Abstract
Objectives
Interventions to prevent postpartum common mental disorders (PCMD) among unselected populations of women have had limited success. The aim was to determine whether What Were We Thinking (WWWT) a gender-informed, psychoeducational programme for couples and babies can prevent PCMD among primiparous women 6 months postpartum.
Design
Cluster-randomised controlled trial.
Setting
48 Maternal and Child Health Centres (MCHCs) from 6 Local Government Areas in Melbourne, Australia were allocated randomly to usual care (24) or usual care plus WWWT (24).
Participants
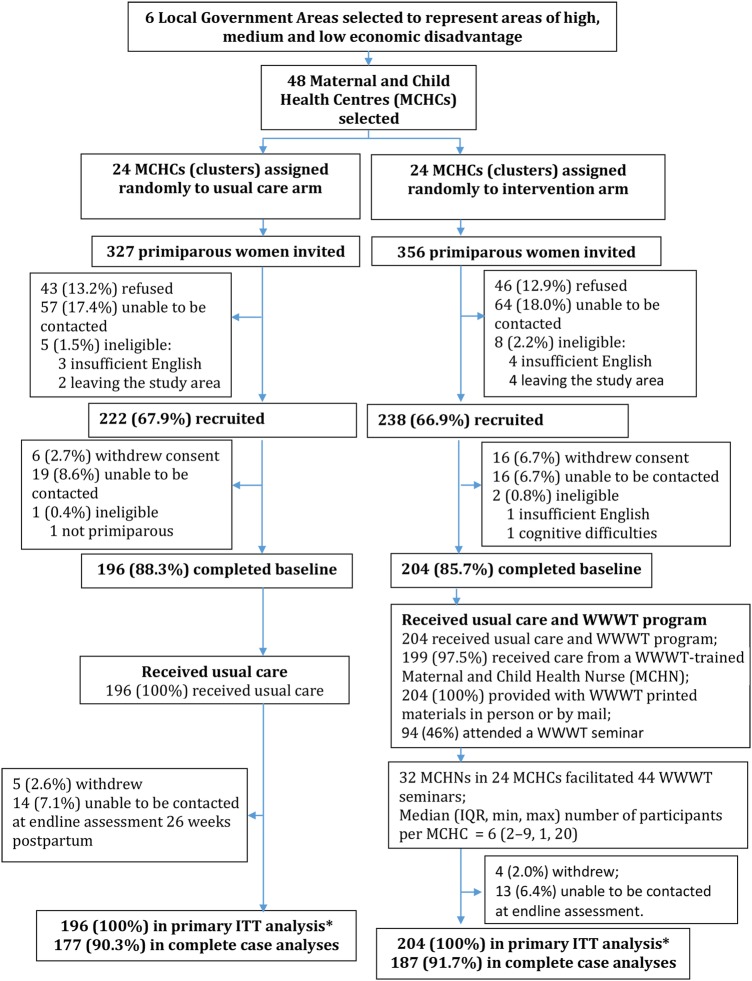
English-speaking primiparous women receiving primary care at trial MCHCs were recruited to the intervention (204) and control (196) conditions. Of these, 187 (91.7%) and 177 (90.3%) provided complete data.
Intervention
WWWT is a manualised programme comprising primary care from a trained nurse, print materials and a face-to-face seminar.
Main outcome measures
Data sources were standardised and study-specific measures collected in blinded computer-assisted telephone interviews at 6 and 26 weeks postpartum. The primary outcome was PCMD assessed by Composite International Diagnostic Interviews and Patient Health Questionnaire (PHQ) Depression and Generalised Anxiety Disorder modules.
Results
In intention-to-treat analyses the adjusted OR (AOR) of PCMD in the intervention compared to the usual care group was 0.78 (95% CI 0.38 to 1.63, ns), but mild to moderate anxiety symptoms (AOR 0.58, 95% CI 0.35 to 0.97) and poor self-rated health (AOR 0.46, 95% CI 0.22 to 0.97) were significantly lower. In a per protocol analysis, comparing the full (three component) intervention and usual care groups, the AOR of PCMD was 0.36, (95% CI 0.14 to 0.95). The WWWT seminar was appraised as salient, comprehensible and useful by >85% participants. No harms were detected.
Conclusions
WWWT is readily integrated into primary care, enables inclusion of fathers and addresses modifiable risks for PCMD directly. The full intervention appears a promising programme for preventing PCMD, optimising family functioning, and as the first component of a stepped approach to mental healthcare.
Trial registration number
ACTRN12613000506796; Results.
Keywords: postnatal common mental disorders, prevention, psychoeducation, father-inclusive, PRIMARY CARE
Strengths and limitations of this study.
This community-based cluster randomised controlled trial was methodologically rigorous in random allocation to trial arms, masking, diagnostic and standardised outcome measures and analysing by intention to treat using imputation to account for all participants.
We achieved a good recruitment fraction of primiparous women <6 weeks postpartum, a very high retention fraction and a sample drawn from across the socioeconomic spectrum.
The approach meets Dennis and Dowswell's central recommendations for prevention of postpartum common mental disorders. It targets fathers and the intimate partner relationship directly, is innovative in including babies, effective across the socioeconomic spectrum and is a straightforward model that can be integrated into routine care.
We did not measure humiliation and entrapment directly and so cannot conclude with certainty that reductions in experiences of these were the psychological process underlying the differences in outcomes between the groups.
The intervention was only accessible to women fluent in English and its impact among women from culturally and linguistically diverse backgrounds is not yet known.
Introduction
Depressive, anxiety and adjustment disorders, which Goldberg and Huxley1 term the common mental disorders, are prevalent among women who have recently given birth. They are associated with disability, reduced participation and compromised caregiving capabilities and can increase risk of adverse developmental outcomes among children.2 There is substantial evidence about the nature, prevalence, correlates of and treatments for postpartum common mental disorders (PCMD).2 However, comprehensive healthcare also requires prevention strategies.3
Diverse indicated (for women with current symptoms), selective (for women at risk of developing symptoms) and universal (for all, unselected, women) interventions to prevent PCMD have been tested in randomised controlled trials (RCTs) among women who have recently given birth.4 Universal interventions for all eligible citizens are preferred, because they are less stigmatising, more likely to be used and even small reductions in population prevalence have a greater public benefit than treating people who are already symptomatic.3 Seven universal interventions offered to unselected populations of individual women who have recently given birth have been trialled: hospital-based debriefing with a psychologist5 or a midwife listening visit,6 earlier-than-usual postnatal general practitioner consultation,7 home visits for practical and emotional care from a trained support worker,8 and an information pack, with or without an invitation to a facilitated group.9 The other two trials tested home-visits from midwives or community nurses trained to identify women's physical and mental health conditions and initiate healthcare.10 11 Of the seven trials, only the midwife-listening visit6 and intensive midwife home-visiting10 were associated with reduced symptoms in the intervention compared to the control group. The midwife-listening study is regarded as a ‘true outlier’ because of apparent selection bias.12 Despite this, a recent Cochrane review, which included indicated and selective as well as universal interventions, rated the methodological quality of these trials as good to excellent.4
We propose several explanations for the lack of impact in most of the trials. The majority only assessed depression or non-specific psychological morbidity.13 No between-group differences in acute stress symptoms were found after psychologist debriefing,5 but lower anxiety symptoms were reported following the midwife-listening intervention.6 It is possible that benefits for other PCMDs, including anxiety and adjustment disorders, might therefore have been undetected. None of the trials reported data about or analysed by prior psychiatric history, so they were unable to detect differences in impact.12 14 Theoretical mechanisms of action were not well described. None of the seven trials specified the risk factor being addressed or whether it was being targeted directly.4
Four major risks for postpartum depression are well recognised15; of these, insufficient social support and quality of intimate partner relationship are more readily modified than psychiatric history and coincidental adverse life events. Most of the interventions appeared to address low social support and did this by providing increased professional care (additional home visits or extra consultations or conversations with a health professional).5 6 8–11 In general the contribution of the intimate partner relationship to postnatal mood among women is not well characterised and none of the trials addressed it. We propose that, after giving birth, women have reduced interactions with workplaces and communities and increased dependence on their intimate partners. An intimate partner relationship characterised by criticism, control and rigid gender-stereotypes about roles and responsibilities can be humiliating. Conversely if the relationship is characterised by empathy, affirmation, encouragement and shared problem-solving, mental health can be protected and promoted.14
While less well recognised, there is growing evidence that dysregulated infant behaviours are associated with postpartum depressive, anxiety and adjustment disorders among their mothers.16–18 Caring well for an infant is sophisticated and technically skilled and few women feel competent when they first become mothers. If infants cry inconsolably, wake after short sleeps or are difficult to feed, women can experience humiliation. Infant crying is intrinsically anxiety arousing and it is common for parents to respond emotionally, using multiple unsustainable techniques to quieten the baby in order to avoid exposure to crying. However, avoidance of crying can lead to increased anxiety among caregivers. Improving infant regulation through using cognitively-focused intentional approaches to the management of infant crying and sleeping difficulties leads to rapid and sustained improvements in maternal psychological functioning.19 These techniques can be used from the earliest weeks of a baby's life with potential to foster more settled infant behaviours and to promote parents’ confidence and reduce anxiety.20
Mothering an infant and managing a household occur in a gendered social context. This occupation is repetitive, isolated, never complete and intrinsically confining, but is not dignified with the language and descriptors of work. Rather, primary caregivers are described as ‘not working’. Health professionals’ routine questions such as ‘Do you work?’ and ‘Does your partner help?’ reflect a public discourse that values paid work and devalues and fails to recognise unpaid work, which is stereotyped as a female responsibility. There is little training in infant care skills, which are presumed to be intuitive to women. Occupational fatigue, well-recognised as a health risk among shift workers, is rarely considered in explaining diminished problem-solving and emotion regulation among mothers of infants.21 None of the seven trials included fathers or infants or addressed gender-based risks.22
What Were We Thinking (WWWT) is a programme that represents a new way of thinking about prevention of PCMD by addressing relevant and potentially modifiable risk factors that have been neglected in previous interventions. We propose that day-to-day interactions among a woman who has recently given birth, her partner and her baby are influential in increasing risk of or protecting against mental health problems and are promising targets for behaviour change. WWWT is based on this reconceptualisation of women's postpartum psychological functioning, Brown and Harris's23 social theory that depression arises in contexts of humiliation and entrapment14 20 and Beck et al's24 theory that anxiety develops as a result of helplessness and lack of agency (see box 1 for a detailed description of theoretical principles, content and structure).
Box 1. The What Were We Thinking (WWWT) Program14 20.
WWWT is a highly structured, gender-informed, interactive psychoeducational programme for couples and their first baby.
Theoretical principles
Improvements in day-to-day interpersonal interactions within families are of fundamental importance to preventing common mental disorders;
Partner and infant behaviours can be modified to decrease those that contribute to psychological distress and increase those that promote confidence and sense of competence;
Women prefer to receive emotional care and practical support within their intimate relationships than increased care from health professionals;
Depressive and anxiety disorders are not easily distinguished and prevention strategies should use a transdiagnostic approach;
Readily-understood, evidence-informed knowledge and opportunities for active learning and skills-development need to be made available at the critical developmental stage at which they are needed;
A psychoeducational approach addresses plausible psychological mechanisms using education to meet salient learning needs;
Language used in the intervention is crucial and needs to challenge gender stereotypes, position mothering and fathering as different but of equal importance, respect the unpaid workload and name and normalise emotions without the use of psychiatric labelling;
Women's experiences of humiliation can be reduced by increasing their partners’ appreciation and empathy, and reducing critical and controlling behaviours;
Experiences of entrapment can be countered by promoting infant care as a shared endeavour in which parents with comparable competence can permit each other independent or shared leisure;
Cognitively-focused rather than emotion-focused responses to infant crying can be promoted by building skills to respond actively and effectively, rather than avoidantly;
Occupational fatigue among parents is minimised by teaching them how to understand and promote adequate infant sleep using evidence-informed behaviour management strategies;
Together these lead to increased confidence and competence, and reduced depression, anxiety and adjustment disorders.
Content and structure
WWWT has an educational framework, comprising structured, easily comprehended learning activities made available at a critical life stage when parenting-specific learning needs are high. It has three interlinked components:
Primary care from a WWWT-trained maternal and child health nurse
Primary care is provided by Maternal and Child Health Nurses who have been trained in programme theory and implementation.
Print materials
Attractively illustrated programme materials in accessible plain language including worksheets for each learning activity and a short book.
Face-to-face seminar offered at 6–8 weeks postpartum
Small group sessions for about five couples and their babies are integrated into a standard primary care programme and offered in a short single day programme on a Saturday to maximise access. The sessions have two sections;
About Babies includes learning activities about infant temperament, crying and fussing, recognition of tired cues, sleep needs, establishing feed-play-sleep routines of daily care and safe, sustainable settling strategies: known collectively as ‘infant behaviour management’.
About Parents includes learning activities about differences between how parenthood had been imagined and is being experienced; recalling the difficult and pleasing aspects of the baby’s birth; recognising, naming and renegotiating the unpaid workload fairly in non-confrontational ways; acknowledging the disenfranchised losses of parenthood as well as the gains; identifying experiences within parents’ families of origin that they wish to duplicate or to relinquish; and identifying gaps in support.
Adult learning strategies including group discussion, focused tasks to be undertaken individually using the print materials and then discussed as a couple; practice in problem solving and negotiation; hands on supported practice in infant wrapping and settling; short talks and practical demonstrations are used.
We have shown in a before-and-after controlled study,20 in which only one component of the WWWT programme was offered (the WWWT seminar facilitated by a specialist nurse), that women without a psychiatric history had significantly reduced 6-month period prevalence of PCMD (AOR 0.43;95% CI 0.21 to 0.89) compared to those receiving usual care, but the full WWWT programme had not been tested in a RCT.
The first aim of this trial was to test whether the population prevalence of PCMD could be reduced when WWWT was implemented in routine primary postpartum care. The second aim was to establish whether the proposed targets for behaviour change: caregiving skills to reduce unsettled infant behaviours and interpersonal skills to renegotiate roles and responsibilities fairly, were linked to the outcome. Some people propose that infant behaviour management strategies carry risks to breastfeeding by encouraging scheduled feeds, rather than giving the baby access to the breast ad libitum, and by settling the baby overnight with patting rather than frequent breastfeeds after the age of 16 weeks.25 It is also argued that these strategies might harm mother–infant relationship by encouraging parents to settle their babies, when tired, in a cot using rhythmic patting rather than in their arms.25 The third aim was to assess whether there was evidence of these harms. We hypothesised that compared to usual care alone, usual care plus WWWT would be associated among primiparous women 6 months postpartum with:
Hypothesis 1.1: Lower 30-day prevalence of Diagnostic and Statistical Manual of Mental Disorders, fourth Edition (DSM IV) diagnoses of depressive, anxiety or adjustment disorders,
Hypothesis 1.2: Better self-rated physical and emotional health;
Hypothesis 2: Lower proportion of infants with unsettled behaviours;
Hypothesis 3: No difference in proportions of breastfed infants;
Hypothesis 4: Similar mother–infant relationship;
Hypothesis 5: Greater satisfaction with the intimate partner relationship.
Methods
Design
To avoid contamination between trial arms, we tested WWWT in a CONSORT-compliant,26 parallel group, prospective, cluster RCT (see trial protocol).27
Setting
The study was implemented in primary maternal and child healthcare (MCH) services in Melbourne, Australia, which are administered in Local Government Areas (LGAs). Nurses qualified in midwifery, and maternal and child health, provide universal, fee-free services from community-based centres (MCHCs). Usual care in these services comprises prescribed sets of child development and health assessments, and parenting information to families with children aged 0–5 years (5 visits in the first 6 months) and facilitated First Time Parents (FTP) Groups (8 sessions in the first year) to foster social connections, and promote caregiving confidence among primiparous women and their partners. Participation in MCH is voluntary and more than 95% of parents with babies attend these local services.28 The 31 Melbourne LGAs were ranked by Socioeconomic Indexes for Areas (SEIFA)29 and allocated to high, medium and low SEIFA tertiles. Two LGAs with at least eight MCHCs providing care to >16 primiparous women annually, which were not current partners in research with this population, and who agreed to random allocation of MCHCs to trial arms, were selected from each tertile. Each LGA signed a research agreement with the administering institution prior to randomisation.
Randomisation and masking
The unit of randomisation was the MCHC. Birth notification lists are provided routinely to LGAs by maternity hospitals and assignment to MCHC is based only on home address. Each LGA identified MCHCs that met inclusion criteria of client volume, and staff assigned exclusively to the centre. In LGAs with >8 eligible MCHCs, an independent statistician selected eight centres randomly. This statistician then generated allocation sequences for each LGA using Stata V.12 random allocation programme, (Stata Statistical Software: Release 12. College Station, Texas, USA: StataCorp LP, 2011) and allocated MCHCs randomly to trial arms in a 1:1 ratio stratified by LGA: 24 MCH Centres per arm. Consistent with CONSORT guidelines26 for cluster RCTs, randomisation of MCHCs (clusters) occurred prior to recruitment of participants. All MCHCs offered usual care. In the intervention arm the seminar, offered within the routine FTPs group programme, and the print materials, were additions to usual care. Apart from the seminar, overall duration of usual care was the same for each group, but it was intended that the training provided to MCH nurses would enhance quality of care in the intervention arm. Outcome assessors were trained graduate research assistants who were not members of the investigator team and were blind to trial arm allocation.
Participants
All primiparous women <6 weeks postpartum, sufficiently literate and fluent in English to comprehend participant information, give consent and complete telephone interviews, and receiving care at selected MCHCs were eligible to participate.
Data sources
Data for primary and secondary outcomes were collected by study-specific questions and standardised psychometric self-report instruments (table 1, adapted from protocol27). Comprehensibility, acceptability and salience of the WWWT seminars were assessed by short, anonymous, post-seminar surveys completed by attendees. Fidelity was assessed in brief post-seminar reviews between facilitators and the project manager and postprogramme semi-structured telephone interviews between facilitators and independent interviewers. Measures were developed and reviewed in collaboration with a community-advisory group, which included primiparous parents.
Table 1.
Data sources and the psychometric properties of standardised measures
| Data source | Assessment point | |
|---|---|---|
| Primary outcome | ||
| Common Mental Disorders in prior 30 days | The Composite International Diagnostic Interview V.3.0 (CIDI)30 Major Depressive Episode, Generalised Anxiety Disorder (GAD), Panic Disorder, Agoraphobia With or Without Panic, Social Phobia and Adult Separation Anxiety Disorder modules. Can be administered by non-clinicians and yields diagnoses meeting the criteria of the Diagnostic and Statistical Manual of Mental Disorders IV (DSM IV).31 | Endline |
| Patient Health Questionnaire modules which are based on DSM IV criteria: | ||
| ▸ PHQ-9 (Depression)32 (9 items): Cronbach’s α ≥0.86 was used to ascertain Adjustment Disorders with Depressed Mood, Anxiety or both Depressed Mood and Anxiety or as baseline values of the outcome for imputation | Baseline and Endline | |
| ▸ PHQ GAD-733: Cronbach’s α=0.92 was used to ascertain Adjustment Disorders with Depressed Mood, Anxiety or both Depressed Mood and Anxiety or as baseline values of the outcome for imputation. | Baseline and Endline | |
| ▸ PHQ panic (5 items) sensitivity and specificity ≥0.82 against clinician diagnosis.34 | Baseline | |
| Secondary outcomes | ||
| Self-rated general health | Single question from the SF-3613 ‘In general, would you say your health is… Excellent/Very good/Good/Fair/Poor’. | Baseline and Endline |
| Modified Fatigue Assessment Scale (FAS) (5 items)35 36 (5 items) a brief self-report measure of physical and cognitive aspects of fatigue: Cronbach's α=0.8836 | Endline | |
| Self-rated symptoms of depression and anxiety in prior 2 weeks | Patient Health Questionnaire modules: | |
| ▸ PHQ-9 (Depression)32 (9 items): Cronbach’s α ≥0.86 | Baseline and Endline | |
| ▸ PHQ GAD-733: Cronbach's α=0.92 | Baseline and Endline | |
| Unsettled infant behaviours | Adapted from the Barr Parental Diary37: how many hours the infant fussed/cried in prior 24 h, problematic crying/fussing ≥3/24 h at 6 weeks (baseline) and ≥2 /24 h at 26 weeks (endline).38 A single question which is an established indicator of day and night time sleep problems39 ‘Over the last 2 weeks, has your baby's sleep generally been a problem for you?’ Y/N. | Baseline and Endline |
| Breastfeeding | Breastmilk, formula or solid foods (Y/N) in prior 24 h.40 | Endline |
| Mother-Infant Relationship | Postnatal Attachment Questionnaire (PAQ)41 (19 items). Yields three subscales and a global score of mother-to-infant attachment: Cronbach's α=0.78.41 | Endline |
| Overall satisfaction with the intimate partner relationship | Single study-specific question: ‘Taking all this into account, how satisfied are you with how things are between you and your partner?’ Likert scale: from Very satisfied (0) to Very dissatisfied (4). | Endline |
| Indicators of behaviour change | ||
| Parenting practices to promote infant sleep | Three modified questions from the ‘Infant Feeding and Sleeping Arrangements’ Questionnaire (IFSAQ)(I St James-Roberts. Infant Feeding and Sleeping Arrangements Questionnaire, Personal communication). | Endline |
| Breastfeeding behaviours | Fixed choice study-specific questions about reasons for ceasing breastfeeding and experiences of mastitis in prior 4 months | Endline |
| Experience of day-to-day interactions with intimate partner | Two perceived partner behaviour factors identified in exploratory factor analysis of 7 study-specific questions. Considerate behaviours: 4 items pertaining to capacity to confide in and solve day-to-day problems with their partner, and satisfaction with the fairness of sharing of household and infant care tasks (weighted score range 0–12, 32.7% variance explained). Emotionally abusive behaviours: 3 items about fear of the partner, and partner criticism of her management of household work and infant care (weighted score range 0–6, further 25% variance explained). Scores calculated for each factor from Varimax rotated component matrix loadings. | Endline |
| Potential effect modifiers | ||
| Participant characteristics | Study-specific fixed-choice questions:27
|
Baseline |
| Personality | Vulnerable Personality Style Questionnaire (VPSQ)43 includes Organised/Responsive subscale (3 items) assessing agency and Vulnerability subscale (6 items) which measures over-sensitivity to the opinions of others and lack of assertiveness: Cronbach's α=0.62, Sensitivity 0.14 and Specificity 0.94. | Baseline |
| Quality of relationship with intimate partner | Intimate Bonds Measure (IBM)44 has two subscales:
|
Baseline |
PHQ, Patient Health Questionnaire; SF-36, Short Form Health Survey; Y/N, yes/no.
Procedures
An LGA officer (who was blind to MCHC trial arm allocation) identified potential participants from birth notification lists and their home address. The LGA officer telephoned potential participants to provide information about the Sleep, Parenting and Relationships in the Community (SPARCS) study, and seek permission to forward contact details to the research team. Women who gave permission were contacted by a research officer, who described the study goals of understanding the health, and health service needs of women with a first baby in order to inform and improve primary care, and participation requirements. The officer sent an explanatory statement and consent form to those willing to join the study. All data were collected in individual computer-assisted telephone interviews at baseline (6 weeks) and endline (26 weeks) postpartum meeting criteria for long-term follow-up.4 These are more convenient to participants than paper-based surveys and minimise attrition and missing data. Contact details were recorded in a dedicated Access database for participant tracking. All other data were entered in a password-protected database under coded identifiers. Retention was optimised by text-message or email reminders for interviews, which were offered in-office and out-of-office hours. Protocols were available for disclosure of suicidal ideas or severe symptoms.
Facilitator training
Training for all maternal and child health nurses (MCHNs) in intervention MCHCs was developed and implemented by JF, HR, KW and the project manager. It comprised a 3 h online active learning module about PCMD, social theories of depression, gender and mental health, and mental health promotion; and one-and-a-half days of face-to-face participatory training addressing gender stereotypes, inclusion of fathers in usual care, evidence-based infant behaviour management, group facilitation skills and the WWWT learning activities. Each MCHN-facilitator was given an infant-sized doll and a muslin wrap to demonstrate settling techniques and a manual with objectives and suggested scripts for each activity. The trial design, including the importance of avoiding talking about WWWT content or sharing materials with colleagues in MCHCs assigned to the control arm were discussed and agreed to.
Implementation of the intervention
Care in intervention MCHCs was provided by a WWWT-trained MCHN. All study participants were given print materials. Invitations to attend a seminar, with their partners and babies as part of the FTP programme, were sent by LGAs to eligible women registered for care at intervention MCHCs. Two MCHN-facilitators ran each seminar for groups of up to five couples with their babies, on a Saturday, in a 6 h session including refreshment breaks.
Parent appraisal of seminars
Immediately after the seminar a brief self-report survey20 was distributed to all women and men who had attended, for anonymous completion. It comprised statements which had been developed in consultation with a project advisory group which had three response options (agree, neutral, disagree), These addressed the usefulness, acceptability, salience and comprehensibility of the content and the print materials, perceptions of the facilitator's skills and knowledge and of the logistics of access to the centre and convenience of the time at which the seminar was offered.
Fidelity
After each seminar delivery, MCHN-facilitators were asked to describe the session in detail, identify activities completed as intended, and problem-solve about any unanticipated difficulties in a short fidelity review with the project manager. Notes were taken and each was discussed at a weekly investigator team meeting, with feedback to the facilitator if required. Six months after the intervention had been completed MCHN-facilitators were invited to have a semi-structured telephone interview about implementation of WWWT practices in usual care with an interviewer who was independent of the research team. They were also asked to appraise delivery quality and parent engagement with the two seminar components on five-point Likert scales from 1=not at all to 5=very well.
Outcomes
Outcomes were assessed at the individual level. The primary outcome was any DSM IV diagnosis of a depressive, anxiety or adjustment disorder in the prior 30 days (PCMD) among women 6 months postpartum. Secondary outcomes were self-rated physical health and fatigue, self-reported depression and anxiety symptoms, unsettled infant behaviours, breastfeeding, mother–infant relationship and satisfaction with intimate partner relationship (table 1).
Data management and statistical analyses
Sample size for the primary outcome, including estimates of intracluster correlation and loss to follow-up, were calculated on our previous study,20 local prevalence data45 and a similar trial in which the clusters were also MCH centres in Victoria.39 To detect a difference between a prevalence of the primary outcome in the control arm of 25% and the intervention arm of 12.5% using logistic regression adjusted for prognostic factors and cluster effects (intracluster correlation of 0.0139), the required sample was 184 per arm (total n=368) (Stata Statistical Software, 2011). Allowing for attrition, 400 (200 per arm) participants were required.
The primary outcome: Diagnostic criteria for PCMD were any DSM IV diagnosis of depressive, anxiety or adjustment disorder in the prior 30 days generated by running standard SAS algorithms on CIDI data, and Patient Health Questionnaire (PHQ) scores. Adjustment Disorder criteria were at least two PHQ-9 or Generalised Anxiety Disorder (GAD)-7 symptoms scored 2 (>50% days) or 3 (nearly every day), any symptom-related functional impairment, onset within 3 months postpartum and no other DSM IV diagnosis. Adjustment Disorder with Depressed Mood required at least one core symptom: sadness or loss of interest (table 1). In order to explore whether there was a difference in the primary outcome between those who received the partial intervention (care from a WWWT-trained MCHN and print materials) or the full intervention (care from a WWWT-trained MCHN, print materials and participation in a face-to-face WWWT seminar) and usual care, we undertook per-protocol analyses on the groups for which we had complete data.
Secondary outcomes: Self-rated physical health was assessed by a standard single question and the Fatigue Assessment Scale. Self-reported symptoms of depression and anxiety in the past 2 weeks were assessed by the PHQ-9 and GAD-7 instruments and calculated both as continuous scores and categorised into three groups using standard criteria: no clinically significant symptoms (≤4), mild symptoms (5–9) and moderate or severe symptoms (10+) groups. Unsettled infant behaviour was a sleep problem in the prior fortnight or the age-appropriate criterion of crying and fussing ≥2 h in the prior 24 h.38 Breastfeeding was any breastmilk in the prior 24 h. All others were scores on standardised measures or responses to single study-specific questions (table 1).
Indicators of behaviour change were assessed in fixed choice questions about parenting practices for management of infant sleeping (I St James-Roberts. Infant Feeding and Sleeping Arrangements Questionnaire, personal communication) quality of day-to-day exchanges between intimate partners and reasons for cessation of breastfeeding (see table 1).
Comparisons between trial arms were calculated as mean differences and 95% CIs using linear regression for continuous, logistic regression for binary and multinomial logistic regression for categorical outcomes. Missing values were imputed using multiple imputation and the imputed data were pooled using Rubin's method. Overall 30 data sets were imputed for each outcome using an imputation model which included baseline characteristics significantly associated with this outcome and missingness as predictors.46
Outcome analyses were adjusted for prognostic factors potentially associated with the outcome: past psychiatric illness, symptoms of depression and anxiety in the early postpartum period (PHQ-9 and GAD-7 baseline scores), unsettled infant behaviours at baseline, quality of relationship with the intimate partner (IBM Care scores at baseline), socioeconomic status (household SEIFA index) and practical and emotional support and coincidental adverse life events at endline. Robust SEs were calculated using the Huber-White Sandwich estimator to account for cluster effects.47 Intraclass correlations for key outcomes were estimated by one-way analysis of variance. All analyses were by full intention to treat at participant level.
Per protocol analyses were undertaken to examine whether there were any differences in impact between receiving the full intervention (seminar, print materials and care from a WWWT-trained MCHN) or the partial intervention (print materials and care from a WWWT-trained MCHN) and usual care. These analyses only included participants for whom complete data were available and were adjusted for the same factors as the other between group analyses.
Ancillary exploratory analyses were undertaken to examine differential effects, and elucidate mechanisms of action. (1) To examine whether there was any impact of the intervention on the prevalence of clinically significant symptoms not meeting diagnostic criteria, a three-category outcome was generated: the first category was women meeting criteria for PCMD, the second was those who had scores ≥5 (cut-off for clinically-significant symptoms) on either PHQ-9 or GAD-7, but did not meet onset, disability or core symptom criteria for Adjustment Disorders, and the third comprised women with no clinically significant symptoms. (2) Comparisons of psychiatric history and baseline PHQ-9 and GAD-7 scores were calculated between these three outcome groups to identify differences in vulnerability.
Given prior evidence that the impact of universal interventions can vary on the basis of participant needs and characteristics, we undertook exploratory analyses for the two targets for the WWWT intervention. (3) Differential effects on infant sleep behaviour and parenting practices to promote infant sleep were examined by fitting an interaction term between trial arm and unsettled infants at baseline (sleep problems in the past fortnight or the age-appropriate criterion of crying and fussing ≥3 h in prior 24 h).48 Differential effects on the quality of day-to-day interactions with the intimate partner were examined by fitting an interaction term between trial arm and suboptimal intimate partner relationships at baseline (IBM Care Subscale scores ≤75th centile and Control Subscale scores ≥25th centile of sample distribution).44 The differential effect analyses used the same models as those used to make all comparisons between trial arms.
Data were analysed using Stata V.12.1 (Stata Statistical Software, 2011, StataCorp LP, Texas, USA).
Results
Recruitment and participation
Overall 683 women consented to contact details being forwarded to the research team, 13 were ineligible because of insufficient English fluency or multiparity, and 67.3% of eligible participants were recruited. Recruitment fractions varied between LGAs (65.0%-71.4%), but not trial arms and retention fraction was 91% (figure 1). All missing data were at outcome and due to participants partially or not completing the endline assessment. Data were missing for 19 women (9.7%) in the control and 17 (9.1%) in the intervention arms. Women whose pregnancy was unintended, who had less education and higher baseline IBM Control scores were less likely to provide complete data. The data were assumed not to be missing completely at random because there were significant differences in some baseline characteristics between those who did and did not provide complete follow-up data. Proportions of missing responses in trial arms were the same. Recruitment started on 10 May 2013 and ceased on 10 April 2014 when the required sample size had been reached; follow-up was completed on 13 August 2014. Participant characteristics at baseline in each of the trial arms are presented in table 2.
Figure 1.
Trial profile. ITT, intention to treat; *Primary outcome analysis imputed missing cases at endline. WWWT, What Were We Thinking; MCHS, Maternal and Child Health Centres.
Table 2.
Baseline characteristics of 400 trial participants
| Control group (N=196) |
Intervention group (N=204) |
|
|---|---|---|
| Sociodemographic | ||
| Age (years) | 32.0 (5.1) | 31.8 (5.2) |
| Born in Australia | 149 (76.0%) | 157 (77.0%) |
| Speak only English at home | 159 (81.1%) | 174 (85.3%) |
| Aboriginal and Torres Strait Islander | 2 (1.0%) | 1 (0.5%) |
| Holds a Health Care card* | 31 (15.8%) | 24 (11.8%) |
| Married/de facto | 185 (94.4%) | 198 (97.1%) |
| Highest education level | ||
| University degree or above | 129 (65.8%) | 120 (58.8%) |
| Postsecondary trade training or certificate | 36 (18.4%) | 41 (20.1%) |
| Up to or complete secondary schooling | 31 (15.8%) | 43 (21.1%) |
| Managerial or professional occupation | 98 (50.0%) | 109 (53.4%) |
| Socio-Economic Index for Area | 1011 (31.8) | 1012 (38.7) |
| Reproductive health | ||
| Prior pregnancy | 56 (28.6%) | 53 (25.0%) |
| Unintended index pregnancy | 49 (25.0%) | 46 (22.6%) |
| Medically assisted conception | 15 (7.7%) | 16 (7.8%) |
| Caesarean birth | 71 (36.2%) | 67 (32.8%) |
| Mental health | ||
| Psychiatric history | ||
| Depression | 27 (13.8%) | 40 (19.6%) |
| Anxiety disorder | 27 (13.8%) | 32 (15.7%) |
| Post-traumatic stress disorder | 7 (3.6%) | 4 (2.0%) |
| Eating or dieting disorder | 3 (1.5%) | 9 (4.4%) |
| Other psychiatric condition including bipolar disorder, alcohol or opiate addiction | 4 (2.0%) | 6 (2.9%) |
| PHQ Depression score | 3.4 (3.3) | 3.9 (3.5) |
| PHQ GAD 7 score | 2.9 (3.1) | 3.6 (3.8) |
| PHQ Panic | 1 (0.5%) | 4 (2.0) |
| Any disability associated with any PHQ symptoms† | 90 (45.9%) | 94 (46.1%) |
| General health and breastfeeding | ||
| Excellent or very good self-rated health | 166 (84.7%) | 169 (82.8%) |
| Ever breastfed | 188 (95.9%) | 197 (96.6%) |
| Current feeding | ||
| Only breast milk | 133 (70.7%) | 134 (68.0%) |
| Only formula | 15 (8.0%) | 22 (11.2%) |
| Both breast milk and formula | 40 (21.3%) | 41 (20.8%) |
| Infant health and infant care | ||
| Gestational age at birth (weeks) | 39.4 (1.6) | 39.5 (1.7) |
| Singleton birth | 194 (99.0%) | 202 (99.0%) |
| Female baby | 99 (50.5%) | 102 (50.0%) |
| Confident about infant care on discharge from maternity hospital | 110 (56.1%) | 103 (50.5%) |
| Baby age at baseline (weeks) | 6.1 (3.3) | 6.2 (3.0) |
| Baby’s health excellent or very good | 183 (93.4%) | 192 (94.1%) |
| Baby's sleep a problem in past 2 weeks | 56 (28.6%) | 55 (27.0%) |
| Duration crying/fussing prior 24 h | 3.2 (2.5) | 2.8 (2.0) |
| Other risk and protective factors for postnatal mental health | ||
| Childhood maltreatment | ||
| Physical abuse | 10 (5.1%) | 19 (9.3%) |
| Sexual abuse | 4 (2.1%) | 4 (2.0%) |
| Vulnerable Personality Scale | ||
| Vulnerability Subscale score | 12.5 (3.9) | 12.1 (4.1) |
| Organised/Responsive Subscale score | 11.7(1.9) | 11.8 (2.0) |
| Intimate Bonds Measure | ||
| Care Subscale score | 33.3 (4.6) | 32.7 (4.7) |
| Control Subscale score | 5.1 (5.2) | 4.6 (4.6) |
Data are n (%), or mean (SD).
*Health Care cards are held by people whose main income is a social protection benefit, who are unwaged students or have a very low household income.
†Only among those with clinically-significant symptoms.
GAD, Generalised Anxiety Disorder; PHQ, Patient Health Questionnaire.
Implementation of the intervention
One MCHN objected to her MCHC's assignment to the intervention arm and refused to participate. Women receiving care here were invited to attend a WWWT seminar in another intervention MCHC in the LGA. Overall 33 MCHNs completed training and 32 implemented the WWWT programme, including facilitating a total of 44 seminars.
The WWWT intervention was offered as part of standard care in intervention MCHCs, so invitations to participate in a seminar were sent by LGAs to all couples with a first baby registered at intervention MCHCs. Overall 262 couples registered their interest in attending a WWWT seminar and, among these, 178 actually attended one. Of the 178 who attended a seminar, 120 women had indicated interest in participating in the research, but 94 actually provided complete baseline data. Among these 94 women, 99% were partnered and seminar attendance lists indicated that 79 (84%) partners attended the seminar. The most common reason given for non-participation in the seminars was because partners had conflicting commitments or were unwilling to attend (figure 1).
All participants who provided baseline data and were registered with intervention MCHCs received the first two WWWT components: primary care from a WWWT-trained MCHN and the print materials.
Fidelity reviews were conducted after 34 (of 44; 77%) seminars; 28 (82%) seminars were delivered as per protocol, but because of time constraints or participant fatigue, up to 3 (of 15) activities were omitted or condensed in 6 (14%) seminars. Post-intervention evaluation interviews were conducted with 21(66%) MCHNs. Mean scores for delivery quality and engagement were: About Babies: 4.6 and 4.4 and About Parents: 3.8 and 3.4. Some MCHNs already taught infant behaviour management skills, but 64% reported changing routine practice to include them and 93% said that since training they included partners, relationship topics and gender-informed language routinely.
Anonymous post-seminar participant surveys indicated that the WWWT content and learning activities were salient, useful and comprehensible (78–99% of women and 71–99% of men agreed with the statements) and that facilitators were knowledgeable. Some found the single-day seminar too long (table 3).
Table 3.
Anonymous post-WWWT seminar participant evaluations (N=303)
| Statement | Women agree* n=167 |
Men agree n=136 |
|---|---|---|
| The facilitator was knowledgeable | 99.4 | 98.5 |
| The facilitator was well prepared | 97.0 | 96.3 |
| The facilitator respected my culture | 95.2 | 95.6 |
| The facilitator understood my needs | 95.8 | 97.1 |
| The session activities were useful | 92.8 | 86.8 |
| The session activities were enjoyable | 88.6 | 89.0 |
| It was useful to learn about our baby's behaviour | 86.8 | 83.8 |
| It was useful to learn how to settle our baby to sleep | 89.8 | 87.5 |
| It was useful to learn how to talk to my partner about parenting | 78.4 | 71.3 |
| It was useful to learn how to share the work with my partner fairly | 82.0 | 71.3 |
| This session would be helpful to all new parents | 95.8 | 91.9 |
| The handouts were easy to read | 98.2 | 95.6 |
| The handouts were easy to understand | 96.4 | 92.6 |
| The programme was at a convenient time | 70.0 | 81.6 |
| The length of the programme was about right | 65.2 | 66.2 |
*Includes women who attended the WWWT seminar as part of the FTP group, but had not agreed to participate in the research.
WWWT, What Were We Thinking; FTP, First Time Parents.
Outcomes
Adjusted endline analyses revealed that there were no significant differences in the primary outcome (DSM IV PCMD) between trial arms. Examination of the secondary outcomes revealed: better self-rated health, but not scores on the fatigue assessment measure; lower prevalence of mild to moderate anxiety symptoms, but no differences in depressive symptoms; no difference in prevalence of unsettled infant behaviours, or overall satisfaction with the intimate partner relationship. There were no between group differences in proportions of infants who were breastfed or quality of mother–infant relationship. There were no between trial arm differences in indicators of behaviour change including parenting practices to promote overnight sleep among infants and considerate and emotionally abusive behaviours in the intimate partner relationship. There were no differences in the adverse breastfeeding outcomes of early breastfeeding cessation or maternal mastitis between groups (table 4).
Table 4.
ORs or mean differences of the outcomes between trial arms
| Control group n (%) or mean (SD) |
Intervention group n (%) or mean (SD) |
ICC | Unadjusted OR or Mean difference (95% CI) |
Adjusted* OR or Mean difference (95% CI) |
Adjusted* OR or Mean difference (95% CI) with imputation of missing data |
|
|---|---|---|---|---|---|---|
| Primary outcome | ||||||
| DSM IV diagnosis of depressive, anxiety, or adjustment disorders prior 30 days | 16 (9.3) | 18 (9.7) | <0.001 | 1.05 (0.52 to 2.15) | 0.83 (0.39 to 1.79) | 0.78 (0.38 to 1.63) |
| Secondary outcomes | ||||||
| Self-rated health | 0.028 | |||||
| Excellent | 29 (16.9) | 36 (19.5) | Ref. | Ref. | Ref. | |
| Very good | 77 (45.0) | 89 (48.1) | 0.93 (0.52 to 1.65) | 0.68 (0.33 to 1.39) | 0.69 (0.34 to 1.39) | |
| Good, fair or poor | 65 (38.1) | 60 (32.4) | 0.74 (0.40 to 1.35) | 0.48 (0.24 to 0.95) | 0.46 (0.22 to 0.97) | |
| PHQ Depression score | 3.26 (3.36) | 3.30 (3.55) | <0.001 | 0.03 (−0.67 to 0.75) | −0.47 (−1.02 to 0.09) | −0.46 (−1.00 to 0.08) |
| PHQ Depression Severity | 0.028 | |||||
| None (score ≤4) | 133 (75.1) | 135 (72.2) | Ref. | Ref. | Ref. | |
| Mild (5–9) | 37 (20.9) | 38 (20.3) | 1.01 (0.60 to 1.68) | 0.87 (0.56 to 1.37) | 0.85 (0.52 to 1.38) | |
| Moderate or severe (10+) | 7 (3.95) | 14 (7.49) | 1.97 (0.77 to 5.03) | 1.48 (0.43 to 5.09) | 1.48 (0.47 to 4.63) | |
| GAD-7 score | 3.35 (3.66) | 3.35 (3.90) | 0.007 | −0.00 (−0.78 to 0.77) | −0.55 (−1.28 to 0.18) | −0.54 (−1.22 to 0.19) |
| GAD severity | <0.001 | |||||
| None (score ≤4) | 125 (70.6) | 136 (72.7) | Ref. | Ref. | Ref. | |
| Mild (5–9) | 43 (24.3) | 36 (19.3) | 0.77 (0.46 to 1.28) | 0.56 (0.33 to 0.94) | 0.57 (0.34 to 0.96) | |
| Moderate or severe (10+) | 9 (5.1) | 15 (8.0) | 1.53 (0.64 to 3.62) | 0.85 (0.28 to 2.51) | 0.77 (0.28 to 2.13) | |
| Fatigue Assessment Scale score | 10.3 (3.7) | 11.0 (3.9) | 0.040 | 0.69 (−0.09 to 1.48) | 0.31 (−0.36 to 0.99) | 0.25 (−0.45 to 0.95) |
| Unsettled infant behaviour | ||||||
| Unsettled infant behaviours | 87 (50.6) | 92 (49.7) | 0.019 | 0.96 (0.63 to 1.46) | 0.90 (0.59 to 1.39) | 0.91 (0.60 to 1.39) |
| Breastfeeding | ||||||
| Any breastmilk in last 24 h | 114 (64.0) | 121 (63.0) | 0.026 | 0.95 (0.62 to 1.46) | 1.14 (0.72 to 1.80) | 1.05 (0.66 to 1.68) |
| Mother-infant relationship | ||||||
| Postnatal Attachment Questionnaire total score | 84.1 (6.8) | 83.6 (6.9) | 0.045 | −0.45 (−1.8 to 0.98) | −0.05 (−1.49 to 1.40) | 0.04 (−1.43 to 1.51) |
| Tolerance and Acceptance subscale | 13.1 (1.7) | 12.9 (1.5) | 0.011 | −0.23 (−0.57 to 0.09) | −0.10 (−0.39 to 0.18) | −0.10 (−0.40 to 0.21) |
| Pleasure in proximity subscale | 8.6 (1.2) | 8.7 (1.2) | 0.010 | 0.12 (−0.14 to 0.38) | 0.14 (−0.14 to 0.44) | 0.14 (−0.16 to 0.45) |
| Competence as parent subscale | 8.5 (0.8) | 8.6 (0.8) | 0.046 | 0.05 (−0.12 to 0.22) | 0.10 (−0.08 to 0.28) | 0.10 (−0.09 to 0.29) |
| Satisfaction with intimate partner relationship | ||||||
| Very satisfied or satisfied with intimate partner relationship (0) vs a bit or very dissatisfied (1) | 11 (6.5) | 15 (8.1) | <0.001 | 1.27 (0.57 to 2.85) | 1.12 (0.48 to 2.62) | 1.13 (0.46 to 2.76) |
| Indicators of behaviour change | ||||||
| Parenting practices to promote infant sleep | ||||||
| Baby usually sleeps in parents’ room but not in parents’ bed OR in separate room (0) vs in parents’ bed (1) | 13 (7.4) | 16 (8.6) | 0.024 | 1.17 (0.55 to 2.51) | 1.00 (0.52 to 1.92) | 0.99 (0.50 to 1.95) |
| In the evening, baby usually falls asleep in cot alone or being patted by an adult until calm (0) vs while being rocked, fed, held or in bed next to parent (1) | 57 (32.4) | 63 (33.7) | 0.043 | 1.06 (0.68 to 1.64) | 0.96 (0.58 to 1.59) | 0.96 (0.59 to 1.56) |
| Use ‘routines’ to help baby to prepare for sleep occasionally/sometimes/most nights (0) vs never (1) | 7 (4.0) | 13 (6.9) | 0.021 | 2.12 (0.76 to 5.49) | 2.07 (0.73 to 5.87) | 2.02 (0.72 to 5.63) |
| Breastfeeding experiences | ||||||
| Ceased breastfeeding because insufficient breastmilk† | 25 (49.0) | 28 (51.9) | 0.007 | 1.12 (0.47 to 2.68) | 1.12 (0.46 to 2.74) | 0.95 (0.44 to 2.04) |
| Mastitis since baseline‡ | 34 (20.2) | 35 (19.4) | 0.001 | 0.95 (0.56 to 1.61) | 0.98 (0.62 to 1.55) | 0.96 (0.60 to 1.56) |
| Quality of day-to-day interactions with the intimate partner | ||||||
| Considerate partner behaviours | 6.5 (1.9) | 6.4 (1.9) | <0.001 | −0.21 (−0.61 to 0.19) | −0.12 (−0.50 to 0.25) | −0.13 (−0.49 to 0.24) |
| Emotionally abusive partner behaviours | 0.41 (0.71) | 0.36 (0.66) | <0.001 | −0.03 (−0.18 to 0.11) | −0.08 (−0.20 to 0.05) | −0.09 (−0.23 to 0.04) |
Bold typeface indicates odds ratios or mean differences that are statistically significant.
*Adjusted for past psychiatric illness, PHQ-9 scores, GAD-7 scores, unsettled infant behaviour, IBM Care scores, and SEIFA index at baseline and practical and emotional support and experience of any adverse life event at endline and for cluster effects.
‡Only assessed in women who had breastfed since baseline.
DSM IV, Diagnostic and Statistical Manual of Mental Disorders, fourth Edition; GAD, Generalised Anxiety Disorder; ICC, intracluster correlation; PHQ, Patient Health Questionnaire; SEIFA, Socioeconomic Indexes for Areas.
Per protocol analyses indicated that there was, however, a significantly lower prevalence of the primary outcome among those who received the full three-component intervention compared to the group who received usual care. Receiving only the partial intervention was not associated with a reduction in the primary outcome (table 5).
Table 5.
Adjusted ORs of the primary outcome between groups receiving the partial or full intervention and usual care*
| Primary outcome | Usual care Control group n (%) |
Received Partial Intervention group n (%) |
Received Full Intervention group n (%) |
Adjusted ORs† (95% CI) between partial intervention (1) vs control (0) | Adjusted ORs† (95% CI) between full intervention (1) vs control (0) |
|---|---|---|---|---|---|
| No diagnoses | 157 (90.7) | 84 (87.5) | 83 (91.6) | Ref. | Ref. |
| DSM IV PCMD prior 30 days | 16 (9.3) | 12 (12.5) | 6 (8.4) | 1.38 (0.58;3.28) | 0.36 (0.14;0.95) |
Bold typeface indicates odds ratios or mean differences that are statistically significant.
*Included only participants for whom complete data were available.
†Adjusted for past psychiatric illness, PHQ-9 scores, GAD-7 scores, unsettled infant behaviour, IBM Care scores, and SEIFA index at baseline and practical and emotional support and experience of any adverse life event at endline and for cluster effects. Partial receipt of the intervention: usual care from a WWWT-trained MCHN and printed materials; Full receipt of the intervention: usual care from a WWWT-trained MCHN, printed materials and attended a WWWT seminar.
DSM IV, Diagnostic and Statistical Manual of Mental Disorders, fourth Edition; GAD, Generalised Anxiety Disorder; MCHN, maternal and child health nurse; PHQ, Patient Health Questionnaire; SEIFA, Socioeconomic Indexes for Areas; WWWT, What Were We Thinking.
The numbers of women meeting diagnostic criteria for a PCMD in the prior 30 days reveal the heterogeneity of these conditions, that anxiety disorders were more common than depressive disorders and the differences among groups at endline (table 6).
Table 6.
DSM IV diagnoses in prior 30 days among trial participants at endline
| Control | Intervention |
|||
|---|---|---|---|---|
| Diagnosis | All participants (N=173) |
All participants (N=185) |
Received partial intervention (N=96) |
Received full intervention (N=89) |
| Any diagnosis | 16 | 18 | 12 | 6 |
| Major depressive disorder only | 1 | 1 | 0 | 1 |
| Generalised anxiety disorder only | 0 | 1 | 1 | 0 |
| Panic disorder with/without agoraphobia only | 2 | 1 | 1 | 0 |
| Social phobia only | 1 | 2 | 1 | 1 |
| Separation anxiety disorder only | 1 | 2 | 1 | 1 |
| Comorbid major depressive and any panic disorder | 1 | 0 | 0 | 0 |
| Comorbid any panic disorder and social phobia | 2 | 1 | 1 | 0 |
| Adjustment disorder with depressed mood only | 1 | 3 | 3 | 0 |
| Adjustment disorder with anxiety only | 5 | 4 | 3 | 1 |
| Adjustment disorder with depressed mood and anxiety | 2 | 3 | 1 | 2 |
DSM IV, Diagnostic and Statistical Manual of Mental Disorders, fourth Edition.
Ancillary exploratory analyses of the whole sample were undertaken to elucidate these findings (table 7). (1) In comparisons made with three outcome categories, there was a significantly lower prevalence of mild-to-moderate symptoms of depression and anxiety in the intervention than the control group. (2) Vulnerability to PCMD is increased among women with a history of mood, anxiety, eating, substance abuse or psychotic disorders or early postpartum symptoms of depression and anxiety. Overall, 44.1% in the PCMD group, 33.0% in the symptomatic group and 17.0% of the asymptomatic group had a personal history of psychiatric disorder (p<0.0001). There was a similar gradient in the baseline mean (SD) PHQ-9 and GAD-7 scores: PCMD group 6.5(5.0) and 5.7(5.0); symptomatic group 4.9(3.3) and 4.6(3.4) and asymptomatic group 2.9(2.8) and 2.4(2.9) (all p<0.001). (3) Babies unsettled at baseline had significantly fewer unsettled behaviours 6 months postpartum in the intervention than the usual care group and their parents were more likely to be adhering to recommendations about safe sleeping place. Although not significant, the AOR suggests that more of those whose babies had been unsettled were adhering to the recommendation about settling the baby to sleep in a cot. Among those whose intimate partner relationship was optimal at baseline, participation in WWWT was associated with significantly fewer emotionally abusive behaviours at endline.
Table 7.
Ancillary exploratory analyses
| Control group n (%) or mean (SD) |
Intervention group n (%) or mean (SD) |
Unadjusted OR or Mean difference (95% CI) |
Adjusted* OR or Mean difference (95% CI) |
Adjusted* OR or Mean difference (95% CI) with imputation of missing data |
|
|---|---|---|---|---|---|
| Primary outcome severity | |||||
| No clinically significant symptoms or diagnoses | 106 (59.9) | 118 (63.1) | Ref. | Ref. | Ref. |
| PHQ-9 or GAD-7 score ≥5, but do not meet all DSM IV criteria for PCMD | 55 (31.1) | 51 (27.3) | 0.83 (0.52 to 1.33) | 0.56 (0.34 to 0.91) | 0.58 (0.35 to 0.97) |
| DSM IV PCMD prior 30 days | 16 (9.0) | 18 (9.6) | 1.01 (0.49 to 2.08) | 0.61 (0.28 to 1.28) | 0.58 (0.27 to 1.21) |
| Differential effects | |||||
| Unsettled infant behaviour | |||||
| Among infants without unsettled behaviours at baseline | 22 (31.9) | 37 (46.8) | 1.88 (0.96 to 3.68) | 1.82 (0.97 to 3.41) | 1.64 (0.87 to 3.10) |
| Among infants with unsettled behaviours at baseline | 65 (63.1) | 55 (51.9) | 0.63 (0.36 to 1.09) | 0.56 (0.35 to 0.88) | 0.58 (0.36 to 0.94) |
| Baby usually sleeps in parents’ room but not in parents’ bed OR in separate room (0) vs in parents’ bed (1) | |||||
| Among infants without unsettled behaviours at baseline | 5 (7.14) | 11 (13.8) | 2.07 (0.68 to 6.29) | 1.79 (0.63 to 5.07) | 1.72 (0.40 to 4.91) |
| Among infants with unsettled behaviours at baseline | 8 (7.55) | 5 (4.7) | 0.60 (0.19 to 1.90) | 0.53 (0.19 to 1.46) | 0.54 (0.19 to 1.52) |
| In the evening, baby usually falls asleep in cot alone or being patted by an adult until calm (0) vs while being rocked, fed, held or in bed next to parent (1) | |||||
| Among infants without unsettled behaviours at baseline | 19 (27.1) | 30 (37.5) | 1.61 (0.80 to 3.22) | 1.43 (0.72 to 2.83) | 1.31 (0.66 to 2.60) |
| Among infants with unsettled behaviours at baseline | 38 (35.9) | 33 (30.8) | 0.80 (0.45 to 1.41) | 0.74 (0.40 to 1.35) | 0.76 (0.41 to 1.38) |
| Use ‘routines’ to help baby to prepare for sleep occasionally sometimes/most nights (0) vs never (1) | |||||
| Among infants without unsettled behaviours at baseline | 3 (4.3) | 6 (7.5) | 1.81 (0.43 to 7.53) | 2.07 (0.52 to 8.20) | 2.11 (0.51 to 8.70) |
| Among infants with unsettled behaviours at baseline | 4 (3.8) | 7 (6.5) | 1.78 (0.51 to 6.29) | 2.06 (0.62 to 6.87) | 1.96 (0.58 to 6.58) |
| Day-to-day interactions in the intimate partner relationship | |||||
| Considerate partner behaviours | |||||
| Among women with optimal intimate partner relationship at baseline | 6.9 (1.5) | 6.8 (1.6) | −0.19 (−0.67 to 0.30) | −0.20 (−0.61 to 0.21) | −0.19 (−0.60 to 0.23) |
| Among women with suboptimal intimate partner relationship at baseline | 5.8 (2.3) | 5.6 (2.2) | −0.13 (−0.77 to 0.51) | −0.02 (−0.75 to 0.79) | −0.02 (−0.76 to 0.72) |
| Emotionally abusive partner behaviours | |||||
| Among women with optimal intimate partner relationship at baseline | 0.29 (0.63) | 0.15 (0.36) | −0.15 (−0.32 to 0.02) | −0.14 (−0.28 to −0.01) | −0.15 (−0.29 to −0.01) |
| Among women with suboptimal intimate partner relationship at baseline | 0.60 (0.81) | 0.71 (0.86) | 0.11 (−0.11 to 0.34) | −0.05 (−0.24 to 0.34) | −0.01 (−0.29 to 0.30) |
Bold typeface indicates odds ratios or mean differences that are statistically significant.
*Adjusted for past psychiatric illness, PHQ-9 scores, GAD-7 scores, unsettled infant behaviour, IBM Care scores, and SEIFA index at baseline and practical and emotional support and experience of any adverse life event at endline and for cluster effects.
DSM IV, Diagnostic and Statistical Manual of Mental Disorders, fourth Edition; GAD, Generalised Anxiety Disorder; PCMD, postpartum common mental disorders; PHQ, Patient Health Questionnaire.
Discussion
Our results demonstrate that WWWT, a novel gender-informed psycho-educational programme implemented by trained generalist MCHNs with unselected primiparous couples within 8 weeks postpartum, was feasible.
Prevention of postpartum mental health problems
There was no difference in the primary outcome of conditions meeting DSM IV criteria for PCMD 6 months postpartum between groups. The prevalence of this outcome was lower than had been estimated and the study might therefore have then underpowered to detect differences between groups. There was, however, promising evidence of WWWT's benefits. Our per protocol analyses indicated that receiving the full intervention (which included the seminar) was effective in reducing PCMD compared to usual care; but the partial intervention was not. This finding should be interpreted with some caution because although all analyses controlled for prognostic factors and clustering, loss of randomisation cannot be controlled for, and it might reflect an undetected participation bias. Among the whole sample, the intervention was associated with significantly lower prevalence of mild to moderate anxiety symptoms and better self-rated health among women 6 months postpartum.
There are debates about the adequacy of a categorical approach to understanding and responding to psychological morbidity. Much prior research categorises people into two groups: those with and without a diagnosable mental disorder or those scoring above or below a clinical cut-off point on a self-report measure. The findings of this study suggest that these binary groupings might be an oversimplification. Our results indicate that more women had clinically significant symptoms that did not meet diagnostic criteria than diagnosable disorders. Using a three-group rather than a binary categorisation, revealed a gradient of vulnerability in terms of prior psychiatric history and baseline levels of symptoms of depression and anxiety, which were significantly higher in the symptomatic group than among those without symptoms. This group therefore occupied a mid-category, which would be missed if outcome assessments were confined to those with mental disorders. When the whole sample was categorised into these three groups, there were significantly lower levels of clinically-relevant mild to moderate symptoms of depression and anxiety among women in the intervention arm than the control arm 6 months postpartum.
Protection of self-reported general health and against fatigue
Self-reported health, an indicator of general well-being including fatigue, was also significantly better among the whole sample of women in the intervention than the control arm, suggesting that occupational fatigue had been modified among them. It is perplexing that this was not reflected in scores on the fatigue-specific measure. One year postpartum, women's self-reported health is associated with infant sleeping problems and fatigue.49 Self-reported health is perhaps a more accurate indicator of WWWT targets than the Fatigue Assessment Scale, which assesses cognitions about motivation and energy.
Reductions in crying and sleeping difficulties among infants
Unsettled behaviour among 6-month-old infants was equally prevalent in trial arms. However, infant behaviour management strategies to reduce crying and promote sleep appear to have been applied by couples in the intervention group whose babies were unsettled early in life, and to have led to more settled behaviours by 6 months of age among them. WWWT content might have been less salient to parents whose babies were settled early in life, but the caregiving skills to manage unsettled behaviours when they emerged had not been acquired. This is similar to the finding of Hiscock et al18 who found that a universal educational intervention to prevent unsettled infant behaviours was effective in reducing daytime sleep and crying problems 6 months postpartum in the subgroup where the infant had been feeding very frequently in the early weeks of life.
Improvements in day-to-day interactions between intimate partners
Most women indicated that they were satisfied with their intimate partner relationship 6 months postpartum and there were no differences between trial arms. There are a number of potential interpretations. It might be that all these relationships were functioning well, and there was no need to change ways of relating to each other. However, at baseline there was variation in the quality of the relationships as indicated by the range of scores on the Care and Control dimensions of the Intimate Bonds Measure (see table 2), which suggests that this is unlikely. It is also possible that this was a psychometric limitation and that a single, fixed-choice, non-validated, study-specific question assessing the global dimension of satisfaction with the relationship was unable to detect variation. The ancillary exploratory analyses revealed that opportunities to learn how to renegotiate roles and responsibilities equitably, and minimise abusive critical or coercive behaviours in interactions with the intimate partner during the transition to parenthood, were applied more successfully by the subgroup of couples whose relationships were functioning optimally in the early postpartum period. It is likely that couples who are less able to affirm and encourage and more likely to criticise and blame at the earliest phase of parenthood will need more than a single session to implement change in these interpersonal interactions.
Harm of infant behaviour management to breastfeeding or mother–infant relationship
There were no differences between trial arms in breastfeeding prevalence, cessation of breastfeeding because of insufficient breastmilk, mastitis or any dimension of the mother–infant relationship, indicating that the approaches to management of unsettled infant behaviour recommended in WWWT were not associated with putative harms.
Strengths and limitations of the trial
This community-based cluster RCT was methodologically rigorous in random allocation to trial arms, masking, diagnostic and standardised outcome measures, analysing by intention to treat using imputation to account for all participants and controlling for factors potentially associated with the outcomes. We achieved a good recruitment fraction50 of primiparous women <6 weeks postpartum, a very high retention fraction and a sample drawn from across the socioeconomic spectrum. The approach meets Dennis and Dowswell's4 central recommendations for PCMD prevention. It targets fathers and the intimate partner relationship directly, is innovative in including babies, effective across the socioeconomic spectrum and is a straightforward model that can be integrated into routine care.
We acknowledge nevertheless, the trial's limitations. We postulated that the mechanisms of action of the intervention were to reduce experiences of humiliation and entrapment and to increase cognitively-focused rather than emotion-focused responses to the adaptive challenges of early parenthood. However, we did not measure these directly and so cannot conclude with certainty that these were the psychological processes underlying the differences in outcomes between the groups. Hypotheses 3 and 4 were framed as null hypotheses, and we acknowledge that the study might not have had sufficient power to detect no differences between groups in breastfeeding or mother–infant relationship. The intervention was only accessible to women fluent in English and its impact among women from culturally and linguistically diverse backgrounds is not yet known. Motivation to adopt WWWT varied among MCHNs. Some MCHNs who managed Centres that were allocated randomly to the intervention arm were philosophically opposed to WWWT components about infant behaviour management or inclusion of men in their services. Implementation in a research context introduced constraints including that MCHNs had to work on a weekend and could not share materials or discuss experiences with colleagues in control MCHCs. While most participated optimally, consistency with programme implementation might have varied. Optimally, assessment of fidelity to the WWWT Facilitator's Guide would have included direct observations, but project resources precluded this. Impact of the trial might have been larger had implementation been flawless. If WWWT were introduced into routine care, it would require comprehensive translation including changes to policy and in-service training, which are likely to contribute to overcoming these barriers.
Implications for universal approaches to prevention of perinatal mental health problems in primary care
Overall the results confirm the findings of our earlier study.20 They suggest that WWWT's novel, gender-informed, structured psycho-educational approach, which addresses a woman's intimate relationships with her partner and baby directly, might modify interactions in the ways we postulated. It is possible that these include by reducing humiliating interactions and increasing those that are affirming and encouraging, and, through promoting fair sharing of unpaid work, limit experiences of occupational fatigue among women. It is also possible that active problem-solving strategies using cognitively-focused rather than emotion-focused responses to unsettled infant behaviours and distribution of household workload can be increased.
Providers are likely to have found it easier to provide the seminar, and routine care, to couples who were interested and motivated to learn, than other couples. It appears from these data that the most powerful component of WWWT is the seminar, but fewer than half the participants received it, most because their partners did not agree to attend. Despite active efforts to invite fathers and make the seminar accessible to them, it remains uncommon in Australia for men to participate in postnatal primary care. Among couples who did attend, fewer men than women found the component about adaptations to changed roles and responsibilities useful. They were perhaps less open to these ideas or willing to act on them, which might have reduced the impact of the intervention. This suggests that the current public health strategy to encourage men to recognise a partner's symptoms and seek treatment could be expanded to make primary care more father-inclusive and raise awareness that changes in men's behaviour might be needed to improve women's mental health.
Learning opportunities are more likely to be used if they address a current need. Rather than suggesting that universal programmes are not of value, these findings indicate that further doses will be required for reinforcement and to address the varied needs and learning capacities within a population. As the first component of a stepped model embedded in the widely used universal primary care system WWWT permits MCHNs to interact with new families and reach those who are more vulnerable or disadvantaged and to reuse components during routine follow-up visits.
The data indicate that WWWT can be integrated into primary care, and has promise when provided as the full intervention as a prevention strategy to reduce population burden of PCMD. It also has benefits for the mid-category of people with mild-to-moderately severe symptoms, which is larger in population terms than the group with diagnosed common mental disorders. The intervention is not harmful. At present the WWWT programme focuses on the adaptive challenges all couples experience as they make the transition from being childless to being parents and so has been designed specifically to meet the learning needs of primiparous women and their partners. The format can be readily adapted for other groups, including parents who already have children or are from culturally and linguistically diverse backgrounds.
The single high quality successful universal PCMD prevention trial, implemented in the British National Health Service,10 involved repeated home visits. Although effective (OR of Edinburgh Postnatal Depression Scale score >13 4 months postpartum was 0.57, 95% CI 0.43 to 0.76), it was resource intensive (mean (SD) of 6 (±1.7) individual home visits, each of about an hour's duration, not including travel time10). The effect of WWWT was of comparable magnitude, for about 1 h additional contact time per couple in the seminar and printed materials. The resource implications of WWWT relative to standard care are being assessed in a cost-effectiveness analysis to provide definitive evidence of programme value.51
This research demonstrates that mental health promotion can be embedded in early parenting education, avoiding explicit psychiatric language and removing stigma, with the additional benefit that parenting skills can be taught directly from the earliest postpartum weeks. We believe that this intervention provides a vehicle for integrating perinatal mental health promotion into community-based primary care services for families and that the findings can be generalised with some confidence to other high-income Anglophone settings. Further research will be required to establish whether these findings can be replicated in future trials; to confirm the theorised mechanisms of action and whether different ways of applying the intervention either in mode of delivery (eg, in smaller components in week-by-week sessions) or in reinforcement sessions would have greater impact among women with different needs and vulnerabilities including past psychiatric disorders. Translational research will be needed to identify strategies, including the use of online resources and social media, to increase programme reach to include a higher proportion of fathers and people from culturally and linguistically diverse groups.
Panel: Research in Context
Evidence before this study
We consulted the Cochrane review of psychosocial and psychological interventions for preventing postnatal common mental disorders (PCMDs) (Dennis and Creedy, 2004; updated by Dennis and Dowswell4 in 2013). Based on the review, we identified seven RCTs of interventions, offered to unselected populations of women who had recently given birth. In only one, a cluster RCT of a resource-intensive intervention embedded in the UK National Health Service: women who received additional home visits from midwives had significantly fewer symptoms of depression at 4 months postpartum. We were unable to find an effective population-based intervention applicable to postnatal primary healthcare in other settings.
We developed What Were We Thinking (WWWT), a gender-informed couples-based psychoeducational intervention that addresses previously neglected modifiable risk factors for postnatal CMD. In a before-and-after-controlled study implemented by specialist nurses, WWWT reduced the prevalence of PCMD (OR=0.43, 95% CI 0.21 to 0.89)20 among primiparous women without a psychiatric history in the first 6 months postpartum.
Added value of this study
In a community-based cluster RCT, we tested WWWT when implemented by trained primary care nurses in local settings. Although there was no overall difference in PCMD between groups, mild to moderate anxiety symptoms were significantly lower and self-rated health was significantly better. In a per protocol analysis WWWT was associated with significantly lower prevalence of PCMDs among women who received the full, three-component intervention compared to usual care.
WWWT's gender-informed, psychoeducational approach, which addresses the relationship between intimate partners and management of unsettled infant behaviours, has promise for PCMD prevention. It was found to be acceptable, salient, useful and comprehensible by participants and is not harmful.
Implications of all the available evidence
This trial provides a considerable advance in the prevention of PCMDs among women in primary healthcare. It is readily integrated into usual care, requires only print materials and about one additional hour of health professional time per couple for a similar benefit to that found in the trial of on average six individual midwife home visits, and is innovative in including fathers and babies. It is applicable to other high-income Anglophone countries with community-based systems of primary postnatal healthcare and can be adapted for low-income settings.
Acknowledgments
The authors are very grateful to Cardinia Shire Council, Frankston City Council, Hobson's Bay City Council, Monash City Council, Moreland City Council and Mornington Peninsula Shire Council for their collaboration in implementing this study; to Ms Joanna Burns and Ms Hau Nguyen for project management and to telephone interviewers Ms Harriet Dwyer, Ms Blathnaid Greene, Ms Cynthia Murray, Ms Debbie Sandler and Ms Carmin Smith and to Mr Eldho Paul, the independent statistician.
Footnotes
Contributors: All authors contributed to the design of the trial, interpretation of results and drafting and approval of the final paper. JF and HR developed the WWWT intervention and supervised all aspects of the study; HR, JF and KW designed the trial and PL, LHA and HH contributed to the selection of measures; KW developed, tested and managed CATIs and the CIDI platform; TT undertook the data analyses and prepared the figure; KW, JF, HR and SR contributed to data analyses; HR and JF developed the training programme and with KW undertook the training of MCHNs; JF, HR, PL, LHA, JP, SR, HH, JB and WC secured the funding and JP facilitated implementation in Local Government Areas.
Funding: This study was funded by competitively awarded grants from the National Health and Medical Research Council (APP1026550), the Australian Government Department of Social Services (formerly Families, Housing, Community Services and Indigenous Affairs) and the Victorian Department of Education and Training (formerly Department of Education and Early Childhood Development). JF is supported by a Monash Professorial Fellowship and the Jean Hailes Professorial Fellowship, which is supported by a grant to the Jean Hailes Foundation from the H and L Hecht Trust managed by Perpetual Trustees. TT is supported by a Monash Bridging Postdoctoral Fellowship. HH is funded by an Australian National Health and Medical Research Council Career Development Award (No. 607351). Murdoch Childrens Research Institute is supported by the Victorian Government's Operational Infrastructure Support Program.
Competing interests: None declared.
Patient consent: Obtained.
Ethics approval: Approval to conduct the study was granted by Southern Health Human Research Ethics (24 April 2013; 11388B) and Monash University Human Research Ethics Committees (30 April 2013; CF12/1022-2012000474).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Goldberg DP, Huxley P. Common mental disorders: a bio-social model. New York: Tavistock / Routledge, 1992. [Google Scholar]
- 2.Howard LM, Molyneaux E, Dennis CL et al. Non-psychotic mental disorders in the perinatal period. Lancet 2014;384:1775–88. 10.1016/S0140-6736(14)61276-9 [DOI] [PubMed] [Google Scholar]
- 3.Mrazek P, Haggerty R. Reducing risks for mental disorders: frontiers for preventive intervention research. Washington DC: National Academy Press, 1994. [PubMed] [Google Scholar]
- 4.Dennis C, Dowswell T. Psychosocial and psychological interventions for preventing postpartum depression (Review). In: The Cochrane Library. Issue 2, 2013.
- 5.Priest SR, Henderson J, Evans SF et al. Stress debriefing after childbirth: a randomised controlled trial. Med J Aust 2003;178:542–5. [DOI] [PubMed] [Google Scholar]
- 6.Lavender T, Walkinshaw SA. Can midwives reduce postpartum psychological morbidity? A randomized trial. Birth 1998;25:215–19. [DOI] [PubMed] [Google Scholar]
- 7.Gunn J, Lumley J, Chondros P et al. Does an early postnatal check-up improve maternal health: results from a randomised trial in Australian general practice. Br J Obstet Gynaecol 1998;105:991–7. 10.1111/j.1471-0528.1998.tb10263.x [DOI] [PubMed] [Google Scholar]
- 8.Morrell C, Spiby H, Stewart P et al. Costs and effectiveness of community postnatal support workers: randomised controlled trial. BMJ 2000;321:593–8. 10.1136/bmj.321.7261.593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Reid M, Glazener C, Murray G et al. A two-centred pragmatic randomised controlled trial of two interventions of postnatal support. BJOG 2002;109:1164–70. 10.1111/j.1471-0528.2002.01306.x [DOI] [PubMed] [Google Scholar]
- 10.MacArthur C, Winter H, Bick D et al. Effects of redesigned community postnatal care on women's health 4 months after birth: a cluster randomised controlled trial. Lancet 2002;359:378–85. 10.1016/S0140-6736(02)07596-7 [DOI] [PubMed] [Google Scholar]
- 11.Lumley J, Watson L, Small R et al. PRISM (Program of Resources, Information and Support for Mothers): a community randomised trial to reduce depression and improve women's physical health six months after birth. BMC Public Health 2006;6:37 10.1186/1471-2458-6-37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lumley J, Austin MP, Mitchell C. Intervening to reduce depression after birth: a systematic review of the randomized trials. Int J Technol Assess Health Care 2004;20:128–44. 10.1017/S0266462304000911 [DOI] [PubMed] [Google Scholar]
- 13.Ware J, Snow K, Kosinski M et al. SF-36® health survey manual and interpretation guide. Boston, MA: New England Medical Center, The Health Institute, 1993. [Google Scholar]
- 14.Rowe HJ, Fisher JR. Development of a universal psycho-educational intervention to prevent common postpartum mental disorders in primiparous women: a multiple method approach. BMC Public Health 2010;10:499 10.1186/1471-2458-10-499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Scottish Intercollegiate Guidelines Network (SIGN). Management of perinatal mood disorders. Edinburgh: SIGN; 2012. http://www.sign.ac.uk
- 16.Martini J, Petzoldt J, Einsle F et al. Risk factors and course patterns of anxiety and depressive disorders during pregnancy and after delivery: a prospective-longitudinal study. J Affect Disord 2015;175:385–95. 10.1016/j.jad.2015.01.012 [DOI] [PubMed] [Google Scholar]
- 17.McMahon C, Barnett B, Kowalenko N et al. Postnatal depression, anxiety and unsettled infant behaviour. Aust N Z J Psychiatry 2001;35:581–8. 10.1080/0004867010060505 [DOI] [PubMed] [Google Scholar]
- 18.Hiscock H, Cook F, Bayer J et al. Preventing early infant sleep and crying problems and postnatal depression: a randomized trial. Pediatrics 2014;133:e346–54. 10.1542/peds.2013-1886 [DOI] [PubMed] [Google Scholar]
- 19.Fisher J, Feekery C, Rowe HJ. Psycho-educational early parenting interventions to promote infant mental health. In: Fitzgerald H, Puura K, Tomlinson M et al., eds International perspectives on child psychology and mental health. Santa Barbara: ABC-CLIO Inc, 2011:205–36. [Google Scholar]
- 20.Fisher JR, Wynter KH, Rowe HJ. Innovative psycho-educational program to prevent common postpartum mental disorders in primiparous women: a before and after controlled study. BMC Public Health 2010;10:432 10.1186/1471-2458-10-432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fisher JRW, Feekery CJ, Rowe-Murray HJ. Nature, severity and correlates of psychological distress in women admitted to a private mother-baby unit. J Paediatr Child Health 2002;38:140–5. 10.1046/j.1440-1754.2002.00723.x [DOI] [PubMed] [Google Scholar]
- 22.Fisher J. The unpaid workload: gender discrimination in conceptualization and its impact on maternal wellbeing. In Section V: gender, social policy and implications for promoting women's mental health. In: Chandra P, Herrman H, Fisher J et al., eds Contemporary topics in women's mental health. Oxford: Wiley Blackwell, 2009:525–37. [Google Scholar]
- 23.Brown GW, Harris T. The social origins of depression. A study of psychiatric disorder in women. London: Tavistock Publications, 1978. [Google Scholar]
- 24.Beck AT, Emery G, Greenberg RL. Anxiety disorders and phobias: a cognitive perspective. New York Basic Books, 1985. [Google Scholar]
- 25.Hiscock H, Fisher J. Sleeping like a baby? Infant sleep: Impact on caregivers and current controversies. J Paediatr Child Health 2015;51:361–4. 10.1111/jpc.12752 [DOI] [PubMed] [Google Scholar]
- 26.Hopewell S, Clarke M, Moher D et al. CONSORT for reporting randomized controlled trials in journal and conference abstracts: explanation and elaboration. PLoS Med 2008;5:e20 10.1371/journal.pmed.0050020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rowe H, Wynter K, Lorgelly P et al. A cluster randomised controlled trial of a brief couple-focused psychoeducational intervention to prevent common postnatal mental disorders among women: study protocol. BMJ Open 2014;4:e006436 10.1136/bmjopen-2014-006436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Victorian Government. Maternal and Child Health Service: Key Ages and Stages Framework. Secondary Maternal and Child Health Service: Key Ages and Stages Framework. http://www.education.vic.gov.au/Documents/childhood/professionals/health/mchkasframework.pdf
- 29.Australian Bureau of Statistics. Socio-Economic Indexes for Areas (SEIFA). Canberra: Australian Bureau of Statistics, 2011. [Google Scholar]
- 30.Kessler RC, Üstün TB. The World Mental Health (WMH) survey initiative version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI). Int J Methods Psychiatr Res 2004;13:93–121. 10.1002/mpr.168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.American Psychiatric Association. DSM-IV-TR. Diagnostic and statistical manual of mental disorders. 4th edn Text revision Arlington, VA: American Psychiatric Association, 2000. [Google Scholar]
- 32.Spitzer RL, Kroenke K, Williams JBW. Validation and utility of a self-report version of PRIME-MD: the PHQ Primary Care Study. JAMA 1999;282:1737–44. 10.1001/jama.282.18.1737 [DOI] [PubMed] [Google Scholar]
- 33.Spitzer RL, Kroenke K, Williams JBW et al. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 2006;166:1092–7. 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- 34.Kroenke K, Spitzer RL, Williams JBW et al. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med 2007;146:317–25. 10.7326/0003-4819-146-5-200703060-00004 [DOI] [PubMed] [Google Scholar]
- 35.Michielsen HJ, De Vries J, Van Heck GL. Psychometric qualities of a brief self-rated fatigue measure: the Fatigue Assessment Scale. J Psychosom Res 2003;54:345–52. 10.1016/S0022-3999(02)00392-6 [DOI] [PubMed] [Google Scholar]
- 36.Giallo R, Wade C, Cooklin A et al. Assessment of maternal fatigue and depression in the postpartum period: support for two separate constructs. J Reprod Infant Psychol 2011;29:69–80. 10.1080/02646838.2010.513050 [DOI] [Google Scholar]
- 37.Barr R, Kramer M, Boisjoly C et al. Parental diary of infant cry and fuss behaviour. Arch Dis Child 1988;63:380–7. 10.1136/adc.63.4.380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Barr RG. The normal crying curve: what do we really know? Dev Med Child Neurol 1990;32:356–62. 10.1111/j.1469-8749.1990.tb16949.x [DOI] [PubMed] [Google Scholar]
- 39.Hiscock H, Bayer J, Gold L et al. Improving infant sleep and maternal mental health: a cluster randomised trial. Arch Dis Child 2007;92:952–8. 10.1136/adc.2006.099812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.World Health Organization. Indicators for assessing breastfeeding practices. Geneva, Switzerland: WHO, 1991. [Google Scholar]
- 41.Condon J, Corkindale C. The assessment of parent-to-infant attachment: development of a self-report questionnaire instrument. J Reprod Infant Psychol 1998;16:57–76. 10.1080/02646839808404558 [DOI] [Google Scholar]
- 42.Australian Bureau of Statistics Catalogue No. 1220.0 Australian and New Zealand Standard Classification of Occupations, Version 1.2. Canberra: Australian Bureau of Statistics, 2013. [Google Scholar]
- 43.Boyce P, Hickey A, Gilchrist J et al. The development of a brief personality scale to measure vulnerability to postnatal depression. Arch Womens Ment Health 2001;3:147–53. 10.1007/s007370170012 [DOI] [Google Scholar]
- 44.Wilhelm K, Parker G. The development of a measure of intimate bonds. Psychol Med 1988;18:225–34. 10.1017/S0033291700002051 [DOI] [PubMed] [Google Scholar]
- 45.Yelland J, Sutherland G, Brown SJ. Postpartum anxiety, depression and social health: findings from a population-based survey of Australian women. BMC Public Health 2010;10:771 10.1186/1471-2458-10-771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rubin DB. Multiple imputation for nonresponse in surveys. New York: Wiley & Sons, 1987. [Google Scholar]
- 47.White H. Maximum likelihood estimation of misspecified models. Econometrica 1982;50:1–25. 10.2307/1912526 [DOI] [Google Scholar]
- 48.Hopkins B. Development of crying in normal infants: method, theory and some speculations. In: Barr G, Hopkins B, Green JA, eds. Crying as a sign, a symptom and a signal. London: MacKeith Press, 2000:176–209. [Google Scholar]
- 49.Schytt E, Waldenström U. Risk factors for poor self-rated health in women at 2 months and 1 year after childbirth. J Womens Health 2007;16:390–405. 10.1089/jwh.2006.0030 [DOI] [PubMed] [Google Scholar]
- 50.Patel MX, Doku V, Tennakoon L. Challenges in recruitment of research participants. Adv Psychiatr Treat 2003;9:229–38. 10.1192/apt.9.3.229 [DOI] [Google Scholar]
- 51.Ride J, Rowe H, Wynter K et al. Protocol for economic evaluation alongside a cluster-randomised controlled trial of a psychoeducational intervention for the primary prevention of postnatal mental health problems in first-time mothers. BMJ Open 2014;4:e006226 10.1136/bmjopen-2014-006226 [DOI] [PMC free article] [PubMed] [Google Scholar]