Abstract
Background:
Non-alcoholic fatty liver is the most chronic liver disease that eventually can become cirrhosis. One of the underlying assumptions for the fatty liver created by inflammation of the hepatocytes. We aimed to assess the association between non-alcoholic fatty liver disease (NAFLD) and sub-clinical inflammation.
Materials and Methods:
This is a cross-sectional study which was conducted on 55 patients over 30 years, with NAFLD. Fatty liver grade was assessed using liver ultrasound. Liver enzymes (alanine aminotransferase, aspartate aminotransferase), anthropometric characteristics and inflammatory marker C-reactive protein (CRP) were measured. Qualitative variables (sex and fatty liver grade) and quantitative variables such as were compared with independent t-test and Chi-square test. Relationship between fatty liver grade and inflammatory index was assessed with SPSS software (version 20; SPSS, Inc. Chicago, IL, USA).
Results:
Non-alcoholic fatty liver grades were associated with CRP level and this relationship remains in statistically significant level even after adjusting the effects of confounding variables such as age, sex and body mass index of participants (P = 0.016).
Conclusion:
In this cross-sectional study, presentation of NAFLD showed a significant correlation with sub-clinical systemic inflammation and CRP level.
Key Words: C-reactive protein, inflammation, non-alcoholic fatty liver
INTRODUCTION
Non-alcoholic fatty liver disease (NAFLD) includes a variety of diseases ranking from simple steatosis or fatty liver through non-alcoholic steatohepatitis (NASH) to fibrosis that may finally lead to irretrievable live cancer.[1] NASH was first defined by Ludwig et al.[2] in a number of patients who presented no alcohol intake but whose liver histology simulated with alcoholic liver diseases.[3] The outbreak of NAFLD has been ongoing augment in equal with the concerning world-wide epidemic of obesity and diabetes and it is anticipated to increase in the future.[4] In the Western countries, NAFLD is formerly becoming the most prevalent reason of liver disease with the assessment of prevalence being between 17% and 33% in the population[5] and increasing as high as 90% in morbidly obese individuals.[6] NASH, the most severe and clinically form of NAFLD, is less common and is anticipated to be present between 5.7% and 17% of the population, steatosis still the numbers rising in the morbidity overweight (37%).[7] The prevalence of overweight among US children has trebled in the last decade, increasing from 5% in 1980 to 15% in 1990 and is present around 17%.[8] This disorders is forcefully in relationship with insulin resistance, hypertension, glucose intolerance, obesity and heperlipidemia and is thus identified as the hepatic appearance of the metabolic syndrome.[9] Simple steatosis is largely benignant and has good prognoses. However, a significant ratio of steatotic patients wills developed steatohepatitis, which is described by hepatocyte injury and inflammation with 20-25% eventuality of developing to fibrosis and cirrhosis.[10] NAFLD is clinically quiet. The symptoms usually explained by the patients, such as fatigue and ambiguous discomfort, are entirely non-specific.[11] NAFLD as systemic inflammatory disorder can lead to the large number of the mentioned life-threaten outcome.
C-reactive protein (CRP) as an acute phase reactive proteins.[12] It is simple to reach, generally used, authentic, cheap serum indicator and widespread used for diagnosis and pursue of several morbidities.[13] CRP is produced largely in the liver tissue. In addition, CRP level was presented to rise in metabolic syndrome and diabetes, obesity, particularly central obesity.[14] CRP has also been proposed as a prognosticator of cardiovascular disease in patients with metabolic syndrome. In studies, high CRP levels have been seen to predict the metabolic syndrome,[15] type 2 diabetes mellitus[16] and coronary heart disease.[17] CRP increases expression of cell adhesion molecules, activation complement. In some studies, the correlation between raised levels CRP and NAFLD have identified,[18,19,20,21] while other studies have not found correlation results.[22] Thus, the aim of this study is defined as survey the association between NAFLD grade and sub-clinical systemic inflammation.
MATERIALS AND METHODS
The type of study is a cross-sectional study. A total of 55 patients were participated with NAFLD. 31 (56%) women and 24 (44%) men participated in this study. The consent was given of all participants. This study was conducted in Liver Disease Research Center in Isfahan University of Medical Science. Study was performed with the approval of Isfahan University of Medical Science Local Ethics Committee. Inclusion criteria were ultrasound positive result. Participants in this study had no hepatitis C, B and Wilson disease and no history of chronic liver disease, a disease that affects gallbladder and bile ducts. None of the patients was using statin, corticosteroids or any other medication that known to affect serum CRP levels. Exclusion criteria included hospitalization, lack of cooperation in the study and suffering from acute illnesses.
Anthropometric measurements
Height was measured without shoes carefully tape standing and weight was evaluated without shoes to the nearest 100 g using a Seca Scale. Body mass index (BMI) is calculated by following the formula (weight [kg]/height [m2]). Demographic information, medical history and taking any drug was collected by questionnaire.
Biochemical measurements
Fasting blood samples were taken. CRP serum was measured by high-sensitivity enzyme (test Pars Tehran, Tehran, Iran). Aspartate aminotransferase (AST) and alanine aminotransferase (ALT) serum levels were measured by using enzymatic photometric method (IFCC) with a sensitivity of 2 U/L and a coefficient of variation of 14% (kit colorimetric AST and ALT, Pars Tehran, Tehran, Iran).
Degree of fat accumulation in liver
Ultrasonography for assessment of hepatic fat accumulation in the liver is conducted to determine the level for esteatosis liver. Hepatic ultrasonography was conducted by someone who is unaware of the objectives of the study. Esaote medical ultrasound machine is used convex 3.5 MHz is equipped with a probe. Patients for ultrasound should be fasting for 8 h. Ultrasonography is done in the supine position and willing to the right hand. Right and left lobes of the upper and lower surface are studied. Echogenicity liver, the presence or absence of bulky tumors cystic or solid and calcification of its tissue was assessed. Intrahepatic bile ducts, portal vein and hepatic artery were evaluated. Esteatosis liver is semi-quantitative scoring (0 as absent of any tissue, 1 mild grade, 2 average grade and 3 grade of esteatosis severe).
Statistics analysis
SPSS statistical package (version 20; SPSS, Inc. Chicago, IL, USA).was used to perform the analyses. Quantitative as (BMI, CRP, weight, height, age, ALT, AST) and qualitative variables are expressed as mean ± standard deviation and qualitative variables (sex and fatty liver grade) was presented as their frequencies. The comparison quantitative was done with analysis of variance between fatty liver grades. Qualitative variables were compared with Chi-square tests. Ordinal regression test assessment fatty liver grades with sub-clinical inflammation. Confounding variables was controlled in regression models. P < 0.05 was considered to be significant.
RESULT
In this study, 55 patients with a mean age 47 ± 11 years participated. About 11% patients were non-alcoholic fatty liver grade 1, 80% patients in grade 2 and 9% patients in grade 3. Characteristics of patients with non-alcoholic fatty liver have been shown in Table 1.
Table 1.
Characteristics of patients with non-alcoholic fatty liver patients according its grade
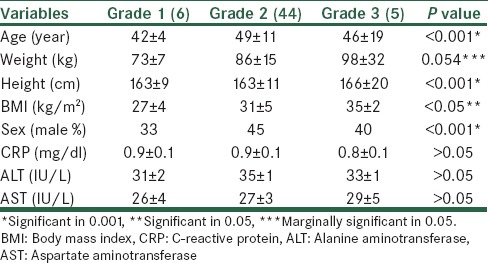
There are significant different between age, weight, height, sex, BMI, CRP, ALT and AST levels between various grades of fatty liver. BMI is directly correlated with fatty liver grade. In addition, fatty liver grade levels were significantly increased with increasing height and weight in patients. AST levels increased with increasing grade of fatty liver, but this increase was not significant.
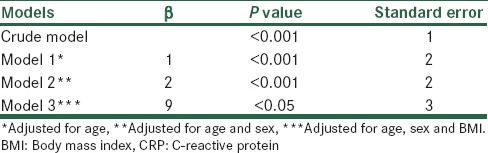
The relationship between fatty liver grades and CRP is presented in Table 2. The correlation between fatty liver grade and crp was significant in the first model (<0.001) and even after adjustment for (age, sex, BMI) this association was significant (<0.05).
Table 2.
Associations between non-alcoholic fatty liver grade and CRP in ordinal regression analysis
DISCUSSION
In this study, significant relationship was found between serum levels of CRP and non-alcoholic fatty liver grades. This finding is similar to the previous observation.
In several studies the correlation between serum CRP level and NAFLD was seen.[18,19,20,21] In a study conducted by Targher et al., CRP levels was higher in patients with fatty liver while adiponectin serum level reduced.[18] Nigma et al., observed a statistically significant association between fatty liver grade and CRP level serum.[19] Similar results were observed in other studies, too.[20,21] However, in the study which was performed by Haukeland et al., in Norway, correlation between fatty liver grade and CRP level was not seen.[22]
In clinical trials CRP increasing was correlated with metabolic syndrome and its components. Although the liver is a principal source of the CRP manufacture, fat tissue, particularly visceral fat significantly chip in to CRP production.[21] It is recognized that CRP concentration was increased in obese patients but this rising was mild and not correlate with metabolic syndrome and importantly to steatohepatitis.[22]
The new definition of metabolic syndrome is based on insulin resistance and liver function that are the result of BMI increased. Grades of fatty liver increased with increasing BMI in our study. BMI was the most important determinant of insulin resistance.[23] A higher BMI was associated with decreased insulin sensitivity and increased inflammatory indices.[24] Tumor necrosis factor-alpha (TNF-α) is a key pro-inflammatory cytokine that plays a fundamental role in intercede inflammation.[21] Hepatic production of TNF-α through is close thoroughly activate by IκB kinase nuclear factor kappa B (NF-κB) pathway. The activation of NF-κB can occur through different signaling mechanisms. It is well-established that reactive oxygen species (ROS)-induced activation pathways rely primarily on the inhibitor of κB-kinase complex activation, a process that may also be triggered by the pro-inflammatory cytokines TNF-α and interleukin-1β (IL-1β) as well as by lipopolysaccharide,[25,26] through different signaling cascades.[27] Hepatocyte damage accompany with cytokine production of Kupffer cells and leaded to further raise expression of TNF-α and IL-6 increasing both liver and systemic levels of pro-inflammatory cytokines. The faulty cycle of rising inflammation and insulin resistance is close.[28] Augmenting path for inflammation beginning with the inability of insulin to repress lipolysis in the adipose tissue that drawback excess free fatty acid (FFA) flux to the liver FFA to raise hepatic β-oxidation. Increase levels of ROS and it start oxidative damage that exacerbates the activation of inflammatory pathways. TNF-α develop expression of IL-6 as the main hepatic excites for the production of CRP).[29] CRP is regarded as a beneficial non-specific biochemical indicator of low grade systemic-inflammation.[30] Our study observed that rises in circulating CRP levels could be by itself as an indicator of the presence of NAFLD. Therefore, we propose that consecutive measurements of CRP can be beneficial in clinical management and follow-up of NAFLD patients.
We had a number of limitations to this study. The first limitation is a small sample size of participants especially various grades of fatty liver. Second limitation is that the use of a liver ultrasound cannot accurately detect fatty liver disease and liver biopsy should be used for accurately diagnosis. Third limitation of this study was design study because in the cross-sectional study cannot confirm associations between variables.
CONCLUSION
In this study, a significant relationship was observed between CRP and grade of fatty liver. Probably increased BMI increases insulin resistance. Insulin resistance causes increased inflammation in hepatocytes and increased inflammation on hepatocytes can increase the severity and grade of fatty liver. Finally, further studies should be done to determine the exact relationship between increased inflammation and NAFLD.
ACKNOWLEDGMENT
We thank all the participants and colleagues of metabolic liver diseases research center.
Footnotes
Source of Support: Nil
Conflicts of Interest: None declared.
REFERENCES
- 1.Browning JD, Szczepaniak LS, Dobbins R, Nuremberg P, Horton JD, Cohen JC, et al. Prevalence of hepatic steatosis in an urban population in the United States: Impact of ethnicity. Hepatology. 2004;40:1387–95. doi: 10.1002/hep.20466. [DOI] [PubMed] [Google Scholar]
- 2.Ludwig J, Viggiano T, Mill B, Ott B. Non alcoholic steatohepatitis: Mayo Clinic experiences with a hitherto unnamed disease. Mayo Clin Proc. 1980;55:434–438. [PubMed] [Google Scholar]
- 3.Farrell GC, Larter CZ. Nonalcoholic fatty liver disease: From steatosis to cirrhosis. Hepatology. 2006;43:S99–112. doi: 10.1002/hep.20973. [DOI] [PubMed] [Google Scholar]
- 4.Adams LA, Angulo P. Recent concepts in non-alcoholic fatty liver disease. Diabet Med. 2005;22:1129–33. doi: 10.1111/j.1464-5491.2005.01748.x. [DOI] [PubMed] [Google Scholar]
- 5.Adams LA, Lymp JF, St Sauver J, Sanderson SO, Lindor KD, Feldstein A, et al. The natural history of nonalcoholic fatty liver disease: A population-based cohort study. Gastroenterology. 2005;129:113–21. doi: 10.1053/j.gastro.2005.04.014. [DOI] [PubMed] [Google Scholar]
- 6.Ahmed MH, Byrne CD. Current treatment of non-alcoholic fatty liver disease. Diabetes Obes Metab. 2009;11:188–95. doi: 10.1111/j.1463-1326.2008.00926.x. [DOI] [PubMed] [Google Scholar]
- 7.Angulo P, Lindor KD. Non-alcoholic fatty liver disease. J Gastroenterol Hepatol. 2002;17(Suppl):S186–90. doi: 10.1046/j.1440-1746.17.s1.10.x. [DOI] [PubMed] [Google Scholar]
- 8.Bansilal S, Farkouh ME, Fuster V. Role of insulin resistance and hyperglycemia in the development of atherosclerosis. Am J Cardiol. 2007;99:6B–14. doi: 10.1016/j.amjcard.2006.11.002. [DOI] [PubMed] [Google Scholar]
- 9.Bass M, Merriman R. Fatty acid metabolism and lipotoxicity in the pathogenesis of NAFLD/NASH. Fatty Liver Disease: NASH and Related Disorders. J Gastroenterol Hepatol. 2010;21:109–22. [Google Scholar]
- 10.Bataller R, Sancho-Bru P, Ginès P, Lora JM, Al-Garawi A, Solé M, et al. Activated human hepatic stellate cells express the renin-angiotensin system and synthesize angiotensin II. Gastroenterology. 2003;125:117–25. doi: 10.1016/s0016-5085(03)00695-4. [DOI] [PubMed] [Google Scholar]
- 11.Blake G, Ridker P. Inflammatory bio-markers and NAFLD. J Intern Med. 2010;4:283–94. doi: 10.1046/j.1365-2796.2002.01019.x. [DOI] [PubMed] [Google Scholar]
- 12.Massaro KS, Costa SF, Leone C, Chamone DA. Procalcitonin (PCT) and C-reactive protein (CRP) as severe systemic infection markers in febrile neutropenic adults. BMC Infect Dis. 2007;7:137. doi: 10.1186/1471-2334-7-137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yudkin JS, Stehouwer CD, Emeis JJ, Coppack SW. C-reactive protein in healthy subjects: Associations with obesity, insulin resistance, and endothelial dysfunction: A potential role for cytokines originating from adipose tissue? Arterioscler Thromb Vasc Biol. 1999;19:972–8. doi: 10.1161/01.atv.19.4.972. [DOI] [PubMed] [Google Scholar]
- 14.Danesh J, Whincup P, Walker M, Lennon L, Thomson A, Appleby P, et al. Low grade inflammation and coronary heart disease: Prospective study and updated meta-analyses. BMJ. 2000;321:199–204. doi: 10.1136/bmj.321.7255.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Farrell GC. Non-alcoholic steatohepatitis: What is it, and why is it important in the Asia-Pacific region? J Gastroenterol Hepatol. 2003;18:124–38. doi: 10.1046/j.1440-1746.2003.02989.x. [DOI] [PubMed] [Google Scholar]
- 16.Angulo P. Nonalcoholic fatty liver disease. N Engl J Med. 2002;346:1221–31. doi: 10.1056/NEJMra011775. [DOI] [PubMed] [Google Scholar]
- 17.Chitturi S, Abeygunasekera S, Farrell GC, Holmes-Walker J, Hui JM, Fung C, et al. NASH and insulin resistance: Insulin hypersecretion and specific association with the insulin resistance syndrome. Hepatology. 2002;35:373–9. doi: 10.1053/jhep.2002.30692. [DOI] [PubMed] [Google Scholar]
- 18.Targher G, Bertolini L, Rodella S, Lippi G, Franchini M, Zoppini G, et al. NASH predicts plasma inflammatory biomarkers independently of visceral fat in men. Obesity (Silver Spring) 2008;16:1394–9. doi: 10.1038/oby.2008.64. [DOI] [PubMed] [Google Scholar]
- 19.Nigam P1, Bhatt SP, Misra A, Vaidya M, Dasgupta J, Chadha DS. Non-alcoholic fatty liver disease is closely associated with sub-clinical inflammation: A case-control study on Asian Indians in North India. J Hepatol. 2006;44:1167–74. doi: 10.1371/journal.pone.0049286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Oruc N, Ozutemiz O, Yuce G, Akarca US, Ersoz G, Gunsar F, et al. Serum procalcitonin and CRP levels in non-alcoholic fatty liver disease: A case control study. BMC Gastroenterol. 2009;9:16. doi: 10.1186/1471-230X-9-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Uchihara M, Izumi N. High-sensitivity C-reactive protein (hs-CRP): A promising biomarker for the screening of non-alcoholic steatohepatitis (NASH) Nihon Rinsho. 2006;64:1133–8. [PubMed] [Google Scholar]
- 22.Haukeland JW, Damås JK, Konopski Z, Løberg EM, Haaland T, Goverud I, et al. Systemic inflammation in nonalcoholic fatty liver disease is characterized by elevated levels of CCL2. J Hepatol. 2006;44:1167–74. doi: 10.1016/j.jhep.2006.02.011. [DOI] [PubMed] [Google Scholar]
- 23.Gandhe MB, M L, Srinivasan AR. Evaluation of body mass index (BMI) percentile cut-off levels with reference to insulin resistance: A comparative study on south Indian obese and non-obese adolescents. J Clin Diagn Res. 2013;7:1579–82. doi: 10.7860/JCDR/2013/6263.3213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lupattelli G, De Vuono S, Boni M, Helou R, Raffaele Mannarino M, Rita Roscini A, et al. Insulin resistance and not BMI is the major determinant of early vascular impairment in patients with morbid obesity. J Atheroscler Thromb. 2013;20:924–33. doi: 10.5551/jat.18663. [DOI] [PubMed] [Google Scholar]
- 25.Kao PC, Shiesh SC, Wu TJ. Serum C-reactive protein as a marker for wellness assessment. Ann Clin Lab Sci. 2006;36:163–9. [PubMed] [Google Scholar]
- 26.Anty R, Bekri S, Luciani N, Saint-Paul MC, Dahman M, Iannelli A, et al. The inflammatory C-reactive protein is increased in both liver and adipose tissue in severely obese patients independently from metabolic syndrome, Type 2 diabetes, and NASH. Am J Gastroenterol. 2006;101:1824–33. doi: 10.1111/j.1572-0241.2006.00724.x. [DOI] [PubMed] [Google Scholar]
- 27.Yoneda M, Mawatari H, Fujita K, Iida H, Yonemitsu K, Kato S, et al. High-sensitivity C-reactive protein is an independent clinical feature of nonalcoholic steatohepatitis (NASH) and also of the severity of fibrosis in NASH. J Gastroenterol. 2007;42:573–82. doi: 10.1007/s00535-007-2060-x. [DOI] [PubMed] [Google Scholar]
- 28.Riquelme A, Arrese M, Soza A, Morales A, Baudrand R, Pérez-Ayuso RM, et al. Non-alcoholic fatty liver disease and its association with obesity, insulin resistance and increased serum levels of C-reactive protein in Hispanics. Liver Int. 2009;29:82–8. doi: 10.1111/j.1478-3231.2008.01823.x. [DOI] [PubMed] [Google Scholar]
- 29.Mohamed-Ali V, Goodrick S, Rawesh A, Katz DR, Miles JM, Yudkin JS, et al. Subcutaneous adipose tissue releases interleukin-6, but not tumor necrosis factor-alpha, in vivo . J Clin Endocrinol Metab. 1997;82:4196–200. doi: 10.1210/jcem.82.12.4450. [DOI] [PubMed] [Google Scholar]
- 30.Wieckowska A, Papouchado BG, Li Z, Lopez R, Zein NN, Feldstein AE. Increased hepatic and circulating interleukin-6 levels in human nonalcoholic steatohepatitis. Am J Gastroenterol. 2008;103:1372–9. doi: 10.1111/j.1572-0241.2007.01774.x. [DOI] [PubMed] [Google Scholar]


