Abstract
Background
Although most people who inject drugs (PWID) in Tijuana, Mexico, primarily inject heroin, injection and non-injection use of methamphetamine and cocaine is common. We examined patterns of polydrug use among heroin injectors to inform prevention and treatment of drug use and its health and social consequences.
Methods
Participants were PWID residing in Tijuana aged ≥ 18 years who reported heroin injection in the past 6 months and were recruited through respondent driven sampling (n=1025). Latent class analysis was conducted to assign individuals to classes on a probabilistic basis, using four indicators of past 6 month polydrug and polyroute use: cocaine injecting, cocaine smoking or snorting, methamphetamine injecting, methamphetamine smoking or snorting. Latent class membership was regressed onto covariates in a multinomial logistic regression.
Results
Latent class analyses testing 1, 2, 3, and 4 classes were fit, with the 3-class solution fitting best. Class 1 was defined by predominantly heroin use (50.2%, n=515); class 2 by methamphetamine and heroin use (43.7%, n=448), and class 3 by methamphetamine, cocaine, and heroin use (6.0%, n=62). Bivariate and multivariate analyses indicated a group of methamphetamine and cocaine users that exhibited higher risk sexual practices and lower heroin injecting frequency, and a group of methamphetamine users who were younger and more likely to be female.
Conclusions
Discrete subtypes of heroin PWID were identified based on methamphetamine and cocaine use patterns. These findings have identified subtypes of heroin injectors who require more tailored interventions to reduce the health and social harms of injecting drug use.
Keywords: polydrug use, latent class analysis, HIV risk, Tijuana, people who inject drugs
Introduction
Use of multiple illicit substances, either over a short period or at the same time, has been associated with greater drug dependence, increased risk for overdose, and behaviors that are associated with increased risk for HIV and related infections. Motivations for polydrug use include preference for specific pharmacological effects, experimentation, availability of different drugs at different times, replacing use of one drug with another, and seeking stronger effects from drugs as tolerance increases (Brecht et al., 2008; EMCDDA 2009; Monga et al. 2007).
Tijuana, Mexico, is located on a major drug trafficking route and is unique as a city where heroin, and to a lesser extent, cocaine and methamphetamine are commonly injected. Heroin in this region is usually in the form of black tar, which is typically injected. On the contrary, white/brown powder, which is more prevalent in other regions, is more easily used through smoking and snorting (Bucardo et al., 2005). Methamphetamine has become a major drug of abuse in Tijuana (Brouwer et al., 2006; Case et al., 2008) and is closely associated with unprotected sex and increased risk of acquiring HIV and other sexually transmitted diseases (Drumright et al., 2006). Among people who inject drugs (PWID), it has also been associated with higher risk of needle and syringe sharing (Rusch et al., 2009). Cocaine is also associated with high risk sexual behavior (Brouwer et al., 2008). Heroin is often injected in combination with methamphetamine or cocaine (i.e., “speedball”) which increases the risk of overdose and drug dependence, as well as high risk sexual risk behaviors.
Latent class analysis assigns individuals to classes on a probabilistic basis based on responses to a set of indicator variables, allowing comparison of covariates across classes. It approaches and groups observations based on similarity, with the goal of dividing a heterogeneous population into more homogenous subgroups (Flaherty & Kiff, 2012). This method has been used to model patterns of substance use in general population samples (Agrawal et al. 2007; Cleveland et al., 2010; Lynskey et al. 2006) as well as high risk drug using populations (Carlson et al. 2005; Harrell et al. 2012; Kuramoto et al. 2011; Monga et al. 2007; Patra et al. 2009; Roy et al. 2013). Although specific drugs and route of administration varied by population and region, all studies found multiple classes of polydrug use, defined by single drug use, pairs of drug use, route of administration, and level of use. For example, in a sample of inner city heroin and cocaine users in Baltimore, Maryland, Kuramoto et al. (2011) identified five classes based on responses to eight indicators of single drug use, with significant differences between classes in depressive symptoms and injection risk. In another sample of heroin and cocaine users in Baltimore, Harrell et al. (2013) identified three classes based on responses to eight different indicators and significant differences between classes in HIV and Hepatitis C (HCV) risk behaviors. Additionally, in a sample of opioid users in five Canadian cities, Monga et al. (2007) identified three classes based on responses to twelve indicators and significant differences between classes in homelessness and HIV and HCV infection prevalence.
Due to different drug availability and contextual factors, drug use profiles of PWIDs in Tijuana are likely to be quite different than those of heroin and opioid users in other parts of North America. The objective of this analysis was to identify classes of polydrug use among heroin users in Tijuana Mexico, and to in turn compare these classes with respect to the HIV risk behaviors associated with each. In this analysis, we applied latent class analysis to describe subgroups or classes of cocaine and methamphetamine injecting and non-injecting polydrug use in a sample of heroin PWID. It was hypothesized that individuals in classes with more polydrug use would report more HIV risk behaviors.
Methods
Study Participants
Participants were PWID enrolled from 2006 to 2007 in a prospective study examining contextual and behavioral risk factors for HIV, syphilis, and tuberculosis infection as previously described (Strathdee et al. 2008). At baseline, eligibility criteria included having injected in the past 30 days, being aged 18 years or older, speaking Spanish or English, and residing in Tijuana with no plans to move over the next 18 months.
Participants were recruited by respondent driven sampling to access a more representative sample of this hard-to-reach population (Heckathorn, 1997). Thirty-two initial “seeds” were selected by local outreach workers (heterogeneous on age, gender, drug preference, and neighborhood) and given unique coupons to refer peers who injected drugs to the study. Eligible peers who enrolled in the study were then given the same number of coupons to recruit additional peers who injected drugs. From the initial group, 24 seeds recruited eligible peers. Additional information on recruitment procedures, tolerance, sample convergence, recruitment chains, and sample characteristics has previously been reported (Brouwer et al., 2012; Rudolph et al., 2014; Strathdee et al., 2008). Participants completed a quantitative survey and underwent testing for HIV, TB, and syphilis at baseline and every six months thereafter for three years (N=1,056). In order to examine polydrug use among heroin injectors, this analysis was restricted to the majority of this sample who reported heroin injection in the past six months prior to baseline (N=1,025). Of note, all 24 seeds were included in the analyses presented here.
Participants provided informed consent and were given pre- and post-test HIV counseling; those testing HIV-positive were referred to local public health providers for free care. Those with syphilis titers ≥ 1:8 were referred to health centers for care. The Ethics Board of Tijuana General Hospital and the Institutional Review Board of University of California San Diego approved this study.
Measures
The survey included questions about demographics, substances used, frequency of use, route of administration, sexual behaviors, and drug use history and behaviors. Regarding substances used, participants were first asked if they have ever used a substance, and in the case of affirmative responses, they were asked to indicate the frequency of use of that substance in the past six months by route of administration (injecting, smoking, or snorting). Frequency of substance use was dichotomized into yes or no for past six month use of cocaine or methamphetamine. Due to smaller prevalence and different risks from injecting, use via snorting and smoking was combined into non-injection use, resulting in four indicators of past six month polydrug use: methamphetamine injecting, methamphetamine non-injecting, cocaine injecting, and cocaine non-injecting.
Demographic factors included age, gender, education, income, homelessness, deportation history, and being born in Tijuana. Education level was dichotomized as incompletion or completion of secondary school. Income level was dichotomized from an eight level categorical scale to greater than or equal to vs. less than 3500 pesos per month (about $335 USD in 2006).
Sexual behaviors in the past six months included reporting sex in exchange for something (e.g., money, food, drugs), any use of illicit drugs before or during sex and number of casual sex partners, dichotomized as 0–1 or 2 or more.
Drug use behaviors included frequency of heroin injection in the past 6 months, years since first injection, overdose in the past year, receptive needle sharing, and distributive needle sharing. Frequency of heroin injection was dichotomized into more than once a day versus once a day or less. Years since first injection was calculated by subtracting the age of first reported injection from the participant’s reported age.
Statistical Analyses
A latent class analysis was conducted to assign individuals to classes on a probabilistic basis, using four indicators of past six month polydrug use: (1) cocaine injecting, (2) cocaine smoking or snorting, (3) methamphetamine injecting, and (4) methamphetamine smoking or snorting.
The latent class analysis was conducted in Mplus version 7.0 (Muthén & Muthén 1998–2012). Models fit to 1, 2, 3, and 4 classes were run and compared using statistical fit indices of Akaike’s information criteria (AIC), sample size adjusted Bayesian information criteria (sBIC), and Lo-Mendell Rubin Test (LMRT), and descriptive fit index of entropy (Flahery & Kiff 2012; Roesch et al. 2010). The best fitting model was selected based on smallest AIC and sBIC, significant LMRT (p < .05), and highest entropy.
Participants were then assigned to classes based on their most likely class membership and Chi-square tests and ANOVAs were conducted in SPSS version 22.0 (IBM Corp. 2013) to detect differences between classes among categorical and continuous risk factors, respectively. Next, several multinomial logistic regression models were fit with the polydrug use latent classes as the outcome variable. Covariates selected for model inclusion were demographic, sexual behavior, and drug use behavior covariates that had significant associations with the polydrug use latent classes in bivariate analyses (p <.05).
To better understand the unique and shared impact of demographics, sex behaviors, and drug use behaviors, three separate models were run with each set of covariates regressed onto the latent class outcome. Significant covariates (p <.05) were carried forward, and a comprehensive multinomial logistic regression was run with significant covariates from each of the three categories regressed onto the latent class outcome.
Peer recruitment through respondent driven sampling may introduce dependence between observations, as participants may tend to recruit others who are similar on given traits of interest. To account for this recruitment homophily on polydrug use class, Model 2 controlled for each participant’s recruiter’s polydrug use class. Additionally, to account for the increased similarity among individuals in the same recruitment chain compared with those in different chains, Model 2 used a generalized estimation equation approach (like the approach used by Rudolph et al. 2014) which clustered on recruitment chain membership in STATA 10 (StataCorp 2007).
Finally, a sub-analysis was run examining simultaneous co-injection of substances. Prevalence of co-injection use was assessed for each class and chi-squared tests of association were run between co-injection and drug and sex risk behaviors.
Results
Among the 1025 participants, 85.5% were male and the median age was 36.6 years. Less than half (41.5%) had completed secondary school and less than half (43.1%) had a monthly income of over 3500 pesos (about US $335). Baseline prevalence of HIV was 4.0%. In the past 6 months, 9.1% reported cocaine injection, 7.4% reported non-injection use of cocaine, 33.7% reported methamphetamine injection, and 38.8% reported non-injection use of methamphetamine.
Latent Class Analysis
Latent class analyses testing 1, 2, 3, and 4 classes were fit to the data. All fit indices (AIC, sBIC, LMRT, and Entropy) indicated that the 3-class solution fit better than the 1- 2- and 4-class solutions [Table 1]. Latent class probabilities for each class were 50.2% (n = 515) in class 1, 43.7% (n = 448) in class 2, and 6.0% (n = 62) in class 3.
Table 1.
Latent class analyses fit indices for 1–4 classes (n = 1,025)
| AIC | sBIC | LMRT (p-value) | Entropy | |
|---|---|---|---|---|
| Class 1 | 3389 | 3396 | NA | NA |
| Class 2 | 3132 | 3147 | <.0001 | 0.632 |
| Class 3 | 3089 | 3113 | <.0001 | 0.855 |
| Class 4 | 3093 | 3127 | 0.2398 | 0.768 |
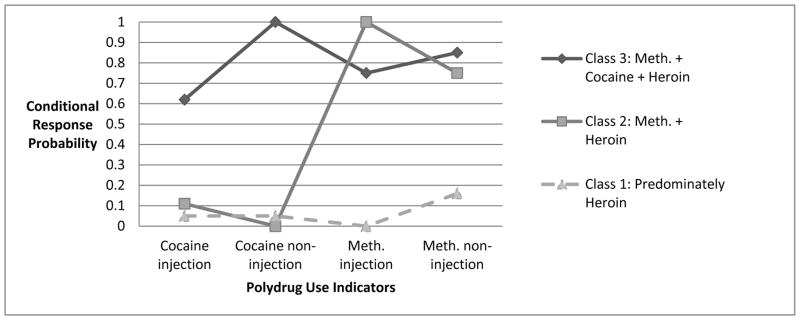
Class 1 was characterized by low probabilities of all four polydrug use indicators (0-.16) and so will be referred to hereafter as “predominantly heroin” use. Class 2 had high probabilities of methamphetamine injection and non-injection (1.00 and .75) but low probabilities of cocaine injection and cocaine non-injection (0 and .11), and will be referred to hereafter as the “methamphetamine” using class of heroin injectors. Class 3 had high probabilities (.62–1.00) of all methamphetamine and cocaine polydrug use indicators and will be referred to hereafter as the “methamphetamine and cocaine” using class of heroin injectors. [Figure 1] Descriptive statistics of demographics and risk behaviors for the sample and by latent class are presented in Table 2.
Figure 1.
Polydrug use profiles by class membership based on conditional response probabilities from the 3 class model (n = 1025)
Table 2.
Comparison of drug use indicators, demographics, sex behaviors, and drug use behaviors among PWID in Tijuana (n = 1,025)
| Total (%) | Class 1: No Polydrug Use (Predominately Heroin) n=515 (%) | Class 2: Meth-amphetamine + Heroin n=448 (%) | Class 3:Meth-amphetamine + Cocaine + Heroin n= 62 (%) | |
|---|---|---|---|---|
| Drug Use Indicators | ||||
|
| ||||
| Cocaine injection | 96 (9.1) | 21 (4.1) | 42 (9.4) | 28 (45.2) |
| Cocaine non-injection | 78 (7.4) | 17 (3.3) | 0 (0.0) | 60 (96.8) |
| Methamphetamine injection | 356 (33.7) | 0 (0.0) | 313 (69.9) | 30 (48.4) |
| Methamphetamine non-injection | 410 (38.8) | 48 (9.3) | 303 (67.6) | 48 (77.4) |
|
| ||||
| Demographics | ||||
|
| ||||
| Age, Mean (SD)* | 36.6 (8.39) | 38.1 (8.40) | 34.9 (8.04) | 37.8 (8.28) |
| Male* | 876 (85.5) | 460 (89.3) | 367 (81.9) | 49 (79.0) |
| Female* | 149 (14.5) | 55 (10.7) | 81 (18.1) | 13 (21.0) |
| Income over 3500 pesos* | 442 (43.1) | 244( 48.4) | 172 (39.4) | 26 (43.3) |
| Secondary school* | 426 (41.5) | 222 (43.1) | 171 (38.2) | 33 (53.2) |
| Homeless | 126 (12.3) | 63 (12.2) | 54 (12.1) | 9 (14.5) |
| Born in Tijuana | 232 (22.6) | 118 (22.9) | 99 (22.1) | 15 (24.2) |
| Deported to Tijuana | 402 (39.2) | 210 (40.8) | 171 (38.2) | 21 (33.9) |
|
| ||||
| Sex behaviors | ||||
|
| ||||
| Sex exchange* | 107 (10.8) | 48 (9.3) | 43 (9.6) | 16 (25.8) |
| 2+ Casual Sex Partners* | 141 (13.7) | 53 (10.3) | 64 (14.3) | 24 (38.7) |
| Drug use before sex* | 164 (15.9) | 60 (11.7) | 82 (18.4) | 22 (35.5) |
|
| ||||
| Disease prevalence | ||||
|
| ||||
| HIV | 41 (4.0) | 18 (3.5) | 22 (4.9) | 1 (1.6) |
| Syphilis | 79 (7.7) | 35 (6.8) | 39 (8.8) | 5 (8.1) |
|
| ||||
| Drug use behaviors | ||||
|
| ||||
| Daily+ Heroin Injecting* | 937 (91.3) | 478 (92.8) | 407 (90.9) | 52 (83.9) |
| Years Injecting, Mean (SD)* | 15 (9.09) | 16.2 (9.39) | 13.7 (8.44) | 15.9 (9.65) |
| Past 6 Month Overdose* | 75 (7.4) | 24 (4.7) | 41 (9.2) | 10 (16.1) |
| Receptive Syringe Sharing* | 602 (58.8) | 246 (47.8) | 313 (69.9) | 43 (69.4) |
| Distributive Syringe Sharing* | 630 (61.4) | 264 (51.3) | 320 (71.4) | 46 (74.2) |
|
| ||||
| Simultaneous injecting use | ||||
|
| ||||
| Speedball (Heroin/Cocaine)* | 120 (11.7) | 30 (5.8) | 64 (14.3) | 26 (41.9) |
| Methamphetamine/Cocaine* | 27 (2.6) | 2 (.4) | 16 (3.6) | 9 (14.5) |
| Methamphetamine/Heroin* | 546 (53.3) | 181 (35.1) | 327 (73.0) | 38 (61.3) |
p<.05,
PWID: People Who Inject Drugs
Correlates of Polydrug Use Class Membership
Despite their increased duration of injecting and more frequent injection of heroin, those using predominantly heroin (class 1) shared syringes less (class 1: 47.8%; class 2: 69.9%; class 3: 69.4%) and have reported fewer overdoses (class 1: 4.7%; class 2: 9.2%; class 3: 16.1%). [Table 2] Those in class 1 were also more likely to be male, older, have higher income, and engage in less risky sexual behaviors. Compared to those using predominately heroin, those in the heroin and methamphetamine use class (class 2) were significantly more likely to be female, to use drugs before sex, and to inject with syringes that had previously been used by others. They were also significantly younger and had lower monthly incomes. Compared with predominately heroin users, those using methamphetamine, cocaine and heroin (class 3) were significantly more likely in the past six months to have multiple casual sex partners, to participate in sex exchange, to report a prior overdose, to inject with syringes that had previously been used by others and they were less likely to report daily heroin injection. Interestingly, this group had higher levels of education and fewer individuals reporting injection of heroin more than once per day (class 3: 83.9%; class 1: 92.8%; class 2: 90.9%).
Multivariate Analysis
After adjustment for all covariates significant at p < .05 (Model 1), those using methamphetamine and heroin (class 2) differed from those using predominantly heroin in that they were slightly younger, were more likely to be female, have lower incomes, and report more receptive syringe sharing. After adjustment, those using methamphetamine, cocaine, and heroin (class 3) were more likely than those using predominantly heroin to report sex exchange involvement, multiple casual sex partners, > daily heroin injection, sharing syringes, and having previously overdosed. [Table 3]
Table 3.
Adjusted association of most likely class membership with demographics, sex behaviors, and drug use behaviors among PWID in Tijuana (n = 1,025)
| Model 1 | Model 2: Adjusting for Homophily | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Methamphetamine + Heroin Use vs. Predominately Heroin Use | Methamphetamine + Cocaine + Heroin Use vs. Predominately Heroin Use | Methamphetamine + Heroin Use vs. Predominately Heroin Use | Methamphetamine + Cocaine + Heroin Use vs. Predominately Heroin Use | |||||
|
| ||||||||
| AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | |
| Age | 0.97 | 0.94–0.99 | 1.02 | 0.98–1.07 | 0.97 | 0.95–0.98 | 1.01 | 0.97–1.05 |
| Female | 1.89 | 1.24–2.99 | 1.30 | 0.52–2.94 | 1.81 | 1.31–2.49 | 1.25 | 0.75–2.08 |
| Income ≥ 3500 pesos/month | 0.62 | 0.48–0.83 | 0.70 | 0.41–1.30 | 0.65 | 0.47–0.89 | 0.75 | 0.51–1.08 |
| Sex exchange | 0.80 | 0.48–1.30 | 2.64 | 1.09–5.44 | 0.86 | 0.52–1.42 | 2.87 | 1.75–4.73 |
| 2+ casual sex partners | 0.59 | 0.27–1.37 | 12.96 | 1.78–36.45 | 0.63 | 0.35–1.16 | 12.54 | 3.48–45.23 |
| Drug use before sex | 2.25 | 1.03–4.55 | 0.24 | 0.09–2.02 | 2.26 | 1.56–3.27 | 0.28 | 0.07–1.08 |
| Daily+ heroin injection | 0.85 | 0.52–1.43 | 0.39 | 0.18–0.95 | 0.86 | 0.56–1.31 | 0.41 | 0.21–0.81 |
| Years injecting | 1.00 | 0.97–1.02 | 1.01 | 0.96–1.04 | 0.99 | 0.98–1.01 | 1.01 | 0.97–1.05 |
| Overdose | 1.59 | 0.89–2.78 | 3.33 | 1.52–8.36 | 1.7 | 0.92–3.13 | 3.55 | 1.32–9.55 |
| Receptive sharing | 2.67 | 1.98–3.51 | 2.36 | 1.31–4.44 | 2.63 | 2.17–3.18 | 2.46 | 1.30–4.65 |
| Recruiter class 2 (dummy) | -- | -- | -- | -- | 0.34 | 0.23–0.62 | 0.29 | 0.16–0.53 |
| Recruiter class 3 (dummy) | -- | -- | -- | -- | 0.38 | 0.18–0.66 | 0.18 | 0.08–0.38 |
PWID: People Who Inject Drugs
Peer Recruitment & Homophily
We assessed recruitment homophily, or the propensity for people to recruit others with similar characteristics, on the outcome of interest (polydrug use class) using RDSAT 5.6. (Volz et al., 2007) Recruitment homophily is measured as an index ranging from −1 to 1. Positive values indicate preferential recruitment of peers who are similar on a characteristic, negative values indicate an increased likelihood of recruiting peers who are dissimilar on a characteristic, and zero indicates that peers recruitment is random with respect to a characteristic. The homophily index was −1.0 for class 3 (e.g., while class 3 had the smallest sample size, class 3 individuals exclusively recruited peers from classes 1 and 2), .168 for class 2, and −.048 for class 1. In order to measure the dependence of one’s polydrug use latent class membership on that of his or her recruit, we used a chi-squared test of independence (p = 0.004). Together, the homophily indices and the p-value from the chi-squared test suggest that latent class membership among respondents was not completely independent of the latent class membership of their peer recruiters.
In Model 2 (Table 3), the lack of independence between individuals and their recruiters on the outcome of interest was accounted for by controlling for the recruiter’s outcome (latent class) and a the lack of independence among individuals in the same RDS recruitment chain was accounted for using a generalized estimated equation (GEE) approach which clustered on recruitment chain and specified robust standard errors. As seen in Table 3, the parameter estimates for Models 1 and 2 were nearly identical, though the confidence intervals were tighter around the parameter estimates in the GEE model.
Simultaneous Use Sub-Analysis
Although these classes were defined by use of methamphetamine or cocaine use by itself, many participants injected combinations of these drugs and heroin, so even in the non-polydrug use class there were individuals who had injected methamphetamine along with heroin, though not methamphetamine by itself. The majority of individuals in the methamphetamine, cocaine, and heroin use class (77.4%) and of those in the methamphetamine and heroin use class (75.7%) reported any simultaneous injection of two substances, compared with only 38.8% in the heroin use class.
In a sub-analysis, we assessed whether simultaneous use of pairs of drugs was associated with variation in sex and drug use behaviors. Chi-square tests of association between each pair of simultaneous drug injection and sex and drug use behaviors showed that injection of heroin and cocaine together (i.e., speedball) was significantly associated with receptive syringe sharing (p = .04), injection of methamphetamine and cocaine together was marginally associated with two or more casual sex partners (p = .08), and injection of methamphetamine and heroin together was significantly associated with both receptive and distributive syringe sharing (p <.001) and marginally associated with overdose (p = .06) and drug use before sex (p = .07). In these bivariate analyses, simultaneous injection of heroin and cocaine or methamphetamine was associated with syringe sharing, and simultaneous injection of methamphetamine with heroin or cocaine was associated with increased sex risk behaviors.
Discussion
In this analysis of polydrug use among heroin injectors in Tijuana, we identified discrete subtypes of heroin injectors based on patterns of concurrent methamphetamine and cocaine use. Substance use type informed the formation of latent classes, but the route of administration did not. Bivariate and multivariate analyses indicated a group of methamphetamine and cocaine users that exhibited higher risk sexual practices and decreased heroin injecting frequency and a group of methamphetamine users who were younger, more likely to be female, and with lower incomes.
In general, the classes defined by use of more substances were associated with higher risk for overdose and with higher levels of HIV drug use and sexual risk behaviors. Receptive syringe sharing was more common in both of the polydrug use classes compared with the predominantly heroin using class. Though prevalence of HIV and syphilis were similar across the classes, higher prevalence of receptive syringe sharing and higher risk sex behaviors in the polydrug use classes (especially the cocaine and methamphetamine use class) poses a greater likelihood of transmission of blood-borne and sexually transmitted infections.
The methamphetamine and cocaine class (class 1) had a higher proportion of females, greater involvement in sex exchange, more casual sex partners, and more drug use before sex, suggesting that cocaine use may be driving these sexual risk behaviors. Interestingly, this group had higher levels of education and lower levels of daily heroin injection, likely supplemented by use of methamphetamine and cocaine. This class was also more likely to have reported an overdose in the past, which may be partly explained by the higher rates of simultaneous injecting drug use. Overall, polydrug use of methamphetamine, cocaine, and heroin compared with predominantly heroin use appears to be associated with more overdoses, more syringe sharing, and higher risk sex behaviors.
We also observed higher prevalence of overdose for the two polydrug use classes: 9.2% in the methamphetamine use class and 16.1% in the methamphetamine and cocaine use class compared to only 4.7% in the no polydrug use (predominantly heroin) class. Although this relationship only retained significance for the methamphetamine and cocaine class in multivariate analyses, polydrug use was in general more common among those with more polydrug use.
Previous research on latent class analysis of polydrug use in users of illicit drugs has been conducted among illicit opioid users in Canada (Monga et al. 2007, Patra et al. 2009) and among heroin and cocaine users in Baltimore (Harrell et al. 2013, Kuramoto et al. 2011). Though these studies had different indicators of polydrug use and were conducted in samples of injection and non-injection drug users in locations with less methamphetamine use, there were several notable consistencies between the present analysis and previous research. Among illicit opioid users in a multisite study in Canada, Monga et al. (2007) found a polysubstance polydrug use class of heroin and cocaine injectors that had higher rates of overdose than the two other classes. In the same sample Patra et al. (2009) also found several classes of concurrent opioid and stimulant use. In a sample of heroin and cocaine users in Baltimore, Kuramoto et al. (2011) identified a heroin injecting class with lower injection risk when compared to a heroin and cocaine injecting class. And in another sample of heroin and cocaine users in Baltimore, Harrell et al. (2012) identified three classes; those in the polysubstance use class were more likely to report sharing needles (like the two polydrug use classes in this analysis) and those in the crack/nasal heroin using class were more likely to report sex work (like the methamphetamine and cocaine using class in this analysis).
There were several limitations to this analysis. Generalizability of these findings to other drug using populations may be limited as these drug use patterns and contextual risk factors may be unique to Tijuana (e.g., the type of black tar heroin used, the increased availability of methamphetamine, and the recruitment of participants from Tijuana red light district). Additionally, to describe basic patterns of use, variability in frequency of use was reduced to any use in the past 6 months. Though there may have been some misclassification into classes, the average probability for most likely class membership was fairly high at 89.4% to 94.6%. Finally, with this cross sectional assessment we are only able to determine association, not causation.
Conclusion
Through this analysis, we identified subtypes of heroin injectors who may require more tailored interventions to reduce the health and social harms of injecting drug use in Tijuana. In this and other resource limited settings, this work may be of value where there is greater need to tailor targeted interventions based on types of concurrent drug use. For example, PWID who use both heroin and cocaine may benefit from interventions that address both injection and sexual risk behaviors. Expanded access to sterile syringes through syringe exchange programs or pharmacies and overdose prevention efforts should be targeted to both groups of polydrug users, who reported higher levels of syringe sharing and overdose history. Future research is needed to explore variability in frequency of use and simultaneous drug use to determine if these patterns predict longitudinal patterns and changes in polydrug use.
Acknowledgments
The authors gratefully acknowledge the contributions of study participants and binational staff and investigators from the University of California San Diego and Pro-COMUSIDA for assistance with data collection, as well as Centro Nacional para la Prevencion y el Control del VIH/SIDA and Instituto de Servicios de Salud de Estado de Baja California. This research was funded by National Institute on Drug Abuse (NIDA) Grants R37 DA019829, R01 DA019829, T32 DA023356, and K01 DA033879.
References
- Agrawal A, Lynskey MT, Madden PA, Bucholz KK, Heath AC. A latent class analysis of illicit drug abuse/dependence: Results from the National Epidemiological Survey on Alcohol and Related Conditions. Addiction. 2007;102(1):94–104. doi: 10.1111/j.1360-0443.2006.01630.x. [DOI] [PubMed] [Google Scholar]
- Brecht ML, Huang D, Evans E, Hser YI. Polydrug use and implications for longitudinal research: Ten-year trajectories for heroin, cocaine, and methamphetamine users. Drug and Alcohol Dependence. 2008;96:193–201. doi: 10.1016/j.drugalcdep.2008.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brouwer KC, Case P, Ramos R, Magis-Rodriguez C, Bucardo J, Patterson T, Strathdee SA. Trends in production, trafficking and consumption of methamphetamine and cocaine in Mexico. Substance Use and Misuse. 2006;41:707–727. doi: 10.1080/10826080500411478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brouwer KC, Rusch ML, Weeks JR, Lozada R, Vera A, Magis-Rodríguez C, Strathdee SA. Spatial epidemiology of HIV among injection drug users in Tijuana, Mexico. Annals of the Association of American Geographers. 2012;102(5):1190–1199. doi: 10.1080/00045608.2012.674896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bucardo J, Brouwer KC, Case P, Magis-Rodriguez C, Fraga M, Perez SG, Strathdee SA. Historical trends in the production and consumption of illicit drugs in Mexico: Implications for the prevention of blood borne infections. Drug and Alcohol Dependence. 2005;79:281–293. doi: 10.1016/j.drugalcdep.2005.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlson RG, Wang J, Falck RS, Siegal HA. Drug use practices among MDMA/ecstasy users in Ohio: A latent class analysis. Drug and Alcohol Dependence. 2005;79(2):167–179. doi: 10.1016/j.drugalcdep.2005.01.011. [DOI] [PubMed] [Google Scholar]
- Case P, Ramos R, Brouwer KC, Firestone-Cruz M, Pollini RA, Fraga MA, Patterson TL, Strathdee SA. At the borders, on the edge: Use of injected methamphetamine in Tijuana and Ciudad Juarez, Mexico. Journal of Immigrant & Minority Health. 2008;10(1):23–33. doi: 10.1007/s10903-007-9051-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cleveland MJ, Collins LM, Lanza ST, Greenberg MT, Feinberg ME. Does individual risk moderate the effect of contextual-level protective factors? A latent class analysis of substance use. Journal of Prevention and Intervention in the Community. 2010;38(3):213–228. doi: 10.1080/10852352.2010.486299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drumwright LN, Patterson TL, Strathdee SA. Club drugs as causal risk factors of HIV acquisition among men who have sex with men: A review. Substance Use & Misuse. 2006;41(10–12):1551–1601. doi: 10.1080/10826080600847894. [DOI] [PubMed] [Google Scholar]
- European Monitoring Centre on Drugs and Drug Addiction. Select issue on polydrug use. Lisbon, Portugal: European Monitoring Centre on Drugs and Drug Addiction; 2009. [Google Scholar]
- Flaherty BP, Kiff CJ. Latent class and latent profile models. In: Cooper H, editor. APA handbook of research methods in psychology, vol. 3. Data analysis and research publication. Washington, DC: American Psychological Association; 2012. pp. 391–404. [Google Scholar]
- Harrell PBM, Petras H, Trenz R, Latimer WW. Latent classes of heroin and cocaine users predict unique HIV/HCV risk factors. Drug and Alcohol Dependence. 2012;122(3):220–227. doi: 10.1016/j.drugalcdep.2011.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heckathorn DD. Respondent-driven sampling: A new approach to the study of hidden populations. Social Problems. 1997;44:174–199. [Google Scholar]
- IBM Corp. IBM SPSS statistics for Windows, version 22.0. Armonk, NY: IBM Corp; 2013. [Google Scholar]
- Kuramoto SJ, Bohnert AS, Latkin CA. Understanding subtypes of inner-city drug users with a latent class approach. Drug and Alcohol Dependence. 2011;118(2–3):237–243. doi: 10.1016/j.drugalcdep.2011.03.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynskey MT, Agrawal A, Bucholz KK, Nelson EC, Madden PA, Todorov AA, Grant JD, Martin NG, Heath AC. Subtypes of illict drug users: A latent class analysis of data from an Australian twin simple. Twin Research and Human Genetics. 2006;9:523–530. doi: 10.1375/183242706778024964. [DOI] [PubMed] [Google Scholar]
- Monga N, Rehm J, Fischer B, Brissette S, Bruneau J, El-Guebaly N, Noël L, Tyndall M, Wild C, Leri F, Fallu JS, Bahl S. Using latent class analysis (LCA) to analyze patterns of drug use in a population of illegal opioid users. Drug and Alcohol Dependence. 2007;88:1–8. doi: 10.1016/j.drugalcdep.2006.08.029. [DOI] [PubMed] [Google Scholar]
- Muthen LK, Muthen BO. Mplus user’s guide. 7. Los Angeles, CA: Muthen & Muthen; 1998, 2012. [Google Scholar]
- Patra J, Fischer B, Maksimowska S, Rehm J. Profiling poly-substance use typologies in a multi-site cohort of illicit opioid and other drug users in Canada—a latent class analysis. Addition Research and Theory. 2009;17(2):168–185. [Google Scholar]
- Roesch SC, Villodas M, Villodas F. Latent class/profile analysis in maltreatment research: a commentary on Nooner et al., Pears et al., and looking beyond. Child Abuse & Neglect. 2010;34:155–160. doi: 10.1016/j.chiabu.2010.01.003. [DOI] [PubMed] [Google Scholar]
- Roy E, Richer I, Arruda N, Vandermeerschen J, Bruneau J. Patterns of cocaine and opioid co-use and polyroutes of administration among street-based cocaine users in Montreal, Canada. International Journal of Drug Policy. 2013;24:142–149. doi: 10.1016/j.drugpo.2012.10.004. [DOI] [PubMed] [Google Scholar]
- Rudolph AE, Gaines TL, Lozada R, Vera A, Brouwer KC. Evaluating outcome-correlated recruitment and geographic recruitment bias in a respondent-driven sample of people who inject drugs in Tijuana, Mexico. AIDS & Behavior. 2014;18(12):2325–2337. doi: 10.1007/s10461-014-0838-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rusch ML, Lozada R, Pollini RA, Vera A, Patterson TL, Case P, Strathdee SA. Polydrug use among IDUs in Tijuana, Mexico: Correlates of methamphetamine use and route of administration by gender. Journal of Urban Health. 2009;86(5):760–775. doi: 10.1007/s11524-009-9377-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp. Stata statistical software: Release 10.0. College Station, TX: Stata Corporation; 2007. [Google Scholar]
- Strathdee SA, Lozada R, Pollini RA, Brouwer KC, Mantsios A, Abramovitz DA, Rhodes T, et al. Individual, social, and environmental influences associated with HIV infection among injection drug users in Tijuana, Mexico. Journal of Acquired Immune Deficiency Syndromes. 2008;47:369–376. doi: 10.1097/QAI.0b013e318160d5ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volz E, Wejnert C, Degani I, Heckathorn DD. Respondent-driven sampling analysis tool (RDSAT), version 5.6. Ithaca, NY: Cornell University; 2007. [Google Scholar]