Abstract
Context:
The surgical management of fistula-in-ano is still debatable and no clear recommendations have been made available until now. The present study analyses the results of ligation of intersphincteric fistula tract (LIFT) technique in treating fistula-in-ano in particular with recurrence, healing time, and continence status.
Aims:
LIFT in the management of patients of fistula-in-ano of cryptoglandular origin.
Settings and Design:
Prospective study.
Materials and Methods:
This is a prospective study of 52 patients admitted from September 2012 to August 2014. Patients were managed with LIFT technique and results of LIFT technique were compared with other studies in terms of recurrence rate, incontinence rate, and other postoperative complications.
Results:
A total of 52 patients were studied. Median follow-up was 24 weeks. Primary healing was achieved in 32 (71.11%) patients. Thirteen patients (28.88%) had a recurrence. No patient reported any subjective decrease incontinence after the procedure.
Conclusions:
LIFT technique is simple and easy to learn. With this method fistula-in-ano could be easily treated even at primary health care level. LIFT technique is a simple and novel modified approach for the treatment of fistula-in-ano with rapid healing rate and without any resultant incontinence.
KEYWORDS: Crypto glandular infection, fistula-in-ano, ligation of intersphincteric fistula tract, sphincter saving operation
INTRODUCTION
Fistula-in-ano is a chronic phase of anorectal infection and is characterized by chronic purulent discharge or cyclical pain associated with the abscess reaccumulation followed by intermittent spontaneous decompression.[1] Surgery remains the only modality for the effective treatment of this condition. The main objective of the operative intervention is to heal the fistula with minimal morbidity.[2] There are a number of sphincter-sparing methods such as fibrin or cyanoacrylate glue injection,[3,4] anal fistula plug,[5] endorectal advancement flap,[6,7] ayurvedic seton,[8] ligation of intersphincteric Fistula tract (LIFT),[9,10] and finally, video-assisted anal fistula treatment.[11] Several sphincter-sparing methods carry their own risk of recurrence and some degree of incontinence. Most of these are complicated and difficult procedures, and require expertise, highly experienced surgeons, or high-technology equipment.[12] LIFT technique is the novel modified approach through the intersphincteric plane for the treatment of fistula-in-ano, known as LIFT procedure. LIFT procedure is based on the secure closure of the internal opening and removal of infected cryptoglandular tissue through the intersphincteric approach.[9,10] This procedure is simple, safe, and minimally invasive. It is also effective, with a high and rapid healing rate without any resultant incontinence.[12] This technique result in faster healing of Fistula-in-ano, and does not divide the anal sphincters and postoperative anal function remain intact.
MATERIALS AND METHODS
This is a prospective study of 52 patients suffering from fistula-in-ano admitted to our Surgery Department during the period of 2 years (September 2012–August 2014). All the patients aged above 18 years with fistula-in-ano of cryptoglandular origin were included in the study and procedures followed were in accordance with the standards of the ethical committee. Patients with complex fistula-in-ano, preoperative incontinence, lost to follow-up, inflammatory bowel disease, tuberculosis, and anorectal tumor were excluded from the study. At the time of admission, a detailed history and the clinical examination were carried out. All the patients were subjected to digital rectal examination, proctoscopy, fistulogram, and transrectal ultrasound. In some selected patients, magnetic resonance imaging was also done. Then every patient with fistula-in-ano was evaluated for associated inflammatory bowel disease, tuberculosis (excluded by X-ray chest), anorectal tumor, HIV, etc. In this study, all the patients having fistula-in-ano were identified and investigations were done to identify the primary fistula tract [Figure 1]. The preoperative rectal enema was carried out the night before surgery. Then all the patients were operated by LIFT technique. The procedures were performed in lithotomy position, under spinal anesthesia. The steps of the procedure are as follows; the location of the internal opening was identified by injection of methylene blue and hydrogen peroxide through the external opening and gently probing the fistula tract. The intersphincteric plane at the site of the fistulous tract was entered via the curvilinear incision. The intersphincteric tract was identified by meticulous dissection, using scissors and electrical cautery [Figure 2]. The exposure of the intersphincteric plane was facilitated using especially designed long and narrow blade retractors. The intersphincteric tract was hooked using a small right-angled clamp. The tract was then ligated close to the internal sphincter with polyglactin-910 size 2/0. After that, the tract was divided distal to the point of ligation. The remnant of the intersphincteric tract or possibly the infected gland was removed. The fistulous tract would then be thoroughly curetted. The external opening was left open for drainage. After the operation, no restriction of diet was required. The patients were advised to self-care their wounds by cleansing with tap water and betadine solution. All the patients were treated with postoperative intravenous antibiotics for 5 days, sitz bath from the first postoperative day, an analgesic for pain relief and stool bulking agents were given.
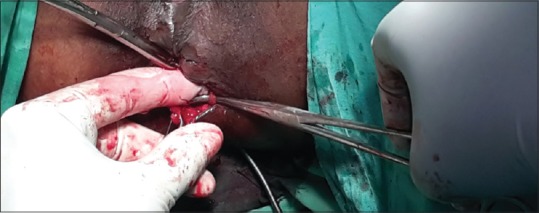
Figure 1.

Preoperative photo of fistula-in-ano
Figure 2.
Intraoperative photo showing fistula tract
All the patients were followed up for a median period of 24 weeks and clinically assessed for incontinence as per Park's classification for incontinence.[13] Patients were also followed up for detection of persistence or recurrence of local sepsis. All the patients were scheduled for follow-up at 2, 4, 8, and 12 weeks postoperatively, and at 4-weekly intervals thereafter up to 24 weeks [Figure 3]. At each visit, the patient's clinical continence status was evaluated, and incontinence rates were recorded. All the results were analyzed and tabulated according to age, sex, different surgical procedures, and their complications.
Figure 3.

Postoperative photo showing healed fistula-in-ano
RESULTS
Totally 52 patients were admitted with Fistula-in-ano in our Department of General Surgery in the period of September 2012–August 2014. After proper investigation, seven patients were excluded from the study. Of 7 patients, 4 patients were found to have tuberculosis one patients had Crohn's disease. In two patients, there was a loss to follow-up. Hence, total 45 patients were included in the study. Primary healing was achieved in 32 (71.11%) patients. Maximum or peak incidence of fistula-in-ano was in the age group 41–50 years. The median age was 46 (range 29–65) years. The oldest patient was a male of 65 years and the youngest patient was female of 29 years. The male to female ratio was 4:1. According to the anatomic level, fistula-in-ano into the high and low level of fistula is found to be 57.77% and 42.22%, respectively. In this study, the most common presenting symptom with patients having a fistula-in-ano was discharge (100%) from the tract, followed by occasional pain (13.33%) and rarely bleeding (4.44%) from the tract was seen. Transsphincteric tract (42.22%) was found in 19 patients. Intersphincteric fistula tract (46.66%) was found in 21 patients. Hence, they are almost same in the incidence, but suprasphincteric tract (11.11%) was found only in five patients. Recurrence was seen in all five patients having suprasphincteric (5 out of 13 recurrences: 38.46%) fistula-in-ano. While seven patients having transsphincteric fistula-in-ano (7 out of 13 recurrences: 53.84%) had a recurrence. Only one patient having an intersphincteric fistula (1 out of 13 recurrences 7.69%) had a recurrence. No patient reported any subjective decrease incontinence after the procedure.
DISCUSSION
LIFT procedure was first proposed by Rojansakul in 2007 in 18 patients with a success rate of 94%.[9] Primary healing occurred in all the patients in less than 3 weeks. There was no change incontinence status with no major postoperative complications.[10] Shanwani et al. applied the same technique on 45 patients with success rate of 77% with a median follow-up of 9 months (range, 2–16), with a median healing time of 7 weeks (range, 4–10). Recurrence occurred in eight patients over a period of 3–8 months, with no significant morbidity.[14]
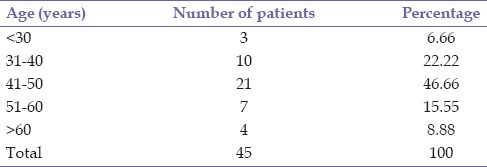
In this study, totally 52 patients were included. Of which seven patients were excluded [Table 1]. Four patients had tuberculosis and a patient with Crohn's disease. Here more people are in a low socioeconomic group and tuberculosis and Crohn's disease are commonly associated as shown by the previous studies.[15,16] Two patients were excluded from the study as they lost follow-up. Hence, total 45 patients were included in the study. Thirty-six patients were male and 9 patients were female with male to female ratio is 4:1 which is similar to the study done previously.[10] According to the previous study, the average age of presentation of fistula-in-ano is 40.78 ± 11.84 years (range: 21–71 years).[12] However, in our study, the incidence of fistula-in-ano was maximum in the age group 41–50 years [Table 2] and the minimum incidence was in the age group <30 years. The oldest patient was a male of 65 years and the youngest patient was female 29 years.
Table 1.
Distribution of excluded patients of fistula-in-ano
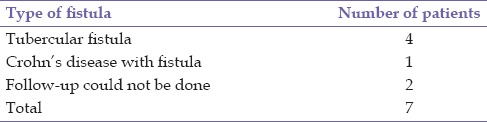
Table 2.
Age distribution of study population
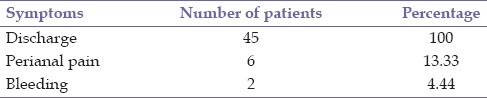
According to the Park's classification the most common fistula-in-ano is intersphincteric (45%) followed by transsphincteric (30%) and suprasphincteric (30%).[17] However, in this study, the most common primary fistula tract is intersphincteric (46.66%) [Table 3] which is nearly same as that of park's classification, followed by transsphincteric (42.22%) which is higher as mentioned in parks classification, but in this study suprasphincteric fistula is less that is, (11.11%) as compared to Park's classification. The most common presentation of fistula-in-ano patients was discharge [Table 4] from the tract which is seen in all cases. In some patients, occasional perianal pain (13.33%) and rarely bleeding (4.44%) from the tract may be seen which is similar to studies done previously.[18]
Table 3.
Distribution of primary fistula tracts among patients of fistula-in-ano
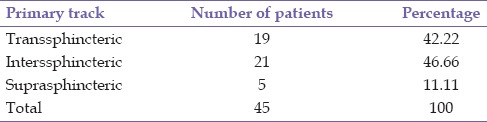
Table 4.
Distribution of symptoms among patients of fistula-in-ano
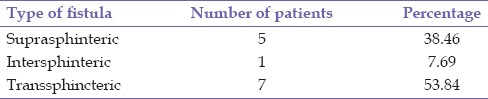
According to the anatomic level, fistula-in-ano can be divided into low and a high level of fistula. In this study, high level of fistula-in-ano [Table 5] was found in (57.77%) while a low level of fistula-in-ano was seen in (42.22%). However, the ratio was 50:50 in other studies, this differences may be attributed to variation in a geographical area.[18] According to the study done by Shanwani et al. primary healing rate was 82%, with a median healing time of 7 weeks (range, 4–10) with recurrence seen in 8 patients over a period of 3–8 months, with no significant morbidity.[14] However, in this study, primary healing was seen in 32 patients (71.11%) with an average healing time of 4 weeks and recurrences in 13 patients (28.88%) over a period of 1–6 months, with no significant morbidity. In this study, one thing which is to be noted is that in none of the patients clinical incontinence was reported. All the five patients with recurrence [Table 6] occurred with high suprasphincteric fistula as the tracts were ligated-below the internal openings. Other eight patients had a recurrence with high transsphinteric fistula. Of which five patients were obese. Failure to identify fistula tract occurred more often in an obese patient which suggest that obesity might be a factor for treatment failure.[19] Recurrence of an anal fistula may be due to infection and technical errors. Infection was one of the reasons for nonhealing of internal opening wounds because it caused the breakdown of the closure wound on the internal sphincter. There were eight patients having a technical error in the identification of fistula tract caused by incorrect ligation of the true fistula tract. The reason for the difficulty in identifying the fistula tract could have been patient's obesity. In this study, 5 out of 8 transsphincteric patients were obese. In other 3 patients, who were not obese the cause of recurrence might be due to technical error in the identification of fistula tract or may be due to thinness or small size of the fistula tract or a deep-seated fistula tract.
Table 5.
Types of fistula according to anatomical level
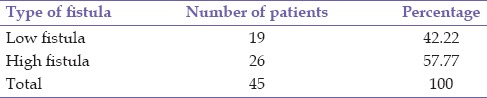
Table 6.
Incidence of recurrence in fistula-in-ano
CONCLUSION
The LIFT procedure is relatively easy to learn and perform; with no high-technology equipment required has a high healing rate and appears to be safe with low morbidity with this method fistula-in-ano could be easily treated even at primary health care level. Finally, the greatest advantage of this procedure is that there is no chance of incontinence as the infective focus is removed without dividing any part of the anal sphincter complex.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Whiteford MH, Kilkenny J, 3rd, Hyman N, Buie WD, Cohen J, Orsay C, et al. Practice parameters for the treatment of perianal abscess and fistula-in-ano (revised) Dis Colon Rectum. 2005;48:1337–42. doi: 10.1007/s10350-005-0055-3. [DOI] [PubMed] [Google Scholar]
- 2.Abbas MA, Jackson CH, Haigh PI. Predictors of outcome for anal fistula surgery FREE. Arch Surg. 2011;146:1011–6. doi: 10.1001/archsurg.2011.197. [DOI] [PubMed] [Google Scholar]
- 3.de la Portilla F, Rada R, León E, Cisneros N, Maldonado VH, Espinosa E. Evaluation of the use of BioGlue in the treatment of high anal fistulas: Preliminary results of a pilot study. Dis Colon Rectum. 2007;50:218–22. doi: 10.1007/s10350-006-0799-4. [DOI] [PubMed] [Google Scholar]
- 4.Barillari P, Basso L, Larcinese A, Gozzo P, Indinnimeo M. Cyanoacrylate glue in the treatment of ano-rectal fistulas. Int J Colorectal Dis. 2006;21:791–4. doi: 10.1007/s00384-006-0090-0. [DOI] [PubMed] [Google Scholar]
- 5.Han JG, Wang ZJ, Zhao BC, Zheng Y, Zhao B, Yi BQ, et al. Long-term outcomes of human acellular dermal matrix plug in closure of complex anal fistulas with a single tract. Dis Colon Rectum. 2011;54:1412–8. doi: 10.1097/DCR.0b013e31822c5398. [DOI] [PubMed] [Google Scholar]
- 6.Abbas MA, Lemus-Rangel R, Hamadani A. Long-term outcome of endorectal advancement flap for complex anorectal fistulae. Am Surg. 2008;74:921–4. [PubMed] [Google Scholar]
- 7.Jarrar A, Church J. Advancement flap repair: A good option for complex anorectal fistulas. Dis Colon Rectum. 2011;54:1537–41. doi: 10.1097/DCR.0b013e31822d7ddd. [DOI] [PubMed] [Google Scholar]
- 8.Ho KS, Tsang C, Seow-Choen F, Ho YH, Tang CL, Heah SM, et al. Prospective randomised trial comparing ayurvedic cutting seton and fistulotomy for low fistula-in-ano. Tech Coloproctol. 2001;5:137–41. doi: 10.1007/s101510100015. [DOI] [PubMed] [Google Scholar]
- 9.Rojanasakul A. LIFT procedure: A simplified technique for fistula-in-ano. Tech Coloproctol. 2009;13:237–40. doi: 10.1007/s10151-009-0522-2. [DOI] [PubMed] [Google Scholar]
- 10.Rojanasakul A, Pattanaarun J, Sahakitrungruang C, Tantiphlachiva K. Total anal sphincter saving technique for fistula-in-ano; the ligation of intersphincteric fistula tract. J Med Assoc Thai. 2007;90:581–6. [PubMed] [Google Scholar]
- 11.Meinero P, Mori L. Video-assisted anal fistula treatment (VAAFT): A novel sphincter-saving procedure for treating complex anal fistulas. Tech Coloproctol. 2011;15:417–22. doi: 10.1007/s10151-011-0769-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sirikurnpiboon S, Awapittaya B, Jivapaisarnpong P. Ligation of intersphincteric fistula tract and its modification: Results from treatment of complex fistula. World J Gastrointest Surg. 2013;5:123–8. doi: 10.4240/wjgs.v5.i4.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Parks AG. Anorectal incontinence. J R Soc Med. 1975;68:21–30. [PMC free article] [PubMed] [Google Scholar]
- 14.Shanwani A, Nor AM, Amri N. Ligation of the intersphincteric fistula tract (LIFT): A sphincter-saving technique for fistula-in-ano. Dis Colon Rectum. 2010;53:39–42. doi: 10.1007/DCR.0b013e3181c160c4. [DOI] [PubMed] [Google Scholar]
- 15.Fansler WA. The relationship of tuberculosis to fistula in ano. J Am Med Assoc. 1925;85:671–4. [Google Scholar]
- 16.Williams JG, Rothenberger DA, Nemer FD, Goldberg SM. Fistula-in-ano in Crohn's disease. Results of aggressive surgical treatment. Dis Colon Rectum. 1991;34:378–84. doi: 10.1007/BF02053687. [DOI] [PubMed] [Google Scholar]
- 17.Parks AG, Gordon PH, Hardcastle JD. A classification of fistula-in-ano. Br J Surg. 1976;63:1–12. doi: 10.1002/bjs.1800630102. [DOI] [PubMed] [Google Scholar]
- 18.Makhlouf G, Korany M. Lift technique for fistula-in-ano. Egypt J Surg. 2013;32:32–6. [Google Scholar]
- 19.Schwandner O. Obesity is a negative predictor of success after surgery for complex anal fistula. BMC Gastroenterol. 2011;11:61. doi: 10.1186/1471-230X-11-61. [DOI] [PMC free article] [PubMed] [Google Scholar]


