private insurance remains the greatest third party payer, there was a relative increase in the proportion of Medicare and Medicaid patients compared to 2007. The lowest collection rates were from self-paying patients (0%). Collection rates from both Medicare and Medicaid increased for both the physician (50.3% vs 37%) and the hospital system (47% vs 33.5%). Four years later there was a 17% decrease in overall hospital collection rates from third party payers.
Table 1.
Payer mix and collection rates for the study sample in 2011 relative to 2007
| Type of Payer | Proportion of Sample (2007 sample) % | Professional Collection Rate (2007 Rate) % | Facility Collection Rate (2007 Rate) % |
|---|---|---|---|
| Private | 87.3 (93.0) | 40.1 (37.5) | 39.0 (61.1) |
| Medicare | 8.9 (3.0) | 50.3 (37.0) | 47.0 (33.5) |
| Medicaid | 3.2 (2.0) | 22.1 (13.0) | 25.0 (20.4) |
| Self-Pay | 0.6 (2.0) | 0.0 (2.0) | 0.0 (33.3) |
| Total collection rate | 40.2 (32.2) | 39.0 (56.0) |
| 2011 | 2007 | |||||
|---|---|---|---|---|---|---|
| Type of payer | Proportion of Sample | Professional Collection Rate (%) | Facility Collection rate (%) | Proportion of Sample | Professional Collection Rate (%) | Facility Collection rate (%) |
| Private | 87.3 | 40.1 | 39.0 | 93.0 | 37.5 | 61.1 |
| Medicare | 8.9 | 50.3 | 47.0 | 3.0 | 37.0 | 33.5 |
| Medicaid | 3.2 | 22.1 | 25.0 | 2.0 | 13.0 | 20.4 |
| Self-Pay | 0.6 | 0.0 | 0.0 | 2.0 | 2.0 | 33.3 |
| Total Collection Rate | 40.2 | 39.0 | 32.2 | 56.0 | ||
Collective professional costs, revenue, and earnings for the academic surgical practice in 2011 are outlined in table 2. Net professional revenue was $647,437, total professional costs were $591,184, and net income was $56,253, which resulted in an 8.7% margin. Table 3 shows the costs, revenue, and earnings for the facility. The total facility costs for breast reconstruction exceeded the generated net facility revenue by $10,756, which resulted in a −0.4% margin incurred by the hospital system.
Table 2.
Professional revenue, costs, and earnings
| Cost | ||
|---|---|---|
| Charges and revenue | Professional surgical charges | $1,663,291 |
| Total net professional revenue | $647,437 | |
| Costs | Physician Salary, benefits, and CME | $499,983 |
| Malpractice | $26,725 | |
| Department and health system | $64,476 | |
| Total professional expenses | $591,184 | |
| Earnings | Total professional revenue | $647,437 |
| Total professional expenses | $591,184 | |
| Operating income (Profit) | $56,253 | |
| Margin | 8.7% |
Table 3.
Facility revenue, cost and earnings
| Cost | ||
|---|---|---|
| Charges and revenue | Facility charges | $7,387,791 |
| Total net facility revenue | $2,762,797 | |
| Costs | Fixed expenses | $598,721 |
| Variable expenses | $1,380,662 | |
| Indirect expenses | $793,747 | |
| Total facility costs | $2,773,130 | |
| Earnings | Total facility revenue | $2,762,797 |
| Total facility expenses | $2,773,130 | |
| Operating income (Profit) | -$10,756 | |
| Margin | −0.4% |
A comparison of revenue and costs associated with implant based and abdominal free flap reconstructions is provided in Table 4. There was no difference in the number of procedures required to complete abdominal free flap or implant based reconstructions. The professional revenue generated after the first stage of abdominal free flap reconstruction was significantly greater than revenue generated with implant reconstruction ($7,816 vs. $2,879, p= 0.000). Completed abdominal free flap reconstructions also generated more in comparison to implant reconstructions ($14,943 vs. $7,952, p=0.033). Facility costs associated with abdominal free flap reconstructions were higher than the costs for implant reconstructions ($27,639 vs. $17,655 p=0.001). The revenue generated for the facility by abdominal free flaps was however significantly greater than the revenue generated by implant reconstructions ($30,034 vs. $14,951 p=0.000). After the first stage of reconstruction, abdominal based free flap reconstruction resulted in a positive margin for the facility (8.0%), while implant reconstructions resulted in a negative margin (−18.1%).
Table 4.
Cost and revenue generated for implant and abdominal free flap reconstruction
| Implant based reconstruction | Abdominal free flap reconstruction | p Value | |
|---|---|---|---|
| Professional revenue per 1st stage reconstruction | $2,879 | $7,816 | .000 |
| Professional revenue per complete reconstruction | $7,952 | $14,943 | .033 |
| Average number of procedures | 3.0 | 2.9 | .673 |
| Facility revenue per 1st stage reconstruction | $14,951 | $30,034 | .000 |
| Facility cost per 1st stage reconstruction | $17,655 | $27,639 | .001 |
| Facility margin after 1st Stage reconstruction | −18.1% | 8.0 % | .073 |
Implant Reconstruction - Single Stage and TE
Abdominal free flap reconstruction- Free TRAM and DIEP/SIEA
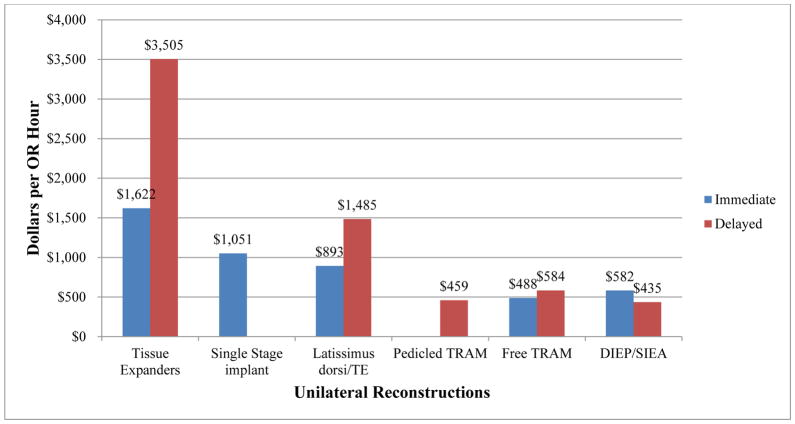
Physician reimbursement by surgical time was highest for delayed tissue expander placement ($3,505/operating room hour) and lowest for delayed DIEP/SIEA reconstruction ($435/operating room hour), as illustrated in Figure 2. The average professional revenue generated for completed reconstructions (Table 5) was greatest following completion of DIEP/SIEA flap reconstructions ($16,131 per reconstruction) and was lowest for pedicled TRAM reconstructions ($4,857 per reconstruction).
Figure 2.
Professional revenue generated per operating room hour for the first stage of reconstruction
Table 5.
Average number of procedures to complete reconstruction and professional revenue generated
| Avg. # of procedures | Physician Revenue per Patient | |
|---|---|---|
| Single-Stage Implant | 2.6 | $7,169 |
| Tissue Expander | 3.1 | $8,102 |
| Latissimus dorsi/TE | 4.0 | $9,522 |
| Pedicled TRAM | 3.0 | $4,857 |
| Free TRAM | 2.6 | $13,042 |
| DIEP / SIEA | 3.1 | $16,131 |
DISCUSSION
The purpose of this study was to critically assess the financial implications associated with the introduction of abdominal perforator flap breast reconstruction to a well-established academic surgical practice. This evaluation is unique as it provides detailed financial information on changes in a surgical practice which previously reported on this topic when implant and pedicled flap reconstructions were the primary techniques performed.18 This evaluation also presents a financial picture of reimbursement completely dependent on insurance at a time when other forms of compensation are thought to be necessary for the success of a practice offering free flap options for breast reconstruction.
We found that relative to the previous report, pedicled TRAM flaps were almost completely replaced by free TRAM flaps (9.6%), DIEP and SIEA flaps (13.4%). The proportion of tissue expander reconstructions (45.2%) and latissimus/implant reconstructions (15.9%) remained essentially the same, with a new implant technique, the single stage reconstruction (14.6%) accounted for (Figure 1). Breast reconstruction remained financially beneficial for the practice with an 8.7% margin while the facility sustained a small loss, −0.4%. Tissue expander reconstructions provided the greatest reimbursement per OR hour. Abdominal based free flap reconstructions provided significantly greater professional and facility revenue for the first stage of reconstruction relative to implant forms of reconstruction. These abdominal based free flaps also provided significantly greater professional revenue for completed reconstructions when compared to implant procedures. In contrast to free flap reconstruction, implant reconstructions were found to result in substantial losses to the facility (8.0 % vs. −18.1% margin).
The merits of all forms of post-mastectomy breast reconstruction are well documented in the literature. With slowly rising overall reconstruction rates, abdominal based autologous free tissue techniques have been outpaced by implant reconstruction techniques.10 Reasons for this discrepancy in reconstructive techniques are likely multifactorial. Patients clearly have a choice and for reasons including age, lifestyle, job demands, aesthetic preferences and social interactions with other reconstructed patients, implant techniques may be more appealing. Access to reconstructive surgeons with microsurgical expertise is another key limiting factor. Though autologous forms of reconstruction are known to be beneficial in the long term from the patient perspective,31,32 when compared to implant reconstruction, surgeons tend to be less enthusiastic about performing these procedures for financial reasons.17–20 The general feeling seems to be that time is more efficiently spent placing implants and that insurance companies reimburse poorly for perforator flap procedures without special arrangements such as a “carve out”. These concerns are even more critical at a time when the financial landscape of healthcare in the United States is changing with goals of cost containment and increasing access.
With the addition of two microsurgeons to the practice, abdominal based perforator flaps were immediately introduced and over the course of the first 12 months, breast reconstruction as a whole continued to be profitable to the practice. However, relative to the previous report18 there has been a noticeable decrease in margins for the plastic surgery section (27% vs. 8.7%) and the institution (15% vs −0.4%). Potential reasons for this decline include an increase in the proportion of Medicare and Medicaid patients cared for (Table 1). We also found that collection rates for the institution decreased by close to 20%. Implant-based reconstructions accounted for approximately 60% of all reconstructions performed (Figure 1), with private insurance accounting for 87% of the third party payers. The hospital collection rates for the private insurance companies declined from 61.1% to 39%, likely making up a good portion of the losses observed. This decreased collection rate for the institution might be related to changes in practice patterns for implant reconstruction over the past few years, with a transition to routine use of acellular dermal matrices (ADM). With lower collection rates, the hospital may sustain losses from expensive ADMs which add to the variable cost of performing these procedures.30
In considering specific reconstruction techniques, tissue expander and latissimus/expander reconstructions reimbursed better per OR hour when compared to autologous free flap techniques (figure 2). Our finding of greater reimbursement per OR hour with implant based reconstruction supports the general notion that time is more efficiently spent with implant procedures.21 The clear reason for this difference relates the greater number of hours spent in the operating room for more demanding microsurgical procedures. As suggested by Fine et al.33, this reimbursement rate for 2 stage implant reconstructions does not take into account additional time spent on outpatient visits required with tissue expander reconstructions; these visits are included in the 90 day global period. Of note, free flap revenue per operating room hour can be expected to be at its worst in the first year of practice for the new microsurgeon because with experience, efficiency can be expected to improve. Though not reported in this study the number of hours spent performing unilateral and bilateral free flap procedures had decreased by 2–4 hours, 2 years after introducing these procedures. This efficiency is reflected in reports from the practice of an experienced microsurgeon23 which showed a trend towards lower institutional costs with free flap reconstructions; this study by Fischer et al. however did not provide data on professional revenue. One practical solution to the problem of efficient time use for the surgeon who performs free autologous flap procedures is to run multiple rooms. In performing an immediate reconstruction, shorter procedures can be performed in one room while a mastectomy is being performed in another by the surgical oncologists. This way a few procedures are performed prior to the lengthy microsurgical procedure.
Though revenue per OR hour was more favorable for implant reconstruction, the professional revenue generated for the first stage of reconstruction was significantly greater for free flap reconstructions ($7,816 vs. $2,879 p= 0.0001). In evaluating professional revenue for patients who had completed all stages of reconstruction, free flaps again were superior ($14,943 vs. $7,952 p= 0.033). Though the first stage of reconstruction is time intensive, autologous free tissue transfers generate greater revenue for the surgeon. This trend is also seen with the facility revenue generated (Table 4). Hospitals for better or worse do well financially with procedures that require hospital stays, exemplified by the fact that outpatient cosmetic surgery is less favorable than surgical procedures which requires an ICU stay for instance. Though our free flaps do not require ICU stays, they are admitted to the hospital for 3–5 days, different from the 23 hour observations required for immediate implant reconstructions; delayed implant reconstructions in our practice are performed as outpatient procedures further compounding the difference seen in facility revenue.
The facility costs associated with the first stage of abdominal free flap reconstructions was significantly higher than the costs for implant reconstruction ($27,639 vs $17,655, p=0.001), in contrast to a recent report.23 However, facility revenue was significantly higher for abdominal free flaps than implant reconstruction ($30,034 vs $14,951, p= 0.0001). In essence free flaps cost more than implant reconstructions but also generated significantly more. These differences in facility cost and revenue account for the positive and negative margins observed for abdominal free flaps and implant reconstructions respectively (Table 4).
Despite a growing trend toward implant-based reconstructions, a recent cost analysis looking at multiple forms of reconstruction found that only autologous reconstruction was cost-effective in both irradiated and non-irradiated patients.34
Our study has certain limitations. Our financial analysis was limited to a single University Health Care System and the findings cannot be generalized to other practice settings with different physician salary structures, hospital accounting systems, procedure/payer mixes, and collection rates. Regional variations in costs and revenue were also not addressed. Additional costs incurred as a result of postoperative complications were not included in this study. Nonetheless, the strategy for this analysis can be applied in different practice settings to evaluate the profitability of a variety of reconstructive procedures.
CONCLUSION
Post-mastectomy breast reconstruction through standard insurance plans remains fiscally profitable for this academic practice. However, there appears to be a financial loss for the health care system. Implant based reconstruction seems to allow for greater surgeon efficiency but ultimately generates less revenue and results in financial losses for the facility. The addition of perforator flap procedures to the reconstructive options offered to mastectomy patients is not only beneficial to patients but is also fiscally advantageous to the academic surgical practice and institution.
Acknowledgments
Support for this study was provided in part by grants from the Plastic Surgery Foundation (to A.O.M) and by a Midcareer Investigator Award in Patient-Oriented Research (K24 AR053120) (to K.C.C.).
References
- 1.Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA Cancer J Clin. 2010;60:277–300. doi: 10.3322/caac.20073. [DOI] [PubMed] [Google Scholar]
- 2.Hernandez-Boussard T, Zeidler K, Barzin A, Lee G, Curtin C. Breast reconstruction national trends and healthcare implications. Breast J. 2013;19:463–9. doi: 10.1111/tbj.12148. [DOI] [PubMed] [Google Scholar]
- 3.Wilkins EG, Cederna PS, Lowery JC, et al. Prospective analysis of psychosocial outcomes in breast reconstruction: one-year postoperative results from the Michigan Breast Reconstruction Outcome Study. Plast Reconstr Surg. 2000;106:1014–25. doi: 10.1097/00006534-200010000-00010. discussion 26–7. [DOI] [PubMed] [Google Scholar]
- 4.Stevens LA, McGrath MH, Druss RG, Kister SJ, Gump FE, Forde KA. The psychological impact of immediate breast reconstruction for women with early breast cancer. Plast Reconstr Surg. 1984;73:619–28. doi: 10.1097/00006534-198404000-00018. [DOI] [PubMed] [Google Scholar]
- 5.Rowland JH, Holland JC, Chaglassian T, Kinne D. Psychological response to breast reconstruction. Expectations for and impact on postmastectomy functioning. Psychosomatics. 1993;34:241–50. doi: 10.1016/S0033-3182(93)71886-1. [DOI] [PubMed] [Google Scholar]
- 6.Nano MT, Gill PG, Kollias J, Bochner MA, Malycha P, Winefield HR. Psychological impact and cosmetic outcome of surgical breast cancer strategies. ANZ J Surg. 2005;75:940–7. doi: 10.1111/j.1445-2197.2005.03517.x. [DOI] [PubMed] [Google Scholar]
- 7.Atisha D, Alderman AK, Lowery JC, Kuhn LE, Davis J, Wilkins EG. Prospective analysis of long-term psychosocial outcomes in breast reconstruction: two-year postoperative results from the Michigan Breast Reconstruction Outcomes Study. Ann Surg. 2008;247:1019–28. doi: 10.1097/SLA.0b013e3181728a5c. [DOI] [PubMed] [Google Scholar]
- 8.Alderman AK, Wei Y, Birkmeyer JD. Use of breast reconstruction after mastectomy following the Women’s Health and Cancer Rights Act. JAMA. 2006;295:387–8. doi: 10.1001/jama.295.4.387. [DOI] [PubMed] [Google Scholar]
- 9.Alderman AK, McMahon L, Jr, Wilkins EG. The national utilization of immediate and early delayed breast reconstruction and the effect of sociodemographic factors. Plast Reconstr Surg. 2003;111:695–703. doi: 10.1097/01.PRS.0000041438.50018.02. discussion 4–5. [DOI] [PubMed] [Google Scholar]
- 10.Albornoz CR, Bach PB, Mehrara BJ, et al. A paradigm shift in U.S. Breast reconstruction: increasing implant rates. Plast Reconstr Surg. 2013;131:15–23. doi: 10.1097/PRS.0b013e3182729cde. [DOI] [PubMed] [Google Scholar]
- 11.Reuben BC, Manwaring J, Neumayer LA. Recent trends and predictors in immediate breast reconstruction after mastectomy in the United States. Am J Surg. 2009;198:237–43. doi: 10.1016/j.amjsurg.2008.11.034. [DOI] [PubMed] [Google Scholar]
- 12.Kruper L, Xu X, Henderson K, Bernstein L. Disparities in reconstruction rates after mastectomy for ductal carcinoma in situ (DCIS): patterns of care and factors associated with the use of breast reconstruction for DCIS compared with invasive cancer. Ann Surg Oncol. 2011;18:3210–9. doi: 10.1245/s10434-011-2010-y. [DOI] [PubMed] [Google Scholar]
- 13.Joslyn SA. Patterns of care for immediate and early delayed breast reconstruction following mastectomy. Plast Reconstr Surg. 2005;115:1289–96. doi: 10.1097/01.prs.0000156974.69184.5e. [DOI] [PubMed] [Google Scholar]
- 14.Horner-Taylor C. The Breast Reconstruction Advocacy Project: one woman can make a difference. Am J Surg. 1998;175:85–6. doi: 10.1016/S0002-9610(97)00271-7. [DOI] [PubMed] [Google Scholar]
- 15.Yang RL, Newman AS, Lin IC, et al. Trends in immediate breast reconstruction across insurance groups after enactment of breast cancer legislation. Cancer. 2013;119:2462–8. doi: 10.1002/cncr.28050. [DOI] [PubMed] [Google Scholar]
- 16.Alderman AK, Hawley ST, Waljee J, Morrow M, Katz SJ. Correlates of referral practices of general surgeons to plastic surgeons for mastectomy reconstruction. Cancer. 2007;109:1715–20. doi: 10.1002/cncr.22598. [DOI] [PubMed] [Google Scholar]
- 17.Wilkins EG, Alderman AK. Breast reconstruction practices in north america: current trends and future priorities. Semin Plast Surg. 2004;18:149–55. doi: 10.1055/s-2004-829049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Alderman AK, Storey AF, Nair NS, Chung KC. Financial impact of breast reconstruction on an academic surgical practice. Plast Reconstr Surg. 2009;123:1408–13. doi: 10.1097/PRS.0b013e3181a0722d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Patel A, Clune JE, Forte A, Chang CC. The impact of the Medicare sustainable growth rate formula on reconstructive plastic surgery. Plast Reconstr Surg. 2010;126:270e–1e. doi: 10.1097/PRS.0b013e3181ef952b. [DOI] [PubMed] [Google Scholar]
- 20.Alderman AK, Atisha D, Streu R, et al. Patterns and correlates of postmastectomy breast reconstruction by U.S. Plastic surgeons: results from a national survey. Plast Reconstr Surg. 2011;127:1796–803. doi: 10.1097/PRS.0b013e31820cf183. [DOI] [PubMed] [Google Scholar]
- 21.Spear SL, Mardini S, Ganz JC. Resource cost comparison of implant-based breast reconstruction versus TRAM flap breast reconstruction. Plast Reconstr Surg. 2003;112:101–5. doi: 10.1097/01.PRS.0000066007.06371.47. [DOI] [PubMed] [Google Scholar]
- 22.Fischer JP, Sieber B, Nelson JA, et al. Comprehensive outcome and cost analysis of free tissue transfer for breast reconstruction: an experience with 1303 flaps. Plast Reconstr Surg. 2013;131:195–203. doi: 10.1097/PRS.0b013e318277856f. [DOI] [PubMed] [Google Scholar]
- 23.Fischer JP, Nelson JA, Cleveland E, et al. Breast reconstruction modality outcome study: a comparison of expander/implants and free flaps in select patients. Plast Reconstr Surg. 2013;131:928–34. doi: 10.1097/PRS.0b013e3182865977. [DOI] [PubMed] [Google Scholar]
- 24.Preminger BA, Pusic AL, McCarthy CM, Verma N, Worku A, Cordeiro PG. How should quality-of-life data be incorporated into a cost analysis of breast reconstruction? A consideration of implant versus free TRAM flap procedures. Plast Reconstr Surg. 2008;121:1075–82. doi: 10.1097/01.prs.0000304246.66477.cd. [DOI] [PubMed] [Google Scholar]
- 25.Kroll SS, Evans GR, Reece GP, et al. Comparison of resource costs of free and conventional TRAM flap breast reconstruction. Plast Reconstr Surg. 1996;98:74–7. doi: 10.1097/00006534-199607000-00011. [DOI] [PubMed] [Google Scholar]
- 26.Kaplan JL, Allen RJ. Cost-based comparison between perforator flaps and TRAM flaps for breast reconstruction. Plast Reconstr Surg. 2000;105:943–8. doi: 10.1097/00006534-200003000-00017. [DOI] [PubMed] [Google Scholar]
- 27.Thoma A, Khuthaila D, Rockwell G, Veltri K. Cost-utility analysis comparing free and pedicled TRAM flap for breast reconstruction. Microsurgery. 2003;23:287–95. doi: 10.1002/micr.10138. [DOI] [PubMed] [Google Scholar]
- 28.Thoma A, Veltri K, Khuthaila D, Rockwell G, Duku E. Comparison of the deep inferior epigastric perforator flap and free transverse rectus abdominis myocutaneous flap in postmastectomy reconstruction: a cost-effectiveness analysis. Plast Reconstr Surg. 2004;113:1650–61. doi: 10.1097/01.prs.0000117196.61020.fd. [DOI] [PubMed] [Google Scholar]
- 29.Serletti JM, Moran SL. Free versus the pedicled TRAM flap: a cost comparison and outcome analysis. Plast Reconstr Surg. 1997;100:1418–24. doi: 10.1097/00006534-199711000-00006. discussion 25–7. [DOI] [PubMed] [Google Scholar]
- 30.de Blacam C, Momoh AO, Colakoglu S, Slavin SA, Tobias AM, Lee BT. Cost analysis of implant-based breast reconstruction with acellular dermal matrix. Ann Plast Surg. 2012;69:516–20. doi: 10.1097/SAP.0b013e318217fb21. [DOI] [PubMed] [Google Scholar]
- 31.Hu ES, Pusic AL, Waljee JF, et al. Patient-reported aesthetic satisfaction with breast reconstruction during the long-term survivorship Period. Plast Reconstr Surg. 2009;124:1–8. doi: 10.1097/PRS.0b013e3181ab10b2. [DOI] [PubMed] [Google Scholar]
- 32.Yueh JH, Slavin SA, Adesiyun T, et al. Patient satisfaction in postmastectomy breast reconstruction: a comparative evaluation of DIEP, TRAM, latissimus flap, and implant techniques. Plast Reconstr Surg. 2010;125:1585–95. doi: 10.1097/PRS.0b013e3181cb6351. [DOI] [PubMed] [Google Scholar]
- 33.Fine NA, Kim JS. Discussion: breast reconstruction modality outcome study: a comparison of expander/implants and free flaps in select patients. Plast Reconstr Surg. 2013;131:935–7. doi: 10.1097/PRS.0b013e318286598f. [DOI] [PubMed] [Google Scholar]
- 34.Grover R, Padula WV, Van Vliet M, Ridgway EB. Comparing five alternative methods of breast reconstruction surgery: a cost-effectiveness analysis. Plast Reconstr Surg. 2013;132:709e–23e. doi: 10.1097/PRS.0b013e3182a48b10. [DOI] [PubMed] [Google Scholar]