Abstract
Background:
Behavioral disorders are common in the pediatric age group. This study aims to assess the relationship between the frequency of behavioral and mental disorders and counseling with family members and friends in a representative sample of Iranian children and adolescents.
Methods:
In this nationwide study, 14880 school students, aged 6–18 years, were selected by cluster and stratified multi-stage sampling method from 30 provinces in Iran. The World Health Organization Global School-based Health Survey questionnaire was used.
Results:
Overall, 13486 students (49.2% girls) with the mean (standard deviation) age of 12.47 (3.36) years completed the study. According to the students’ self-report, 56.1% of boys and 42.2% of girls shared their problems with their fathers. All behavioral disorders were less prevalent in children and adolescents who consulted with their father compared with those who did not (P < 0.001). In addition, 84.6% of boys and 84.0% of girls shared their problem with their mother. All behavioral disorders were less prevalent in children and adolescents who consulted with their mother compared with those who did not (P < 0.001). 45.6% of boys and 44.8% of girls shared their problem with their brother or sister. Some behavioral disorders were less prevalent in children and adolescents who consulted with their brother or sister (P < 0.01); however, the prevalence was not statistically different for most disorders (P > 0.05). Moreover, 60.4% of boys and 66.0% of girls shared their problems with their friends. The prevalence of most behavioral disorders was lower in those who consulted with their friends (P < 0.001).
Conclusions:
Children and adolescents should be encouraged to consult with their parents and friends about their problems. Parents should offer their children an opportunity to express their views and wishes about their problems.
Keywords: Children and adolescents, consultation, mental health
INTRODUCTION
During the recent two decades, more studies on the epidemiology of mental disorders in children and adolescents have been conducted, as the number of 10,000 papers published in this field during 1980–1993 has increased to 40,000 papers in 1993–2000.[1,2,3] Results of these studies showed that one out of every three to four child or adolescent worldwide suffers from mental disorders, and one out of every 10 youths meets criteria for serious emotional disturbance.[3,4,5] These disorders can affect social-educational functions and public life of children and adolescents.[6]
On the other hand, more recent studies showed that suicide is the third leading cause of death for children and adolescents, and more than 50% of mental disorders in adults have childhood onset.[7] It is also estimated that behavioral disorders are more prevalent than physical diseases as asthma and diabetes in children and adolescents.[8,9] While more attention of the medical community was focused to physical illness, actually the importance of behavioral disorders is being taken into account.[10]
Several factors are associated with the incidence and persistence of mental disorders in children and adolescents. These factors can be categorized into the child characteristics as well as family and parental factors.[10] The main child factors include gender, race, age, physical health, nutritional status, underweight, overweight and obesity, prenatal and perinatal medical history, alcohol use, medications, infectious and chronic noninfectious diseases, previous exposure to environmental toxins such as lead and mercury. The main family factors include parents’ educational level, social class, occupation, family number, immigration, parents’ divorce, mental and physical health of the parents and other relatives.[6,11,12,13,14,15] Anxiety disorders are the most common mental disorders in children and adolescents. About 30% of children and adolescents suffer from kind of anxiety disorder, and 2.2% of them are suffering from generalized anxiety.[16] Anxiety disorders are more prevalent in girls; they may occur alone or along with other disorders.[17,18] Several studies have shown that the peak onset age of anxiety disorders varies, as separation anxiety and specific phobia occurs in middle childhood, social anxiety occurs in middle adolescence, panic disorder in late adolescence.[10,19] In addition, the peak onset of the behavioral disorder are at age 11, mood disorders at age 13, and substance abuse at age 15.[20,21,22,23]
Given the high prevalence of behavioral and mental disorders in communities, and their early onset and persistence throughout life in one side, and their negative impact on social, educational, and economic functions of individual and society on the other side, understanding the epidemiology and risk factors of these disorders is essential.[7,10,16]
Since there is no extensive study so far concerning the relationship between behavioral and mental disorders and counseling with family members and friends, this study aimed to extensively study this subject in Iranian children and adolescents.
METHODS
This nationwide study was conducted in 2011–2012 as the fourth national survey of a school-based surveillance program entitled the Childhood and Adolescence Surveillance and Prevention of Adult Noncommunicable Disease (CASPIAN-IV) study. We have previously reported the methodology of this study,[24] and here, we explain the methods related to the current paper.
Study population and sampling framework
The study population consisted of elementary, secondary, and high-school students from rural and urban areas of Iran. They were selected by multistage, cluster sampling method from 30 provinces of the country (48 clusters of 10 students in each province). Stratification was performed in each province according to location of residence (urban, rural), and school grade (elementary, middle- and high-school) proportional to size and with equal sex ratio; that is, in each province, the number of boys and girls were the same and the ratios in urban and rural areas were proportionate to the population of students in each area. In this way, the number of samples in rural, urban areas and in each school grade was divided proportionally to the population of students in each grade.
Cluster sampling with equal clusters was used in each province to reach the sample size of interest. The clusters were determined at the level of schools, containing 10 samples in each cluster.
The sample size was determined according to the cluster sampling method; the maximum sample size which could give a good estimate of all risk factors of interest was selected. Thus, the sample size was calculated as 480 subjects in each province; therefore, 48 clusters of 10 subjects were selected in each province. Overall, 14880 students were selected by multi-stage sampling from 30 provinces in Iran. The questionnaire of the World Health Organization-Global School-based Student Health Survey was used.
Statistical analysis
Continuous variables are presented as mean (standard deviation), and categorical data as a number (percent). Categorical data were analyzed by Chi-square test. Statistical analysis was done by the Stata Corp. 2011 (Stata Statistical Software: Release 12. College Station, TX, USA: Stata Corp. LP. Package) using the survey (cluster) analysis design. P < 0.05 was considered as statistically significant.
RESULTS
The participation rate of this survey was 90.6%, and participants consisted of 13486 students (49.2% girls). They had a mean age of 12.47 (3.36) years without significant difference between boys (12.36 [3.40]) and girls (12.58 [3.32]). A total of 75.6% of students were from urban, and 24.4% were from rural areas and 46%, 25.9%, and 28.1% were in elementary, secondary, and high-school levels, respectively.
The association between worthless and counseling with each of family members, including father, mother, sister, brother, as well as with friends in girls and boys are presented in Tables 1 and 2, respectively. According to these results, 56.1% of boys and 42.2% of girls shared their problems with their father. Worthless was less prevalent in children and adolescents who consult with their father compared with those who did not consult (P < 0.001). In addition, 84.6% of boys and 84.1% of girls shared their problems with their mother. Similarly, the prevalence of worthless was lower in children and adolescents who consulted with their mother compared with those who did not consult (P < 0.001). Overall, 45.6% of boys and 44.8% of girls shared their problems with their brother or sister. Worthless was less prevalent in boys who consulted with their brother or sister compared with those who did not consult (P < 0.001). However, it was not statistically significant in girls (P > 0.0.5). It was also shown that 60.4% of boys and 66.0% of boys shared their problems with their friends. Worthless was less prevalent in children and adolescents who consult with their friends compared with those who did not consult (P < 0.001).
Table 1.
Association of psychiatric distress and consultation with family members and friends in girls: The CASPIAN-IV study
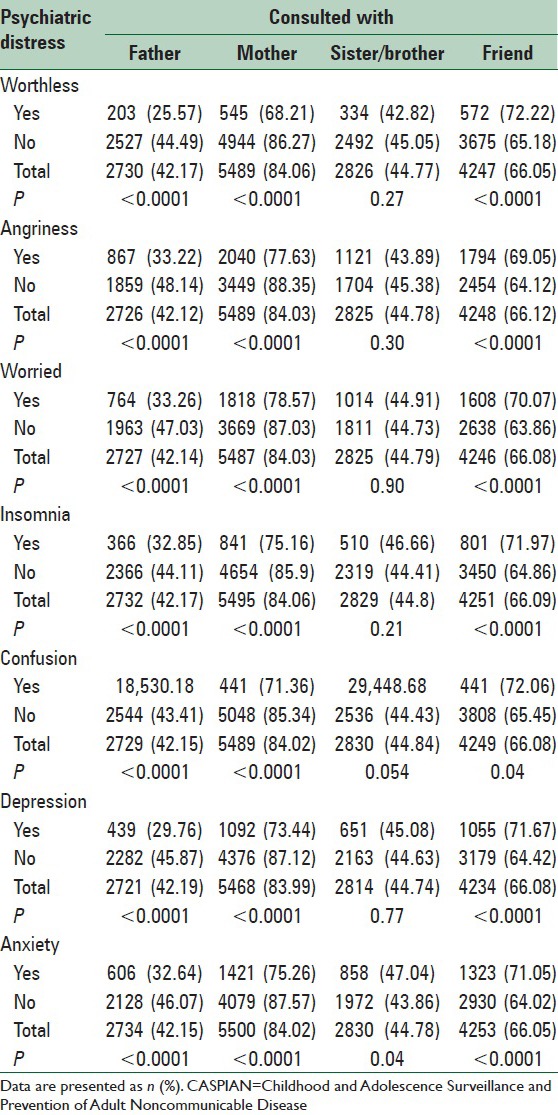
Table 2.
Association of psychiatric distress and consultation with family members and friends in boys: The CASPIAN-IV study
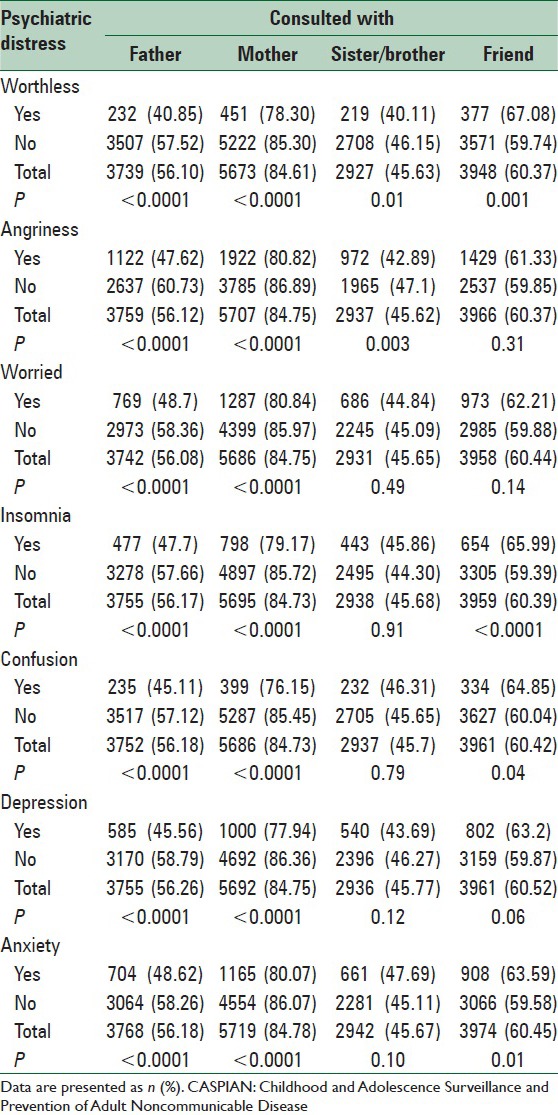
Regarding the association between angriness and counseling with each of family members, including father, mother, sister, brother, as well as with friends, we found that 56.1% of boys and 42.1% of girls shared their problems with their father. Angriness was less prevalent in children and adolescents who consulted with their father compared with those who did not consult (P < 0.001). In addition, 84.7% of boys and 84.0% of girls shared their problems with their mother. Similarly, the prevalence of angriness was lower in children and adolescents who consulted with their mother compared with those who did not consult (P < 0.001). Moreover, 45.6% of boys and 44.8% of girls shared their problems with their brother or sister. Angriness was less prevalent in boys who consulted with their brother or sister compared with those who did not consult (P < 0.001). However, it was not statistically significant in girls (P > 0.0.5). It was also shown that 60.4% of boys and 66.1% of boys shared their problems with their friends. Angriness was less prevalent in girls who consulted with their friends (P < 0.001), but it was not statistically significant in boys.
Worried was less prevalent in children and adolescents who consulted with their father or mother compared with those who did not consult (P < 0.001). The prevalence of worried was not different in boys who consulted with their brother or sister or friend compared with those who did not consult (P > 0.05). Similarly, the prevalence of worried was not different in girls who consulted with their brother or sister compared with those who did not consult (P > 0.05), but it was less prevalent in girls who consulted with their friends (P < 0.001).
Anxiety, depression, confusion, insomnia were less prevalent in children and adolescents who consulted with their father or mother compared with those who did not consult (P < 0.001). Anxiety, confusion, and insomnia were less prevalent in those who consulted with their friends (P < 0.05), but the corresponding figure was not significant for depression (P > 0.05).
The prevalence of depression, confusion, and insomnia was not different in children and adolescents who consulted with their brother or sister compared with those who did not consult (P > 0.05). The prevalence of anxiety was lower in girls who consulted with their brother or sister (P < 0. 01), but this prevalence was not different in boys (P > 0.05).
DISCUSSION
This study shows that the prevalence of all mental disorders including worthless, angriness, worried, anxiety, insomnia, confusion, and depression were lower in children and adolescents who consulted with their father or mother compared with those who did not consult. In addition, this association was significant for most of these mental disorders including insomnia, confusion, anxiety, worthless, and worried in those who consult with their friends. The prevalence of some of these disorders was lower in those who consulted with their brother or sister.
Previous studies have shown that behavioral disorders are less common in those who have the support of families, especially parents. Furthermore, consultation with family members and friends reduces the prevalence of behavioral disorders.[7,10,11,12,13,14,15,16,25] It is noteworthy that previous studies have described the results as a whole, but we have presented results by family members and friends, and also by the type of mental disorder.
Several studies have also investigated the effect of parents’ socioeconomic status and their attention to their children's problems. Results of these studies indicate that mental disorders are less prevalent in children from families with higher socioeconomic status and with more parents’ attention.[26,27,28,29] The education level of parents, especially mothers is also important in this regard.[29]
These findings of the present study suggest that children and adolescents should discuss about their problems with their parents and friends, and parents should talk to their children and should care more about their children's problems. Unfortunately, most studies show that only less than half of children and adolescents with behavioral disorders are being identified and in good and timely service, which is a worrying problem in both developed and developing countries.[30,31] Most of these children and adolescents are being identified and treated just after school failures, conflicts or dispute or attempts to suicide.[12,32,33]
Behavioral disorders impose a heavy economic cost on families and society, both directly and indirectly.[34] Such disorders can also cause or aggravate physical problems in children and adolescents, many of which have persisted into adulthood.[29,35] Thus, the global health communities have focused attention to behavioral problems in recent years, and significant advances have been achieved in prognosis, regular servicing, care, and control of behavioral disorders. However, still a large gap exists to reach the desired results.[7] Therefore, the family, parents, friends, school staff, pediatricians, psychologists, and psychiatrists have a very important role in this context.[31,36]
The main limitations of this study are its cross-sectional nature, and using self-reported data of students. The strengths of the current study are using an internationally accepted questionnaire, including a large sample size at the national level, and studying the consult with each family members or friends, and categorized by behavioral disorders.
CONCLUSIONS
Children and adolescents should be encouraged to consult with their parents and friends about their problems. Parents should offer their children an opportunity to express their views and wishes about their problems.
Footnotes
Source of Support: Data of a national surveillance program was used for this study
Conflict of Interest: None declared.
REFERENCES
- 1.Costello EJ, Mustillo S, Keller G, Angold A. Prevalence of psychiatric disorders in childhood and adolescence. In: Levin BL, Petrila J, Hennessy KD, editors. Mental Health Services: A Public Health Perspective. 2nd ed. Oxford, UK: Oxford University Press; 2004. pp. 111–28. [Google Scholar]
- 2.Weich S, Araya R. International and regional variation in the prevalence of common mental disorders: Do we need more surveys? Br J Psychiatry. 2004;184:289–90. doi: 10.1192/bjp.184.4.289. [DOI] [PubMed] [Google Scholar]
- 3.Costello EJ, Egger H, Angold A. 10-year research update review: The epidemiology of child and adolescent psychiatric disorders: I. Methods and public health burden. J Am Acad Child Adolesc Psychiatry. 2005;44:972–86. doi: 10.1097/01.chi.0000172552.41596.6f. [DOI] [PubMed] [Google Scholar]
- 4.Kessler RC, Amminger GP, Aguilar-Gaxiola S, Alonso J, Lee S, Ustün TB. Age of onset of mental disorders: A review of recent literature. Curr Opin Psychiatry. 2007;20:359–64. doi: 10.1097/YCO.0b013e32816ebc8c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Merikangas KR, He JP, Brody D, Fisher PW, Bourdon K, Koretz DS. Prevalence and treatment of mental disorders among US children in the 2001-2004 NHANES. Pediatrics. 2010;125:75–81. doi: 10.1542/peds.2008-2598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brauner CB, Stephens CB. Estimating the prevalence of early childhood serious emotional/behavioral disorders: Challenges and recommendations. Public Health Rep. 2006;121:303–10. doi: 10.1177/003335490612100314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Belfer ML. Child and adolescent mental disorders: The magnitude of the problem across the globe. J Child Psychol Psychiatry. 2008;49:226–36. doi: 10.1111/j.1469-7610.2007.01855.x. [DOI] [PubMed] [Google Scholar]
- 8.Akinbami LJ, Schoendorf KC, Parker J. US childhood asthma prevalence estimates: The Impact of the 1997 National Health Interview Survey redesign. Am J Epidemiol. 2003;158:99–104. doi: 10.1093/aje/kwg109. [DOI] [PubMed] [Google Scholar]
- 9.CDC. National Diabetes Fact Sheet. 2007. [Last accessed on 2010 Jan 25]. Available from: http://www.cdc.gov/diabetes/pubs/pdf/ndfs_2007.pdf .
- 10.Merikangas KR, Nakamura EF, Kessler RC. Epidemiology of mental disorders in children and adolescents. Dialogues Clin Neurosci. 2009;11:7–20. doi: 10.31887/DCNS.2009.11.1/krmerikangas. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Earls F. Epidemiology and child psychiatry: Future prospects. Compr Psychiatry. 1982;23:75–84. doi: 10.1016/0010-440x(82)90011-6. [DOI] [PubMed] [Google Scholar]
- 12.Fergusson DM, Horwood LJ. The Christchurch Health and Development Study: Review of findings on child and adolescent mental health. Aust N Z J Psychiatry. 2001;35:287–96. doi: 10.1046/j.1440-1614.2001.00902.x. [DOI] [PubMed] [Google Scholar]
- 13.Goodman SH, Hoven CW, Narrow WE, Cohen P, Fielding B, Alegria M, et al. Measurement of risk for mental disorders and competence in a psychiatric epidemiologic community survey: The National Institute of Mental Health Methods for the Epidemiology of Child and Adolescent Mental Disorders (MECA) Study. Soc Psychiatry Psychiatr Epidemiol. 1998;33:162–73. doi: 10.1007/s001270050039. [DOI] [PubMed] [Google Scholar]
- 14.Buka SL, Monuteaux M, Earls F. The epidemiology of child and adolescent mental disorders. In: Tsuang MT, Tohen M, editors. Textbook in Psychiatric Epidemiology. 2nd ed. New York: John Wiley and Sons Inc; 2002. pp. 629–55. [Google Scholar]
- 15.Jari M, Qorbani M, Motlagh ME, Heshmat R, Ardalan G, Kelishadi R. Association of overweight and obesity with mental distress in Iranian adolescents: The CASPIAN-III Study. Int J Prev Med. 2014;5:256–61. [PMC free article] [PubMed] [Google Scholar]
- 16.Merikangas KR, He JP, Burstein M, Swanson SA, Avenevoli S, Cui L, et al. Lifetime prevalence of mental disorders in U.S. adolescents: Results from the National Comorbidity Survey Replication-Adolescent Supplement (NCS-A) J Am Acad Child Adolesc Psychiatry. 2010;49:980–9. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 18.Merikangas KR, Avenevoli S. Epidemiology of mood and anxiety disorders in children and adolescents. In: Tsaung MT, Tohen M, editors. Textbook in Psychiatric Epidemiology. 2nd ed. New York: Wiley-Liss; 2002. pp. 657–704. [Google Scholar]
- 19.Pine DS, Cohen P, Gurley D, Brook J, Ma Y. The risk for early-adulthood anxiety and depressive disorders in adolescents with anxiety and depressive disorders. Arch Gen Psychiatry. 1998;55:56–64. doi: 10.1001/archpsyc.55.1.56. [DOI] [PubMed] [Google Scholar]
- 20.Cohen P, Cohen J, Kasen S, Velez CN, Hartmark C, Johnson J, et al. An epidemiological study of disorders in late childhood and adolescence - I. Age-and gender-specific prevalence. J Child Psychol Psychiatry. 1993;34:851–67. doi: 10.1111/j.1469-7610.1993.tb01094.x. [DOI] [PubMed] [Google Scholar]
- 21.McGee R, Feehan M, Williams S, Anderson J. DSM-III disorders from age 11 to age 15 years. J Am Acad Child Adolesc Psychiatry. 1992;31:50–9. doi: 10.1097/00004583-199201000-00009. [DOI] [PubMed] [Google Scholar]
- 22.Kim-Cohen J, Caspi A, Moffitt TE, Harrington H, Milne BJ, Poulton R. Prior juvenile diagnoses in adults with mental disorder: Developmental follow-back of a prospective-longitudinal cohort. Arch Gen Psychiatry. 2003;60:709–17. doi: 10.1001/archpsyc.60.7.709. [DOI] [PubMed] [Google Scholar]
- 23.Costello EJ, Egger HL, Angold A. The developmental epidemiology of anxiety disorders: Phenomenology, prevalence, and comorbidity. Child Adolesc Psychiatr Clin N Am. 2005;14:631–48. doi: 10.1016/j.chc.2005.06.003. vii. [DOI] [PubMed] [Google Scholar]
- 24.Kelishadi R, Heshmat R, Motlagh ME, Majdzadeh R, Keramatian K, Qorbani M, et al. Methodology and Early Findings of the Third Survey of CASPIAN Study: A National School-based Surveillance of Students’ High Risk Behaviors. Int J Prev Med. 2012;3:394–401. [PMC free article] [PubMed] [Google Scholar]
- 25.Cheng Y, Tao M, Riley L, Kann L, Ye L, Tian X, et al. Protective factors relating to decreased risks of adolescent suicidal behaviour. Child Care Health Dev. 2009;35:313–22. doi: 10.1111/j.1365-2214.2009.00955.x. [DOI] [PubMed] [Google Scholar]
- 26.Shanahan L, Copeland W, Costello EJ, Angold A. Specificity of putative psychosocial risk factors for psychiatric disorders in children and adolescents. J Child Psychol Psychiatry. 2008;49:34–42. doi: 10.1111/j.1469-7610.2007.01822.x. [DOI] [PubMed] [Google Scholar]
- 27.Dodge KA, Pettit GS. A biopsychosocial model of the development of chronic conduct problems in adolescence. Dev Psychol. 2003;39:349–71. doi: 10.1037//0012-1649.39.2.349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kumpfer KL, Summerhays JF. Prevention approaches to enhance resilience among high-risk youth: Comments on the papers of Dishion and Connell and Greenberg. Ann N Y Acad Sci. 2006;1094:151–63. doi: 10.1196/annals.1376.014. [DOI] [PubMed] [Google Scholar]
- 29.Parry-Langdon N, Clements A, Fletcher D, Goodman R. Newport, UK: Office for National Statistics; 2008. Three years on: Survey of the development and emotional Weil-being of children and young people. [Google Scholar]
- 30.Wu P, Hoven CW, Bird HR, Moore RE, Cohen P, Alegria M, et al. Depressive and disruptive disorders and mental health service utilization in children and adolescents. J Am Acad Child Adolesc Psychiatry. 1999;38:1081–90. doi: 10.1097/00004583-199909000-00010. [DOI] [PubMed] [Google Scholar]
- 31.Ford T. Practitioner review: How can epidemiology help us plan and deliver effective child and adolescent mental health services? J Child Psychol Psychiatry. 2008;49:900–14. doi: 10.1111/j.1469-7610.2008.01927.x. [DOI] [PubMed] [Google Scholar]
- 32.Angold A, Erkanli A, Farmer EM, Fairbank JA, Burns BJ, Keeler G, et al. Psychiatric disorder, impairment, and service use in rural African American and white youth. Arch Gen Psychiatry. 2002;59:893–901. doi: 10.1001/archpsyc.59.10.893. [DOI] [PubMed] [Google Scholar]
- 33.Lewinsohn PM, Rohde P, Seeley JR. Major depressive disorder in older adolescents: Prevalence, risk factors, and clinical implications. Clin Psychol Rev. 1998;18:765–94. doi: 10.1016/s0272-7358(98)00010-5. [DOI] [PubMed] [Google Scholar]
- 34.Hsia RY, Belfer ML. A framework for the economic analysis of child and adolescent mental disorders. Int Rev Psychiatry. 2008;20:251–9. doi: 10.1080/09540260802002434. [DOI] [PubMed] [Google Scholar]
- 35.Chavira DA, Garland AF, Daley S, Hough R. The impact of medical comorbidity on mental health and functional health outcomes among children with anxiety disorders. J Dev Behav Pediatr. 2008;29:394–402. doi: 10.1097/DBP.0b013e3181836a5b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cheung AH, Dewa CS. Mental health service use among adolescents and young adults with major depressive disorder and suicidality. Can J Psychiatry. 2007;52:228–32. doi: 10.1177/070674370705200404. [DOI] [PubMed] [Google Scholar]


