Abstract
We recently described a novel, non-inherited syndrome of tumor-specific mutations of hypoxia-inducible factor 2α, encoded by EPAS1, leading to formation of multiple paragangliomas and somatostatinomas in the setting of congenital polycythemia. Although we had suspected that somatic mosaicism of EPAS1 mutations was the underlying cause of tumorigenesis, we could not validate this theory in our initial findings. In this report, we developed a sensitive, peptide nucleic acid sequencing assay to uncover the presence of EPAS1 mutations in blood and other somatic tissues of the two patients who were described in the initial characterization of this syndrome. As such, the current study demonstrates that the underlying pathogenesis of the syndrome of multiple paraganglioma and somatostatinoma formation with congenital polycythemia is somatic mosaicism of EPAS1 mutations.
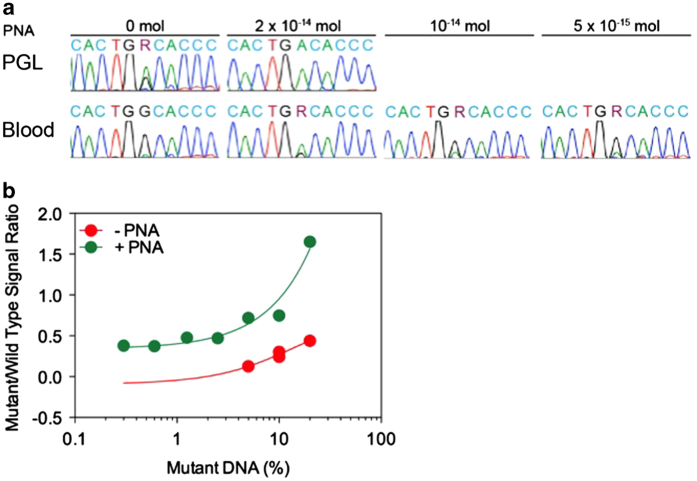
We previously reported a new syndrome, characterized by tumor-specific gain-of-function mutations of hypoxia-inducible factor 2α (encoded by EPAS1), leading to the development of multiple paragangliomas and duodenal somatostatinomas in the setting of congenital secondary polycythemia.1–3 We found that all EPAS1 mutations occurred near the primary hydroxylation site of hypoxia-inducible factor 2α, resulting in augmented EPAS1 transcriptional activity leading to increased erythropoietin (EPO) and polycythemia. We had hypothesized that a somatic EPAS1 mutation may have occurred early in embryogenesis, leading to tissue-restricted somatic mosaicism (such as in neural crest cells) as this mutation was not detected in blood, nail, urine, buccal mucosa or skin DNA. This conclusion of ruling out germ-line mutations was further strengthened by the fact that the EPAS1 mutation was not detected in the parents and other relatives of the affected patients. As such, the presence of EPAS1 mutations in the tissues with mosaicism was postulated to render affected cells susceptible to tumorigenesis and retinal abnormalities,4 leading to simultaneous manifestation of separate and functionally distinct tumors and other manifestations. In a separate study, we did not detect such mutations in normal tissues from four additional patients.2 Furthermore, more recently EPAS1 mutations were found in DNA from blood leukocytes and buccal mucosa in one of two patients affected with paraganglioma, somatostatinoma and polycythemia, suggesting this syndrome may be secondary to somatic mosaicism that has variable tissue distribution.5 We also suspected that at least in some tissues a proportion of EPAS1-mutated non-tumor cells existed but was too minute to be detected by routine Sanger sequencing. To further investigate this possibility, we developed a peptide nucleic acid (PNA, PNA Bio, Thousands Oaks, CA, USA) assay designed to hybridize with the wild-type EPAS1 sequence at codons 528–532 (Supplementary Appendix)—the sites of tumor mutations in our initially reported patients. PNAs have been previously used as an effective PCR clamp to detect somatic mosaicisms of GNAS mutations in blood DNA of patients with McCune–Albright syndrome.6 Using a combined PNA and PCR assay, we detected mutations in the blood DNA of two patients, identical to those in the tumors of the patients we had described in our initial report (Figure 1a and Supplementary Figure S1 in the Supplementary Appendix).1 Additional testing of DNA extracted from hair, nail and saliva from patient 1 revealed the same mutation present in the tumor tissue (Supplementary Figure S2) but not in the same tissues of patient 2. We quantified the degree of heterozygosity present in the blood of our patients through TA cloning, detecting 10 mutants out of 90 clones in patient 1 and 1 mutant out of 72 clones in patient 2. These data suggested that 22.2% of circulating cells in patient 1 and 2.8% of circulating cells in patient 2 harbored EPAS1 mutations, respectively. Using serially titrated combined PNA and PCR assay experiments, we demonstrated that the PNA could detect as low as 2.5% of EPAS1-mutated cells (Figure 1b). Detailed materials and methods may be found in the Supplementary Appendix.
Figure 1.
EPAS1 sequencing of tumor and blood. (a) shows standard Sanger sequencing results, demonstrating a c.G1588A (p.A530T) mutation in DNA derived from paraganglioma (PGL; upper left sequence) but not blood leukocytes (lower left sequence) from patient 1. Addition of 2×10−14 mol peptide nucleic acid (PNA) resulted in amplification of the mutant allele signal in PGL DNA and uncovered the mutation in blood DNA. The mutant allele signal in blood DNA was still detectable using 50% and 75% diluted concentrations of the PNA. (b) illustrates results from serially titrated PCR reactions of TA clone-derived wild type and EPAS1-mutated plasmids with and without the PNA. Addition of the PNA allowed for detection of as low as 1.25% mutant plasmids, correlating with 2.5% mutant cells.
The data presented in this report demonstrate that the syndrome of paraganglioma and somatostatinoma associated with polycythemia occurs secondary to somatic mosaicism of EPAS1 mutations, affecting cells in different tissues. Although we initially hypothesized that polycythemia predominantly occurred secondary to increased erythropoietin (EPO) production by EPAS1-mutated tumor cells, we now acknowledge that it is more likely either EPAS1-mutated mosaic non-tumor neural crest cells in the adrenal medulla, gastrointestinal tract or other tissues (a non-EPO producing tissue type) or EPAS1-mutated mosaic cells in tissues naturally producing EPO are responsible for polycythemia, especially before tumors develop. However, we currently cannot directly test this hypothesis because of lack of access to normal adrenal, renal and hepatic tissues. Given our two patients developed polycythemia shortly after birth, long before their tumor diagnoses, it is also plausible to suspect that EPAS1 mutations may have involved hematopoietic precursor cells. Further testing of bone marrow-derived hematopoietic stem cells may answer this question.
In summary, we have demonstrated the presence of somatic mosaicism of EPAS1 mutation-bearing cells in our initially described syndromic patients. We propose that EPAS1 mutations occur early in embryogenesis, affecting hematopoietic and other tissue precursors and giving rise to early onset polycythemia, as well as affecting neuroendocrine cells, thus predisposing patients to paraganglioma and somatostatinoma formation later in life. Importantly, somatic mosaicism of EPAS1 mutations should be considered in patients presenting with congenital polycythemia for whom conventional testing cannot detect EPAS1 mutations. Application of the PNA assay described in this correspondence may be of clinical utility for detecting EPAS1 mutations in these patients. In addition, further work may uncover EPAS1 mutations in other tissues of affected patients, potentially predisposing to additional tumor types.
Acknowledgments
This study was funded by the Intramural Research Program of the National Institutes of Health (Bethesda, MD, USA).
Footnotes
Supplementary Information for this article can be found on the Human Genome Variation website (http://www.nature.com/hgv).
The authors declare no conflict of interest.
References
- Zhuang Z , Yang C , Lorenzo F , Merino M , Fojo T , Kebebew E et al. Somatic HIF2A gain-of-function mutations in paraganglioma with polycythemia. N Engl J Med 2012; 367: 922–930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacak K , Jochmanova I , Prodanov T , Yang C , Merino MJ , Fojo T et al. New syndrome of paraganglioma and somatostatinoma associated with polycythemia. J Clin Oncol 2013; 31: 1690–1698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang C , Sun MG , Matro J , Huynh TT , Rahimpour S , Prchal JT et al. Novel HIF2A mutations disrupt oxygen sensing, leading to polycythemia, paragangliomas, and somatostatinomas. Blood 2013; 121: 2563–2566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacak K , Chew EY , Pappo AS , Yang C , Lorenzo FR , Wilson MW et al. Ocular manifestations of hypoxia-inducible factor-2alpha paraganglioma-somatostatinoma-polycythemia syndrome. Ophthalmology 2014; 121: 2291–2293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buffet A , Smati S , Mansuy L , Menara M , Lebras M , Heymann MF et al. Mosaicism in HIF2A-related polycythemia-paraganglioma syndrome. J Clin Endocrinol Metab 2014; 99: E369–E373. [DOI] [PubMed] [Google Scholar]
- Lietman SA , Ding C , Levine MA . A highly sensitive polymerase chain reaction method detects activating mutations of the GNAS gene in peripheral blood cells in McCune-Albright syndrome or isolated fibrous dysplasia. J Bone Joint Surg Am 2005; 87: 2489–2494. [DOI] [PubMed] [Google Scholar]
Data Citations
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.