Abstract
Extracellular matrix (ECM) proteins collectively represent a class of naturally derived proteinaceous biomaterials purified from harvested organs and tissues with increasing scientific focus and utility in tissue engineering and repair. This interest stems predominantly from the largely unproven concept that processed ECM biomaterials as natural tissue-derived matrices better integrate with host tissue than purely synthetic biomaterials. Nearly every tissue type has been decellularized and processed for re-use as tissue-derived ECM protein implants and scaffolds. To date, however, little consensus exists for defining ECM compositions or sources that best constitute decellularized biomaterials that might better heal, integrate with host tissues and avoid the foreign body response (FBR). Metrics used to assess ECM performance in biomaterial implants are arbitrary and contextually specific by convention. Few comparisons for in vivo host responses to ECM implants from different sources are published. This review discusses current ECM-derived biomaterials characterization methods including relationships between ECM material compositions from different sources, properties and host tissue response as implants. Relevant preclinical in vivo models are compared along with their associated advantages and limitations, and the current state of various metrics used to define material integration and biocompatibility are discussed. Commonly applied applications of these ECM-derived biomaterials as stand-alone implanted matrices and devices are compared with respect to host tissue responses.
Keywords: decellularized, implants, integration, ECM, protein scaffolds, tissue engineering
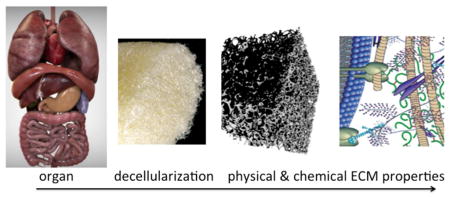
Graphical Abstract
Introduction
The extracellular matrix (ECM) in various forms and preparations has been pursued as a biomaterial for decades [2–4]. In general, ECM-based biomaterials represent lipid-free, decellularized protein-based derivatives and purified protein extracts of previously living tissues or organs. This final form differentiates the extracted ECM as a biomaterial compared to its living tissue precursor representing an organ or tissue graft for transplant. The functional and technical justification for using purified ECM as an implant instead of the viable complete tissue or organ form often stems from versatility and flexibility of using the ECM-derived material in many manipulated and inanimate implantable forms incompatible with living cells in full tissues, perceived immune complications of full transplanted tissues or grafted organs, and likely rejection of grafted tissue through extensive immune responses to introduction of non-self biological entities. Decellularized ECM material extracts, rigorously purified of all cellular components, have generally been thought to be free of the practical and physiological limitations of implanting living grafts. This presumption, however, is rarely verified to completion in content and composition resulting in biomaterials that have poorly defined impure states and arbitrary levels of decellularization. This includes constraints of allogeneic sourcing, diverse opportunities to form, print, and process acellular ECM protein biomaterials, new capabilities to seed ECM materials with select cells, growth factors, drugs, and even inorganic components to produce context- or tissue-specific regenerative composite implants.
Initial Host Tissue Responses to Implants
All implanted materials invoke an initial inflammatory response that progresses to an unresolved chronic inflammatory immune response referred to as the host foreign body reaction (FBR) [5–8]. The classic host response’s temporal description is generally broken into several stages, beginning with the wounding injury during implant placement and continuing throughout the wound-healing period. Ultimately, the host response reaches a relative impasse with most implants, unresolved in its chronic inflammatory state as long as the implant remains. This terminal state is defined by the prolonged presence of both activated macrophages and associated foreign body giant cells (FBGC’s) at the tissue/biomaterial interface, and formation of a dense fibrous collagenous capsule around the implant. These two features - presence of FBGCs and fibrous capsule thickness - represent the two most common metrics applied to assessing the severity of the FBR (see Table 1). This chronic local condition remains over the life of the implanted material, resolving to normal wound healing only when the implant is removed or completely degraded. While modulated to varying degrees depending on site, implant morphology and biomaterial, the local host reaction to implant placement persists seemingly regardless of the material chemistry, implant size or method of introduction. This response remains a daunting challenge for implanted biomaterials.
Table 1.
Metrics of Importance in Determining Extent of the Host FBR
| Host Response Metric | Identification/Measurement | Source |
|---|---|---|
| FBGC | Number of cells with 3 or more nuclei | [14] |
| Fibrosis | Capsule thickness | [15, 16] |
| Capsule collagen density | [17] | |
| Macrophage Phenotype | M1/M2 ratio | [18] |
| Tissue Ingrowth | Angiogenesis - Timing and Rate | [19] |
| Rate of neotissue formation | [20] | |
| Inflammatory Markers | Cytokines/Chemokines | [5, 16, 21] |
| IL4 | ||
| IL13 | ||
| IL6 | ||
| MCP-1 | ||
| TNF | ||
| MIP-1α | ||
| RANTES | ||
| Inflammatory cell density | [22] | |
| Macrophages | ||
| PMN | ||
| Lymphocytes | ||
| Infection | Cultured microbes | [23] |
As a completely natural material, the ECM has been proposed to be immune-privileged in the sense that, as a natural material, ECM may not succumb to the typical implant fate and series of host reactions to foreign bodies [9–12]. The logic driving this idea is that naturally derived matrix materials represented by the ECM present naturally derived biomolecular designs and architecture, and biological compositions to interrogating host cells after implantation that attenuate the FBR. By presenting physically and biochemically “native” matrices to implants sites, ECM biomaterials are proposed to rapidly re-establish healing cues and limit foreign body reactions. Nonetheless, despite a significant history of ECM development, analysis and implant use for decades, currently little consensus exists regarding its ultimate capabilities in modulating host reactions. Certainly, host privilege with regards to minimizing the FBR and improving implanted materials performance has not been unequivocally demonstrated. ECM biomaterial utility in implanted forms and its eventual progress in biomedical applications will rely on improved knowledge of compositional identity of decellularized natural materials and how these factors influence host recognition and ultimate implant integration, regeneration and healing. This review examines methods to process tissue explants to yield various ECM materials, assess their composition and then validate their use as biomaterials in preclinical implant models. Understanding the critical performance issues has direct implications on efforts regarding translation of these materials into commercial medical products.
Increased interest in protein-based implant materials over the past decade [2–4] has been inspired by both the demand for improved implant materials and tissue transplants and the realization that all synthetic materials elicit a host response that is sustained until the foreign material is removed or degraded. Strategies to modify synthetic implant materials through physical and chemical means have had few noted successes [13] and little effect on long term FBR outcomes [5]. Exploiting the intrinsic ability of ECM to engage with host cells upon implantation is thought to duplicate aspects of wound healing and ameliorate biocompatibility issues.
ECM Composition and Architecture
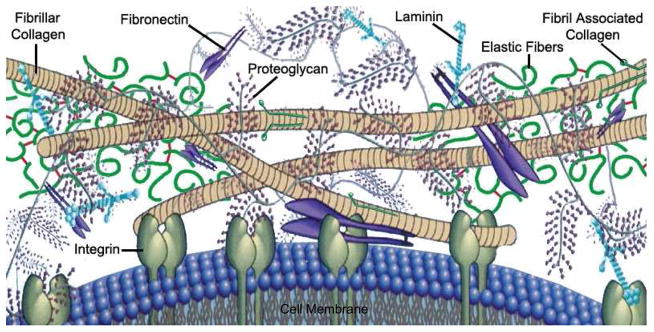
ECM-specific components include collagens, elastins, trace cell-engaging proteins (fibronectin, vitronectin, osteopontin, glycosaminoglycans (GAGs), and growth factors (Figure 1). Collagens and elastins serve as primary structural elements of the ECM and are typically the most abundant proteins present. Associated macromolecular non-protein GAGs (heparans, dermatans, chondroitins and hyaluronans) largely serve as ECM crosslinkers and reservoirs for water, growth factors, and cytokines/chemokines due to their highly negative charge and binding sites for specific proteins. This signaling cache and control of tissue osmotic pressure is the predominant reason why GAG presence is advantageous in ECM properties. Cell-engaging proteins are interspersed throughout the ECM and interact with both ECM and with integrin receptors found on cell surfaces. These cell-ECM interactions can dictate cell phenotype and responses through the control of intracellular signaling cascades. Beyond compositional conservation, decellularization processes can seek to preserve native ECM structure through maintenance of protein-GAG and protein-protein interactions. There is still a large debate regarding the importance of spatial relationships between ECM components and complete ECM composition to determine the ultimate utility of a biomaterial [3]. Further, more complete, discussions on ECM composition, structure and components can be found in the cited resources [24–26].
Figure 1.
Representative cartoon of ECM compositional layout indicating cellular engagement with ECM biomolecules and primary components of general ECM space. (Adapted with permission from [1])
Collagen represents the simplest and most abundant class of structural ECM protein used as an implant material. It has been studied and applied in purified forms sourced from ECM-rich tissues such as tendon and dermis with interest as an implant material dating back to the early 1960’s [27, 28], and citations dating to the 1940’s and 1950’s relating to experimental collagen implantation [29, 30]. Collagen has a substantial clinical history of use, primarily in an injectable form [31, 32], and sheet form [33–35], and is also reported in many fundamental studies of implants as a coating [36, 37], chemically modified form [38–40], and in diverse solid implant forms [41, 42].
This rich history of xenogeneic collagen implantation shows that host immune responses can occur. The most predominant clinically used injectable collagen implant material, Zyderm®, has shown susceptibility (although rare) to abscess formation and local necrosis [41]; foreign body granuloma and foreign body giant cells [43]. Furthermore, up to 3% of the population suffers from collagen allergy [44], enough so that allergy testing is routinely performed prior to material implantation. Additional concerns arise from the potential for zoonotic disease transmission from xenogeneic sourced materials. While adverse reactions are noted, these animal-sourced collagen materials have seen widespread human use with few serious clinical complications. The predominant final response to implanted collagen is complete resorption [41].
Crosslinked Protein Implants and the FBR
Resorption and removal of the collagen foreign body leads to an interesting hypothesis that collagen elicits a host response until it is degraded. Evidence supporting this hypothesis can be found through investigation of host responses to cross-linked collagen implants, rendering their degradation and removal more difficult. Analysis of host responses to cross-linked collagen is detailed elsewhere [45]. Numerous studies conclude that prolonged degradation rates from increasing crosslink density are associated with more severe host FBRs as evidenced by the presence of FBGC’s, and fibrous capsule formation around the implanted material [39, 45–47]. The method of crosslinking seems to be largely irrelevant to the FBR intensity achieved. Interestingly, there has been little research into naturally cross-linked collagen host FBRs. While collagen crosslinking via lysyl oxidase, an enzyme responsible for natural collagen crosslinking in vivo, has not been feasible ex vivo, other natural cross-linking methods such as the use of transglutaminases have not been studied with respect to the host FBR [45, 48–50]. This would substantiate the operative hypothesis that unnatural, therefore difficult-to-breakdown, crosslinking leads to the observed increased FBR to crosslinked collagen implants [45].
Natural collagen remodeling is performed through the coordinated enzymatic actions of assorted matrix metalloproteinases (MMPs), with nearly 30 known enzyme members [16]. Combinations of these collagenases/gelatinases are responsible for tissue matrix turnover, regeneration and homeostasis. Non-natural crosslinking using diverse chemical agents (e.g., glutaraldehyde, genipin) likely affects MMP bioactivities against native collagen substrates, producing an imbalance in ECM turnover. Delayed resorption and even substrate inertness to degradation prolongs crosslinked collagen implant presence in tissue, exacerbating host responses to the implant. Non-natural collagen degradation fragments, bearing remnants of added synthetic chemical crosslinkers, are known antigens [51, 52].
Beyond Collagen: The Shift to More Complex ECM Implant Materials
Despite collagen’s ubiquitous and structurally critical presence in all tissues and organs in its different isoforms as an essential structural ECM protein [44, 53, 54], few studies specifically show seamless integration of collagen implants without foreign body reactions or with the expected “natural” tolerance or biocompatibility. Yet, serious clinical adverse reactions are not commonly reported either. Collagens from autologous or xenogeneic sources are weakly immunogenic in antibody cross-reactivity studies [55]. Clinical observations indicate that only 2–4% of human populations possess inherent immunity (i.e., allergic sensitivity) to bovine collagen [56]. Additionally, animal-sourced collagen extracts may exhibit minor human antigenicity, but traditionally, this sensitivity has been considered generally acceptable for tissue engineered implants for human use [57]. Lastly, published data supporting human immunological benefits of engineered telopeptide-deficient collagens (i.e. free of antigenic epitopes) remains equivocal [58].
Despite substantial medical history, collagen has long operated clinically in a gray zone of implant acceptability with respect to specific host tissue responses. Given the notable lack of prominent, consistent host responses throughout its historical clinical utility, collagen implants have essentially addressed tissue bulking. Further biomedical interest in studying purely collagen implants and host FBR has diminished. Collagen’s development as an implant material continues, even after decades of research and translation, but interest in protein-based implant materials has gradually shifted towards decellularized ECM-based extracts, containing collagen as the predominant compositional fraction, but also a much more complex biopolymer composition and architecture. ECM-based scaffolding as a more complex tissue engineered/implantable structure is now attractive. This is perhaps due to specific requirements deemed essential for implant performance, including multiple cell-engaging peptides, complex proteoglycan/protein structural interactions, and natural affinities for soluble cell signal mediators unmet with a homogeneous scaffold biomaterial like collagen or synthetically duplicated from pure components de novo. Despite logical principles for ECM bottom-up synthetic design, that a more complete ECM matrix comprising much more than collagen I might improve host compatibility as a biomaterial for implant use remains to be validated in vivo. Instead of bottom-up construction, the most common method for obtaining these complete ECM matrices is through harvesting and decellularizing native tissues and organs from various human and animal species.
Tissue decellularization and characterization
Distinct from living tissue or organ transplantation, decellularization of full tissues and organs is consistently pursued as a required purification procedure for producing any ECM-derived biomaterial [59]. Successful decellularization is a tissue-dependent procedure, requiring optimization of protocols for each tissue source and applications. However, what constitutes decellularization is not rigorously defined currently. For ECM-derived biomaterials, endogenous cells represent a contaminant and source of diverse cell-based antigens and host reactivity. Abundant organelles, lipid membranes, membrane-associated and cytosolic proteins and cell-derived nucleic acids must be completely removed to yield a pure ECM-only material that is both implant processable and less host reactive. Examples of cellular proteins known for their inflammatory stimulus and implant rejection are markers for effective decellularization are the α-gal epitope and MHC-1 [9, 52, 60–62]. The hypothesis that certain threshold amounts of these proteins are required to invoke implant rejection and a host response remains to be validated [9]. This concept derives largely from clinical evidence showing no elevation of host antibodies in human serum samples after implantation of small intestinal submucosa (SIS) with known low quantities of the α-gal epitope. Nonetheless, further work to elucidate this theory is most certainly required. Clinical consequences of incomplete decellularization can be dire, as shown in the case of incompletely decellularized Synegraft™ heart valves in pediatric patients [63].
Methods of decellularizing tissues have been extensively reviewed elsewhere [3, 4, 59]. In general, decellularization procedures utilize mechanical, enzymatic, and chemical means to remove as much cellular material as possible while leaving the ECM biopolymer components structurally and/or chemically intact. Manipulation and processing to remove cellular components inevitably removes or alters some of the desired ECM components and native architectures as well. This necessitates post-decellularization characterization methods that verify complete cellular component removal and sufficient retention of desirable ECM entities and structure. This balance is often analytically elusive and difficult to validate.
Characterization of decellularized tissues/organs as ECM biomaterials
Decellularized tissue characterization serves two purposes: 1) to verify removal of cellular components, and 2) to identify protein/ECM species and ECM-like structures and tissue-like architectures present within the processed final material. This is simply a balance of the removal of undesired materials while preserving desired materials and natural structures and their intrinsic bioactivities. General pre-implant characterization of decellularized materials should focus on: protein/biomolecule identity, presence of contaminants (represented by tissue sourced residual cellular proteins/biomolecules and added biomolecule/chemical entities through decellularization procedures), protein/biomolecule (e.g. proteoglycan/GAG) spatial distributions, matrix mechanical strength (modulus), degradability and chemical stability, and intrinsic ability to promote cell attachment and growth. Implant characterization should emphasize host responses including immunogenicity and sensitivity, fibrosis and scarring, and degradation.
Despite substantial history, decellularization protocols are still evolving, with limited standards and guidances for what must or must not be present within the final material, and how to validate it. [64]. No general or universally accepted methods exist to completely characterize the complex ECM remnants in their entirety following decellularization. Furthermore, the high levels of donor variability to naive ECM composition undoubtedly leads to different ECM fractional composition post-decellularization. Hence, ECM standardization as a biomaterial remains elusive.
A diverse toolbox of multiple, often tedious, techniques must be used to completely identify residual components during ECM extraction from full tissues. To date, little consensus supports what protocols and standard methods must be used and what biologic components must be monitored and analyzed to assert adequate purity of the resulting matrix. In many cases these criteria will be application-specific, as different tissues gain their unique properties from tissue-specific components that comprise them. In general, decellularized tissues should be verified to be substantially free of known toxic/deleterious materials such as residual cellular debris, lipids, nucleic acids, endotoxins, and known antigenic/immunogenic proteins. No standards currently exist to guide such validation. This ambiguity in what constitutes ECM “purity” presents problems for understanding and achieving common, comparable outcomes for final ECM-based products and for comparing and assessing how they perform in vivo.
Methods commonly employed for analyzing ECM products from decellularized materials include immunohistochemistry (IHC) [65, 66], histologic staining (hematoxylin and eosin, Masson’s trichrome stain, Oil Red O) [67, 68], ELISA techniques [69], and mass spectrometry [70–72]. These techniques can all also be used to determine residual cellular components, and with the exception of mass spectrometry, specific proteins to analyze must be selected and tailored to each assay. This a priori selection of analytes for ECM characterization provides specific, sensitive and detailed information on composition, but is arbitrary and often variable in assay quality, and without content standards. Those ECM components left unmonitored in ECM therefore remain unknown, leading to potential confirmation bias in published results. Additional techniques that are present, but not universally employed, include biomechanical testing [73, 74], permeability measurements within decellularized scaffolding [75], and laser microscopy [74] (Table 2). Few, if any, standardized metrics or assay specifications exist for determining presence or importance of any component in a decellularized material
Table 2.
Traditional decellularized material characterization techniques
| Method | Components Identified | |
|---|---|---|
| Histology (Common stains include hematoxylin and eosin, Masson’s Trichrome, and Pentachrome) | Spatial location of remnant nucleic acid Tissue spatial organization | Spatial (Yes), Quantitative (No) |
| IHC/IF | Specific ECM proteins/structures of interest i.e. Collagen type, growth factors, immunogenic proteins |
Spatial (Yes), Quantitative (No) |
| Mass Spec | Quantify protein/biomolecule composition | |
| ToF-SIMS | Surface analytic compositional technique | Spatial (Yes), Quantitative (Yes) |
| Tandem MS | Bulk analytic compositional technique | Spatial (Yes), Quantitative (No) |
| Biopolymer Assays | Specific biopolymer identification | |
| Collagen (Hydroxyproline, Sircol™) | Mass fraction of collagen | Spatial (No), Quantitative (Yes) |
| GAG/Proteoglycan (Dimethylmethylene blue, Blyscan™) | Mass fraction of GAG | Spatial (No), Quantitative (Yes) |
| Elastin (Ninhydrin, Fastin™) | Mass fraction of Elastin | Spatial (No), Quantitative (Yes) |
| ELISA | Detection of soluble protein (growth factors) | Spatial (No), Quantitative (Yes) |
| Nucleic Acid (Hoescht based, Picogreen™, gel electrophoresis) | Rresidual DNA | Spatial (No), Quantitative (Yes) |
| Endotoxin (Limulus amebocyte lysate [LAL]) | Contaminating endotoxins | Spatial (No), Quantitative (Yes) |
| Mechanical Testing | ||
| Indentation | Modulus, Poisson ratio, permeability | Spatial (No), Quantitative (Yes) |
| Tensile | Stress-strain/Modulus | Spatial (No), Quantitative (Yes) |
| Thermal Denaturation | Crosslinking status | Spatial (No), Quantitative (Yes) |
| Fluorescence recovery after photobleaching (FRAP) | Small molecule diffusivity within decellularized construct | Spatial (No), Quantitative (Yes) |
| Laser Microscopy | Collagen, elastic fiber spatial organization | Spatial (Yes), Quantitative (No) |
An analogous scenario with respect to a biologically derived, clinically useful and purified biomaterial extract, also exhibiting highly variable characterization methods and composition without consensus, is demineralized bone matrix (DBM), approved for clinical use as a minimally manipulated biologically derived material. DBM composition varies from source to source and by commercial formulation, and like ECM, final DBM material composition and biological properties can also be highly variable [76], also without standards. Additionally, decellularized ECM biocompatibility, like DBM, is often assessed using experiment-specific testing methodologies that are often incomparable.
Improved characterization of ECM to better assert critical properties should consider techniques producing the type of data desired. Many techniques are destructive and result in a loss of spatial or location-specific biological properties of the ECM. For overall bulk compositional assessments, this is not an issue, but ECM microstructural or spatial compositional information at high resolution is often critical to inform or detail implant function [3, 77]. Comprehensive ECM structural and compositional information requires application of several different complimentary techniques focused on bulk and location-specific ECM properties. All analytical methods have intrinsic limitations and figures of merit to consider for the value of each assessment to the overall goal.
Decellularization residuals and trace contaminants
Innate host cell recognition of ECM components and architecture and resulting functional engagement in vivo makes a decellularized matrix product more attractive over most synthetic biomaterials for implant use and possible tissue regeneration. Therefore, ECM proteins, proteoglycans, glycoproteins, and other biomolecules – collectively responsible both for producing ECM’s important microstructure as well as maintaining natural cell interactions -- are essential to retain in natural chemical and structural forms in decellularized ECM [26]. Native matricellular polymers such as collagens, elastins, proteoglycans/GAGs, and growth factor contents are commonly assessed. Important trace matrix proteins fibronectin, vitronectin, osteopontin, decorin, biglycan, SPARC, thrombospondin, fibril-associated and network-forming collagens, and many others are less assayed and difficult to quantitate, but are equally important for ECM structure and function [78]. Little discussion is given to other ECM components such as proteinases and proteinase inhibitors, despite their important role in shaping cell actions [79]. Residual ECM proteinases can be regarded as undesirable remnants of decellularization; their residual proteolytic functions after decellularization would degrade desired ECM proteins. It may be more advantageous then for these proteins to be removed from ECM to be restored eventually by incoming newly resident host cells upon implantation.
As there are many fundamentally important molecules within native tissue that guide cell functions both spatially and temporally, it is currently unknown what specific molecules are essential for neo-tissue formation. In response to this ignorance, a large push to more quantitatively describe what remains within a decellularized tissue, represented by both desired and undesired components, is frequently urged.
Mass spectrometry techniques
Due to its large-scale protein detection capability with a single experiment, mass spectrometry (MS) has become a key analytical method for decellularization characterization [80]. Different MS approaches have been applied to decellularized ECM materials, including LC/MS/MS [71, 72, 81], ToF-SIMS [70, 82], and MALDI/ToF [83]. The most common of these techniques is by far the ‘shotgun’ peptide identification approach using LC/MS/MS. Known generally as ‘tandem MS’, LC/MS/MS relies on heavy pre-analysis techniques to isolate and purify the protein samples for MS [84]. Generally, whole protein samples are first reduced and run on a PAGE gel, often performed on two-dimensional gels, followed by gel extraction and cleanup with liquid chromatography. This is all performed with the intent of reducing sample complexity, remove dominant uninteresting protein background, and enrich the sample in less abundant proteins of interest for identification. Mass spectra are then analyzed and proteins identified using database search programs on derived fragment libraries with user-defined input search parameters. The complex overlap between protein spectra makes for difficult analysis: database searches are not perfect at identifying proteins, and in some cases may falsely identify a protein [85, 86].
Time of flight secondary ion mass spectrometry (ToF-SIMS) is an attractive surface analytical method in principle due to its ability to detect proteins on the outer surface of solid or porous ECM implant materials without the extensive preprocessing and solubilization steps required for LC/MS/MS and MALDI/ToF MS. This method will identify species from the outermost 1–2 nm layer of the ECM material. The difficulty in this method, and all MS techniques with proteins, lies in correctly deciphering the complex spectra obtained, correlating up to 104 mass peaks to known protein species. Despite multiple attempts, ToF-SIMS has so far been unable to make specific directed assignments to proteins within a decellularized material [70, 82]. This technique is still largely unsuccessful due to the immense overlap of multiple peptides in MS spectra derived from complex decellularized materials composed of hundreds of individual proteins. Continued optimization of spectral analysis may make this a credible ECM analysis technique in the future. Results currently show possibilities to run decellularized ECM MS results against control protein standards to make good approximations of ECM surface composition, particularly if the experimental sample is known to be rich in some specific-signature amino acids [87, 88]. However, since ToF-SIMS does not provide a complete parent ion of a protein, ambiguity in identification remains an issue. Nonetheless, due to its inherent sensitivity, MS will pick out differences when other techniques (e.g., histology or biochemical assays) show that the ECM samples are identical. For example, total protein quantification, immunostaining, and histology all might support two differently prepared or sourced samples ultimately seeming analogous. However, ToF-SIMS can show that they are indeed compositionally different at their surfaces, and that they then could respond differently to cell infiltrates when implanted.
Additional contaminants in the ECM sample from decellularization processes could also be confounding factors in MS spectral analysis. Common decellularization buffers include sodium dodecyl sulfate (SDS) and sodium deoxycholate (SDC), of which both could leave remnants without extensive sample washing. These could lead to issues with interpreting positive ion spectra confounded by high amounts of metal (typically sodium) ions preset [89]. In addition to this, other detergents such as Triton and others may also be confusing in MS [90]. While these contaminants should have low abundance with proper decellularization techniques, accurate accounting is required in analysis. MS methods could also serve an important role for the detection of these residual decellularization contaminants in ECM samples.
Drawbacks of MS Techniques
The major drawback of any MS technique is that a protein’s presence is inferred based on amino acid fragment analysis, and does so in a way that does not provide precise amounts of protein present, yielding a non-quantitative “yes-or-no” answer, although the field of quantitative proteomics is developing rapidly [91]. The generalized proposal in the literature suggests that a threshold amount of residual cellular material in ECM after decellularization is necessary to invoke a host immune response [81, 92]. MS techniques are not yet able to decipher this threshold level or supply meaningful quantitative data to test this hypothesis and validate threshold levels for purity. So-called “matrix effects” for MS ion extraction efficiencies, overwhelming metal ion MS noise from biological salines, subtle protein isoforms produce further challenges for MS metrics from ECM.
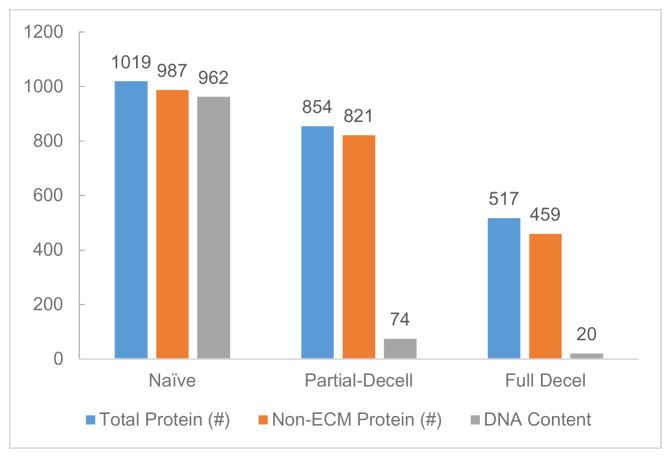
Reviews of ECM decellularization results to date based on MS data have been mixed. In many cases cellular proteins are identified with this technique after decellularization [71, 72]; however, it has also been used to show that the majority of remnants are related to the ECM [81]. In all cases, large numbers, some greater than 300, of distinct proteins are identified with this method (Figure 2). It is unclear, though, if the large variation of reported results with respect to cellular components and numbers of ECM components reported in MS protein data is based on poor sample preparation for analysis or from poor decellularization. Ultimately, with careful analytical validation and standard comparisons, this technique could serve as a valuable tool for identification of important ECM remnant components in tissue replacement/engineered products.
Figure 2.
Example of residual protein contributions to MS spectra analysis of rat liver decellularized by freeze/thaw, SDS, and Triton X-100 treatment. Results suggest a large decrease in proteins contributing to the total amount in decellularized tissue that contains a significant fraction of non-ECM proteins and residual DNA. Reported values are total number of proteins detected and ng/mg dry weight of DNA. (Adapted with permission from [88])
Unwanted ECM residual material analysis
Cellular Nucleic Acids
Removal of undesired residual cellular material from tissue is predominantly verified by examining remaining DNA and genomic residues [92]. Interestingly, residual ECM RNA is not discussed as a major concern compared to residual DNA, and the prevalence of RNase use in decellularization protocols is comparatively low. It could be that the limited concern is due to the general rapid natural destruction of RNA. Therefore, residual cellular-derived DNA has been adopted as a surrogate marker for contaminating cellular materials. Importantly, affirmation of its complete removal is also associated with the important presumption that all other undesired cellular components are also removed including proteins/GAGs, amino acids, and lipids. This assumption is largely unproven and unjustified: nuclear material does not necessarily share the same physicochemical properties as all other intra- and extra-cellular components (e.g., membrane proteins, lipids, enzymes) and would not necessarily interact with decellularization protocols, agents or remaining ECM proteins in the same ways during extractions and purification steps. A seminal recent decellularization review indicates that no studies had yet been performed at that time to understand the effects of ECM-residual DNA towards altering host response or potential for host rejection of that implanted material [4]. However, verification of sufficient cell removal has largely been ascribed in literature to the absence of nucleic acids. In all likelihood, DNA has remained the standout reporter, simply through its ease of quantitation using commercial dye-based optometric assays (e.g., PicoGreen, Invitrogen, and other Hoechst based assays), DAPI/hematoxylin or other histologic staining techniques, and lack of other readily available and acceptable material characterization methods (i.e., without excessive, tedious analysis, inconvenience or expense). At the very least, DNA absence verifies that cell lysis and washing steps were sufficiently rigorous to remove DNA below the detection limits of these DNA assays. However, beyond this, lack of other critical cellular components remains unconfirmed.
Additionally, thresholding the functional significance of remnant DNA post-decellularization remains unvalidated. Current reporting of residual DNA amounts representative of sufficient ECM decellularization reference a cut-off of less than 50 ng DNA per mg of dry ECM product with remaining DNA length of less than 300 bp [92]. These values are unvalidated by any known report and therefore are apparently quite arbitrary, representing debatable criteria when considering mechanisms of DNA recognition by host immune cells still incompletely understood. Current understanding of DNA stimulation of immune cells is related to DNA binding of Toll-like recepter-9 (TLR9), although other pathways have also been suggested [93–95]. Additionally, it has been shown that a minimum DNA cutoff length of 24 bp, or two double helical turns, is required to stimulate RAW 267.4 cells, a length much lower than the proposed 300 bp cutoff [94].
Increasing evidence largely disproves the commonly published idea that residual DNA is an accurate and reliable representative universal reporter of cellular contamination [96]. Interestingly, many clinically available ECM devices have shown desired efficacy, even with the presence of remnant DNA (and therefore presumed other unidentified cellular components) [81, 92]. Many successful decellularized implant materials have reported DNA contents of 60 ng/mg and see regular clinical use [97]. This DNA-ECM purity correlation requires substantial expert analysis and verification for consensus.
Endotoxins
Endotoxin contamination must be considered in any implantable material due to its potent ability to stimulate inflammatory responses. Also known as lipopolysaccharides (LPS), endotoxins comprise a complex family of related peptidoglycan-lipid components of cell membranes of gram negative bacteria, often a contaminant in biologically derived materials[98]. LPS are tenacious adsorbates, surface-active and common processing remnants even if sterilized and seemingly ubiquitous without living bacterial presence [99]. As a potent stimulator of acute inflammatory responses, endotoxin activates different cell types with varying threshold levels of contamination. Monocytes and macrophages can be activated by very small amounts of endotoxin, as low as 0.5 EU/mL. Due to their known potent, adverse host reaction, the US FDA currently dictates that all medical devices demonstrate less than 0.5 EU/mL in a device previously soaked in endotoxin-free water for at least 1 hour [99]. However, it has been suggested that this value may be below the threshold for negative inflammatory responses occurring due to contaminated decellularized devices [100]. While this value is regulated, simply soaking a biomaterial in water is likely insufficient to allow accurate analysis of adherent LPS on a potential implantable device. Critical to endotoxin determinations required for ECM-derived materials, the conventional Limulus Amebocyte Lysate (LAL) assays are not suitable for determining endotoxin in tissues due to known assay interference from β-glucan-like molecules present in tissues. A modified LAL assay unaffected by β-glucan-like molecules was shown to be capable of detecting endotoxin in clinically aseptic tissues [101].
Endotoxin, with its intrinsic poor water solubility and surfactant-like structure, does not necessarily leach substantially from materials into solution during a 1-hour immersion in water. Since all current endotoxin assays only detect solution-phase LPS [99, 102], adsorbed amounts are not quantified for compliance with the FDA threshold. To combat this risk, modified protocols and LPS-spiked controls should be used to detect adherent endotoxin [103–105]. New testing through the use of commercialized endotoxin-sensitive RAW-Blue™ LPS-indicator cells may prove as an alternate to overcome the hurdle of accurate endotoxin contamination on solid surfaces and complex materials [106]. The nature and amount of ECM endotoxin contamination must be reliably known to properly explain observed host response to ECM implanted materials.
Inflammatory ECM proteins
Analytical benchmarking of purified ECM has focused on residual cell contaminants or extracellular components. Two common proteins of interest are the potent host rejection proteins, α-gal epitope and MHC-1 [9, 52, 60–62]. Their inflammatory and implant rejection mechanisms have been widely discussed [107–110]. The α-gal epitope is much more of a concern when implant sourcing is xenogeneic due to natural antibody production towards α-gal in humans [111], while MHC could provoke host responses from both xeno- and improperly matched allo-sourced biological materials [112]. These two select proteins, however, represent the few known proteins that must be eliminated from purified ECM intended for implant use. The hypothesis that threshold amounts of these two proteins, as well as all other non-autologous proteins, are required to invoke implant rejection and an adverse host response [81, 92] remains unverified. Clearly defining critical proteins verified to be “low tolerance” contaminants, and their amounts required to induce host responses remains a challenge. Analytical techniques should be standardized and adopted to make such determinations routine, allowing a parsing of ECM preparation methods and resulting products into “safe” and “unsafe” categories for research and clinical translation.
Asserting tissue-specific ECM identities
Throughout the past decade, most tissue types have been decellularized for various reuse applications [3, 113, 114]. The provocative issues underscoring these studies regard 1) how different tissue sources might produce distinct ECM characteristics after complete decellularization, and 2) that these tissue-specific ECM compositional and structural differences are distinct and important to how they recruit host cells in vivo to generate tissue-specific responses. Producing valid and verifiable answers to address these issues has significant user implications for translation as some tissues, (e.g., adipose) are much more readily available than others, such as heart, kidney, lung, liver and brain If “throw-away” tissues, readily harvested like adipose, can be made compositionally representative (through further processing/modification and compositional validation of the resultant material) to other tissue types after decellularization, they would represent a universal ECM source with a verifiable quality standard. This validation would diminish the need to acquire and process difficult-to-source and less abundant organs and tissues for tissue-specific ECM implants and regeneration needs.
The lack of currently accepted compositional standards in decellularized matrix purification and characterization tools, and the numerous different published decellularization methods used currently [59, 74, 115–118] does not facilitate ready answers to these issues. Studies have compared different decellularization protocols on the same tissue source. Direct comparisons have been performed for adipose tissue [115], porcine heart valves [119], and whole hearts [120], showing that decellularization protocols greatly affect the biomolecular compositional remnants, particularly with respect to GAG content and thus growth factor content as well. These molecules are more susceptible to detergent treatments and provide the most variability in decellularization outcomes from similar tissues [121].
All tissues predominantly comprise analogous base biopolymer materials (collagens, GAGs/proteoglycans, structural proteins elastin and laminin) with the majority of tissues being collagen I by weight. The uniqueness of any tissue is therefore defined by the minor differences in biopolymer composition and structure, and the important different cellular phenotypes organized and orchestrated within it. Most decellularization procedures are deemed successful by comparing the resulting ECM to native tissue using few specific tissue markers. For example, components deemed critical to the identity of cartilage are collagen II and high GAG content [122] while collagens I, IV, laminin, and fibronectin (predominant contributors to the basement membrane) have been deemed critical components to retain in many different tissue types to promote epithelialization (including angiogenesis) [81, 121, 123–125]. Therefore identifying minimal ECM compositional requirements that functionally distinguish different tissue sources in clinical outcomes for ECM use are likely required to understand exactly what ECM requirements direct tissue-specific host healing properties. While this is the overall goal, functional proof of these tissue specific markers has yet to be shown as a requirement for functional tissue replacement.
One future approach to explore this issue would be to analyze a decellularized ECM material’s inherent ability to stimulate stem cell populations to inhabit, create, and sustain tissue function of any desired type. This is particularly pertinent to tissue-engineered devices where exogenously seeded progenitor cells are promoted to differentiate down specific pathways (often ex vivo) to provide the majority of the neo-tissue function upon implantation. Recruited host cells are sensitive to several other cues secondary to ECM engagement, such as cell-cell contacts, paracrine signaling, growth factor presence, and local mechanics [126–128]. The role of ECM compositional variation as supplied from different tissues and any significance to ECM-based cellular and tissue endpoints in affecting recruited stem cell phenotypic behaviors, differentiation and eventual cellular functionality in tissue-specific context is largely unknown. To provide mechanistic evidence for this influence, initial efforts will need to report differences in tissue-specific ECM compositions and microstructures with high accuracy to be able to correlate resulting cell phenotypes and ultimately regenerated tissue behaviors in vivo. That these ECM factors could also affect inflammation and chronic host FBR to implants is equally important for clinical use but requires similarly complex studies on controlled ECM materials to provide this information.
Similar to all cells, stem cells interact with their tissue surroundings primarily through cell-matrix engagement, cell-cell engagement and soluble signal processing. Integrins represent a major cell receptor class facilitating direct cellular recognition of cell-binding peptide domains within ECM molecules [24, 78]. Integrin-mediated interactions stimulate intracellular signaling cascades that control cell behavior, including recruitment, proliferation and differentiation. Stem cell differentiation varies based on the protein substrates they encounter [reviewed in [128]]. Hence, if tissue-specific ECM truly comprises distinct matrix protein components in their native presentation, then this tissue context should somehow be imparted to resident cells through matrix-cell interactions. This is the basis for tissue engineering designs that often synthetically place different cell integrin recognition motifs deliberately into biomaterials scaffolds [129–133]. Several studies provide evidence for decellularized tissue directing stem cell differentiation into tissue proper phenotypes during in vitro culture [61, 121, 123, 134]. Highlighted mechanisms relate to both the mechanical nature of the decellularized product as well as the constituent proteins and molecules retained from decellularization. At some level these two variables are correlated, perhaps inseparable, mechanistically. These studies indicate that mesenchymal stem cell (MSC) or induced pluripotent stem (iPS) cells seeded onto purified heart matrix differentiate into cardiomyocytes [116, 123]. Similarly, MSC seeding into a human decellularized trachea ECM and grown in an air interface bioreactor showed preferential differentiation into the desired cell phenotypes [61]. These examples, though, have other confounding, uncontrolled factors that may also contribute to stem cell fate within ECM. These experiments were performed with both soluble signaling factors as well as tissue-specific decellularized ECM. Nonetheless, cell differentiation was more efficient on decellularized matrix materials regardless of growth factor-conditioned media. This indicates that ECM material composition positively affects seeded cellular outcomes in vitro.
The possibility that ‘cross talk’ between the two differing signal sources (physical and soluble) [135] combine to produce this positive feedback system [136, 137] is suggested but largely unverified in ECM. Nonetheless, it seems very likely that addition of soluble signals complements ECM to direct cell-specific phenotypes [138–141]. Heart-derived decellularized ECM produces the desired cell differentiation to cardiomyocytes, but only circumstantial evidence supports ECM insoluble signaling sufficient to drive cell fate. Interestingly, defining control experiments to validate this idea are not yet been reported. For example, cells not specific to the tissue-specific decellularized ECM material have not been studied to understand how ECM alone dictates cell phenotype. Few reports describe stem cell growth on decellularized ECM where the original ECM source is not the same as the desired targeted tissue type. Mechanistically, only intrinsic ECM-characteristic matrix stiffness and mechanics has been demonstrated to control differentiation [128], with no known experiments yet reporting the mechanism for how tissue-specific ECM might guide differentiation to tissue-specific resident cell phenotypes required for regenerative medicine.
Critical roles of ECM microstructure and composition are evident in a recent study that cultured fibroblasts on both decellularized diseased (i.e., idiopathic pulmonary fibrosis) and healthy lung tissue. Fibroblasts were similarly sourced from both healthy and diseased tissues. It was found that ECM source, instead of cell source, had the greater effect on resulting cell phenotype, with diseased ECM driving fibroblast gene expression towards the diseased state [142].
In vivo assessment of ECM implant biocompatibility
Material biocompatibility is the composite result of a complex series of biological/immunological events and the host physiological context in which the material is placed [143]. Hence, biocompatibility cannot be accurately assessed in vitro where full competence of either the host biology or physiology is lacking. Despite FDA recommendations for extensive ISO10993 in vitro assays as a biocompatibility assessment, comprehensive assessment of both of these biocompatibility criteria mandates use of in vivo test systems [144, 145]. Importantly, even the relevance of in vivo models for biomaterial implant assessment is questioned since commonly used rodent physiological and immunological systems are distinct from humans in many respects [146–148]. Choice of animal species used, in vivo site of placement (e.g., subdermal, intramuscular, percutaneous, transcortical), time point to explantation, and metrics used to assess host tissue responses are variable and lack standardizations for reporting. Hence, common animal implant models for host material response analysis, linking common host responses across various species, and variations in response varying by implant anatomical location are now discussed. Surprisingly, little consensus or consistency is found in published literature for host-implant integration metrics for implant healing versus FBR. Comparisons of ECM implant capsular thickness, neovascularization, giant cell formation, leukocyte infiltrates, select cellular inflammatory markers (e.g., chemokines, cytokines) with standardized endotoxin-controlled implants in standardized surgical procedures, sites and accepted animal models would be useful for comparative ranking and assessments. These in vivo implant metrics for ECM biomaterials require an understanding of the relative benefits and deficiencies of current implant models used routinely for assessing host response.
Recognized differences between rodent species in wound healing research relevant to the FBR
Rodent species (syngeneic mice and rats) remain the most common animals used to probe biomaterial-host responses [149]. Their utility lies with their ease of use related to relative cost, housing, adaptable surgical procedures, handling and throughput. Availability of genetic mutants, knock-ins, and knock-outs in the mouse and the relative abundance of murine-specific molecular probes for histology, biological assays, and PCR are both substantial benefits as well. Rodents also lie near the boundary of the lowest mammalian species required to provide a representative host tissue response to humans [150]. The guinea pig is another rodent used, although more rarely, as an animal model in FBR research. By contrast, large animal models are much more rarely compared to mice and rats due to logistic/ethical/cost concerns as well as lack of molecular probes for histology and profiling. However, large animals remain useful, and often required due to closer physiologic overlap with humans than rodents, for late stage/pre-clinical experimentation [149].
Differences in rodent tissue physiology and immune responses compared to humans, and even within the different rodent species, must be explained and justified for any model. Several studies show differences in the reported host tissue responses to subdermal collagen and synthetic fluoropolymer (ePTFE) implant materials between mice and rats [151–153]. These studies were primarily focused on differing immune systems and implant activation of immune cells [152] and cytokine/chemokine signaling differences [153]. These studies compared different material chemistries (ePTFE and dermal collagen, respectively), noting increased inflammatory cells (macrophages) and inflammatory signaling in rats compared to mice. Not only was the final outcome noted to be different, but cellular and inflammatory signaling dynamics were shown to differ as well. Results such as these serve as examples of nuanced differences between rodent species that may lead to altered interpretations of host FBR development when biomaterial and implant location are controlled. Ultimately, these seemingly subtle differences have the potential to lead to translational issues as ECM materials are scaled up towards clinical testing. Additionally, the mere presence of these differences in host response could be indicative of further unknown differences yet to be investigated.
Differences in host response to implant location
A similar yet distinct collagen implant study comparing host tissue response development between differing implant locations in a common animal model showed that host immune response mechanisms vary within the same animal [16]. This study compared collagen discs implanted at two different locations in a mouse model: supra-epicardially and subcutaneously. Differing inflammatory cytokine signaling was noted between these two locations along with a change in MMP activity, leading to differing collagen implant degradation rates with a stronger FBR developed in the epicardial region. The observed collagen disc FBR was assessed based on higher influx of inflammatory cells, including macrophages and polymorphonuclear (PMN) cells, increased angiogenesis, and increased inflammatory signaling profiles in the superepicardial region. These two examples emphasize that appropriate expert attention be directed to selecting an animal model for host response assessments to implants. Additionally, should this prove representative of the human scenario, these results may also offer insight into whether eventual clinical device utilization may be implant location-dependent for performance outcomes.
Mouse models seeking mechanisms to in implant-related wound healing and the FBR
Several mouse models have been reported for elucidation of more detailed mechanisms of the host response to implanted biomaterials. These include both genetically altered, or knock-out-based, and surgical models. Prominent murine knock-out systems have been used to determine the importance of certain matrix metalloproteinases and their control by thrombospondins 1 and 2 [154] in host-implant FBR development. Similar matricellular proteins -- SPARC, tenascin-C, and osteopontin -- have also been implicated in FBR development through similar knock-out mouse models [155]. These proteins are now implicated in roles related to increased angiogenesis and development of a fibrous capsule. Other knock-out models have demonstrated the importance of fibronectin in mounting a strong host tissue response to implants [156] and the presence of FBGCs, despite lack of IL-4, in a T-cell deficient mouse model [157]. Other knock-out mice models have been applied to ECM-based implant materials as well, predominantly studying the effects of cytokines and signaling molecules implicated in host FBR development [151, 158, 159]. An interferon-γ (i.e., a macrophage-activating cytokine) knock-out model was used to identify its relationship to host rodent FBR mechanisms to dermal sheep collagen implants, and showed that interferon-γ had little effect on host response outcomes in mice, with similar presence of macrophages and FBGCs [151]. These unique mouse models serve as precision tools to analyze specific molecular or cellular contributions to implant-centered healing and FBR development. Furthermore, they may prove beneficial in probing individual influences of biochemical and biomechanical effects on decellularized ECM integration and host response developments. While their use in FBR studies has spanned more than a decade, wide adoption has yet to be seen and consensus on their general utility in this context is not established.
Common surgical implant models to study the FBR include the subcutaneous pouch (either through blunt dissection or minimally invasive needle injection) [8, 13, 19, 22, 160, 161], abdominal wall defect [162, 163], intraperitoneal space [154, 164, 165] and dorsal skinfold chamber [166–168] models. Previously, the cage implant system was a popular method for studying implant/host tissue responses [169–171]. This model has seen less use recently compared to heavy use 20–30 years ago, due possibly to recognized limitations in delineating the host response to the implanted cage material itself versus the test materials within the subdermal cage. As discussed above, differing implant locations may provoke differing FBR responses, making direct comparisons between anatomical implant locations difficult without careful controls. Other less common models are typically contextually based on specific disease states such as surgical removal of muscle or the abdominal wall as a mimic of hernia [172], replacement of the aorta for testing synthetic vascular grafts [173], brain implantation of neuronal stimulating electrodes [174] and hard tissue implants in bony defects either with or without fixation tools to stabilize the implant site [175].
Collectively, rodent implant studies highlight the prominent mechanistic differences occurring within similar species, and that the FBR for implants develops ubiquitously as a complex process dependent on several requisite but independent physiological cues. To dissect this complex parameter set affecting ECM-based implants, further insight must be gained as improved models, particularly using CRISPR-based genomic modifications [176–178], knock-out/in, and new gene reporter (i.e., fluorescent protein) systems are developed and utilized in FBR assessments to various ECM to distinguish key determinants for host tolerance and regenerative medicine. Host response variability depending on host species physiology and immune competence, wound healing dynamics and mechanisms, tissue site, genetic strain, and types of implantation methods are all potentially confounding factors influencing FBR results that may be improved using these new techniques. Host responses are a complex set of dynamic tissue site reactions to material presentation: both sides contribute to the resulting balance of observed FBR responses. Given the plethora of variables in these models, concluding that the in vivo response observed is solely implant material-dependent (or biomaterial-controlled) is rarely unequivocally shown. Importantly, ECM-based implants to date show few clinically important differences to any other implant material class: their utility and possible advantages need to be vetted in the proper (currently unidentified) in vivo FBR models, of which no rationale currently exists for any particular animal model over another with regards to reliable predictability of general FBR outcomes.
Cell phenotypic differences between implant responses in rodents versus humans
The utility of any animal model in translation is only verified if it actually serves as an accurate and predictive representation of the analogous human scenario. In this context, to correlate host FBR mechanisms to ECM implants to those gleaned from non-standardized rodents, differences between rodents and humans relevant to their healing transition from acute to chronic inflammatory responses must be elucidated and acknowledged. Unfortunately, relatively few studies directly compare cellular and molecular details for onset of FBRs between humans and rodents compared to other disease states such as cancer [179]. Fortunately, evidence indicates that the monocyte-macrophage system is relatively conserved between wild type mice and human (though not necessarily in specialized murine models compatible with biologically derived humanized implants, e.g. NOD/SCID mice) [180]. The dynamic mobilization process of monocyte extravasation from bone marrow to the circulatory system and recruitment response to tissue inflammation tends to follow the same differentiation pathways. Given the macrophage’s central role in developing and sustaining the FBR [5, 15, 181], murine macrophages are likely to respond in a contextually accurate manner in mice, representative of the human scenario. Mast cells, more recently emphasized as a dominant early cell type directing the host FBR [5, 182–184], show marked differences between murine and human systems [185]. Most significantly, mast cell numbers are much lower in the mouse -- only 10–20% of that seen in humans. Additionally, mast cells have been shown to populate the peritoneal space in mice, but are not seen in human peritoneum. These differences, while not functionally conclusive, highlight the potential for altered immune cell responses to implanted materials between these two species. New developments of humanized mouse models, also given noted deficiencies, could pave the way for more representative preclinical testing for material compatibility which to date have focused more on intra-cellular dynamics, instead of the larger scale material/host interactions [186].
Comparisons between rodent and human host responses to ECM materials
Decellularized ECM-derived implants in humans: explanted analyses
Several clinically used implant materials are derived from decellularized tissues [see Table 3]. These biomaterials vary across their sourced species of ECM origin, physical and chemical forms, and intended uses, each applying proprietary decellularization methods. Their ECM clinical use in humans and preclinical testing in laboratory animals facilitates some comparisons of host responses to these particular ECM materials between species where reported. However, comparisons between preclinical research animal data and human clinical use is difficult due to the lack of direct side-by-side comparison studies using the same metrics for determining their representative host FBR’s. The general clinical expectation is that a device is safe and provides better results than what may be achieved with either no, or other, treatment. This focus does not necessarily include screening for common FBR/tissue integration results (Table 1).
Table 3.
Examples of Clinically Used Decellularized Products (adapted with permission from [59])
| Product | Manufacturor | Tissue Source | Application Focus |
|---|---|---|---|
| AlloDerm® | Lifecell Corp | Human Dermis | Soft Tissue |
| AlloPatch HD™, FlexHD® | ConMed (Musculoskeletal Trasplant Foundation) | Human Dermis | Tendon, Breast |
| NeoForm™ | Mentor Worldwide LLC | Human Dermis | Breast |
| GraftJacket® | Wright Medical Technology Inc. | Human Dermis | Soft tissue, Chronic wounds |
| Strattice™ | Lifecell Corp | Porcine Dermis | Soft Tissue |
| Zimmer Collagen Repair Patch™ | Zimmer Inc. | Porcine Dermis | Soft Tissue |
| TissueMend® | Stryker | Bovine Dermis | Soft Tissue |
| MatriStem®, Acell Vet | Acell Inc. | Porcine Urinary Bladder | Soft Tissue |
| Oasis®, Surgisis® | Cook Biotech Inc. | Porcine Small Intestine | Soft Tissue |
| Restore™ | DePuy Orthopaedics | Porcine Small Intestine | Soft Tissue |
| FortaFlex® | Organogenesis Inc. | Porcine Small Intestine | Soft Tissue |
| CorMatrix ECM™ | CorMatrix Cardiovascular Inc. | Porcine Small Intestine | Soft Tissue |
| Meso BioMatrix™ | Kensey Nash Corp. | Porcine Mesothelium | Soft Tissue |
| IOPatch™ | IOP Inc. | Human Pericardium | Opthalmology |
| OrthAdapt®, Unite® | Synovis Orthopedic and Woundcare Inc. | Equine Pericardium | Soft tissue, Chronic wounds |
| CopiOs® | Zimmer Inc. | Bovine Pericardium | Dentistry |
| Lyoplant® | B.Braun Melsungen AG | Bovine Pericardium | Dura Mater |
| Perimount® | Edwards Lifesciences LLC | Bovine Pericardium | Valve replacement |
| Hancock® II, Mosaic®, Freestyle® | Medtronic INC. | Porcine heart valve | Valve replacement |
| Prima™ Plus | Edwards Lifesciences LLC | Porcine heart valve | Valve replacement |
| Epic™, SJM Biocor® | St. Jude Medical Inc. | Porcine heart valve | Valve replacement |
| MiroMesh® | Miromatrix Medical Inc. | Porcine Liver | Soft Tissue |
| Avance® Nerve Graft | AxoGen | Human Nerve Tissue | Peripheral Nerve Discontinuity |
| MatrACELL® | LifeNet Health | Human dermis | Soft Tissue, Chronic wounds |
In general, the decellularized implant products shown in Table 3 tend to perform well with few reported issues with their use in diverse implant sites (typically soft tissue), particularly in humans [35, 187, 188]. A number of clinically approved matrix protein-derived devices see regular use in patients in numerous locations in vivo, primarily as tissue fillers/bulking agents (see Table 3) with safe outcomes. There are, however, reports indicating negative clinical results with some products. It has been shown that porcine small intestinal submucosa (SIS – see Table 3), at least in an 8-ply configuration, is associated with post-procedural complications in vaginal wall repair, with up to 60% of patients in one study showing intense inflammation through 39 days after implantation [189]. Associated complications included lack of tissue repopulation and blood vessel infiltration, with high levels of fibrosis in the periphery of the implanted material. However, no immune screening was performed on these patients and biopsies were not examined for typical signs of a foreign body response such as presence of FBGCs. Porcine SIS used in other surgical sites did not necessarily follow this particular intense inflammatory trend. The use of Surgisis™ in hernia repair shows safe and satisfactory results out to five years [190], with some evidence of dense fibrous connective tissue and a slight FBGC response in the repaired abdominal wall at 5 years, Other reports in human clinical use also report positive outcomes using Surgisis™ material for hernia repair often indicating better results than repair with synthetic mesh alternatives, although specific host response metrics were not examined in these studies [162, 191]. The general trend for this material’s use in hernia repair was some general post-procedural inflammation with a slight FBGC response.
Unfortunately, these human results are not fully consistent with preclinical rodent models of hernia repair with this same decellularized ECM implant material. Studies performed in rats are mixed overall representing both positive and negative outcomes related to FBR development and implant biocompatibility concerns [192–194]. Results of these animal studies all represent more severe outcomes than what is implied by human clinical reports to date. However, there is a range for how far the rodent implant response to ECM seems to deviate from the human scenario. Based on these reports, the predictive accuracy of preclinical rodent testing, at least for decellularized materials intended to aid in hernia repair, is questionable at best. Further discrepancy is shown in porcine SIS implant studies performed in mice, exhibiting no abnormal inflammation or pathology in both abdominal wall defect and subcutaneous pocket models, and with a noted lack of FBGC formation and increase in macrophage numbers [195, 196]. This indicates a potential difference, then, between mouse, rat, and human responses to porcine mucosa-sourced ECM implants.
Many other clinical examples of both porcine SIS use and other decellularized tissues from various ECM-sourced species are reported (Table 3). Simply stated, a lack of consensus between rodent studies and clinical outcomes predominates. Confounding this scenario is a general lack of reported literature results that directly compare the two host scenarios for common human vs. rodent tolerability metrics. Given the general positive response for SIS implants in human hernia repair, the question becomes whether the same host response is actually seen, but has no effect on patient well-being, or whether there truly is a less severe host FBR observed in human use versus animal models. Beyond the example of SIS for hernia repair, that this finding consistently represents the general case for SIS in all implant locations remains unproven. Such a retrospective analysis of results to date and their reporting is challenging but needed.
Porcine SIS has been studied for over 20 years, yet there remains no direct consensus on the detailed biocompatiblity outcomes and how host response varies across mammalian species. Currently, SIS is regarded as safe to use and is thought to be a better mesh implant than similar synthetic polymeric materials [197]. The extensive history and ongoing work with this ECM-based biomaterial should serve as the standard for benchmarking future decellularized biomaterial development, informing the biomaterials community as to how to accurately assess preclinical and clinical outcomes and evaluate successes and failures in translation. Importantly, different tissue processing techniques from the same source (i.e., porcine SIS) show markedly different results [198], further complicating the selection and de-risking of new efficacious ECM-based materials, and highlighting the need for detailed material characterization post-decellularization/processing. As more tissues are decellularized and developed as possible clinical products, SIS history should be carefully examined to not repeat the same mistakes, and to emulate relative SIS success with other future ECM-derived implant materials.
Conclusions
Matrix protein-based biomaterials and ECM implants have a long track record of investigation, some with clinical translation. Yet, despite substantial clinical experience, basic mechanisms of biomaterial integration with human tissues, and rejection responses in some cases, remain unexplained and poorly dissected. In many respects, researchers still pursue questions posed nearly a half century ago as to how to craft human proteins into functional, compatible biomaterials. Decellularization of tissues and organs to produce tissue-specific ECM represents the latest chapter in this protein-based biomaterials saga, facing primarily the same issues and questions, and with similarly few answers. Host response mechanisms are not well understood, and design principles for guiding ECM processing, purity, composition, and microstructure are not evident or benchmarked.
Nearly all major organs and tissue have been decellularized for use as scaffolding biomaterials, both for in vitro cell growth or implantation as complex biomaterials, primarily to guide wound healing and tissue regeneration. Some ECM clinical translation has occurred, but this has occurred slowly, at substantial cost, commercial risk, and without much momentum as difficulties remain in identifying and validating what important ECM components must be included in purified product, and what potential contaminants must be eliminated. Even those obvious contaminants that must be eliminated (e.g., endotoxins, nucleic acids, extraction aids) have few validated ECM-relevant assays to monitor them. What else that remains as trace contaminants or that constitutes ECM compositional and structural heterogeneity and that might therefore define ECM purity and performance in vivo remains unknown. The current non-standard, unvalidated and arbitrary collection of tissue decellularization protocols has little guidance or enforcement from recognized expert bodies such as ASTM, FDA, or ISO organizations. Identification and standard execution of best-practices decellularization protocols are best obtained through consensus via endorsed, rigorously applied, proven and then standardized methods.
Sufficient evidence exists that decellularized and other protein- and ECM-based biomaterials can have interesting research-focused and impacting clinical applications and contains the requisite properties to regenerate into functional tissue. Increasing amounts of human-relevant data can serve as precedent to establishing new decellularized biomaterials technologies. However, a full, scientifically mature understanding of how decellularized ECM biomaterials specifically engage host tissues, and how host tissue reacts to ECM implants, compositions and forms in diverse context is required. Comprehensive analytical validations of matrix purity, standardization of methods of extraction and purification, and vetting in proper preclinical models using accepted methods are compelling. Without such protocols and evidence, currently required for all synthetic biomaterial implants, protein- and ECM-based biomaterials development will remain inconsistent and empirically based without rational scientific explanations for its implant performance.
Acknowledgments
Authors acknowledge support from NIH grant EB011879
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Karp G. Cell and molecular biology concepts and experiments. Hoboken, NJ: John Wiley; 2010. [Google Scholar]
- 2.Badylak SF, Freytes DO, Gilbert TW. Extracellular matrix as a biological scaffold material: Structure and function. Acta Biomater. 2009;5:1–13. doi: 10.1016/j.actbio.2008.09.013. [DOI] [PubMed] [Google Scholar]
- 3.Badylak SF, Taylor D, Uygun K. Whole-organ tissue engineering: decellularization and recellularization of three-dimensional matrix scaffolds. Annu Rev Biomed Eng. 2011;13:27–53. doi: 10.1146/annurev-bioeng-071910-124743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gilbert TW, Sellaro TL, Badylak SF. Decellularization of tissues and organs. Biomaterials. 2006;27:3675–83. doi: 10.1016/j.biomaterials.2006.02.014. [DOI] [PubMed] [Google Scholar]
- 5.Anderson JM, Rodriguez A, Chang DT. Foreign body reaction to biomaterials. Semin Immunol. 2008;20:86–100. doi: 10.1016/j.smim.2007.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Coleman D, King R, Andrade J. The foreign body reaction: a chronic inflammatory response. Journal of biomedical materials research. 1974;8:199–211. doi: 10.1002/jbm.820080503. [DOI] [PubMed] [Google Scholar]
- 7.Onuki Y, Bhardwaj U, Papadimitrakopoulos F, Burgess DJ. A review of the biocompatibility of implantable devices: current challenges to overcome foreign body response. Journal of diabetes science and technology. 2008;2:1003–15. doi: 10.1177/193229680800200610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ward WK. A review of the foreign-body response to subcutaneously-implanted devices: the role of macrophages and cytokines in biofouling and fibrosis. Journal of diabetes science and technology. 2008;2:768–77. doi: 10.1177/193229680800200504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Badylak SF. Xenogeneic extracellular matrix as a scaffold for tissue reconstruction. Transpl Immunol. 2004;12:367–77. doi: 10.1016/j.trim.2003.12.016. [DOI] [PubMed] [Google Scholar]
- 10.Badylak SF. Decellularized allogeneic and xenogeneic tissue as a bioscaffold for regenerative medicine: factors that influence the host response. Annals of biomedical engineering. 2014;42:1517–27. doi: 10.1007/s10439-013-0963-7. [DOI] [PubMed] [Google Scholar]
- 11.Badylak SF, Gilbert TW. Immune response to biologic scaffold materials. Semin Immunol. 2008;20:109–16. doi: 10.1016/j.smim.2007.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Singelyn JM, Christman KL. Injectable materials for the treatment of myocardial infarction and heart failure: the promise of decellularized matrices. Journal of Cardiovascular Translational Research. 2010;3:478–86. doi: 10.1007/s12265-010-9202-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang L, Cao Z, Bai T, Carr L, Ella-Menye JR, Irvin C, et al. Zwitterionic hydrogels implanted in mice resist the foreign-body reaction. Nature biotechnology. 2013;31:553–6. doi: 10.1038/nbt.2580. [DOI] [PubMed] [Google Scholar]
- 14.Yagi M, Miyamoto T, Sawatani Y, Iwamoto K, Hosogane N, Fujita N, et al. DC-STAMP is essential for cell–cell fusion in osteoclasts and foreign body giant cells. The Journal of experimental medicine. 2005;202:345–51. doi: 10.1084/jem.20050645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kyriakides TR, Foster MJ, Keeney GE, Tsai A, Giachelli CM, Clark-Lewis I, et al. The CC Chemokine Ligand, CCL2/MCP1, Participates in Macrophage Fusion and Foreign Body Giant Cell Formation. The American journal of pathology. 2004;165:2157–66. doi: 10.1016/S0002-9440(10)63265-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Luttikhuizen DT, Harmsen MC, Van Luyn MJ. Cellular and molecular dynamics in the foreign body reaction. Tissue Eng. 2006;12:1955–70. doi: 10.1089/ten.2006.12.1955. [DOI] [PubMed] [Google Scholar]
- 17.Ratner BD. Reducing capsular thickness and enhancing angiogenesis around implant drug release systems. Journal of Controlled Release. 2002;78:211–8. doi: 10.1016/s0168-3659(01)00502-8. [DOI] [PubMed] [Google Scholar]
- 18.Badylak SF, Valentin JE, Ravindra AK, McCabe GP, Stewart-Akers AM. Macrophage phenotype as a determinant of biologic scaffold remodeling. Tissue Engineering Part A. 2008;14:1835–42. doi: 10.1089/ten.tea.2007.0264. [DOI] [PubMed] [Google Scholar]
- 19.Kyriakides TR, Leach KJ, Hoffman AS, Ratner BD, Bornstein P. Mice that lack the angiogenesis inhibitor, thrombospondin 2, mount an altered foreign body reaction characterized by increased vascularity. Proceedings of the National Academy of Sciences. 1999;96:4449–54. doi: 10.1073/pnas.96.8.4449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.van Tienen TG, Heijkants RGJC, Buma P, de Groot JH, Pennings AJ, Veth RPH. Tissue ingrowth and degradation of two biodegradable porous polymers with different porosities and pore sizes. Biomaterials. 2002;23:1731–8. doi: 10.1016/s0142-9612(01)00280-0. [DOI] [PubMed] [Google Scholar]
- 21.Holt DJ, Chamberlain LM, Grainger DW. Cell-cell signaling in co-cultures of macrophages and fibroblasts. Biomaterials. 2010;31:9382–94. doi: 10.1016/j.biomaterials.2010.07.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Higgins DM, Basaraba RJ, Hohnbaum AC, Lee EJ, Grainger DW, Gonzalez-Juarrero M. Localized immunosuppressive environment in the foreign body response to implanted biomaterials. Am J Pathol. 2009;175:161–70. doi: 10.2353/ajpath.2009.080962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Busscher HJ, van der Mei HC, Subbiahdoss G, Jutte PC, van den Dungen JJ, Zaat SA, et al. Biomaterial-associated infection: locating the finish line in the race for the surface. Science Translational Medicine. 2012;4:153rv10–rv10. doi: 10.1126/scitranslmed.3004528. [DOI] [PubMed] [Google Scholar]
- 24.Bruce Alberts AJ, Lewis Julian, Raff Martin, Roberts Keith, Walter Peter. Molecular Biology of the Cell. 5. New York, NY: Garland Science; 2008. [Google Scholar]
- 25.Harbers GM, Grainger DW. Cell-material interactions: fundamental design issues for tissue engineering and clinical considerations. CRC Press; Boca Raton, FL: 2005. [Google Scholar]
- 26.Rosso F, Giordano A, Barbarisi M, Barbarisi A. From cell-ECM interactions to tissue engineering. J Cell Physiol. 2004;199:174–80. doi: 10.1002/jcp.10471. [DOI] [PubMed] [Google Scholar]
- 27.Chvapil M, Holuša R. Experimental experiences with the collagen sponge as hemostaticum and tampon. Journal of biomedical materials research. 1968;2:245–64. doi: 10.1002/jbm.820020208. [DOI] [PubMed] [Google Scholar]
- 28.Mergenhagen SE, Martin GR, Rizzo AA, Wright DN, Scott DB. Calcification in vivo of implanted collagen. Biochimica et biophysica acta. 1960;43:563–5. doi: 10.1016/0006-3002(60)90488-1. [DOI] [PubMed] [Google Scholar]
- 29.Pullinger B, Pirie A. Chronic inflammation due to implanted colagen. The Journal of Pathology and Bacteriology. 1942;54:341–4. [Google Scholar]
- 30.Ungar H, Feldman JD. The Absorption of Collagen in the Liver: I. Histologic Changes Accompanying the Absorption of Implanted Surgical Gut in the Liver*. The American journal of pathology. 1953;29:963. [PMC free article] [PubMed] [Google Scholar]
- 31.Kamer FM, Churukian MM. Clinical use of injectable collagen: a three-year retrospective review. Archives of Otolaryngology. 1984;110:93–8. doi: 10.1001/archotol.1984.00800280027008. [DOI] [PubMed] [Google Scholar]
- 32.Keefe J, Wauk L, Chu S, DeLustro F. Clinical use of injectable bovine collagen: a decade of experience. Clinical materials. 1992;9:155–62. doi: 10.1016/0267-6605(92)90095-b. [DOI] [PubMed] [Google Scholar]
- 33.Parker DM, Armstrong PJ, Frizzi JD, North JH. Porcine dermal collagen (Permacol) for abdominal wall reconstruction. Current surgery. 2006;63:255–8. doi: 10.1016/j.cursur.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 34.Ruszczak Z. Effect of collagen matrices on dermal wound healing. Advanced Drug Delivery Reviews. 2003;55:1595–611. doi: 10.1016/j.addr.2003.08.003. [DOI] [PubMed] [Google Scholar]
- 35.Ueno T, Pickett LC, Sebastian G, Lawson DC, Pappas TN. Clinical application of porcine small intestinal submucosa in the management of infected or potentially contaminated abdominal defects. Journal of gastrointestinal surgery. 2004;8:109–12. doi: 10.1016/j.gassur.2003.09.025. [DOI] [PubMed] [Google Scholar]
- 36.Rammelt S, Schulze E, Bernhardt R, Hanisch U, Scharnweber D, Worch H, et al. Coating of titanium implants with type-I collagen. Journal of Orthopaedic Research. 2004;22:1025–34. doi: 10.1016/j.orthres.2004.02.011. [DOI] [PubMed] [Google Scholar]
- 37.Sinani VA, Koktysh DS, Yun B-G, Matts RL, Pappas TC, Motamedi M, et al. Collagen Coating Promotes Biocompatibility of Semiconductor Nanoparticles in Stratified LBL Films. Nano Letters. 2003;3:1177–82. [Google Scholar]
- 38.Cen L, Liu W, Cui L, Zhang W, Cao Y. Collagen tissue engineering: development of novel biomaterials and applications. Pediatric research. 2008;63:492–6. doi: 10.1203/PDR.0b013e31816c5bc3. [DOI] [PubMed] [Google Scholar]
- 39.Rothamel D, Schwarz F, Sager M, Herten M, Sculean A, Becker J. Biodegradation of differently cross-linked collagen membranes: an experimental study in the rat. Clinical oral implants research. 2005;16:369–78. doi: 10.1111/j.1600-0501.2005.01108.x. [DOI] [PubMed] [Google Scholar]
- 40.Umashankar P, Arun T, Kumari T. Short duration gluteraldehyde cross linking of decellularized bovine pericardium improves biological response. Journal of Biomedical Materials Research Part A. 2011;97:311–20. doi: 10.1002/jbm.a.33061. [DOI] [PubMed] [Google Scholar]
- 41.Hanke CW, Higley HR, Jolivette DM, Swanson NA, Stegman SJ. Abscess formation and local necrosis after treatment with Zyderm or Zyplast collagen implant. Journal of the American Academy of Dermatology. 1991;25:319–26. doi: 10.1016/0190-9622(91)70200-l. [DOI] [PubMed] [Google Scholar]
- 42.Mermoud A, Schnyder CC, Sickenberg M, Chiou AG, Hédiguer SE, Faggioni R. Comparison of deep sclerectomy with collagen implant and trabeculectomy in open-angle glaucoma. Journal of Cataract & Refractive Surgery. 1999;25:323–31. doi: 10.1016/s0886-3350(99)80079-0. [DOI] [PubMed] [Google Scholar]
- 43.Brooks N. A Foreign Body Granuloma Produced by an Injectable Collagen Implant at a Test Site. The Journal of Dermatologic Surgery and Oncology. 1982;8:111–4. doi: 10.1111/j.1524-4725.1982.tb00247.x. [DOI] [PubMed] [Google Scholar]
- 44.Lynn AK, Yannas IV, Bonfield W. Antigenicity and immunogenicity of collagen. J Biomed Mater Res B Appl Biomater. 2004;71:343–54. doi: 10.1002/jbm.b.30096. [DOI] [PubMed] [Google Scholar]
- 45.Delgado Luis M, Zeugolis Dimitrios I. To cross-link or not to cross-link? Cross-linking associated foreign body response of collagen-based devices. Tissue Engineering Part B: Reviews. 2015 doi: 10.1089/ten.teb.2014.0290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.McPherson J, Sawamura S, Armstrong R. An examination of the biologic response to injectable, glutaraldehyde cross-linked collagen implants. Journal of biomedical materials research. 1986;20:93–107. doi: 10.1002/jbm.820200109. [DOI] [PubMed] [Google Scholar]
- 47.Niu G, Criswell T, Sapoznik E, Lee S, Soker S. The influence of cross-linking methods on the mechanical and biocompatible properties of vascular scaffold. J Sci Appl Biomed. 2013;1:1–7. [Google Scholar]
- 48.Chau DY, Collighan RJ, Verderio EA, Addy VL, Griffin M. The cellular response to transglutaminase-cross-linked collagen. Biomaterials. 2005;26:6518–29. doi: 10.1016/j.biomaterials.2005.04.017. [DOI] [PubMed] [Google Scholar]
- 49.Fortunati D, San Chau DY, Wang Z, Collighan RJ, Griffin M. Cross-linking of collagen I by tissue transglutaminase provides a promising biomaterial for promoting bone healing. Amino acids. 2014;46:1751–61. doi: 10.1007/s00726-014-1732-0. [DOI] [PubMed] [Google Scholar]
- 50.Jus S, Stachel I, Schloegl W, Pretzler M, Friess W, Meyer M, et al. Cross-linking of collagen with laccases and tyrosinases. Materials Science and Engineering: C. 2011;31:1068–77. [Google Scholar]
- 51.Deeken CR, Eliason BJ, Pichert MD, Grant SA, Frisella MM, Matthews BD. Differentiation of biologic scaffold materials through physicomechanical, thermal, and enzymatic degradation techniques. Annals of surgery. 2012;255:595–604. doi: 10.1097/SLA.0b013e3182445341. [DOI] [PubMed] [Google Scholar]
- 52.Sandor M, Xu H, Connor J, Lombardi J, Harper JR, Silverman RP, et al. Host response to implanted porcine-derived biologic materials in a primate model of abdominal wall repair. Tissue Eng Part A. 2008;14:2021–31. doi: 10.1089/ten.tea.2007.0317. [DOI] [PubMed] [Google Scholar]
- 53.Gorgieva S, Kokol V. Collagen-vs. gelatine-based biomaterials and their biocompatibility: review and perspectives. INTECH Open Access Publisher; 2011. [Google Scholar]
- 54.Mescher AL. Junqueira’s basic histology: text & atlas. McGraw-Hill Medical; New York: 2010. [Google Scholar]
- 55.Gorham S. Biomaterials. Stockton Press; New York: 1991. Collagen; pp. 55–122. [Google Scholar]
- 56.Cooperman L, Michaeli D. The immunogenicity of injectable collagen. I. A 1-year prospective study. Journal of the American Academy of Dermatology. 1984;10:638–46. doi: 10.1016/s0190-9622(84)80271-6. [DOI] [PubMed] [Google Scholar]
- 57.Friess W. Collagen – biomaterial for drug delivery 1. European Journal of Pharmaceutics and Biopharmaceutics. 1998;45:113–36. doi: 10.1016/s0939-6411(98)00017-4. [DOI] [PubMed] [Google Scholar]
- 58.Wahl D, Czernuszka J. Collagen-hydroxyapatite composites for hard tissue repair. Eur Cell Mater. 2006;11:43–56. doi: 10.22203/ecm.v011a06. [DOI] [PubMed] [Google Scholar]
- 59.Crapo PM, Gilbert TW, Badylak SF. An overview of tissue and whole organ decellularization processes. Biomaterials. 2011;32:3233–43. doi: 10.1016/j.biomaterials.2011.01.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.McPherson TBLH, Record RD, Badylak SF. Gal(alpha1,3)Gal Epitope in Porcine Small Intestinal Submucosa. Tissue Engineering. 2000;6:233–9. doi: 10.1089/10763270050044416. [DOI] [PubMed] [Google Scholar]
- 61.Paolo Macchiarini PJ, Go Tetsuhiko, Adelaide Asnaghi M, Rees Louisa E, Cogan Tristan A, Dodson Amanda, Martorell Jaume, Silvia Bellini PPP, Dickinson Sally C, Hollander Anthony P, Mantero Sara, Conconi Maria Teresa, Birchall Martin A. Clinical transplantation of a tissue-engineered airway. The Lancet. 2008;372:2023–30. doi: 10.1016/S0140-6736(08)61598-6. [DOI] [PubMed] [Google Scholar]
- 62.Rieder E, Kasimir M-T, Silberhumer G, Seebacher G, Wolner E, Simon P, et al. Decellularization protocols of porcine heart valves differ importantly in efficiency of cell removal and susceptibility of the matrix to recellularization with human vascular cells. The Journal of Thoracic and Cardiovascular Surgery. 2004;127:399–405. doi: 10.1016/j.jtcvs.2003.06.017. [DOI] [PubMed] [Google Scholar]
- 63.Simon P, Kasimir M, Seebacher G, Weigel G, Ullrich R, Salzer-Muhar U, et al. Early failure of the tissue engineered porcine heart valve SYNERGRAFT® in pediatric patients. European journal of cardio-thoracic surgery. 2003;23:1002–6. doi: 10.1016/s1010-7940(03)00094-0. [DOI] [PubMed] [Google Scholar]
- 64.Simon CG, Yaszemski MJ, Ratcliffe A, Tomlins P, Luginbuehl R, Tesk JA. ASTM international workshop on standards and measurements for tissue engineering scaffolds. Journal of Biomedical Materials Research Part B: Applied Biomaterials. 2014 doi: 10.1002/jbm.b.33286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Grauss RW, Hazekamp MG, Oppenhuizen F, van Munsteren CJ, Gittenberger-de Groot AC, DeRuiter MC. Histological evaluation of decellularised porcine aortic valves: matrix changes due to different decellularisation methods. Eur J Cardiothorac Surg. 2005;27:566–71. doi: 10.1016/j.ejcts.2004.12.052. [DOI] [PubMed] [Google Scholar]
- 66.Schenke-Layland K, Riemann I, Opitz F, König K, Halbhuber K, Stock U. Comparative study of cellular and extracellular matrix composition of native and tissue engineered heart valves. Matrix biology. 2004;23:113–25. doi: 10.1016/j.matbio.2004.03.005. [DOI] [PubMed] [Google Scholar]
- 67.Valentin JE, Badylak JS, McCabe GP, Badylak SF. Extracellular matrix bioscaffolds for orthopaedic applications. A comparative histologic study. J Bone Joint Surg Am. 2006;88:2673–86. doi: 10.2106/JBJS.E.01008. [DOI] [PubMed] [Google Scholar]
- 68.Yu C, Bianco J, Brown C, Fuetterer L, Watkins JF, Samani A, et al. Porous decellularized adipose tissue foams for soft tissue regeneration. Biomaterials. 2013;34:3290–302. doi: 10.1016/j.biomaterials.2013.01.056. [DOI] [PubMed] [Google Scholar]
- 69.Hoganson DM, O’Doherty EM, Owens GE, Harilal DO, Goldman SM, Bowley CM, et al. The retention of extracellular matrix proteins and angiogenic and mitogenic cytokines in a decellularized porcine dermis. Biomaterials. 2010;31:6730–7. doi: 10.1016/j.biomaterials.2010.05.019. [DOI] [PubMed] [Google Scholar]
- 70.Barnes CA, Brison J, Michel R, Brown BN, Castner DG, Badylak SF, et al. The surface molecular functionality of decellularized extracellular matrices. Biomaterials. 2011;32:137–43. doi: 10.1016/j.biomaterials.2010.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Boer U, Lohrenz A, Klingenberg M, Pich A, Haverich A, Wilhelmi M. The effect of detergent-based decellularization procedures on cellular proteins and immunogenicity in equine carotid artery grafts. Biomaterials. 2011;32:9730–7. doi: 10.1016/j.biomaterials.2011.09.015. [DOI] [PubMed] [Google Scholar]
- 72.Welham NV, Chang Z, Smith LM, Frey BL. Proteomic analysis of a decellularized human vocal fold mucosa scaffold using 2D electrophoresis and high-resolution mass spectrometry. Biomaterials. 2013;34:669–76. doi: 10.1016/j.biomaterials.2012.09.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Elder BD, Eleswarapu SV, Athanasiou KA. Extraction techniques for the decellularization of tissue engineered articular cartilage constructs. Biomaterials. 2009;30:3749–56. doi: 10.1016/j.biomaterials.2009.03.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Schenke-Layland K, Vasilevski O, Opitz F, König K, Riemann I, Halbhuber KJ, et al. Impact of decellularization of xenogeneic tissue on extracellular matrix integrity for tissue engineering of heart valves. Journal of Structural Biology. 2003;143:201–8. doi: 10.1016/j.jsb.2003.08.002. [DOI] [PubMed] [Google Scholar]
- 75.Dunne LW, Huang Z, Meng W, Fan X, Zhang N, Zhang Q, et al. Human decellularized adipose tissue scaffold as a model for breast cancer cell growth and drug treatments. Biomaterials. 2014;35:4940–9. doi: 10.1016/j.biomaterials.2014.03.003. [DOI] [PubMed] [Google Scholar]
- 76.Holt DJ, Grainger DW. Demineralized bone matrix as a vehicle for delivering endogenous and exogenous therapeutics in bone repair. Advanced Drug Delivery Reviews. 2012;64:1123–8. doi: 10.1016/j.addr.2012.04.002. [DOI] [PubMed] [Google Scholar]
- 77.Uygun BE, Soto-Gutierrez A, Yagi H, Izamis M-L, Guzzardi MA, Shulman C, et al. Organ reengineering through development of a transplantable recellularized liver graft using decellularized liver matrix. Nature medicine. 2010;16:814–20. doi: 10.1038/nm.2170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Harbers DWGGM. Cell-material interactions: fundamental design issues for tissue engineering and clinical considerations. In: Guelcher SA, editor. An introduction to biomaterials. Boca Raton, FL: CRC Press; 2006. [Google Scholar]
- 79.Werb Z. ECM and cell surface proteolysis: regulating cellular ecology. Cell. 1997;91:439–42. doi: 10.1016/s0092-8674(00)80429-8. [DOI] [PubMed] [Google Scholar]
- 80.Bantscheff M, Schirle M, Sweetman G, Rick J, Kuster B. Quantitative mass spectrometry in proteomics: a critical review. Analytical and bioanalytical chemistry. 2007;389:1017–31. doi: 10.1007/s00216-007-1486-6. [DOI] [PubMed] [Google Scholar]
- 81.Goh SK, Bertera S, Olsen P, Candiello JE, Halfter W, Uechi G, et al. Perfusion-decellularized pancreas as a natural 3D scaffold for pancreatic tissue and whole organ engineering. Biomaterials. 2013;34:6760–72. doi: 10.1016/j.biomaterials.2013.05.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Brown BN, Barnes CA, Kasick RT, Michel R, Gilbert TW, Beer-Stolz D, et al. Surface characterization of extracellular matrix scaffolds. Biomaterials. 2010;31:428–37. doi: 10.1016/j.biomaterials.2009.09.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Griffiths LG, Choe LH, Reardon KF, Dow SW, Christopher Orton E. Immunoproteomic identification of bovine pericardium xenoantigens. Biomaterials. 2008;29:3514–20. doi: 10.1016/j.biomaterials.2008.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Hernandez PMM, Appel RD. Automated Protein Identification by Tandem Mass Spectrometry: Issues and Strategies. Mass Spectrometry Reviews. 2006:235–54. doi: 10.1002/mas.20068. [DOI] [PubMed] [Google Scholar]
- 85.Nesvizhskii AI. A survey of computational methods and error rate estimation procedures for peptide and protein identification in shotgun proteomics. Journal of proteomics. 2010;73:2092–123. doi: 10.1016/j.jprot.2010.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Salmi J, Nyman TA, Nevalainen OS, Aittokallio T. Filtering strategies for improving protein identification in high-throughput MS/MS studies. Proteomics. 2009;9:848–60. doi: 10.1002/pmic.200800517. [DOI] [PubMed] [Google Scholar]
- 87.Canavan HE, Graham DJ, Cheng X, Ratner BD, Castner DG. Comparison of native extracellular matrix with adsorbed protein films using secondary ion mass spectrometry. Langmuir. 2007;23:50–6. doi: 10.1021/la062330o. [DOI] [PubMed] [Google Scholar]
- 88.Li Q, Uygun BE, Geerts S, Ozer S, Scalf M, Gilpin SE, et al. Proteomic analysis of naturally-sourced biological scaffolds. Biomaterials. 2016;75:37–46. doi: 10.1016/j.biomaterials.2015.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Lee CH, GM, Grainger DW, Gamble LJ, Castner DG. Fluorescence, XPS, and TOF-SIMS Surface Chemical State Image Analysis of DNA Microarrays. J Am Chem Soc. 2007:9429–38. doi: 10.1021/ja071879m. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Keller Bernd OJS, Young Alex B, Whittal Randy M. Interferences and contaminants encountered in modern mass spectrometry. Analytica Chimica Acta. 2008:71–81. doi: 10.1016/j.aca.2008.04.043. [DOI] [PubMed] [Google Scholar]
- 91.Bantscheff M, Lemeer S, Savitski MM, Kuster B. Quantitative mass spectrometry in proteomics: critical review update from 2007 to the present. Analytical and bioanalytical chemistry. 2012;404:939–65. doi: 10.1007/s00216-012-6203-4. [DOI] [PubMed] [Google Scholar]
- 92.Gilbert TW, Freund JM, Badylak SF. Quantification of DNA in biologic scaffold materials. J Surg Res. 2009;152:135–9. doi: 10.1016/j.jss.2008.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Hemmi H, Takeuchi O, Kawai T, Kaisho T, Sato S, Sanjo H, et al. A Toll-like receptor recognizes bacterial DNA. Nature. 2000;408:740–5. doi: 10.1038/35047123. [DOI] [PubMed] [Google Scholar]
- 94.Karayel E, Burckstummer T, Bilban M, Durnberger G, Weitzer S, Martinez J, et al. The TLR-independent DNA recognition pathway in murine macrophages: Ligand features and molecular signature. European journal of immunology. 2009;39:1929–36. doi: 10.1002/eji.200939344. [DOI] [PubMed] [Google Scholar]
- 95.Stacey KJ, Sweet MJ, Hume DA. Macrophages ingest and are activated by bacterial DNA. The Journal of Immunology. 1996;157:2116–22. [PubMed] [Google Scholar]
- 96.Wong ML, Griffiths LG. Immunogenicity in xenogeneic scaffold generation: antigen removal vs. decellularization. Acta Biomater. 2014;10:1806–16. doi: 10.1016/j.actbio.2014.01.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Aurora A, McCarron J, Iannotti JP, Derwin K. Commercially available extracellular matrix materials for rotator cuff repairs: state of the art and future trends. Journal of Shoulder and Elbow Surgery. 2007;16:S171–S8. doi: 10.1016/j.jse.2007.03.008. [DOI] [PubMed] [Google Scholar]
- 98.Magalhães PO, Lopes AM, Mazzola PG, Rangel-Yagui C, Penna T, Pessoa A., Jr Methods of endotoxin removal from biological preparations: a review. J Pharm Pharm Sci. 2007;10:388–404. [PubMed] [Google Scholar]
- 99.Gorbet MB, Sefton MV. Endotoxin: the uninvited guest. Biomaterials. 2005;26:6811–7. doi: 10.1016/j.biomaterials.2005.04.063. [DOI] [PubMed] [Google Scholar]
- 100.Daly KA, Liu S, Agrawal V, Brown BN, Huber A, Johnson SA, et al. The host response to endotoxin-contaminated dermal matrix. Tissue Engineering Part A. 2012;18:1293–303. doi: 10.1089/ten.TEA.2011.0597. [DOI] [PubMed] [Google Scholar]
- 101.Nalepka JL, Greenfield EM. Detection of bacterial endotoxin in human tissues. Biotechniques. 2004;37:413–7. doi: 10.2144/04373ST06. [DOI] [PubMed] [Google Scholar]
- 102.Jones CF, Grainger DW. In vitro assessments of nanomaterial toxicity. Adv Drug Deliv Rev. 2009;61:438–56. doi: 10.1016/j.addr.2009.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Ragab AA, Van De Motter R, Lavish SA, Goldberg VM, Ninomiya JT, Carlin CR, et al. Measurement and removal of adherent endotoxin from titanium particles and implant surfaces. Journal of Orthopaedic Research. 1999;17:803–9. doi: 10.1002/jor.1100170603. [DOI] [PubMed] [Google Scholar]
- 104.Roch T, Schulz C, Jung F, Ma N, Lendlein A. Interaction of poly (ether imide) films with early immune mechanisms. Clinical hemorheology and microcirculation. 2014;57:203–12. doi: 10.3233/CH-141831. [DOI] [PubMed] [Google Scholar]
- 105.Ung DY, Woodhouse KA, Sefton MV. Tumor necrosis factor (TNFα) production by rat peritoneal macrophages is not polyacrylate surface-chemistry dependent. Journal of biomedical materials research. 1999;46:324–30. doi: 10.1002/(sici)1097-4636(19990905)46:3<324::aid-jbm3>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 106.Haile LA, Puig M, Kelley-Baker L, Verthelyi D. Detection of Innate Immune Response Modulating Impurities in Therapeutic Proteins. PLoS One. 2015;10:e0125078. doi: 10.1371/journal.pone.0125078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Benichou G, Takizawa P, Olson C, McMillan M, Sercarz E. Donor major histocompatibility complex (MHC) peptides are presented by recipient MHC molecules during graft rejection. The Journal of experimental medicine. 1992;175:305–8. doi: 10.1084/jem.175.1.305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Galili U, Clark MR, Shohet SB, Buehler J, Macher BA. Evolutionary relationship between the natural anti-Gal antibody and the Gal alpha 1----3Gal epitope in primates. Proceedings of the National Academy of Sciences. 1987;84:1369–73. doi: 10.1073/pnas.84.5.1369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Gould DS, Auchincloss H. Direct and indirect recognition: the role of MHC antigens in graft rejection. Immunology today. 1999;20:77–82. doi: 10.1016/s0167-5699(98)01394-2. [DOI] [PubMed] [Google Scholar]
- 110.Vaughan HA, Loveland BE, Sandrin MS. GAL [alpha](1, 3) GAL IS THE MAJOR XENOEPITOPE EXPRESSED ON PIG ENDOTHELIAL CELLS RECOGNIZED BY NATURALLY OCCURRING CYTOTOXIC HUMAN ANTIBODIES. Transplantation. 1994;58:879–82. doi: 10.1097/00007890-199410270-00003. [DOI] [PubMed] [Google Scholar]
- 111.Sandrin M, Mckenzie IF. Galα (1, 3) Gal, the major xenoantigen (s) recognised in pigs by human natural antibodies. Immunological reviews. 1994;141:169–90. doi: 10.1111/j.1600-065x.1994.tb00877.x. [DOI] [PubMed] [Google Scholar]
- 112.Auchincloss H., Jr XENOGENEIC TRANSPLANTATION: A REVIEW. Transplantation. 1988;46:1–20. doi: 10.1097/00007890-198807000-00001. [DOI] [PubMed] [Google Scholar]
- 113.Badylak SF. The extracellular matrix as a scaffold for tissue reconstruction. Semin Cell Dev Biol. 2002;13:377–83. doi: 10.1016/s1084952102000940. [DOI] [PubMed] [Google Scholar]
- 114.He W, Yong T, Teo WE, Ma Z, Ramakrishna S. Fabrication and endothelialization of collagen-blended biodegradable polymer nanofibers: potential vascular graft for blood vessel tissue engineering. Tissue Engineering. 2005;11:1574–88. doi: 10.1089/ten.2005.11.1574. [DOI] [PubMed] [Google Scholar]
- 115.Brown BN, Freund JM, Han L, Rubin JP, Reing JE, Jeffries EM, et al. Comparison of three methods for the derivation of a biologic scaffold composed of adipose tissue extracellular matrix. Tissue Eng Part C Methods. 2011;17:411–21. doi: 10.1089/ten.tec.2010.0342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Ott HC, Matthiesen TS, Goh SK, Black LD, Kren SM, Netoff TI, et al. Perfusion-decellularized matrix: using nature’s platform to engineer a bioartificial heart. Nature medicine. 2008;14:213–21. doi: 10.1038/nm1684. [DOI] [PubMed] [Google Scholar]
- 117.Whitlock PW, Smith TL, Poehling GG, Shilt JS, Van Dyke M. A naturally derived, cytocompatible, and architecturally optimized scaffold for tendon and ligament regeneration. Biomaterials. 2007;28:4321–9. doi: 10.1016/j.biomaterials.2007.05.029. [DOI] [PubMed] [Google Scholar]
- 118.Elder BD, Eleswarapu SV, Athanasiou KA. Extraction techniques for the decellularization of tissue engineered articular cartilage constructs. Biomaterials. 2009;30:3749–56. doi: 10.1016/j.biomaterials.2009.03.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Kasimir M, Rieder E, Seebacher G, Silberhumer G, Wolner E, Weigel G, et al. Comparison of different decellularization procedures of porcine heart valves. The International journal of artificial organs. 2003;26:421–7. doi: 10.1177/039139880302600508. [DOI] [PubMed] [Google Scholar]
- 120.Akhyari P, Aubin H, Gwanmesia P, Barth M, Hoffmann S, Huelsmann J, et al. The quest for an optimized protocol for whole-heart decellularization: a comparison of three popular and a novel decellularization technique and their diverse effects on crucial extracellular matrix qualities. Tissue Engineering Part C: Methods. 2011;17:915–26. doi: 10.1089/ten.TEC.2011.0210. [DOI] [PubMed] [Google Scholar]
- 121.Flynn LE. The use of decellularized adipose tissue to provide an inductive microenvironment for the adipogenic differentiation of human adipose-derived stem cells. Biomaterials. 2010;31:4715–24. doi: 10.1016/j.biomaterials.2010.02.046. [DOI] [PubMed] [Google Scholar]
- 122.Li W-J, Tuli R, Okafor C, Derfoul A, Danielson KG, Hall DJ, et al. A three-dimensional nanofibrous scaffold for cartilage tissue engineering using human mesenchymal stem cells. Biomaterials. 2005;26:599–609. doi: 10.1016/j.biomaterials.2004.03.005. [DOI] [PubMed] [Google Scholar]
- 123.Cortiella J, Niles J, Cantu A, Brettler A, Pham A, Vargas G, et al. Influence of acellular natural lung matrix on murine embryonic stem cell differentiation and tissue formation. Tissue Eng Part A. 2010;16:2565–80. doi: 10.1089/ten.tea.2009.0730. [DOI] [PubMed] [Google Scholar]
- 124.Flynn L, Prestwich GD, Semple JL, Woodhouse KA. Adipose tissue engineering with naturally derived scaffolds and adipose-derived stem cells. Biomaterials. 2007;28:3834–42. doi: 10.1016/j.biomaterials.2007.05.002. [DOI] [PubMed] [Google Scholar]
- 125.Gui L, Muto A, Chan SA, Breuer CK, Niklason LE. Development of decellularized human umbilical arteries as small-diameter vascular grafts. Tissue Engineering Part A. 2009;15:2665–76. doi: 10.1089/ten.tea.2008.0526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Discher DE, Mooney DJ, Zandstra PW. Growth factors, matrices, and forces combine and control stem cells. Science. 2009;324:1673–7. doi: 10.1126/science.1171643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Higuchi A, Ling Q-D, Chang Y, Hsu S-T, Umezawa A. Physical cues of biomaterials guide stem cell differentiation fate. Chemical reviews. 2013;113:3297–328. doi: 10.1021/cr300426x. [DOI] [PubMed] [Google Scholar]
- 128.Reilly GC, Engler AJ. Intrinsic extracellular matrix properties regulate stem cell differentiation. Journal of biomechanics. 2010;43:55–62. doi: 10.1016/j.jbiomech.2009.09.009. [DOI] [PubMed] [Google Scholar]
- 129.Blit PH, Shen YH, Ernsting MJ, Woodhouse KA, Santerre JP. Bioactivation of porous polyurethane scaffolds using fluorinated RGD surface modifiers. J Biomed Mater Res A. 2010;94:1226–35. doi: 10.1002/jbm.a.32804. [DOI] [PubMed] [Google Scholar]
- 130.Lutolf M, Hubbell J. Synthetic biomaterials as instructive extracellular microenvironments for morphogenesis in tissue engineering. Nature biotechnology. 2005;23:47–55. doi: 10.1038/nbt1055. [DOI] [PubMed] [Google Scholar]
- 131.Rosso F, Marino G, Giordano A, Barbarisi M, Parmeggiani D, Barbarisi A. Smart materials as scaffolds for tissue engineering. Journal of cellular physiology. 2005;203:465–70. doi: 10.1002/jcp.20270. [DOI] [PubMed] [Google Scholar]
- 132.Stevens MM, George JH. Exploring and engineering the cell surface interface. Science. 2005;310:1135–8. doi: 10.1126/science.1106587. [DOI] [PubMed] [Google Scholar]
- 133.Lynn AD, Kyriakides TR, Bryant SJ. Characterization of the in vitro macrophage response and in vivo host response to poly(ethylene glycol)-based hydrogels. J Biomed Mater Res A. 2010;93:941–53. doi: 10.1002/jbm.a.32595. [DOI] [PubMed] [Google Scholar]
- 134.Lu T-Y, Lin B, Kim J, Sullivan M, Tobita K, Salama G, et al. Repopulation of decellularized mouse heart with human induced pluripotent stem cell-derived cardiovascular progenitor cells. Nature communications. 2013;4 doi: 10.1038/ncomms3307. [DOI] [PubMed] [Google Scholar]
- 135.Elman JS, Murray RM, Wang F, Shen K, Gao S, Conway KE, et al. Pharmacokinetics of Natural and Engineered Secreted Factors Delivered by Mesenchymal Stromal Cells. PLoS One. 2014;9:e89882. doi: 10.1371/journal.pone.0089882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Flaim CJ, Chien S, Bhatia SN. An extracellular matrix microarray for probing cellular differentiation. Nature methods. 2005;2:119–25. doi: 10.1038/nmeth736. [DOI] [PubMed] [Google Scholar]
- 137.Kou PM, Babensee JE. Macrophage and dendritic cell phenotypic diversity in the context of biomaterials. J Biomed Mater Res A. 2011;96:239–60. doi: 10.1002/jbm.a.32971. [DOI] [PubMed] [Google Scholar]
- 138.Breier G, Albrecht U, Sterrer S, Risau W. Expression of vascular endothelial growth factor during embryonic angiogenesis and endothelial cell differentiation. Development. 1992;114:521–32. doi: 10.1242/dev.114.2.521. [DOI] [PubMed] [Google Scholar]
- 139.Johe KK, Hazel TG, Muller T, Dugich-Djordjevic MM, McKay R. Single factors direct the differentiation of stem cells from the fetal and adult central nervous system. Genes & development. 1996;10:3129–40. doi: 10.1101/gad.10.24.3129. [DOI] [PubMed] [Google Scholar]
- 140.Kratchmarova I, Blagoev B, Haack-Sorensen M, Kassem M, Mann M. Mechanism of divergent growth factor effects in mesenchymal stem cell differentiation. Science. 2005;308:1472–7. doi: 10.1126/science.1107627. [DOI] [PubMed] [Google Scholar]
- 141.Schuldiner M, Yanuka O, Itskovitz-Eldor J, Melton DA, Benvenisty N. Effects of eight growth factors on the differentiation of cells derived from human embryonic stem cells. Proceedings of the National Academy of Sciences. 2000;97:11307–12. doi: 10.1073/pnas.97.21.11307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Parker MW, Rossi D, Peterson M, Smith K, Sikström K, White ES, et al. Fibrotic extracellular matrix activates a profibrotic positive feedback loop. The Journal of clinical investigation. 2014;124:1622. doi: 10.1172/JCI71386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Williams DF. On the mechanisms of biocompatibility. Biomaterials. 2008;29:2941–53. doi: 10.1016/j.biomaterials.2008.04.023. [DOI] [PubMed] [Google Scholar]
- 144.Anderson JM. Biological responses to materials. Annu Rev Mater Res. 2001;31:81–110. [Google Scholar]
- 145.Pearce A, Richards R, Milz S, Schneider E, Pearce S. Animal models for implant biomaterial research in bone: a review. Eur Cell Mater. 2007;13:1–10. doi: 10.22203/ecm.v013a01. [DOI] [PubMed] [Google Scholar]
- 146.Himms-Hagen J. Physiological roles of the leptin endocrine system: differences between mice and humans. Critical reviews in clinical laboratory sciences. 1999;36:575–655. doi: 10.1080/10408369991239259. [DOI] [PubMed] [Google Scholar]
- 147.Odom DT, Dowell RD, Jacobsen ES, Gordon W, Danford TW, MacIsaac KD, et al. Tissue-specific transcriptional regulation has diverged significantly between human and mouse. Nature genetics. 2007;39:730–2. doi: 10.1038/ng2047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Puente XS, Sánchez LM, Overall CM, López-Otín C. Human and mouse proteases: a comparative genomic approach. Nature Reviews Genetics. 2003;4:544–58. doi: 10.1038/nrg1111. [DOI] [PubMed] [Google Scholar]
- 149.Angius D, Wang H, Spinner RJ, Gutierrez-Cotto Y, Yaszemski MJ, Windebank AJ. A systematic review of animal models used to study nerve regeneration in tissue-engineered scaffolds. Biomaterials. 2012;33:8034–9. doi: 10.1016/j.biomaterials.2012.07.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Wong VW, Sorkin M, Glotzbach JP, Longaker MT, Gurtner GC. Surgical approaches to create murine models of human wound healing. BioMed Research International. 2010:2011. doi: 10.1155/2011/969618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Khouw IMSL, Van Wachem PB, Plantinga JA, Haagmans BL, De Leij LFMH, Van Luyn MJA. Foreign-body reaction to dermal sheep collagen in interferon-γ-receptor knock-out mice. J Biomed Mater Res. 2000;50:259–66. doi: 10.1002/(sici)1097-4636(200005)50:2<259::aid-jbm21>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 152.Kidd KR, Dal Ponte DB, Kellar RS, Williams SK. A comparative evaluation of the tissue responses associated with polymeric implants in the rat and mouse. Journal of biomedical materials research. 2002;59:682–9. doi: 10.1002/jbm.10032. [DOI] [PubMed] [Google Scholar]
- 153.Luttikhuizen DT, Harmsen MC, van Luyn MJ. Cytokine and chemokine dynamics differ between rats and mice after collagen implantation. J Tissue Eng Regen Med. 2007;1:398–405. doi: 10.1002/term.50. [DOI] [PubMed] [Google Scholar]
- 154.Hu W-J, Eaton JW, Ugarova TP, Tang L. Molecular basis of biomaterial-mediated foreign body reactions. Blood. 2001;98:1231–8. doi: 10.1182/blood.v98.4.1231. [DOI] [PubMed] [Google Scholar]
- 155.Kyriakides TR, Bornstein P. Matricellular proteins as modulators of wound healing and the foreign body response. THROMBOSIS AND HAEMOSTASIS-STUTTGART- 2003;90:986–92. doi: 10.1160/TH03-06-0399. [DOI] [PubMed] [Google Scholar]
- 156.Keselowsky BG, Bridges AW, Burns KL, Tate CC, Babensee JE, LaPlaca MC, et al. Role of plasma fibronectin in the foreign body response to biomaterials. Biomaterials. 2007;28:3626–31. doi: 10.1016/j.biomaterials.2007.04.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Rodriguez A, MacEwan SR, Meyerson H, Kirk JT, Anderson JM. The foreign body reaction in T-cell-deficient mice. Journal of Biomedical Materials Research Part A. 2009;90:106–13. doi: 10.1002/jbm.a.32050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Kheir E, Stapleton T, Shaw D, Jin Z, Fisher J, Ingham E. Development and characterization of an acellular porcine cartilage bone matrix for use in tissue engineering. Journal of Biomedical Materials Research Part A. 2011;99:283–94. doi: 10.1002/jbm.a.33171. [DOI] [PubMed] [Google Scholar]
- 159.Rowland CR, Little D, Guilak F. Factors influencing the long-term behavior of extracellular matrix-derived scaffolds for musculoskeletal soft tissue repair. Journal of long-term effects of medical implants. 2012;22 doi: 10.1615/jlongtermeffmedimplants.2013006120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Takahashi H, Wang Y, Grainger DW. Device-based local delivery of siRNA against mammalian target of rapamycin (mTOR) in a murine subcutaneous implant model to inhibit fibrous encapsulation. J Control Release. 2010;147:400–7. doi: 10.1016/j.jconrel.2010.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Bratlie KM, Dang TT, Lyle S, Nahrendorf M, Weissleder R, Langer R, et al. Rapid biocompatibility analysis of materials via in vivo fluorescence imaging of mouse models. PLoS One. 2010;5:e10032. doi: 10.1371/journal.pone.0010032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Ansaloni L, Catena F, Gagliardi S, Gazzotti F, D’Alessandro L, Pinna A. Hernia repair with porcine small-intestinal submucosa. Hernia. 2007;11:321–6. doi: 10.1007/s10029-007-0225-4. [DOI] [PubMed] [Google Scholar]
- 163.Medberry CJ, Tottey S, Jiang H, Johnson SA, Badylak SF. Resistance to Infection of Five Different Materials in a Rat Body Wall Model. Journal of surgical research. 2012;173:38–44. doi: 10.1016/j.jss.2010.08.035. [DOI] [PubMed] [Google Scholar]
- 164.Mooney JE, Rolfe BE, Osborne GW, Sester DP, van Rooijen N, Campbell GR, et al. Cellular plasticity of inflammatory myeloid cells in the peritoneal foreign body response. The American journal of pathology. 2010;176:369–80. doi: 10.2353/ajpath.2010.090545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Poland CA, Duffin R, Kinloch I, Maynard A, Wallace WA, Seaton A, et al. Carbon nanotubes introduced into the abdominal cavity of mice show asbestos-like pathogenicity in a pilot study. Nature nanotechnology. 2008;3:423–8. doi: 10.1038/nnano.2008.111. [DOI] [PubMed] [Google Scholar]
- 166.Rucker M, Laschke MW, Junker D, Carvalho C, Schramm A, Mulhaupt R, et al. Angiogenic and inflammatory response to biodegradable scaffolds in dorsal skinfold chambers of mice. Biomaterials. 2006;27:5027–38. doi: 10.1016/j.biomaterials.2006.05.033. [DOI] [PubMed] [Google Scholar]
- 167.Laschke MW, Vollmar B, Menger MD. The dorsal skinfold chamber: window into the dynamic interaction of biomaterials with their surrounding host tissue. Eur Cell Mater. 2011;22:147–64. doi: 10.22203/ecm.v022a12. discussion 64–7. [DOI] [PubMed] [Google Scholar]
- 168.Laschke M, Häufel J, Thorlacius H, Menger M. New experimental approach to study host tissue response to surgical mesh materials in vivo. Journal of Biomedical Materials Research Part A. 2005;74:696–704. doi: 10.1002/jbm.a.30371. [DOI] [PubMed] [Google Scholar]
- 169.Marchant R, Hiltner A, Hamlin C, Rabinovitch A, Slobodkin R, Anderson JM. In vivo biocompatibility studies. I. The cage implant system and a biodegradable hydrogel. Journal of biomedical materials research. 1983;17:301–25. doi: 10.1002/jbm.820170209. [DOI] [PubMed] [Google Scholar]
- 170.Ronneberger B, Kao WJ, Anderson JM, Kissel T. In vivo biocompatibility study of ABA triblock copolymers consisting of poly (L-lactic-co-glycolic acid) A blocks attached to central poly (oxyethylene) B blocks. Journal of biomedical materials research. 1996;30:31–40. doi: 10.1002/(SICI)1097-4636(199601)30:1<31::AID-JBM5>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 171.Kim J, Dadsetan M, Ameenuddin S, Windebank AJ, Yaszemski MJ, Lu L. In vivo biodegradation and biocompatibility of PEG/sebacic acid-based hydrogels using a cage implant system. Journal of Biomedical Materials Research Part A. 2010;95:191–7. doi: 10.1002/jbm.a.32810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Wolf MT, Daly KA, Brennan-Pierce EP, Johnson SA, Carruthers CA, D’Amore A, et al. A hydrogel derived from decellularized dermal extracellular matrix. Biomaterials. 2012;33:7028–38. doi: 10.1016/j.biomaterials.2012.06.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Lopez-Soler RI, Brennan MP, Goyal A, Wang Y, Fong P, Tellides G, et al. Development of a mouse model for evaluation of small diameter vascular grafts. Journal of surgical research. 2007;139:1–6. doi: 10.1016/j.jss.2006.07.040. [DOI] [PubMed] [Google Scholar]
- 174.Biran R, Martin DC, Tresco PA. Neuronal cell loss accompanies the brain tissue response to chronically implanted silicon microelectrode arrays. Experimental neurology. 2005;195:115–26. doi: 10.1016/j.expneurol.2005.04.020. [DOI] [PubMed] [Google Scholar]
- 175.Puleo D, Nanci A. Understanding and controlling the bone–implant interface. Biomaterials. 1999;20:2311–21. doi: 10.1016/s0142-9612(99)00160-x. [DOI] [PubMed] [Google Scholar]
- 176.Cong L, Ran FA, Cox D, Lin S, Barretto R, Habib N, et al. Multiplex genome engineering using CRISPR/Cas systems. Science. 2013;339:819–23. doi: 10.1126/science.1231143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Honda A, Hirose M, Sankai T, Yasmin L, Yuzawa K, Honsho K, et al. Single-step generation of rabbits carrying a targeted allele of the tyrosinase gene using CRISPR/Cas9. Experimental Animals. 2015;64:31. doi: 10.1538/expanim.14-0034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Wang H, Yang H, Shivalila CS, Dawlaty MM, Cheng AW, Zhang F, et al. One-step generation of mice carrying mutations in multiple genes by CRISPR/Cas-mediated genome engineering. Cell. 2013;153:910–8. doi: 10.1016/j.cell.2013.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Hahn WC, Weinberg RA. Rules for making human tumor cells. New England Journal of Medicine. 2002;347:1593–603. doi: 10.1056/NEJMra021902. [DOI] [PubMed] [Google Scholar]
- 180.Gordon S, Taylor PR. Monocyte and macrophage heterogeneity. Nature Reviews Immunology. 2005;5:953–64. doi: 10.1038/nri1733. [DOI] [PubMed] [Google Scholar]
- 181.Valentin JE, Stewart-Akers AM, Gilbert TW, Badylak SF. Macrophage participation in the degradation and remodeling of extracellular matrix scaffolds. Tissue Engineering Part A. 2009;15:1687–94. doi: 10.1089/ten.tea.2008.0419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Tang L, Jennings TA, Eaton JW. Mast cells mediate acute inflammatory responses to implanted biomaterials. Proceedings of the National Academy of Sciences of the United States of America. 1998;95:8841–6. doi: 10.1073/pnas.95.15.8841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Thevenot PT, Baker DW, Weng H, Sun MW, Tang L. The pivotal role of fibrocytes and mast cells in mediating fibrotic reactions to biomaterials. Biomaterials. 2011;32:8394–403. doi: 10.1016/j.biomaterials.2011.07.084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Avula MN, Rao AN, McGill LD, Grainger DW, Solzbacher F. Foreign body response to subcutaneous biomaterial implants in a mast cell-deficient Kit murine model. Acta Biomater. 2014 doi: 10.1016/j.actbio.2013.12.056. [DOI] [PubMed] [Google Scholar]
- 185.Bischoff SC. Role of mast cells in allergic and non-allergic immune responses: comparison of human and murine data. Nature Reviews Immunology. 2007;7:93–104. doi: 10.1038/nri2018. [DOI] [PubMed] [Google Scholar]
- 186.Shultz LD, Brehm MA, Garcia-Martinez JV, Greiner DL. Humanized mice for immune system investigation: progress, promise and challenges. Nature Reviews Immunology. 2012;12:786–98. doi: 10.1038/nri3311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Bee YS, Alonzo B, Ng JD. Review of AlloDerm Acellular Human Dermis Regenerative Tissue Matrix in Multiple Types of Oculofacial Plastic and Reconstructive Surgery. Ophthalmic plastic and reconstructive surgery. 2015;31:348–51. doi: 10.1097/IOP.0000000000000339. [DOI] [PubMed] [Google Scholar]
- 188.Franklin M, Gonzalez J, Michaelson R, Glass J, Chock D. Preliminary experience with new bioactive prosthetic material for repair of hernias in infected fields. Hernia. 2002;6:171–4. doi: 10.1007/s10029-002-0078-9. [DOI] [PubMed] [Google Scholar]
- 189.Ho K-LV, Witte MN, Bird ET. 8-Ply Small Intestinal Submucosa Tension-Free Sling:: Spectrum of Postoperative Inflammation. The Journal of urology. 2004;171:268–71. doi: 10.1097/01.ju.0000098680.60020.32. [DOI] [PubMed] [Google Scholar]
- 190.Franklin ME, Jr, Treviño JM, Portillo G, Vela I, Glass JL, González JJ. The use of porcine small intestinal submucosa as a prosthetic material for laparoscopic hernia repair in infected and potentially contaminated fields: long-term follow-up. Surgical endoscopy. 2008;22:1941–6. doi: 10.1007/s00464-008-0005-y. [DOI] [PubMed] [Google Scholar]
- 191.Ansaloni L, Catena F, Coccolini F, Gazzotti F, D’Alessandro L, Pinna AD. Inguinal hernia repair with porcine small intestine submucosa: 3-year follow-up results of a randomized controlled trial of Lichtenstein’s repair with polypropylene mesh versus Surgisis Inguinal Hernia Matrix. The American Journal of Surgery. 2009;198:303–12. doi: 10.1016/j.amjsurg.2008.09.021. [DOI] [PubMed] [Google Scholar]
- 192.Konstantinovic ML, Lagae P, Zheng F, Verbeken EK, De Ridder D, Deprest JA. Comparison of host response to polypropylene and non-cross-linked porcine small intestine serosal-derived collagen implants in a rat model. BJOG: An International Journal of Obstetrics & Gynaecology. 2005;112:1554–60. doi: 10.1111/j.1471-0528.2005.00688.x. [DOI] [PubMed] [Google Scholar]
- 193.Petter-Puchner A, Fortelny R, Mittermayr R, Walder N, Öhlinger W, Redl H. Adverse effects of porcine small intestine submucosa implants in experimental ventral hernia repair. Surgical Endoscopy and Other Interventional Techniques. 2006;20:942–6. doi: 10.1007/s00464-005-0568-9. [DOI] [PubMed] [Google Scholar]
- 194.Prevel CD, Eppley BL, Summerlin D-J, Jackson JR, McCarty M, Badylak SF. Small intestinal submucosa: utilization for repair of rodent abdominal wall defects. Annals of plastic surgery. 1995;35:374–80. [PubMed] [Google Scholar]
- 195.Badylak S, Kokini K, Tullius B, Simmons-Byrd A, Morff R. Morphologic study of small intestinal submucosa as a body wall repair device. Journal of surgical research. 2002;103:190–202. doi: 10.1006/jsre.2001.6349. [DOI] [PubMed] [Google Scholar]
- 196.Zheng M, Chen J, Kirilak Y, Willers C, Xu J, Wood D. Porcine small intestine submucosa (SIS) is not an acellular collagenous matrix and contains porcine DNA: possible implications in human implantation. Journal of Biomedical Materials Research Part B: Applied Biomaterials. 2005;73:61–7. doi: 10.1002/jbm.b.30170. [DOI] [PubMed] [Google Scholar]
- 197.Nie X, Xiao D, Wang W, Song Z, Yang Z, Chen Y, et al. Comparison of Porcine Small Intestinal Submucosa versus Polypropylene in Open Inguinal Hernia Repair: A Systematic Review and Meta-Analysis. PLoS One. 2015;10:e0135073. doi: 10.1371/journal.pone.0135073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.de Castro Bras LE, Proffitt JL, Bloor S, Sibbons PD. Effect of crosslinking on the performance of a collagen-derived biomaterial as an implant for soft tissue repair: a rodent model. J Biomed Mater Res B Appl Biomater. 2010;95:239–49. doi: 10.1002/jbm.b.31704. [DOI] [PubMed] [Google Scholar]