Abstract
Aim
To describe the perceptions of young adults with sickle cell disease concerning their disease experience.
Background
Sickle cell disease is a lifelong, genetic condition with both acute and chronic painful exacerbations. Little is known of the experiences of young adults with sickle cell disease.
Design
This study used a qualitative, descriptive design with semi-structured, life-review interviews.
Methods
Between August 2010 – September 2012, purposive sampling was used to recruit participants with a known sickle cell disease diagnosis who were ages 18–35 years, were being seen in an outpatient sickle cell clinic and were English speaking. Participants provided demographic information and responded to two interviews. A content analysis was then used to interpret participants’ narratives of their experiences of living with sickle cell disease.
Results/Findings
A sample of 29 young adults with sickle cell disease consisted of 79.3% females, 35.6% employed full-time or part-time, 71.6% single/never married and 57.8% with sickle cell anemia. Their mean age was 25.8 with 13.2 years of education. Four major interview themes were identified: 1) struggles to maintain or achieve good quality of life or life satisfactions; 2) strategies to maintain self-care; 3) interruptions to family, work and social roles; and 4) difficulties accessing needed healthcare.
Conclusion
Young adults face many challenges while living with sickle cell disease. With a better understanding of their disease experience and how it influences their quality of life, researchers can begin tailoring appropriate interventions to improve health outcomes in this vulnerable, minority population.
Keywords: sickle cell disease, sickle cell, young adults, chronic disease challenges, chronic disease management, nursing
INTRODUCTION
Sickle cell disease (SCD) is the most common, genetic, blood disorder in the United States (Genetic Home Reference 2015). Approximately 100,000 individuals are affected and the disease occurs primarily among individuals of African descent (Centers for Disease Control and Prevention 2011). The disease is associated with abnormal hemoglobin and sickle-shaped red blood cells that result in vaso-occlusion, ischemia, tissue damage, progressive organ damage and early death (Ballas et al. 2012, Darbari et al. 2014, Olowoyeye & Okwundu 2014). It is mainly characterized by chronic pain with periods of acute, severe pain (called pain crises) that occur throughout life and are often unpredictable (Howard & Oteng-Ntim 2012). Bone marrow or stem cell transplantation is the only cure for SCD but this is not possible for many because of limited, potential donors (Ataga 2009), procedural complications due to age and advanced disease and fatal side effects (Buchanan et al. 2010). Consequently, disease management occurs mostly at home and focuses on pain, hydration and preventing complications that result in pain crises (Lee et al. 2012).
Sickle cell disease is nationally and internationally associated with pain (Ballas et al. 2012), high healthcare costs (Kauf et al. 2009), lost productivity (Taylor et al. 2010) and impaired quality of life (Panepinto & Bonner 2012). Young adults with SCD, in particular, face many issues and experience health-related challenges which include managing the chronic illness while accessing and navigating the healthcare system (Jenerette & Brewer 2010). Successful living with SCD requires using management strategies to overcome the many challenges that are experienced. There are limited studies which evaluate the perceptions of young adults with SCD concerning their disease experience, thus this required investigation.
Background
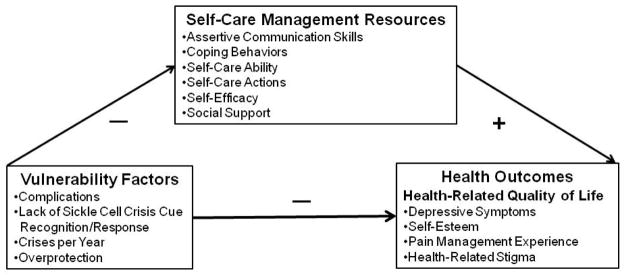
Living with a chronic illness like SCD requires lifestyle changes to manage or control symptoms and to prevent potential life-threatening complications (Lowe & McBride-Henry 2012). These lifestyle changes include learning to cope with the illness, growing as a person and incorporating the illness into the context of one’s life rather than focusing on illness needs (Schulman-Green et al. 2012). Because self-care management is important to these processes, the Theory of Self-Care Management for SCD (Figure 1) guided this research. This theory, developed by the fourth author, states that self-care management resources positively mediate the relationships among vulnerability factors and health outcomes (Jenerette et al. 2014). Vulnerability factors, which relate to additional challenges of the disease, negatively affect care resources and health outcomes. Because self-care management resources can mitigate the influence of vulnerability factors on health outcomes, it was expected that study participants would report using the resources included in the theory as they are vital to the disease management process. Disease management strategies used by middle-aged and older adults with SCD are physiologic, psychological and provider-related (Jenerette et al. 2011). They also note the importance of emotional support, career selection and success factors, advocacy and physical activity (Tanabe et al. 2010).
Figure 1.
Theory of Self-Care Management for Sickle Cell Disease
As individuals aim to continue daily activities and live a good life despite having a chronic illness (Audulv 2013), challenges often arise. This is particularly true for young adults living with SCD. Young adults, ages 18–39, with SCD experience the highest rates of pain crises (Yusuf et al. 2010), hospitalizations and rehospitalizations (Brousseau et al. 2010). Approximately 1.8 years after young adults transition from pediatric to adult care, typically between ages 18 and 25 (Sobota et al. 2011), there is a high risk of early death (Quinn et al. 2010). Young adults are not knowledgeable of the adult SCD care system and they have limited decision-making experience (Jordan et al. 2013). Given their African descent, young adults with SCD also experience a confluence of racial issues and they are at risk for health-related stigmatization due to disease challenges (Jenerette & Brewer 2010).
Healthcare is another important aspect of SCD management. Gaining access to this care, however, is often difficult. In general, African Americans experience less access to care than Caucasians, they experience higher rates of being uninsured or having Medicaid coverage and are most likely to use the emergency department (ED) for primary care (Cheatham et al. 2008, United States Department of Health and Human Services, Agency for Healthcare Research and Quality 2012). Individuals with SCD experience disease challenges that result in a lack of education and employment, thus financial hardships (Matthie et al. 2014). Young adults are not likely to be financially independent and they have had a change in or loss of insurance (Jordan et al. 2013). Altogether, these factors limit the ability of young adults with SCD to consistently access healthcare and/or afford some management modalities. There is also a shortage of providers with SCD expertise, especially in low-income areas (Sobota et al. 2011). Few care resources are available to those who are uninsured or under-insured and there are likely to be reimbursement issues and/or low profits associated with coverage through aid programs; providers are less apt to accept patients with this type of coverage. Consequently, young adults with SCD often use the ED as a primary source of care.
THE STUDY
Aim
To describe the perceptions of young adults with SCD concerning their disease experience.
Design
This study used a qualitative, descriptive design (Sandelowksi 2010) that included criterion purposeful sampling (Patton 2002), semi-structured interviews and conventional content analysis (Hsieh & Shannon 2005).
Participants
Criterion purposeful sampling guided the recruitment process to target African Americans with a diagnosis of SCD and to be able to discuss their disease experience and use of any self-care strategies. Participants were drawn from individuals randomized to the attention control group of a self-care management intervention study (Jenerette et al. 2014). Eligibility criteria for participants in this larger study included an age of 18–35 years, a confirmed diagnosis of SCD and an ability to participate in the life review interviews.
Data collection
Potential participants for the interviews were contacted, in person, during a scheduled clinic visit and were provided information about the study. Written consent was obtained prior to the interviews and participants received a $25 store gift card for each completed interview. Interviews were conducted in a private area of a SCD clinic before or immediately after a scheduled appointment or via telephone. All interviews were conducted by the fourth author and were audio recorded.
The final sample size of 29 was determined by the number of individuals randomized to the control group who were willing to participate in the interviews. Data collection started in August 2010 and was completed in September 2012. The interviews were conducted in two sessions that coincided with the delivery of the two-session intervention. Session 1 of the interviews focused on childhood to high school memories while session 2 focused on participants’ lives as young adults living with SCD. Interview questions were guided by a modified Successful Aging with SCD Life Review Interview Guide that was previously used among middle-aged and older adults with SCD (Jenerette et al. 2011, Jenerette & Lauderdale 2008). Questions included: ‘Can you talk about some of the main difficulties you feel like you’ve experienced as a young adult living with sickle cell disease?’ ‘So thinking back about some difficulties you’ve encountered, can you tell me more about…?’ The average interview time was approximately 30 minutes for each session. A complete description and rationale for the life review interviews was previously reported (Jenerette et al. 2014).
Ethical considerations
Prior to study initiation, approval was obtained from the Institutional Review Board of the university associated with the SCD clinic. Study details, the ability to withdraw at any time and confidentiality issues (including the anonymous reporting of findings) were discussed with each potential participant during recruitment. Subsequently, written informed consent was obtained from all participants.
Data analysis
The interviews were audiotaped, transcribed verbatim and checked for accuracy by the fourth author. A conventional, qualitative, content analysis was then used to describe participants’ disease experience (Hsieh & Shannon 2005). The analysis of narratives from open-ended interviews generated categories or a typology of disease management strategies through a process of coding expressions directly from text (Hsieh & Shannon 2005). The initial coding consisted of reading the narrative text and highlighting words or phrases that captured the experience. Labeling was done for codes that emerged from the narratives and were organized into meaningful categories and subcategories (Hsieh & Shannon 2005). In the final step, a table with categories and subcategories of data, along with definitions for each category, was constructed. All authors reviewed this table and provided feedback.
Rigour
Strategies to optimize validity of the data included verification of the accuracy of the transcripts, prolonged engagement with respondents with persistent observation and respondent validation of interviewer understandings of the data throughout the interviews (Maxwell 2013). Specifically, member checking was conducted throughout data collection whereby the interviewer asked respondents to clarify statements made during the interviews or to explain the meaning of expressions observed during responses to questions. Member checking during data collection also consisted of asking respondents to comment on the accuracy of the interviewer’s conclusions or summaries of phrases or statements made during the interviews (Sandelowski 2008). In addition, the coding was reviewed by all authors and refined until agreement was reached. The fourth author is a researcher with over 20 years of experience on topics related to challenges encountered by individuals with SCD. The second author is an expert in qualitative methods and led the data analysis. All authors reviewed the findings for accuracy of the themes generated, interpretations of data and conclusions.
FINDINGS
A total of 29 young adults with SCD participated in the life review interviews. The sample consisted of 79.3% females, 35.6% employed full-time or part-time, 71.6% single/never married and 57.8% with a SCD type of sickle cell anemia. Their mean age was 25.8 (SD 4.8) years with 13.2 (SD 2.3) years of education. All participants self-identified as African American and were English speaking.
The four interview themes included: 1) struggles to maintain or achieve good quality of life or life satisfactions; 2) strategies to maintain self-care; 3) interruptions to family, work and social roles; and 4) difficulties accessing needed healthcare. They are presented according to the frequency with which they were discussed among participants. Table 1 depicts demographic data for the participants who were selected for thematic exemplars. Pseudonyms have been used to maintain their confidentiality.
Table 1.
Select Participant Demographic Data
| Pseudonym | Age (M = 25.8) | SCD Type | Pain Level | Crises per Year |
|---|---|---|---|---|
| Amy | 31 | Beta Thal. | 8 | 3 |
| Beverly | 28 | SC | 10 | 1 |
| Evelyn | 29 | SS | 10 | 2.5 |
| Francine | 28 | SS | 10 | 0.5 |
| Gabriella | 31 | SS | 9 | 1 |
| Henry | 22 | SS | 7.5 | 3 |
| Isaac | 28 | Beta Thal. | 10 | 0.5 |
| Jasmine | 20 | NS | 10 | 12 |
| Kimberly | 28 | NS | 8 | 2 |
Beta Thal = Sickle beta thalassemia; SC = Sickle hemoglobin C; SS = Sickle cell anemia; NS = Respondent not sure
Struggles to maintain or achieve good quality of life or life satisfactions
All participants discussed their struggles to achieve what they believed was a good quality of life or life satisfactions. These discussions focused on mental and physical health issues participants had to overcome and on their struggles to be ‘normal’, that is, to be like or to do activities similar to their peers:
Acceptance of SCD was a part of these discussions. Evelyn stated:
I just struggle day to day just to make it and not have pain… Yeah, I would love to not have sickle cell no more, but I’ve grown to accept it. It’s a part of me…It’s not who I am, but this is what I have to live with.
For other participants, perceptions of quality of life and being ‘normal’ were influenced by having an optimistic perceptive on life in general. Jasmine stated:
I know how I am and I really don’t like to let many things take me down, so I would say my quality of life is great. You deal with the things that come. I really wouldn’t say I have a bad quality of life. I don’t look at it that way… because I have a cousin that’s my age. Well, I have a lot of cousins, but the ones that is around my age, I could do everything they did, even if it wasn’t as long as they did it or if they did, I still did pretty much the same thing they did, just not as much.
Supportive family, friends and religion also influenced quality of life for participants. Friendships were not always easy to come by and were difficult to maintain. However, religion was the foundation for a positive outlook on life. Gabriella explains:
Religion plays a huge role. My family….religion has always been an essential thing in our family and my relationship with the Lord and just involvement in church, it played a big role for me and as far as my sickle cell and, number one, just helping me to stay positive to realize that, OK, yeah, I might have this, but there is obviously a purpose or reason for it and even though I don’t understand it, that I’m going to be OK and just helping me to stay positive.
Strategies to maintain self-care
Among the 29 participants, 28 used strategies to maintain self-care. Self-care strategies are activities and behaviors used to enhance health, limit disability from SCD, or control symptoms occurring as a direct result of SCD. Participants discussed the effect of pain and painful SCD crises on every aspect of their lives and the strategies they used to minimize pain or to prevent the occurrence of painful SCD crises that would lead to hospitalizations. The recognition of cues or triggers to a crisis was of paramount importance in avoiding hospitalizations. Isaac described averting a crisis by taking immediate actions to start over-the-counter pain medications and to bolster his immune system:
I was going to say if you could catch it right at the beginning…the beginning stages of sickle cell you feel a little nag. I would say take whatever medicine – Ibuprofen, that’s what I take…I take medicine as needed. If I need medicine, then I will take medicine. That’s just me. Other people might disagree or whatever but I found that if you use your natural body immune system and you try to up your immune system as best possible and then as needed do take medicine.
Henry also spoke of strategies used to respond to early cues of a SCD crisis:
…some of my first cues are, normally my body feels real dry. It’s hard to explain, but you normally can tell when you feel dehydrated and that’s normally one of my first cues that I know I am going to start hurting. Then the second cue would normally be my eyes because my eyes always start to turn a yellowish color normally before I get sick. And one of the third things is I might end up having small aches, like the aches that don’t stop me from doing anything, but I know that if I don’t try to catch it early, it’s going to go into something else…I start noticing little things like that. That’s when you’ll notice I’ll always have a water bottle in my hand even though I know I should keep one in my hand at all times. But I normally would try to do stuff like that or try to soak in a bathtub and try to figure out whether it’s because I’m sore from working out or normally if you soak and you’re sore from working out, it gets better. But when it’s a pain crisis and you soak, it [soaking] normally doesn’t really help.
Participants learned early in life that avoidance of extreme temperatures, stress and fatigue would aid in preventing SCD crises. They used strategies to control their physical environment and stressful situations or to control their food and drink intake. For example, Francine reported the following:
Sometimes I’ll get just small lower back pain or sharp pains through my legs…Either I try to figure if I’m too hot or too cold and I adjust the temperature or I rest…Drink a lot more fluids.
Amy learned to recognize fatigue and to limit physical activities when needed:
You need to know when you’ve been running too much, running around because I know I’ve pushed myself to the limit so I’ll get really tired. I’m like, OK, let me lay down, because next step is you’re going to be sick and your defenses are low, you know, down, you running yourself ragged. So you just need to know when it’s time to lay down and do nothing…I think mostly that you have to know your limits and just knowing your limits and not getting stressed out because I noticed that causes me crisis sometimes and just having a balance of things.
Participants also used their religion as a form of comfort when in pain. Beverly stated:
…because it’s God who gets me through the pain. All I can do is pray when the pain is unbearable…Prayer helps. It really does. It soothes me and calms me down at the same time.
A final strategy used among participants was that of just being aware and increasing their own self-knowledge of how to care for themselves. Gabriella stated:
Learning to recognize what works for you as far as your treatment goes. When you go to the doctor, don’t be afraid to ask questions. If they are giving you something, don’t be afraid to ask, ‘OK, what is that? How much did you give me?’ and pay attention. When you went to the emergency room and they gave you morphine, did that work? If that didn’t work, the next time you went and they gave you something different, did that work? So just pay attention to your body. Pay attention to your crises and what happens when you have one. Pay attention to what works for you as far as your treatment goes. I mean, even with home medicine, paying attention. OK, if I just lay here and be still and be quiet, does that help or do I need to get up and move around or should I turn on the radio? I think it’s a lot of self-knowledge. You have to just really be aware and then being aware of what works for you and what doesn’t because what makes me feel better might not make you feel better.
Interruptions to family, work and social roles
Among 25 participants, discussions focused on ways SCD led to interruptions to family, work and social roles. Interruptions included the lack of completion of a traditional four-year college degree, the inability to obtain and maintain employment and difficulties in maintaining social relationships.
Participants discussed the challenges of obtaining an education and maintaining employment. One participant spoke of not being able to endure the physical requirements for a four-year college degree and having to choose career paths that required a less strenuous time commitment. Participants also described how the disease interrupted their ability to obtain what they described as the ‘good jobs’ or even to maintain these jobs. Beverly shared her experience:
I lost a lot of jobs behind being sick and in pain and lot of jobs were challenging because of the pains. So I would say it was poor because I wasn’t able to keep a job and I wasn’t able to get a good job because of the poor work history behind it… It’s just…most of those jobs, it felt like after I got sick and I went in the hospital and everything… After I went back, it was pretty much over with – the job… I didn’t think they wanted to hold on to someone that was questionable, whether they are going to be there for a couple of days or so a lot of it ended up like that.
Some jobs were too physically demanding. Evelyn stated:
…it started getting to where I couldn’t stand. Well, I was having trouble standing because I was a cashier. I had to let that go because I couldn’t do that much standing.
Also problematic were the interruptions to developing and maintaining social relationships that occurred as a direct result of SCD and other associated morbidities. In one interview, Kimberly described interruptions to her social life:
I specifically remember before I had the second hip replacement I went on vacation with a bunch of friends. We went on a beach vacation and I was honestly, stuck on the beach the whole time because I couldn’t do the other things they were doing. I couldn’t go parasailing. I couldn’t really get in the water. I didn’t do a lot because it just hurt to move all the time. . . .
Difficulties accessing needed healthcare
For 9 participants, transitioning to adulthood meant a loss of private insurance and changes in healthcare providers, disruptions to quality of care and continuity of care, challenges to paying healthcare bills and delays in seeking healthcare. Amy described her experience: stated:
I started out with a private doctor when I was in college and then when I got too old to be on my parents’ medical insurance…But not having health insurance didn’t stop me from going to the doctor…I’m sick, I just have to [get some service] and worry about it [paying] later because there are lot of people dying because they don’t have insurance and they think they can’t pay for it or they know they can’t and they just don’t go to the doctor…I’m going to go regardless and figure out how to pay for it later.
Although participants continued to have physical access to healthcare, their care may have been less than optimal or not of the same quality as that received through private insurance and under the watchful eye of a parent. Participants’ experience with pain control from healthcare providers outside of specialized SCD clinics was sometimes not satisfactory and may have contributed to delays in care. For example, Gabriella stated:
Like locally, like around where I live at, they act like they don’t know what to do. You have to tell them, I’m a patient, but you have to tell the doctor what to do for you because they don’t know what they doing. Then, when you ask for, because I take morphine, when you ask for morphine, ‘why do you need this for?’ To get rid of my pain and then I go to the emergency room and sometimes, they don’t even draw my blood to see what is going on with my blood. I’m like, did you draw my blood? ‘Well, why would we draw your blood?’ Because I got sickle cell. You should draw it to see what is going on with my sickle cell. So I don’t like going to the emergency room unless I come here [Sickle Cell Clinic] because they know what they doing over here, but…where I live at, they act like they don’t know. They act like I am a junkie or something because I ask for pain medication, which I don’t feel that is right, because if I go into a pain crisis, you should give me the medication.
Participants delayed going to the hospital when in pain for fear of being judged or stigmatized by healthcare providers. One participant who admitted being a cigarette smoker to a healthcare provider shared a recent encounter with his physician that resulted in his delay in seeking care. Henry stated:
…normally I just try to see if it will pass over by itself. Normally, I just feel like I cause it myself. I feel like since I do cause the pain myself, I need to try to fix it myself and I feel like the doctors are…I don’t know. It’s just I feel like some doctors are judgmental. You know how when you going to the hospital, they always ask you questions like, ‘Well, do you smoke? Do you drink?’ and all that type of stuff and I’m honest about those questions. So I do smoke and I do drink so it kind of makes me feel kind of ashamed, like I’m doing this and I know I do have a serious disease. So that’s another reason [to delay going to the hospital when in pain].
Overall, participants noted the importance of self-care in the management of SCD. Disease management focused on learning one’s body, controlling pain and preventing painful SCD crises. Healthcare is typically sought when clinical assistance is necessary to further manage these crises. Because they often experience difficulties in accessing consistent, quality healthcare, self-care management is the first line of treatment for young adults with SCD.
DISCUSSION
The findings of this research were not previously known as there are no known studies that specifically identify the disease experiences of young adults living with SCD. Moreover, life reviews have only been conducted with middle-age and older adults with SCD (Jenerette et al. 2011, Jenerette & Lauderdale 2008). Even though advances in SCD treatment have decreased pain and prolonged survival, adults with SCD often experience unpredictable, painful crises requiring healthcare visits. Young adults with SCD face additional issues and are at risk for health-related stigmatization due to many challenges of the disease that include managing the chronic illness while accessing and navigating the healthcare system (Jenerette & Brewer 2010). As they transition from a nurturing, family-oriented, pediatric care environment, they must quickly learn how to balance self-care with both daily responsibilities and accessing the healthcare system in a timely, appropriate manner. Young adults with diabetes, another population requiring daily self-care, often experience similar difficulties in balancing self-care with other responsibilities (Pyatak et al. 2014). The interview themes reflect the challenges of this balancing act. The result of imbalance may be reflected in the highest rates of pain crises (Yusuf et al. 2010), hospitalizations and rehospitalizations (Brousseau et al. 2010) in young adults with SCD as well as the high risk of early death after transition from pediatric care (Quinn et al. 2010). Although the self-care strategies of young adults focus on pain management and avoiding the healthcare system, these strategies may in fact lead to poor health outcomes. Because these young adults are delaying care-seeking (Jenerette et al. 2014), they may be more vulnerable when they need to seek care; thus continuing the cycle of stigmatization and lack of satisfaction with treatment.
It is not surprising that most participants discussed self-care activities. This is similar to previous life reviews conducted with middle-aged and older adults with SCD who credit self-care for their longevity (Jenerette et al. 2011) and report learning these self-care activities either from caregivers or simply because they have lived with the disease (Jenerette & Lauderdale 2008). Given that middle–aged and older adults with SCD have lived longer with the lifelong illness, it is understandable that age would have some bearing on attaining, understanding and using self-care resources.
Self-care activities are inherent to living with a chronic illness- especially when the healthcare system often does not meet expectations as evidenced by negative interactions between individuals with SCD and healthcare providers being common (O’Connor et al. 2014). Participants in this study reported being negatively perceived by healthcare providers, experiencing poor pain control and receiving inadequate information about treatment options. This is similar to previous studies where individuals with SCD reported being stigmatized as drug seekers (Jenerette et al. 2014), receiving inadequate pain management (Zempsky 2010) and experiencing insufficient involvement in their care (Lattimer et al. 2010). Individuals with cystic fibrosis (another genetic, chronic disease requiring both chronic and acute care) have a different experience when they access the healthcare system. Adults with cystic fibrosis report that providers offer explanations, answer questions, are courteous and respectful and that they involve patients/family in decisions (Homa et al. 2015). Matthie and colleagues (2014) describe the particular importance of self-care activities for young adults with SCD due to their disproportionate healthcare use compared with other adults with SCD. Because self-care is an important aspect of SCD management, providers need to assess healthcare practices and educate young adults with SCD about other potentially effective self-care strategies.
Participants expressed more about self-care descriptors than accessing the healthcare system; however, the challenges they expressed are reflective of the current state of healthcare for adults with SCD, specifically young adults. Treadwell and colleagues (2011) discuss the systemic issues in transition from pediatric to adult care for young adults with SCD that include limited access to appropriate adult SCD healthcare providers as well as inadequate communication and follow-up between pediatric and adult providers. During transition, young adults with diabetes also report poor provider and health system communication, difficulty navigating the healthcare system and limited providers with disease-specific knowledge (Pyatak et al. 2014). These factors and others result in what Smith and colleagues (2011) describe as a ‘medical abyss’ (p. 297) after leaving pediatric care. This abyss is related to delays in care-seeking for young adults with SCD. The most common reasons young adults with SCD delay care-seeking until their pain is an average of 8.7 (on a scale of 1 to 10) are trying to treat pain at home, avoiding the ED due to past negative experiences and the desire to avoid a hospital admission (Jenerette et al. 2014).
Self-care must be balanced with appropriate and timely care-seeking. Jenerette and Brewer suggest a well-known communication technique (SBAR - situation, background, assessment and recommendation) for individuals such as those with SCD who frequent the ED (Jenerette et al. 2014, Jenerette & Brewer 2011). This technique is a collaborative, communication strategy that provides a structured, easy-to-remember tool. Interventions that focus on skills, such as SBAR, will help young adults navigate the healthcare system and should improve health outcomes included in the Theory of Self-Care Management for Sickle Cell Disease such as stigmatization and satisfaction with care-seeking. Although Jenerette and colleagues have developed and tested a communication skills intervention, there are no other published interventions specifically tailored to address the self-care needs of young adults with SCD. Self-care interventions aimed at helping young adults to achieve similar life satisfactions as their peers and accessing healthcare may prove useful in enhancing health outcomes in young adults with SCD. For example, if an evidence-based exercise training program could be tailored to meet the needs of young adults with SCD, as recommended by Connes and colleagues (2011), it could lead to improved psychosocial and physical health; thus, improving health-related quality of life.
Comparing study findings to previous life reviews with middle-aged and older adults with SCD, there is support for the importance of access to appropriate medical care. Older adults also credit medical care for their longevity (Jenerette et al. 2011, Jenerette & Lauderdale 2008). Because young adults have not had the opportunity (either due to their actions or the availability of providers) to develop ongoing relationships with providers in the adult care system, maintaining healthcare when needs are beyond self-care can be challenging.
Limitations
The data from the study should be considered in the context of a few limitations. First, the number of participants for this study was determined by the size of the attention control group of the larger study and conventional, content analysis was used to review the data. One limitation of conventional, content analysis is that there is no attempt to develop theory or to saturate the categories identified in the data (Hsieh & Shannon 2005). Second, study findings are based on reliance on participants’ self-report of SCD type, the recall of life review events and feelings at the time of those events. Third, all participants were recruited from one comprehensive SCD program. Thus, responses may be reflections limited by experiences related to one center and its resources. Finally, these data were collected before the Patient Protection and Affordable Care Act was fully implemented. This act addresses many barriers to quality care because it creates opportunities for those living with SCD to access affordable health insurance and medical services. Additionally, young adults with SCD can remain on their parents’ insurance until 26 years of age (Akosa Antwi et al. 2015). Although participants still have difficulties in the healthcare system, some barriers have been decreased and/or eliminated. Despite these limitations, the life review, even in young adults, provides a unique opportunity to gather information that may be useful in identifying challenges and potential interventions to assist individuals living with SCD to successfully move through each stage of life.
CONCLUSION
Information obtained from these young adults with SCD requires healthcare providers to take action. Due to the many challenges in the adult healthcare system, pediatric providers need to be vigilant in transitioning individuals with SCD in the best position possible to optimize health outcomes. Transition must include maximizing self-care management resources as expressed in the Theory of Self-Care Management for Sickle Cell Disease. For example, participants noted how important it is to develop and use coping behaviors such as prayer and to participate in self-care activities such as hydration and dressing appropriately. Providers need to use the lessons learned from middle-aged and older adults with SCD to better inform the transition and care of young adults with SCD. It may also be useful to develop mentoring relationships between middle-aged/older adults with SCD who are successfully aging and young adults as they transition to provide social support in addition to knowledge of living with SCD.
Although some young adults are successfully living with SCD, many struggle with the challenges of SCD. Interventions need to be developed to help young adults find balance between self-care strategies and accessing the healthcare system in an appropriate, timely manner. Some self-care skills develop over time as learned behaviors from parents or perhaps as individuals living with SCD learn their bodies. However, skills to navigate the healthcare system such as communicating with healthcare providers need to be developed in a structured way and not during a time of crisis. While transition is improved and interventions are developed, healthcare providers, especially nurses, need to be aware of the challenges of young adults with SCD and advocate on their behalf.
SUMMARY STATEMENT.
Why is this research or review needed?
Perceptions of young adults with sickle cell disease concerning disease management, their quality of life and access to healthcare are limited in the literature.
It is important to understand the challenges experienced and the disease management strategies used by young adults with sickle cell disease to better address their needs and to develop appropriate interventions.
What are the key findings?
Self-management is an important aspect of care for young adults living with sickle cell disease. To manage their disease, participants reported using self-care strategies to enhance health, control symptoms and limit disability.
Participants reported experiencing difficulties getting healthcare needs met. Poor outcomes in young adults with sickle cell disease may be due in part to their lack of skills, resources and desire to access the healthcare system.
Young adults with sickle cell disease strive to achieve the same life satisfactions as individuals not living with the chronic, lifelong disease.
How should the findings be used to influence policy/practice/research/education?
Providers in pediatric care need to be sure that young adults with sickle cell disease are transitioned to adult care with the skills they need to optimize health outcomes.
Understanding the disease experiences of young adults with sickle cell disease is important for developing interventions to help them find balance between self-management and accessing the healthcare system in an appropriate, timely manner.
Acknowledgments
This study was funded by the National Institute of Nursing Research (K23NR011061) to Coretta Jenerette, the National Institute of Nursing Research (T32NR007091) to Nadine Matthie, and the Institute of African American Research Working Group Program at the University of North Carolina at Chapel Hill to all authors.
We thank the individuals with SCD who participated in this study.
Footnotes
Conflict of Interest Statement: No conflict of interest has been declared by the authors.
Author Contributions:
All authors have agreed on the final version and meet at least one of the following criteria (recommended by the ICMJE*):
- substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data;
- drafting the article or revising it critically for important intellectual content.
Contributor Information
Nadine MATTHIE, Email: nmatthie@email.unc.edu.
Jill HAMILTON, Email: jhamil32@jhu.edu.
Diana WELLS, Email: diana_wells@med.unc.edu.
Coretta JENERETTE, Email: coretta.jenerette@unc.edu.
References
- Akosa Antwi Y, Moriya AS, Simon KI. Access to health insurance and the use of inpatient medical care: evidence from the Affordable Care Act young adult mandate. Journal of Health Economics. 2015;39:171–187. doi: 10.1016/j.jhealeco.2014.11.007. [DOI] [PubMed] [Google Scholar]
- Ataga KI. Novel therapies in sickle cell disease. Hematology/the Education Program of the American Society of Hematology. 2009;2009:54–61. doi: 10.1182/asheducation-2009.1.54. [DOI] [PubMed] [Google Scholar]
- Audulv A. The over time development of chronic illness self-management patterns: a longitudinal qualitative study. BMC Public Health. 2013;13:452–466. doi: 10.1186/1471-2458-13-452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ballas SK, Kesen MR, Goldberg MF, Lutty GA, Dampier C, Osunkwo I, Wang WC, Hoppe C, Hagar W, Darbari DS, Malik P. Beyond the definitions of the phenotypic complications of sickle cell disease: an update on management. The Scientific World Journal. 2012;2012:1–55. doi: 10.1100/2012/949535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brousseau DC, Owens PL, Mosso AL, Panepinto JA, Steiner CA. Acute care utilization and rehospitalizations for sickle cell disease. The Journal of the American Medical Association. 2010;303:1288–1294. doi: 10.1001/jama.2010.378. [DOI] [PubMed] [Google Scholar]
- Buchanan G, Vichinsky E, Krishnamurti L, Shenoy S. Severe sickle cell disease--pathophysiology and therapy. Biology of Blood and Marrow Transplantation: Journal of the American Society for Blood and Marrow Transplantation. 2010;16(1 Suppl):S64–7. doi: 10.1016/j.bbmt.2009.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. [2014, November/21];Data & statistics. 2011 Available: http://www.cdc.gov/ncbddd/sicklecell/data.html.
- Cheatham CT, Barksdale DJ, Rodgers SG. Barriers to health care and health-seeking behaviors faced by Black men. Journal of the American Academy of Nurse Practitioners. 2008;20(11):555–562. doi: 10.1111/j.1745-7599.2008.00359.x. [DOI] [PubMed] [Google Scholar]
- Connes P, Machado R, Hue O, Reid H. Exercise limitation, exercise testing and exercise recommendations in sickle cell anemia. Clinical Hemorheology and Microcirculation. 2011;49(2011):151–163. doi: 10.3233/CH-2011-1465. [DOI] [PubMed] [Google Scholar]
- Darbari DS, Ballas SK, Clauw DJ. Thinking beyond sickling to better understand pain in sickle cell disease. European Journal of Haematology. 2014;93(2):89–95. doi: 10.1111/ejh.12340. [DOI] [PubMed] [Google Scholar]
- Genetic Home Reference. [2015, May/5];Sickle cell disease. 2015 Available: http://ghr.nlm.nih.gov/condition/sickle-cell-disease.
- Homa K, Sabadosa KA, Marrow LC, Marshall BC. Experience of care from the perspective of individuals with cystic fibrosis and families: results from 70 CF Foundation accredited programs in the USA. Journal of Cystic Fibrosis: Official Journal of the European Cystic Fibrosis Society. 2015 doi: 10.1016/j.jcf.2014.12.011. [DOI] [PubMed] [Google Scholar]
- Howard J, Oteng-Ntim E. The obstetric management of sickle cell disease. Best Practice & Research. Clinical Obstetrics & Gynaecology. 2012;26(1):25–36. doi: 10.1016/j.bpobgyn.2011.10.001. [DOI] [PubMed] [Google Scholar]
- Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qualitative Health Research. 2005;15(9):1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- Jenerette C, Brewer C. Situation, background, assessment and recommendation (SBAR) may benefit individuals who frequent emergency departments: adults with sickle cell disease. Journal of Emergency Nursing: Official publication of the Emergency Department Nurses Association. 2011;37(6):559–561. doi: 10.1016/j.jen.2011.02.012. [DOI] [PubMed] [Google Scholar]
- Jenerette CM, Brewer C. Health-related stigma in young adults with sickle cell disease. Journal of the National Medical Association. 2010;102(11):1050–1055. doi: 10.1016/s0027-9684(15)30732-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenerette CM, Brewer C, Leak AN. Self-care recommendations of middle-aged and older adults with sickle cell disease. Nursing Research and Practice. 2011;2011:270594. doi: 10.1155/2011/270594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenerette CM, Brewer CA, Ataga KI. Care seeking for pain in young adults with sickle cell disease. Pain Management Nursing: Official Journal of the American Society of Pain Management Nurses. 2014;15(1):324–330. doi: 10.1016/j.pmn.2012.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenerette CM, Brewer CA, Edwards LJ, Mishel MH, Gil KM. An intervention to decrease stigma in young adults with sickle cell disease. Western Journal of Nursing Research. 2014;36(5):599–619. doi: 10.1177/0193945913512724. [DOI] [PubMed] [Google Scholar]
- Jenerette CM, Lauderdale G. Successful aging with sickle cell disease: using qualitative methods to inform theory. Journal of Theory Construction & Testing. 2008;12(1):16–24. [PMC free article] [PubMed] [Google Scholar]
- Jenerette CM, Leak AN, Sandelowski M. Life stories of older adults with sickle cell disease. The ABNF Journal: Official Journal of the Association of Black Nursing Faculty in Higher Education, Inc. 2011;22(3):58–63. [PubMed] [Google Scholar]
- Jordan L, Swerdlow P, Coates TD. Systematic review of transition from adolescent to adult care in patients with sickle cell disease. Journal of Pediatric Hematology/Oncology. 2013;35(3):165–169. doi: 10.1097/MPH.0b013e3182847483. [DOI] [PubMed] [Google Scholar]
- Kauf TL, Coates TD, Huazhi L, Mody-Patel N, Hartzema AG. The cost of health care for children and adults with sickle cell disease. American Journal of Hematology. 2009;84(6):323–327. doi: 10.1002/ajh.21408. [DOI] [PubMed] [Google Scholar]
- Lattimer L, Haywood C, Jr, Lanzkron S, Ratanawongsa N, Bediako SM, Beach MC. Problematic hospital experiences among adult patients with sickle cell disease. Journal of Health Care for the Poor and Underserved. 2010;21(4):1114–1123. doi: 10.1353/hpu.2010.0940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee L, Askew R, Walker J, Stephen J, Robertson-Artwork A. Adults with sickle cell disease: an interdisciplinary approach to home care and self-care management with a case study. Home Healthcare Nurse. 2012;30(3):172–83. doi: 10.1097/NHH.0b013e318246d83d. [DOI] [PubMed] [Google Scholar]
- Lowe P, McBride-Henry K. What factors impact upon the quality of life of elderly women with chronic illnesses: three women’s perspectives. Contemporary Nurse. 2012;41(1):18–27. doi: 10.5172/conu.2012.41.1.18. [DOI] [PubMed] [Google Scholar]
- Matthie N, Jenerette C, McMillan S. Role of self-care in sickle cell disease. Pain Management Nursing: Official Journal of the American Society of Pain Management Nurses. 2014 doi: 10.1016/j.pmn.2014.07.003. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maxwell J. Qualitative research design: An interactive approach. Sage Publications; Thousand Oaks, CA: 2013. [Google Scholar]
- O’Connor S, Hanes D, Lindsey A, Weiss M, Petty L, Overcash J. Attitudes among healthcare providers and patients diagnosed with sickle cell disease. Clinical Journal of Oncology Nursing. 2014;18(6):675–680. doi: 10.1188/14.CJON.675-680. [DOI] [PubMed] [Google Scholar]
- Olowoyeye A, Okwundu CI. Gene therapy for sickle cell disease. The Cochrane Database of Systematic Reviews. 2014;10:CD007652. doi: 10.1002/14651858.CD007652.pub4. [DOI] [PubMed] [Google Scholar]
- Panepinto JA, Bonner M. Health-related quality of life in sickle cell disease: past, present and future. Pediatric Blood & Cancer. 2012;59(2):377–385. doi: 10.1002/pbc.24176. [DOI] [PubMed] [Google Scholar]
- Patton M. Qualitative research & evaluation methods. 3. Sage Publications; Thousand Oaks, CA: 2002. [Google Scholar]
- Pyatak EA, Sequeira PA, Whittemore R, Vigen CP, Peters AL, Weigensberg MJ. Challenges contributing to disrupted transition from paediatric to adult diabetes care in young adults with type 1 diabetes. Diabetic Medicine: A Journal of the British Diabetic Association. 2014;31(12):1615–1624. doi: 10.1111/dme.12485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinn CT, Rogers ZR, McCavit TL, Buchanan GR. Improved survival of children and adolescents with sickle cell disease. Blood. 2010;115(17):3447–3452. doi: 10.1182/blood-2009-07-233700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandelowski M. What’s in a name? Qualitative description revisited. Research in Nursing & Health. 2010;33(1):77–84. doi: 10.1002/nur.20362. [DOI] [PubMed] [Google Scholar]
- Sandelowski M. Member Check. In: Given L, editor. The SAGE Encyclopedia of Qualitative Research Methods. Sage; Thousand Oaks, CA: 2008. pp. 501–502. [Google Scholar]
- Schulman-Green D, Jaser S, Martin F, Alonzo A, Grey M, McCorkle R, Redeker NS, Reynolds N, Whittemore R. Processes of self-management in chronic illness. Journal of Nursing Scholarship: An Official Publication of Sigma Theta Tau International Honor Society of Nursing. 2012;44(2):136–144. doi: 10.1111/j.1547-5069.2012.01444.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith WR, Jordan LB, Hassell KL. Frequently asked questions by hospitalists managing pain in adults with sickle cell disease. Journal of Hospital Medicine. 2011;6(5):297–303. doi: 10.1002/jhm.933. [DOI] [PubMed] [Google Scholar]
- Sobota A, Neufeld EJ, Sprinz P, Heeney MM. Transition from pediatric to adult care for sickle cell disease: results of a survey of pediatric providers. American Journal of Hematology. 2011;86(6):512–515. doi: 10.1002/ajh.22016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanabe P, Porter J, Creary M, Kirkwood E, Miller S, Ahmed-Williams E, Hassell K. A qualitative analysis of best self-management practices: sickle cell disease. Journal of the National Medical Association. 2010;102(11):1033–1041. doi: 10.1016/s0027-9684(15)30730-6. [DOI] [PubMed] [Google Scholar]
- Taylor LE, Stotts NA, Humphreys J, Treadwell MJ, Miaskowski C. A review of the literature on the multiple dimensions of chronic pain in adults with sickle cell disease. Journal of Pain and Symptom Management. 2010;40(3):416–435. doi: 10.1016/j.jpainsymman.2009.12.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Treadwell M, Telfair J, Gibson RW, Johnson S, Osunkwo I. Transition from pediatric to adult care in sickle cell disease: establishing evidence-based practice and directions for research. American Journal of Hematology. 2011;86(1):116–120. doi: 10.1002/ajh.21880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Department of Health and Human Services, Agency for Healthcare Research and Quality. National Healthcare Disparities Report 2011. 2012. [Google Scholar]
- Yusuf HR, Atrash HK, Grosse SD, Parker CS, Grant AM. Emergency department visits made by patients with sickle cell disease: a descriptive study, 1999–2007. American Journal of Preventive Medicine. 2010;38(4 Suppl):S536–41. doi: 10.1016/j.amepre.2010.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zempsky WT. Evaluation and treatment of sickle cell pain in the emergency department: paths to a better future. Clinical Pediatric Emergency Medicine. 2010;11(4):265–273. doi: 10.1016/j.cpem.2010.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]