Sir,
We would like to describe an unusual case of unilateral macular coloboma alongside a coloboma in a child with multi-system involvement. A 5-year-old male child, with hydrocephalus, born of nonconsanguineous marriage was evaluated after a ventriculoperitoneal shunt procedure. His best-corrected visual acuity was 20/40 in the right eye and 20/400 in the left eye with compound myopic astigmatism. He also had 15° exotropia in the left eye.
Anterior segment and pupillary reaction were normal in both eyes. The fundus evaluation of the right eye revealed a coloboma inferior to the optic disc about 3 disc diameters in size extending beyond the equator anteriorly with laser scars around the coloboma [Figure 1]. The left eye had a coloboma just inferior to the optic disc extending beyond the equator with chorioretinal atrophy in the peripapillary area. Left macula showed a coloboma of 2 disc diameter in size [Figure 2]. Systemic evaluation showed generalized ligament laxity, tapering fingers, bilateral genu and cubitus valgus and platybasily. He had undergone surgical treatment for inguinal hernia and hydrocoele. He was also treated for pulmonary tuberculosis. No syndromes or associations were detected in this child and ocular examination of family members revealed no abnormalities. Our patient seemed to be a case of isolated coloboma. Regular follow-up was advised to correct the changes in refraction associated with the growth of the child and also fundus examination.
Figure 1.
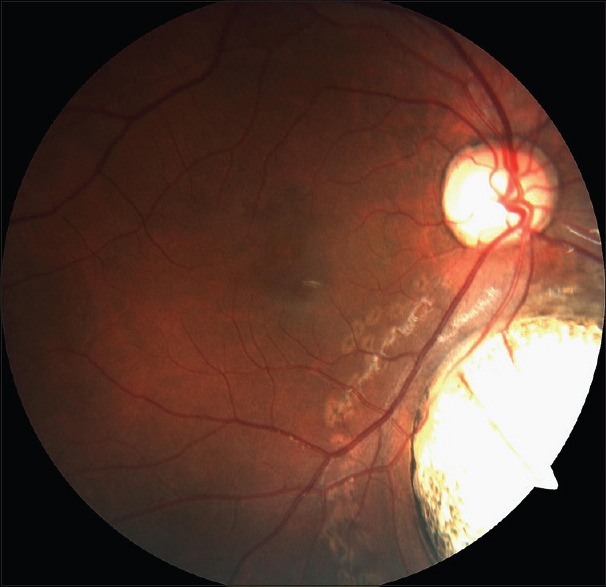
Fundus picture of right the eye showing coloboma inferior to optic disc
Figure 2.
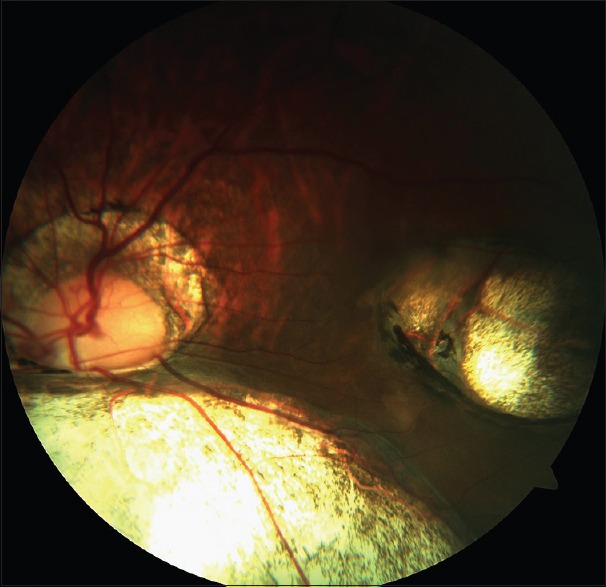
Fundus picture of the left eye showing coloboma inferior to optic disc and also coloboma involving the macula
Congenital coloboma is a relatively rare condition involving 0.5–0.7/10,000 births.[1] It is most often seen as isolated cases without inheritance pattern though rarely autosomal dominant and other inheritance patterns have been reported. It occurs due to the failure of fusion of the optic fissure that normally occurs at 5–7 weeks. It is more commonly found at the infero-nasal quadrant in line with the embryological development and thus termed as typical coloboma.[2] An even rarer atypical variant is the macular coloboma that is often bilateral and symmetrical. A chromosomal analysis and genetic counseling are also often relevant.[2,3] A chorioretinal coloboma, especially involving the posterior pole predisposes the eye to retinal detachment. Hence regular monitoring is indicated.[4] Fundus evaluation also should be done to look for breaks at the edge of the coloboma. Prophylactic laser photocoagulation may be indicated for colobomas not involving the macula and papillomacular bundle. However, the role of laser photocoagulation remains controversial. The visual prognosis in such cases is difficult to predict as patients with large colobomata and optic nerve involvement can still have near normal vision and stereopsis. However, all such children should receive careful treatment for refractive errors and possible amblyopia.[5] Unilateral coloboma should be managed aggressively to maximize visual potential as there is often refractive error present putting the patients at risk of amblyopia. Low vision rehabilitation services are also to be borne in mind during the rehabilitative management. The presence of a macular coloboma not only warrants an ophthalmic evaluation and management but also a multi-disciplinary approach for the appropriate management of the associated abnormalities.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Hornby SJ, Adolph S, Gilbert CE, Dandona L, Foster A. Visual acuity in children with coloboma: Clinical features and a new phenotypic classification system. Ophthalmology. 2000;107:511–20. doi: 10.1016/s0161-6420(99)00140-2. [DOI] [PubMed] [Google Scholar]
- 2.Onwochei BC, Simon JW, Bateman JB, Couture KC, Mir E. Ocular colobomata. Surv Ophthalmol. 2000;45:175–94. doi: 10.1016/s0039-6257(00)00151-x. [DOI] [PubMed] [Google Scholar]
- 3.Gonzalez-Rodriguez J, Pelcastre EL, Tovilla-Canales JL, Garcia-Ortiz JE, Amato-Almanza M, Villanueva-Mendoza C, et al. Mutational screening of CHX10, GDF6, OTX2, RAX and SOX2 genes in 50 unrelated microphthalmia-anophthalmia-coloboma (MAC) spectrum cases. Br J Ophthalmol. 2010;94:1100–4. doi: 10.1136/bjo.2009.173500. [DOI] [PubMed] [Google Scholar]
- 4.Schubert HD. Structural organization of choroidal colobomas of young and adult patients and mechanism of retinal detachment. Trans Am Ophthalmol Soc. 2005;103:457–72. [PMC free article] [PubMed] [Google Scholar]
- 5.Chang L, Blain D, Bertuzzi S, Brooks BP. Uveal coloboma: Clinical and basic science update. Curr Opin Ophthalmol. 2006;17:447–70. doi: 10.1097/01.icu.0000243020.82380.f6. [DOI] [PubMed] [Google Scholar]


