Abstract
Background/Objectives
W eightloss is common in old age, but it is unclear how patterns of change associate with change in lean mass and physical function. The aim of the study was to examine BMI trajectories with change in lean mass and physical function.
Design
Prospective cohort study.
Setting
Health, Aging and Body Composition Study.
Participants
Black and white men (n=482) and women (n=516) aged 73.1±2.7 years and initially free of disability.
Measurements
BMI trajectories( annually measured weight and baseline height) were determined using a group-based trajectory model. Appendicular lean mass, gait speed, grip strength and isometric knee extension strength were assessed at baseline and after 9 years, and relative changes were calculated. Multivariable linear regression (regression coefficient (95% CI)) was used to determine associations between trajectories with relative change in lean mass and physical function.
Results
We identified four BMI trajectories for both men and women . While all demonstrated a decline in BMI, the rate of decline differed by trajectory . Relative to the trajectory 1 (BMI 22.9 kg/m2), men in trajectory 4 (BMI 33.9 kg/m2)declined more in gait speed (−10.50%( −15.74; −5.26)) and leg strength( −8.37% (−15.31; −1.42)). Relative to women in trajectory 1 (BMI 20.5 kg/m2), women in trajectory 4 (BMI 34.9 kg/m2) had greater losses in lean mass in the arms (−3.24%( −6.18; −0.30)). No other associations were observed.
Conclusion
Older adults in BMI trajector y 4 have greater declines in lean mass and physical function, however, gender differences were observed. Our results show the importance of preventing obesity.
Keywords: aging, body mass index, lean mass, physical function, trajectories
INTRODUCTION
Aging is associated with changes in body composition [1]and deterioration of physical function [2]. Weight changes may be related to impaired physical function. One study showed a failure to conserve lean mass with weight loss [3]. Approximately one-third of weight loss reflects a loss of lean mass [4, 5], therefore, greater weight loss may accelerate loss of skeletal muscle and subsequent physical function.
It is unclear whether different patterns of weight loss relate to changes in body composition or physical function. Previous studies investigating changes in weight in relation to function have defined weight change groups by cut points, or used mixed effect models which may be prone to misclassification. An advantage of group-based trajectory modeling is that it is data driven; it identifies distinctive clusters of individual trajectories that follow similar developmental trajectories [6–8]. Using trajectories as determinants could be informative , since the rate of weight loss is taken into account rather than one’s initial weight.
To date, no large cohort study has used a trajectory modelling approach to describe weight trajectories (expressed as BMI) overtime in community -dwelling older adults. The purpose of this study was to examine BMI trajectories over a 9 year period in initially well-functioning older men and women using group-based trajectory modeling. Additionally, we investigated the relationship between BMI trajectories with contemporaneous changes in lean mass and physical function. We hypothesized that men and women who lose weight at a faster rate will lose relatively more lean mass and physical function compared to participants who lose weight at the lowest rate.
METHODS
Study population
The Health, Aging, and Body Composition (Health ABC) Study is a prospective longitudinal study of 3,075 community-dwelling initially well-functioning black and white men and women initially aged 70–79 as previously published [9]. Participants were recruited from a random sample of white Medicare beneficiaries and all age-eligible black residents from the Memphis, TN, and Pittsburgh, PA areas . Participants were eligible if they reported no difficulty in walking a quarter of mile, walking up 10 steps without resting or performing mobility-related activities of daily living. Exclusion criteria were a history of active cancer treatment in the prior 3 years, planned to move out of the study area in the next 3 years, or current participation in a lifestyle intervention. Baseline data was collected between April 1997 and June 1998. Clinic visits were repeated annually for 10 years, with the exception of years 7 and 9. The study was approved by the institutional review boards of the study sites and the coordinating center ;written informed consent was obtained from all participants. For our analyses, only participants with 3 measures of BMI over the 9-year period(n= 2755), and with baseline and Year 10 measurements of lean mass and physical function were included (n=1019). Of those, we excluded participants with missing data on covariates (n=21), resulting in a final sample of 99 8. Excluded participants were older, more likely to be black, less educated, more likely to be former or current smokers, less physically active, had more comorbidities, and lower baseline gait speed, grip and leg strength. BMI was higher among excluded women but did not differ between included and excluded men (P <0.05 for all).
Assessment of body composition
BMI was calculated from body weight measured annually with a standard balance beam scale and body height was measured at year 1 using a Harpenden stadiometer (Holtain Ltd, Crosswell, UK). Total lean mass(excluding bone mineral content) was determined at baseline and at year 10 from total body scans using fan-beam dual energy X-ray absorptiometry (Hologic QDR 4500A; Hologic, Bedford, MA). Appendicular lean mass was calculated as the sum of lean mass of arms and legs (kg). The validity and reproducibility of the dual energy X -ray absorptiometry scanner have been reported previously [10, 11].
Assessment of physical function
Physical function was assessed at baseline and Year 10 from gait speed, grip strength and leg strength. Usual 20 meter gait speed (m/s) was determined during the first lap of the 400 meter Long Distance Corridor Walk [12]. Participants were allowed to use walking aids during the test, such as canes or walkers, if needed. Grip strength (dominant hand (kg)) was assessed using a Jamar dynamometer (Sammons Preston Rolyan, Bolingbrook, IL) [13]. The maximum strength of two trials was analyzed. Leg strength was based on knee extension strength, which was measured concentrically at 60 degrees/second on an isokinetic dynamometer (Kin-Com dynamometer, 125 AP; Chattanooga, TN). The right leg was tested unless there was a contraindication such as joint replacement or knee pain (n=10 at baseline, n= 52 at Year 10). The maximum muscle torque (Newton meters (Nm)) was selected from the three reproducible and acceptable trials from a maximum of six.
Covariates
Demographic characteristics (age, sex, race, study site and education), smoking status (never, current, or former) and physical activity (kilocalories/kg/week) of all self-reported activity in the week prior to baseline [14]were ascertained by an interviewer -administered questionnaire at baseline. Prevalent hypertension, diabetes, cardiovascular disease(percutaneous transluminal coronary angioplasty, angina, myocardial infarction, bypass surgery, stroke, TIA, cerebral vascular accident), heart failure, edema and cancer were determined from self-report, medication use, and clinical assessments which were similar to the Cardiovascular Health Study [15].
Statistical analysis
Because of differences with regard to body composition [16]and physical performance [17], analyses were stratified by sex. Trajectories were estimated with a group-based trajectory modeling [18, 19]using proc traj for STATA. The trajectories were derived by modeling BMI as a function over time, (participants’ age at each follow-up measurement). The best fitting model was based on the Bayesian Information Criterion and the presence of a minimum of 5% of participants per trajectory to ensure stable estimates per trajectory[ 6, 8]. After the number of trajectories was defined, non-significant quadratic and cubic terms were removed, but linear parameters stayed in the model, regardless of significance. Posterior probabilities of group membership were estimated to assess the adequacy of the selected model [6]. Specifically, higher probability values indicate higher likelihood that an individual’s trajectory pattern fits within the broader trajectory group. The posterior probability of allocating each participant into the BMI trajectory groups was greater than 0.97, indicating a good fit of the models. A Wald test was performed to determine whether slopes of trajectories were significantly different.
Linear regression analyses were conducted to examine trends across trajectories for continuous variables. For categorical variables, chi-square tests were performed . The absolute and relative changes (%) between Year 1 and Year 10 of BMI , lean mass and physical function were calculated. Multivariable linear regression analyses were used to determine the association of BMI trajectories with relative change in lean mass and physical function. Unstandardized regression coefficients (B) and 95% confidence intervals (CI) were reported for each BMI trajectory after adjustment for covariates. Model 1 was adjusted for age, race, study site and education. Model 2 was additionally adjusted for smoking status, physical activity, hypertension, diabetes, cardiovascular disease, heart failure, edema, and cancer. Trajectory 1 (participants with the lowest mean BMI over time) was considered the reference group. Because adjustment for hospitalization did not attenuate associations in both men and women, it was not included in the model. All P-values are two-tailed (α=0.05). Data were analyzed with STATA version 12.1.
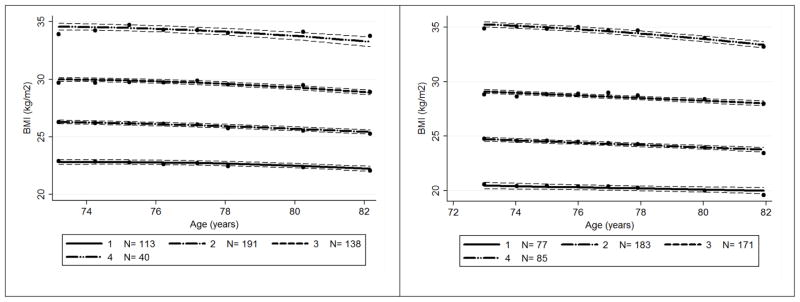
RESULTS
We identified four BMI trajectories for 482 men and 516 women. Baseline demographics, lifestyle factors and comorbidities are presented per trajectory in table 1. All trajectories among men followed a quadratic relationship (Figure 1). The absolute change over the 9 year period (mean±SD) in BMI among men was −0.85±1.94, −1.02±1.92, −0.79±2.46, and −0.15±2.48 for trajectory 1, 2, 3 and 4, respectively. However, the slopes were not significantly different between trajectories groups (P=0.260). Among women, the lowest three trajectories followed a linear relationship, while trajectory 4 followed a quadratic relationship (Figure 1). Change in BMI was −1.00±1.67, −1.31±2.22, −0.81±2.44, and −1.75±3.27 for BMI trajectory 1, 2, 3 and 4. The slopes of trajectories were significantly different between groups (P=0.031).
Table 1.
Baseline Characteristics of 482 Men and 516 Women according to BMI Trajectories
| BMI trajectories
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Men | Women | |||||||||
|
|
||||||||||
| 1 | 2 | 3 | 4 | P-for trend | 1 | 2 | 3 | 4 | P-for trend | |
| Trajectory group, n (%) | 113 (23.3) | 191 (39.8) | 138 (28.5) | 40 (8.4) | 77 (15.1) | 183 (34.9) | 171 (33.6) | 85 (16.4) | ||
| Age (years) | 73.5 ± 2.7 | 73.4 ± 2.8 | 72.9 ± 2.7 | 72.6 ± 2.5 | 0.040 | 73.3 ± 2.9 | 73.2 ± 2.8 | 72.8 ± 2.6 | 72.8 ± 2.7 | 0.149 |
| Race, white, n (%) | 80 (71) | 149 (78) | 92 (67) | 26 (65) | 0.093 | 61 (79) | 140 (77) | 89 (52) | 28 (33) | <0.001 |
| Site, Memphis, n (%) | 65 (58) | 89 (47) | 64 (46) | 20 (50) | 0.252 | 47 (61) | 102 (56) | 81 (47) | 42 (49) | 0.162 |
| BMI at year 1 (kg/m2) | 22.9 ± 1.58 | 26.3 ± 1.28 | 29.7 ± 1.70 | 33.9 ± 2.27 | <0.001 | 20.5 ± 1.64 | 24.8 ± 1.51 | 28.8 ± 1.72 | 34.9 ± 3.01 | <0.001 |
| BMI at year 10 (kg/m2) | 22.0 ± 2.00 | 25.3 ± 1.66 | 28.9 ± 1.90 | 33.8 ± 3.07 | <0.001 | 19.5 ± 1.84 | 23.4 ± 1.88 | 28.0 ± 2.34 | 33.2 ± 3.36 | <0.001 |
| BMI change (kg/m2) | −0.85 ± 1.94 | −1.02 ± 1.92 | −0.79 ± 2.46 | −0.15 ± 2.48 | 0.054 | −1.00 ± 1.67 | −1.31 ± 2.22 | −0.81 ± 2.44 | −1.75 ± 3.27 | 0.143 |
| Education level, n (%) | 0.399 | 0.520 | ||||||||
| Less than high school | 15 (13) | 32 (17) | 31 (22) | 7 (18) | 9 (11) | 28 (15) | 32 (19) | 16 (19) | ||
| High school graduate | 26 (23) | 48 (25) | 39 (29) | 10 (25) | 27 (35) | 70 (38) | 64 (37) | 37 (44) | ||
| Postsecondary | 75 (64) | 111 (58) | 68 (49) | 23 (58) | 41 (53) | 85 (46) | 75 (44) | 32 (38) | ||
| Smoking status, n (%) | 0.314 | 0.017 | ||||||||
| Never | 44 (39) | 69 (36) | 47 (34) | 10 (25) | 52 (68) | 109 (60) | 106 (62) | 53 (62) | ||
| Current | 12 (11) | 14 (7) | 10 (7) | 1 (3) | 10 (13) | 12 (7) | 6 (4) | 2 (2) | ||
| Former | 57 (50) | 108 (57) | 81 (59) | 29 (73) | 15 (19) | 62 (34) | 59 (35) | 30 (35) | ||
| Physical activity (kcal/kg/week) | 95 ± 84 | 92 ± 69 | 88 ± 63 | 83 ± 97 | 0.346 | 90 ± 49 | 96 ± 74 | 100 ± 75 | 85 ± 60 | 0.793 |
| Hypertension, n (%) | 57 (50) | 119 (62) | 74 (54) | 1251 (63) | 0.150 | 26 (34) | 95 (52) | 110 (64) | 63 (74) | <0.001 |
| Diabetes, n (%) | 10 (9) | 21 (11) | 26 (19) | 5 (13) | 0.085 | 5 (6) | 10 (5) | 17 (10) | 13 (15) | 0.045 |
| Cardiovascular disease, n (%) | 23 (20) | 51 (27) | 31 (22) | 16 (40) | 0.077 | 4 (5) | 25 (14) | 19 (11) | 7 (8) | 0.195 |
| Coronary heart failure, n (%) | 12 (11) | 24 (13) | 20 (14) | 9 (23) | 0.279 | 5 (6) | 15 (8) | 17 (9) | 16 (19) | 0.031 |
| Edema, n (%) | 7 (6) | 16 (8) | 11 (8) | 7 (18) | 0.173 | 2 (3) | 6 (3) | 10 (6) | 7 (8) | 0.230 |
| Cancer, n (%) | 25 (21) | 31 (16) | 32 (23) | 10 (26) | 0.304 | 19 (25) | 43 (24) | 19 (11) | 10 (12) | 0.003 |
| Hospitalization, n (%) | 0.911 | 0.106 | ||||||||
| Never | 10 (9) | 19 (10) | 17 (12) | 4 (10) | 12 (16) | 43 (24) | 30 (18) | 20 (24) | ||
| 1–3 admissions | 63 (56) | 101 (53) | 63 (47) | 20 (50) | 49 (64) | 85 (47) | 88 (52) | 39 (46) | ||
| 4–5 admissions | 24 (21) | 36 (19) | 30 (22) | 9 (23) | 10 (13) | 29 (16) | 30 (18) | 8 (9) | ||
| 6 or more admissions | 16 (14) | 35 (18) | 28 (20) | 7 (18) | 6 (8) | 26 (14) | 23 (13) | 18 (22) | ||
Baseline characteristics are presented according to BMI trajectories which were derived by modeling BMI as a function over time. Continuous variables are reported as mean ± standard deviation. Linear regression analyses were used to calculate P-for trend values. For description of the trajectories, see text.
Figure 1.
BMI trajectories among participants from the Health, Aging, and Body Composition study during a 9 year follow-up.
Subheading – left side figure
Men
N=482
Subheading – right side figure
Women
N=516
The lines are the mean values of BMI and the dashed lines represent their 95% confidence intervals.
Table 2 depicts absolute and relative changes in lean mass and physical function and associations between trajectories with relative changes in lean mass and physical function. Compared to men in trajectory 1 (reference), men in the trajectory 4 had a significantly greater decrease in gait speed: −10.50 % (95% CI −15.74; −5.26) (P-for trend <0.001)(Model 2) . Men in the trajectory 4 lost relatively more leg strength compared to men trajectory 1: −8.37 % (−15.31; −1.42) (P-for trend=0.013) (Model 2). There were no significant differences between trajectories with relative change in grip strength or change in lean mass in men, nor was there a significant trend across trajectories. Women in the trajectory 4 lost relatively more lean mass in the arms compared to women in trajectory 1 (reference): −3.24 % (95% CI −6.18; −0.30) (Model 2). BMI trajectories were not associated with change in total appendicular lean mass or leg lean mass. No significant differences for physical function were observed between and across trajectories in women.
Table 2.
Associations between BMI Trajectories in Relation to Relative Changes from Baseline to the 9 year Follow up in Body Composition and Physical Function
| MEN | WOMEN | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||
| n | Absolute | Relative | Model 1 | Model 2 | n | Absolute | Relative | Model 1 | Model 2 | |
| Body composition | ||||||||||
| Total appendicular lean mass (kg) | ||||||||||
| Trajectory 1 | 113 | −1.29±1.57 | −5.8±7.1 | reference | reference | 77 | −0.44±0.86 | −3.1±6.0 | reference | reference |
| Trajectory 2 | 191 | −1.36±1.53 | −5.6±6.3 | −0.40 (−1.90; 1.10) | −0.45 (−1.95; 1.06) | 183 | −0.61±1.09 | −3.9±7.1 | −0.89 (−2.79; 1.01) | −0.85 (−2.80; 1.11) |
| Trajectory 3 | 138 | −1.33±1.91 | −4.9±7.1 | 0.40 (−1.21; 2.01) | 0.31 (−1.31; 1.93) | 171 | −0.64±1.30 | −3.5±7.2 | −0.45 (−2.41; 1.51) | −0.38 (−2.42; 1.67) |
| Trajectory 4 | 40 | −1.34±2.33 | −4.3±8.1 | 1.04 (−1.27; 3.36) | 1.24 (−1.11; 3.60) | 85 | −0.78±1.64 | −3.7±8.5 | −0.35 (−2.65; 1.94) | −0.15 (−2.56; 2.26) |
| P-for trend | 0.902 | 0.180 | 0.278 | 0.224 | 0.079 | 0.663 | 0.865 | 0.997 | ||
| Lean mass in the arms (kg) | ||||||||||
| Trajectory 1 | 113 | −0.45±0.50 | −7.3±8.1 | reference | reference | 77 | −0.12±0.22 | −3.4±6.3 | reference | reference |
| Trajectory 2 | 191 | −0.50±0.51 | −7.3±7.4 | −0.87 (−2.52; 0.77) | −0.97 (−2.64; 0.70) | 183 | −0.17±0.36 | −4.1±9.5 | −0.94 (−3.28; 1.39) | −0.98 (−3.39; 1.42) |
| Trajectory 3 | 138 | −0.53±0.62 | −7.0±8.0 | −0.56 (−2.33; 1.20) | −0.55 (−2.35; 1.24) | 171 | −0.19±0.41 | −4.0±9.5 | −1.07 (−3.48; 1.34) | −1.15 (−3.67; 1.37) |
| Trajectory 4 | 40 | −0.63±0.74 | −7.5±9.5 | −0.90 (−3.44; 1.65) | −0.67 (−3.28; 1.94) | 85 | −0.33±0.49 | −6.3±10.1 | −3.07 (−5.89; −0.25) | −3.19 (−6.16; −0.23) |
| P-for trend | 0.073 | 0.984 | 0.550 | 0.698 | <0.001 | 0.052 | 0.038 | 0.040 | ||
| Lean mass in the legs (kg) | ||||||||||
| Trajectory 1 | 113 | −0.85±1.18 | −5.2±7.3 | reference | reference | 77 | −0.31±0.75 | −2.9±7.0 | reference | reference |
| Trajectory 2 | 191 | −0.86±1.17 | −4.9±6.7 | −0.22 (−1.85; 1.41) | −0.25 (−1.88; 1.39) | 183 | −0.45±0.85 | −3.8±7.3 | −0.88 (−2.93; 1.16) | −0.83 (−2.93; 1.28) |
| Trajectory 3 | 138 | −0.80±1.43 | −4.1±7.5 | 0.78 (−0.97; 2.54) | 0.66 (−1.10; 2.42) | 171 | −0.46±0.98 | −3.3±7.3 | −0.27 (−2.38; 1.84) | −0.16 (−2.36; 2.04) |
| Trajectory 4 | 40 | −0.72±1.77 | −3.1±8.4 | 1.79 (−0.72; 4.31) | 2.00 (−0.56; 4.56) | 85 | −0.45±1.40 | −2.8±9.6 | 0.46 (−2.01; 2.93) | 0.74 (−1.85; 3.34) |
| P−for trend | 0.542 | 0.074 | 0.105 | 0.085 | 0.395 | 0.858 | 0.613 | 0.483 | ||
| Physical function | ||||||||||
| Gait speed (m/s) | ||||||||||
| Trajectory 1 | 113 | −0.37±0.23 | −23.5±14.2 | reference | reference | 77 | −0.37±0.20 | −25.5±12.1 | reference | reference |
| Trajectory 2 | 191 | −0.43±0.24 | −27.3±13.6 | −4.00 (−7.33; −0.67) | −3.58 (−6.94; −0.23) | 183 | −0.33±0.21 | −23.6±14.5 | 1.49 (−2.43; 5.41) | 2.33 (−1.68; 6.34) |
| Trajectory 3 | 138 | −0.36±0.24 | −23.7±14.7 | −1.12 (−4.70; 2.46) | −0.77 (−4.36; 2.83) | 171 | −0.33±0.22 | −24.1±15.6 | 0.22 (−3.82; 4.27) | 1.20 (−3.00; 5.39) |
| Trajectory 4 | 40 | −0.50±0.26 | −33.4±17.4 | −11.11(−16.26; −5.97) | −9.91 (−15.15; −4.67) | 85 | −0.31±0.22 | −25.2±16.7 | −1.11 (−5.84; 3.62) | −0.24 (−5.18; 4.70) |
| P-for trend | 0.018 | 0.001 | <0.001 | 0.001 | 0.075 | 0.978 | 0.539 | 0.813 | ||
| Grip strength (kg) | ||||||||||
| Trajectory 1 | 113 | −6.87±6.30 | −16.3±16.5 | reference | reference | 77 | −2.94±4.31 | −9.4±26.0 | reference | reference |
| Trajectory 2 | 191 | −6.19±6.48 | −14.4±16.2 | 0.97 (−2.88; 4.81) | 0.49 (−3.45; 4.35) | 183 | 3.56±4.65 | −12.8±18.0 | −3.99 (−9.92; 1.95) | −3.02 (−9.08; 3.04) |
| Trajectory 3 | 138 | −5.70±6.97 | −12.6±17.3 | 2.54 (−1.59; 6.68) | 2.42 (−1.76; 6.62) | 171 | −2.98±5.28 | −9.0±26.6 | −1.28 (−7.40; 4.85) | −0.01 (−6.35; 6.34) |
| Trajectory 4 | 40 | −7.00±6.67 | −15.2±16.5 | 0.07 (−5.86; 6.01) | −0.01 (−6.07; 6.06) | 85 | −3.34±4.79 | −11.2±18.2 | −3.63 (−10.79;3.54) | −3.04 (−10.51;4.43) |
| P-for trend | 0.979 | 0.586 | 0.846 | 0.841 | 0.789 | 0.876 | 0.472 | 0.609 | ||
| Leg strength (Nm) | ||||||||||
| Trajectory 1 | 113 | −36.8±27.4 | −26.1±21.9 | reference | reference | 77 | −19.7±14.9 | −24.9±22.4 | reference | reference |
| Trajectory 2 | 191 | −35.5±29.2 | −24.0±19.9 | −0.07 (−4.49; 4.35) | −0.44 (−4.91; 4.03) | 183 | −19.0±18.1 | −20.9±23.3 | 3.21 (−3.30; 9.73) | 3.94 (−2.68; 10.56) |
| Trajectory 3 | 138 | −41.0±33.7 | −26.1±20.9 | −2.46 (−7.21; 2.29) | −2.40 (−7.20; 2.41) | 171 | −22.4±23.6 | −22.5±24.5 | 0.70 (−6.03; 7.42) | 1.41 (−5.52; 8.34) |
| Trajectory 4 | 40 | −56.0±52.4 | −32.8±20.9 | −8.59 (−15.42;−1.76) | −8.63 (−15.62;−1.64) | 85 | −24.5±23.8 | −23.0±33.2 | 1.09 (−6.78; 8.95) | 1.83 (−6.32; 9.99) |
| P-for trend | <0.001 | 0.060 | 0.009 | 0.011 | 0.078 | 0.741 | 0.953 | 0.819 | ||
Model 1 was adjusted for age, race, study site, and education.
Model 2 was adjusted for model 1 plus smoking status, physical activity, hypertension, diabetes, cardiovascular disease, heart failure, edema, and cancer.
DISCUSSION
This study identified four distinctive BMI trajectories for both men and women over a period of 9 years. All trajectories were characterized by a decline in BMI. Participants with the highest mean BMI (trajectory 4) lost relatively more lean mass or had a greater decline in physical function over 9 years. However significant gender differences were observed. In men, there were no differences in relative loss in lean mass between the 4 trajectory groups. However, men in trajectory 4 had greater loss in leg strength and gait speed compared to men in trajectory 1. Conversely, women trajectory 4 lost relatively more lean mass in the arms than their counterparts in trajectory 1, but had no difference in physical function.
Duration and type of physical activity may explain the gender differences observed in this study. Results from the NHANES study showed that even though men and women reached similar activity counts per minute, older women had greater light-intensity activity than men, and spent more overall time in non-sedentary activity intensities compared to men [20]. While using self- report questionnaire data in this study, at baseline men were less physically active than women; 91±74 and 95±69 kcal/kg/week, respectively (Mann-Whitney test; p=0.06). Additionally, a nationally representative British birth cohort indicated gender differences in activity diversity and the levels of activity. Men more often reported greater intensity activities at early old age, yet changes in activity type may occur more among men than women with increasing age [21]. While women are more likely to report lighter-intensity activities such as household activities compared to men [22]. Little is known about house hold activities among older adults, and how they mightimpact changes in body composition and areas of lean tissue loss. More studies are warranted to investigate whether differences in type and duration of activities in older age might prevent loss in function.
Despite being an initially well -functioning cohort, all participants lost weight, lean mass and physical function. This is comparable with results from across -sectional study that showed that men and women aged 60–80 years become less physically active with age , which results in a reduction in physical function, e.g. 8-foot up and go or 2-minute step test [23]. In addition, recent findings from the Baltimore Longitudinal Study of Aging showed that physical activity counts, measured with an accelerometer, were 1.3% lower for each year increase in age, which was especially due to lower afternoon and evening activity in older individuals [24]. Although loss of function is a common occurrence of aging, our results show that loss of physical function varies by BMI trajectory with trajectory 1 most closely representing healthy aging.
Men in trajectory 4 had greater decline of gait speed and greater loss of leg strength compared to men in trajectory 1, which could not be explained by health or lifestyle variables. Our data indicates that the BMI with which a person enters into old age is an important determinant of the trajectory they follow in later life. The Health ABC study has previously shown that the onset of overweight and obesity in midlife or earlier contributes to an increased risk of incident mobility limitation [25]. Participants in trajectory 4 were obese (men; 33.9 kg/m2 (30.5–44.2), women 34.9 kg/m2(28.8 –46.1)) and therefore our findings are also in line with results of a recent meta - analyses that showed that obesity is associated with greater risk of functional decline in old age compared to normal weight/overweight [26]. Taken together, our results provide further evidence of the importance of preventing obesity before entering old age.
Strengths of our study first include the large study sample of community -dwelling black and white men and women were followed over 9 years. Second, we used group-based trajectory modeling to determine BMI trajectories which identified distinctive trajectories within the study population and enables us to investigate differences in participants’ characteristics within trajectories [27]. Third, the use of DXA provides an accurate measurement of appendicular lean mass; fourth, we assessed physical function using multiple indicators including gait speed, grip and leg strength. Finally, reverse causation was minimized in this study because participants were initially free from mobility disability. Some limitations need to be acknowledged. Though our statistical methods allowed us to investigate differences in lean mass and physical function changes by BMI trajectories, fewer people were allocated to trajectory1 and 4 , which might have resulted in low statistical power to detect differences between groups. Future larger studies, with a wider BMI range, are warranted. Of the 2,193 participants who were alive at follow-up, 998 participants (45.3%) with at least 3 measurements of BMI, data on change in lean mass and physical function, and complete data on baseline covariates were included in the analyses because we were interested in long-term weight change. This may have resulted in a healthier analytic sample. We observed differences in declines in lean mass and physical function, although the magnitude of change may be even greater among less-healthy populations, therefore observed associations are likely to be underestimated.
In conclusion, despite a well-functioning population at baseline, all BMI trajectories showed a decline over 9 years. Participants in BMI trajectory 4 had greater decreases in arm lean mass, and physical function, however, results differed by gender. Interestingly, the associations between BMI change and decline in physical function do not appear to be solely reflected by lean mass. Finally, the decline in BMI was modest and the rate of decline was not different among trajectory groups in men, suggesting that although BMI may change over time, those changes tend to be modest and the change in BMI does not depend on where you start. The weight a person enters old age is informative for predicting loss in lean mass or physical function which illustrates the importance of monitoring weight.
Acknowledgments
Funding sources: This research was supported by National Institute on Aging (NIA) Contracts N01-AG-6-2101; N01-AG-6-2103; N01-AG-6-2106; NIA grant R01-AG028050, and NINR Accepted for publication – 1/21/2015. May not be duplicated or reproduced without permission of the Journal of the American Geriatrics Society. grant R01-NR012459. This research was supported in part by the Intramural Research Program of the NIH, National Institute on Aging.
Footnotes
Conflict of Interest: The authors do not have any conflicts of interest to disclose.
Author Contributions: The authors’ contributions were as follows: Study was designed and conducted by Tamara B. Harrisand Denise K. Houston . Ilse Reinders performed statistical analyses and wrote the manuscript. Rachel A Murphy, Kathryn R. Martin, Ingeborg A Brouwer, Marjolein Visser, Daniel K. White, Anne B. Newman, Denise K. Houston Alka M. Kanaya, Daniel S. Nagin and Tamara B. Harris critically revised the manuscript. All authors had full access to all of the data in the study and approved the final manuscript. Ilse Reinders takes responsibility for the integrity of the data and the accuracy of data analysis.
Sponsor’s Role: None
Financial Disclosure: This research was supported by National Institute on Aging (NIA) Contracts N01-AG-6-2101; N01-AG-6-2103; N01-AG-6-2106; NIA grant R01-AG028050, and NINR grant R01-NR012459. This research was supported in part by the Intramural Research Program of the NIH, National Institute on Aging.
References
- 1.Kuk JL, Saunders TJ, Davidson LE, et al. Age-related changes in total and regional fat distribution. Ageing Res Rev. 2009;8:339–348. doi: 10.1016/j.arr.2009.06.001. [DOI] [PubMed] [Google Scholar]
- 2.Fried LP, Ferrucci L, Darer J, et al. Untangling the concepts of disability, frailty, and comorbidity: implications for improved targeting and care. J Gerontol A Biol Sci Med Sci. 2004;59:255–263. doi: 10.1093/gerona/59.3.m255. [DOI] [PubMed] [Google Scholar]
- 3.Lee JS, Visser M, Tylavsky FA, et al. Weight loss and regain and effects on body composition: the Health, Aging, and Body Composition Study. J Gerontol A Biol Sci Med Sci. 2010;65:78–83. doi: 10.1093/gerona/glp042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Beavers KM, Beavers DP, Nesbit BA, et al. Effect of an 18 -month physical activity and weight loss intervention on body composition in overweight and obese older adults. Obesity (Silver Spring) 2013:325–331. doi: 10.1002/oby.20607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chaston TB, Dixon JB, O'Brien PE. Changes in fat-free mass during significant weight loss: a systematic review. Int J Obes (Lond) 2007;31:743–750. doi: 10.1038/sj.ijo.0803483. [DOI] [PubMed] [Google Scholar]
- 6.Nagin DS. Group-based Modeling of Development. Cambridge, MA: Harvard University Press; 2005. [Google Scholar]
- 7.Nagin DS, Odgers CL. Group-based trajectory modeling in clinical research. Annu Rev Clin Psychol. 2010;6:109–138. doi: 10.1146/annurev.clinpsy.121208.131413. [DOI] [PubMed] [Google Scholar]
- 8.Nagin DS. Analyzing developmental trajectories: A semiparametric, group-based approach. Psychological Methods. 1999;4:139–157. doi: 10.1037/1082-989x.6.1.18. [DOI] [PubMed] [Google Scholar]
- 9.Simonsick EM, Newman AB, Nevitt MC, et al. Measuring higher level physical function in well-functioning older adults: expanding familiar approaches in the Health ABC study. J Gerontol A Biol Sci Med Sci. 2001;56:M644–649. doi: 10.1093/gerona/56.10.m644. [DOI] [PubMed] [Google Scholar]
- 10.Visser M, Fuerst T, Lang T, et al. Validity of fan-beam dual-energy X-ray absorptiometry for measuring fat-free mass and leg muscle mass. Health, Aging, and Body Composition Study--Dual-Energy X-ray Absorptiometry and Body Composition Working Group. J Appl Physiol. 1999;87:1513–1520. doi: 10.1152/jappl.1999.87.4.1513. [DOI] [PubMed] [Google Scholar]
- 11.Salamone LM, Fuerst T, Visser M, et al. Measurement of fat mass using DEXA: a validation study in elderly adults. J Appl Physiol. 2000;89:345–352. doi: 10.1152/jappl.2000.89.1.345. [DOI] [PubMed] [Google Scholar]
- 12.Simonsick EM, Montgomery PS, Newman AB, et al. Measuring fitness in healthy older adults: the Health ABC Long Distance Corridor Walk. J Am Geriatr Soc. 2001;49:1544–1548. doi: 10.1046/j.1532-5415.2001.4911247.x. [DOI] [PubMed] [Google Scholar]
- 13.Harkonen R, Harju R, Alaranta H. Accuracy of the Jamar dynamometer. J Hand Ther. 1993;6:259–262. doi: 10.1016/s0894-1130(12)80326-7. [DOI] [PubMed] [Google Scholar]
- 14.Brach JS, Simonsick EM, Kritchevsky S, et al. The association between physical function and lifestyle activity and exercise in the health, aging and body composition study. J Am Geriatr Soc. 2004;52:502–509. doi: 10.1111/j.1532-5415.2004.52154.x. [DOI] [PubMed] [Google Scholar]
- 15.Fried LP, Borhani NO, Enright P, et al. The Cardiovascular Health Study: design and rationale. Ann Epidemiol. 1991;1:263–276. doi: 10.1016/1047-2797(91)90005-w. [DOI] [PubMed] [Google Scholar]
- 16.Nindl BC, Scoville CR, Sheehan KM, et al. Gender differences in regional body composition and somatotrophic influences of IGF-I and leptin. J Appl Physiol. 2002;92:1611–1618. doi: 10.1152/japplphysiol.00892.2001. [DOI] [PubMed] [Google Scholar]
- 17.Tseng LA, Delmonico MJ, Visser M, et al. Body Composition Explains Sex Differential in Physical Performance Among Older Adults. J Gerontol A Biol Sci Med Sci. 2014;69:93–100. doi: 10.1093/gerona/glt027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jones BL, Nagin DS. Advances in group-based trajectory modeling and an SAS procedure for estimating them. Sociological Methods & Research. 2007;35:542–571. [Google Scholar]
- 19.Jones BL, Nagin DS. A Note on a Stata Plugin for Estimating Group-based Trajectory Models. Sociological Methods & Research. 2013;42:608–613. [Google Scholar]
- 20.Martin KR, Koster A, Murphy RA, et al. Changes in Daily Activity Patterns with Age in U.S. Men and Women: National Health and Nutrition Examination Survey 2003–04 and 2005–06. J Am Geriatr Soc 2014; 21. Martin KR, Cooper R, Harris TB et al. Patterns of leisure-time physical activity participation in a British birth cohort at early old age. PLoS One. 2014;9:e98901. [Google Scholar]
- 22.Tudor-Locke C, Johnson WD, Katzmarzyk PT. Frequently reported activities by intensity for U.S. adults: the American Time Use Survey. Am J Prev Med. 2010;39:e13–20. doi: 10.1016/j.amepre.2010.05.017. [DOI] [PubMed] [Google Scholar]
- 23.Milanovic Z, Pantelic S, Trajkovic N, et al. Age-related decrease in physical activity and functional fitness among elderly men and women. Clin Interv Aging. 2013;8:549–556. doi: 10.2147/CIA.S44112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schrack JA, Zipunnikov V, Goldsmith J, et al. Assessing the "physical cliff": detailed quantification of age-related differences in daily patterns of physical activity. J Gerontol A Biol Sci Med Sci. 2014;69:973–979. doi: 10.1093/gerona/glt199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Houston DK, Ding J, Nicklas BJ, et al. Overweight and obesity over the adult life course and incident mobility limitation in older adults: the health, aging and body composition study. American Journal of Epidemiology. 2009;169:927–936. doi: 10.1093/aje/kwp007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schaap LA, Koster A, Visser M. Adiposity, Muscle Mass, and Muscle Strength in Relation to Functional Decline in Older Persons. Epidemiol Rev. 2013;35:51–65. doi: 10.1093/epirev/mxs006. [DOI] [PubMed] [Google Scholar]
- 27.Jones BL, Nagin DS. A Stata Plugin for Estimating Group-Bases Trajectoriy Models. 2012. [Google Scholar]