Abstract
The dose, volume, and clinical outcome data for penile bulb are reviewed for patients treated with external-beam radiotherapy. Most, but not all, studies find an association between impotence and dosimetric parameters (e.g., threshold doses) and clinical factors (e.g., age, comorbid diseases). According to the data available, it is prudent to keep the mean dose to 95% of the penile bulb volume to <50 Gy. It may also be prudent to limit the D70 and D90 to 70 Gy and 50 Gy, respectively, but coverage of the planning target volume should not be compromised. It is acknowledged that the penile bulb may not be the critical component of the erectile apparatus, but it seems to be a surrogate for yet to be determined structure(s) critical for erectile function for at least some techniques.
Keywords: Erectile dysfunction, Penile bulb, Radiation
Clinical Significance
Erectile dysfunction (ED), the consistent inability to attain or maintain an erection of sufficient quality to permit satisfactory sexual intercourse, is a common complication resulting from radiotherapy (RT) for prostate cancer (1). Many patients choose RT for their clinically localized prostate cancer because they believe there may be a lower risk of ED compared with radical prostatectomy (RP); however, this remains controversial. Posttreatment ED rates have been reported to be approximately 24% (brachytherapy alone), 40% (brachytherapy plus external RT), 45% (external RT alone), 66% (nerve-sparing RP), 75% (non–nerve-sparing RP), and 87% for cryosurgery, but physician-reported rates are known to be less reliable than patient-reported outcomes, so the optimal comparison studies have yet to be done (2).
Endpoints
The time course for RT-associated ED is variable (reported as days to years) and often evolves gradually. Ascribing ED to RT alone is difficult because men lose some erectile function with age, and other common diseases (e.g., diabetes, hypertension) may contribute. Various self-administered questionnaires have been used to assess erectile function in clinical studies (e.g., the International Index of Erectile Function [IIEF]) (3). Additional objective diagnostic tests can be performed (e.g., nocturnal penile tumescence, somatosensory evoked potentials, bulbocavernous reflex latency, penile electromyography, color duplex Doppler ultrasound, dynamic infusion cavernosometry, and pharmacotesting), but these are generally applied to establish the etiology of ED (4).
Challenges Defining Volume
The anatomy of the pelvic floor is challenging to visualize on CT or MRI, and hence definition of the penile bulb (PB) varies. This may contribute to inconsistent reports (5–15). The PB appears as an oval-shaped, hyperintense midline structure on T2-weighted MR images; on axial CT imaging it is bounded by the crura, corpora spongiosum, and the levator ani muscle (Fig. 1; see ref. 16 for details). At University of California-San Francisco, the bulb is defined as the most proximal portion of the penis sitting immediately caudal to the prostate. We also recognize that the bulb itself is not part of the erectile apparatus but consider it an anatomic surrogate for periprostatic tissue likely to receive high doses of RT.
Fig. 1.

Penile and erectile tissue anatomy with CT (A) and MR (B–D) images of the penile bulb (*). Adapted from Wallner et al. (16).
Review of Dose–Volume Data
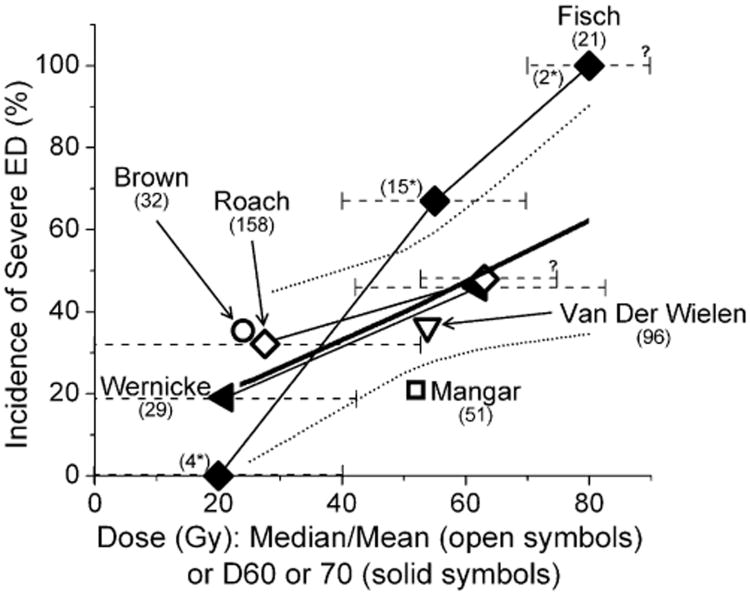
Published studies assessing the correlations between the dose of external-beam RT, the PB volume irradiated, clinical factors, and ED are summarized in Table 1. Figure 2 shows a summary of PB dose–volume data vs. rates of ED. Studies that reported an association between RT dose and ED suggested that a dose of approximately 50 Gy to essentially the entire PB was a threshold dose for an increased risk of ED. However, several studies did not identify an association between RT dose and ED (5, 11, 13).
Table 1. Erectile dysfunction after external-beam radiotherapy and correlated parameters.
| First author, year (reference) | N | Assessment method* | Prescribed dose, treatment | OAR definition | Severe ED rate (%) | Correlated parameters | |
|---|---|---|---|---|---|---|---|
|
| |||||||
| Dose–volume | Clinical | ||||||
| Fisch, 2001 (7) | 21 | Questionnaire† | 65–72 Gy, 3D | Penile bulb | 33‡ | D70 ≥70 Gy§ | No other endpoints analyzed |
| Roach, 2004 (10) | 158 | Patient report, (RTOG)‖ | 68.4 Gy, 73.8 Gy, 3D | Penile bulb¶ | 41 | Median penile bulb dose ≥52.5 Gy¶ | No other endpoints analyzed |
| Wernicke, 2004 (14) | 29 | Questionnaire† | 66.6–79.2 Gy, 3D | Penile bulb# | NS | D30 ≥67 Gy¶ D45 ≥63 Gy¶ D60 ≥42 Gy¶ D75 ≥20Gy¶ |
Alcohol and smoking not significant, dose and volume significant |
| Selek, 2004 (11) | 28 | Questionnaire† | 78 Gy, 3D | Penile bulb# | 35.7% at 2 y | Mean dose to penile structure 38.2 Gy, no dose–volume effect was found# | Up to 68% may have had ED posttreatment? ED correlated with hypertension |
| Mangar, 2006 (8) | 51 | Questionnaire† | 64 Gy, 74 Gy, 3D | Penile bulb, crura and cavernosum** | 24 | D15, D30, D50, D90 of penile bulb¶ | Adjusted for age, bulb volume, hypertension, and previous pelvic surgery |
| Zelefsky, 2006 (15) | 561 | Patient report (NCI)†† | 81 Gy, IMRT | ‡‡ | 49 | Not evaluated | Hormone therapy |
| Brown, 2007 (5) | 32 | Questionnaire† | NS, IMRT | Penile bulb | 34 | No relationship noted | Hypertension, pre-RT erectile function |
| Cahlon, 2008 (6) | 478 | Patient report (NCI)†† | 86.4 Gy, IMRT | ‡‡ | 30 | Not evaluated | Age >70 y, diabetes, hormone therapy |
| van der Wielen, 2008 (13) | 70 | Questionnaire† | 68 vs. 78 Gy | Penile bulb | 36 | No correlations between ED and dose–volume of crura, or the penile bulb# | Adjusted for diabetes and history of cardiovascular disease |
| Pinkawa, 2009 (9) | 123 | Questionnaire‡ | 70.2–72 Gy, 3D | NS | 73§§ | Not evaluated | Age, diabetes |
Abbreviations: OAR = organs at risk; ED = erectile dysfunction; RTOG = Radiation Therapy Oncology Group; NCI =National Cancer Institute; NS = not significant.
All assessments are patient-reported, based on questionnaires or morbidity scoring scales (e.g., RTOG, NCI), as noted.
All questionnaires are self-administered.
Potency scale declined ≥2.
Dx is dose delivered to the x% penile bulb volume.
RTOG radiation morbidity scoring scale.
Penile bulb was defined as proximal portion of the penis.
The penile bulb is here specifically defined as proximal enlargement of the corpus spongiosum that is secured to the urogenital diaphragm and covered by the bulbospongiosus muscle.
The penile bulb was here defined as a structure, whereas the crura and the cavernosum as a separate one.
NCI common toxicity criteria for adverse events.
Penile bulb not defined as a specific structure.
No erections firm enough for sexual intercourse.
Fig. 2.
Incidence of erectile dysfunction according to the radiation dose to the penile bulb. The x axis values are estimated according to the range of doses reported. The data for Fisch et al. (7) at 20, 55, and 80 Gy represent the reported rates of erectile dysfunction at <40, 40–70, and >70 Gy, respectively. Similarly, for Wernicke et al. (14) and Roach et al. (10), each symbol represents the rates of erectile dysfunction at ≤42 vs. >42 and <52.5 vs. ≥52.5 Gy, respectively. The dashed horizontal lines reflect the dose ranges ascribed to each data point. The upper x-axis range of the highest data point for Fisch et al. (7) and Roach et al. (10) are unknown. The mean doses of van der Wielen et al. (13) and Mangar et al. (8) are estimated from the subgroup data. The x-axis values for Wernicke et al. (14) are D60 and for Fisch et al. (7) are D70 (i.e., minimum dose received by 60% or 70% volume of the penile bulb). A thick solid line represents the fitted model with sample size correction, with 95% confidence intervals (dotted curves).
In general, it is difficult to extract a definite conclusion from these results, owing to relatively small numbers of patients, different anatomic definitions and endpoints for defining ED, and some potential methodologic problems. For example, Selek et al. (11) reported that 10 of 28 patients were completely impotent after RT (zero function on a 5-point scale) but that most of these were hypertensive. Furthermore, their choice of 0 on their scale to define an event may not be appropriately sensitive. The most widely accepted scale for evaluating sexual function is the IIEF (which spans from 0 to 25). The original IIEF, described by Rosen et al. (3), included 15 items and five domains. They subsequently developed an abridged version of the questionnaire that contained five questions, and the scores ranged from 5 to 25 (17).
In the 1999 report the authors found that 21 was the optimal cutoff score. Thus, whenever possible investigators are encouraged to use this cutoff to define ED instead of the mild, moderate, and severe categories (unless independently validated). Thus for example, in the case of the report by Selek et al. (11) it is likely than only assigning patients with a score “0” as being impotent underestimated the true baseline level of ED in their study population (see recommendations in “Toxicity Scoring”).
In addition, several of these studies included a sizable fraction of patients who received phosphodiesterase type 5 inhibitors that might attenuate the effects of RT on sexual function (18, 19). Earlier studies were less likely to be contaminated by this issue because these agents were not available when most of these patients were treated (7, 10).
Brown et al. (5) studied 32 patients and noted no dose–response association for ED. However, they used intensity-modulated RT and attempted to spare the PB, resulting in a mean dose to the bulb of only 25 Gy. Thus, their data do not explicitly refute the presence of a dose–response association at higher doses.
Several studies reported a significant dose–volume effect correlated with risk of ED using the metrics of Dx (i.e., the minimum dose received by x% volume of the PB). For example, Fisch et al. (7) noted ED in 0, 80%, or 100% of patients with a D70 of 0–40, 40–70, and >70 Gy, respectively. Similarly, Mangar et al. (8) reported that a D90 ≥50 Gy is associated with a significant risk of ED. Wernicke et al. (14) reported that D30, D45, D60, and D75 correlated with an increased risk of ED. Roach et al. (10) reported a significant correlation between a median PB dose of 52.5 Gy and an increase in ED. Brachytherapy studies are mixed in their support for an association between PB doses and ED. Merrick et al. (20) used a matched-pair study of ED after brachytherapy and related PB dose–volume metrics to patient-reported questionnaire data. The rate of ED was associated with doses to the PB (particularly median dose [D50]) and to a lesser degree the crura. On the other hand, the Macdonald et al. (21) review of 342 patients after brachytherapy failed to show an association between median PB dose and ED.
Factors Affecting Risk
Patient-related factors for ED have not been emphasized, except for a few reports. Post-RT ED rates have been reported to be higher with baseline pretreatment ED, diabetes, smoking history, or a history of hypertension (5, 7, 20, 22). The data, however, are somewhat conflicting (Table 1).
Mathematic/Biologic Models
Penile bulb dose–volume parameters may be associated with the incidence of ED, although the results are conflicting to prove a clear correlation between those parameters (Fig. 2). For example, van der Wielen et al. (23) reviewed the literature and concluded that “sparing of the penile bulb to improve potency-preservation is not sufficiently supported by the current literature…” and questioned whether the potential “oncological risk” was justified given the uncertainty of potency sparing. It is possible that the key anatomic structures involved in ED pathophysiology have not been defined. Moreover, dosimetric accuracy of the true accumulated dose distribution has seldom been examined in detail. The data are sparse. Overall, the data plotted in Fig. 2 may be consistent with either a causal or surrogate relationship.
Special Situations
Hormonal therapy itself is associated with the ED. Several studies reported the deleterious impact of hormonal therapy on erectile function (3, 17, 23–27). However, the association of hormonal therapy with RT dose/volume of the PB is unknown.
Recommended Dose/Volume Limits
On the basis of the data available, it is prudent to keep the mean dose to 95% of the PB volume to <50 Gy. It may also be prudent to limit the D70 and D90 to 70 Gy and 50 Gy, respectively. It is acknowledged that the PB may not be the critical component of the erectile apparatus, but it seems to be a surrogate for yet to be determined structure(s) critical for erectile function for at least some techniques.
Future Toxicity Studies
Standard methods to define the PB and associated critical structures should become more widely used. A standard method to score ED should be more widely adopted. Systematic prospective clinical trials that attempt to relate the three-dimensional dose–volume parameters from all of the potentially critical structures to clinical outcomes should be considered. Such studies may help to identify which pelvic structures are critical for ED. Dosimetric/imaging studies estimating uncertainties in the overall accumulated “true dose distribution” should be considered. This may be a key cause of inconsistencies between reported results. Anatomic studies to better define the critical anatomic sites for RT-associated ED may be helpful. Well-characterized data (including full dose distribution and imaging information) should be pooled from multiple studies where possible.
Toxicity Scoring
We recommend that patients undergo pre- and post-RT assessment of ED using the IIEF. Patients can be grouped into five groups according to their scores; for example, in none (25–22), mild (21–17), mild to moderate (16–12), moderate (11–8), and severe (7–5). It is important that the evaluation of ED is performed with a detailed history including sexual, medical, and psychosocial status and other laboratory tests (3, 17, 26, 27). Further clinical studies may be needed to validate the IIEF for the assessment of ED after RT.
Acknowledgments
M.R. has received recent funding from GSK, Siemens, CareCore National, the National Cancer Institute, Molecular Insight, TROFEX, General Electric, Novartis, CPAC (Tomotherapy, Inc.), and has acted as a consultant (Proton and Carbon Accelerator development). L.B.M. has received honoraria from Varian Medical Systems, as well as grant support from the National Institutes of Health (NIH), the Lance Armstrong Foundation, and the U.S. Department of Defense. J.O.D. receives funding from the NIH, Varian Medical Systems, and Tomotherapy, Inc. I.E.-N. receives funding from the NIH, Varian Medical Systems, and Tomotherapy, Inc.
Footnotes
Conflict of interest: All other authors have no conflict of interest.
References
- 1.Sanda MG, Dunn RL, Michalski J, et al. Quality of life and satisfaction with outcome among prostate-cancer survivors. N Engl J Med. 2008;358:1250–1261. doi: 10.1056/NEJMoa074311. [DOI] [PubMed] [Google Scholar]
- 2.Robinson JW, Moritz S, Fung T. Meta-analysis of rates of erectile function after treatment of localized prostate carcinoma. Int J Radiat Oncol Biol Phys. 2002;54:1063–1068. doi: 10.1016/s0360-3016(02)03030-4. [DOI] [PubMed] [Google Scholar]
- 3.Rosen RC, Riley A, Wagner G, et al. The international index of erectile function (IIEF): A multidimensional scale for assessment of erectile dysfunction. Urology. 1997;49:822–830. doi: 10.1016/s0090-4295(97)00238-0. [DOI] [PubMed] [Google Scholar]
- 4.Broderick GA. Evidence based assessment of erectile dysfunction. Int J Impot Res. 1998;10(Suppl. 2):S64–S73. discussion S77–S69. [PubMed] [Google Scholar]
- 5.Brown MW, Brooks JP, Albert PS, et al. An analysis of erectile function after intensity modulated radiation therapy for localized prostate carcinoma. Prostate Cancer Prostatic Dis. 2007;10:189–193. doi: 10.1038/sj.pcan.4500938. [DOI] [PubMed] [Google Scholar]
- 6.Cahlon O, Zelefsky MJ, Shippy A, et al. Ultra-high dose (86.4 Gy) IMRT for localized prostate cancer: Toxicity and biochemical outcomes. Int J Radiat Oncol Biol Phys. 2008;71:330–337. doi: 10.1016/j.ijrobp.2007.10.004. [DOI] [PubMed] [Google Scholar]
- 7.Fisch BM, Pickett B, Weinberg V, et al. Dose of radiation received by the bulb of the penis correlates with risk of impotence after three-dimensional conformal radiotherapy for prostate cancer. Urology. 2001;57:955–959. doi: 10.1016/s0090-4295(01)00940-2. [DOI] [PubMed] [Google Scholar]
- 8.Mangar SA, Sydes MR, Tucker HL, et al. Evaluating the relationship between erectile dysfunction and dose received by the penile bulb: Using data from a randomised controlled trial of conformal radiotherapy in prostate cancer (MRC RT01, ISRCTN47772397) Radiother Oncol. 2006;80:355–362. doi: 10.1016/j.radonc.2006.07.037. [DOI] [PubMed] [Google Scholar]
- 9.Pinkawa M, Gagel B, Piroth MD, et al. Erectile dysfunction after external beam radiotherapy for prostate cancer. Eur Urol. 2009;55:227–236. doi: 10.1016/j.eururo.2008.03.026. [DOI] [PubMed] [Google Scholar]
- 10.Roach M, Winter K, Michalski JM, et al. Penile bulb dose and impotence after three-dimensional conformal radiotherapy for prostate cancer on RTOG 9406: Findings from a prospective, multi-institutional, phase I/II dose-escalation study. Int J Radiat Oncol Biol Phys. 2004;60:1351–1356. doi: 10.1016/j.ijrobp.2004.05.026. [DOI] [PubMed] [Google Scholar]
- 11.Selek U, Cheung R, Lii M, et al. Erectile dysfunction and radiation dose to penile base structures: A lack of correlation. Int J Radiat Oncol Biol Phys. 2004;59:1039–1046. doi: 10.1016/j.ijrobp.2003.12.028. [DOI] [PubMed] [Google Scholar]
- 12.Skala M, Rosewall T, Dawson L, et al. Patient-assessed late toxicity rates and principal component analysis after image-guided radiation therapy for prostate cancer. Int J Radiat Oncol Biol Phys. 2007;68:690–698. doi: 10.1016/j.ijrobp.2006.12.064. [DOI] [PubMed] [Google Scholar]
- 13.van der Wielen GJ, Hoogeman MS, Dohle GR, et al. Dose-volume parameters of the corpora cavernosa do not correlate with erectile dysfunction after external beam radiotherapy for prostate cancer: Results from a dose-escalation trial. Int J Radiat Oncol Biol Phys. 2008;71:795–800. doi: 10.1016/j.ijrobp.2007.10.052. [DOI] [PubMed] [Google Scholar]
- 14.Wernicke AG, Valicenti R, DiEva K, et al. Radiation dose delivered to the proximal penis as a predictor of the risk of erectile dysfunction after three-dimensional conformal radiotherapy for localized prostate cancer. Int J Radiat Oncol Biol Phys. 2004;60:1357–1363. doi: 10.1016/j.ijrobp.2004.05.030. [DOI] [PubMed] [Google Scholar]
- 15.Zelefsky MJ, Chan H, Hunt M, et al. Long-term outcome of high dose intensity modulated radiation therapy for patients with clinically localized prostate cancer. J Urol. 2006;176:1415–1419. doi: 10.1016/j.juro.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 16.Wallner KE, Merrick GS, Benson ML, et al. Penile bulb imaging. Int J Radiat Oncol Biol Phys. 2002;53:928–933. doi: 10.1016/s0360-3016(02)02805-5. [DOI] [PubMed] [Google Scholar]
- 17.Rosen RC, Cappelleri JC, Smith MD, et al. Development and evaluation of an abridged, 5-item version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction. Int J Impot Res. 1999;11:319–326. doi: 10.1038/sj.ijir.3900472. [DOI] [PubMed] [Google Scholar]
- 18.Weber DC, Bieri S, Kurtz JM, et al. Prospective pilot study of sildenafil for treatment of postradiotherapy erectile dysfunction in patients with prostate cancer. J Clin Oncol. 1999;17:3444–3449. doi: 10.1200/JCO.1999.17.11.3444. [DOI] [PubMed] [Google Scholar]
- 19.Zelefsky MJ, McKee AB, Lee H, et al. Efficacy of oral sildenafil in patients with erectile dysfunction after radiotherapy for carcinoma of the prostate. Urology. 1999;53:775–778. doi: 10.1016/s0090-4295(98)00594-9. [DOI] [PubMed] [Google Scholar]
- 20.Merrick GS, Butler WM, Wallner KE, et al. The importance of radiation doses to the penile bulb vs crura in the development of postbrachytherapy erectile dysfunction. Int J Radiat Oncol Biol Phys. 2002;54:1055–1062. doi: 10.1016/s0360-3016(02)03031-6. [DOI] [PubMed] [Google Scholar]
- 21.Macdonald AG, Keyes M, Kruk A, et al. Predictive factors for erectile dysfunction in men with prostate cancer after brachytherapy: Is dose to the penile bulb important? Int J Radiat Oncol Biol Phys. 2005;63:155–163. doi: 10.1016/j.ijrobp.2004.12.056. [DOI] [PubMed] [Google Scholar]
- 22.Goldstein I, Feldman MI, Deckers PJ, et al. Radiation-associated impotence. A clinical study of its mechanism. JAMA. 1984;251:903–910. doi: 10.1001/jama.251.7.903. [DOI] [PubMed] [Google Scholar]
- 23.van der Wielen GJ, van Putten WLJ, Incrocci L. Sexual function after three-dimensional conformal radiotherapy for prostate cancer: Results from a dose-escalation trial. Int J Radiat Oncol Biol Phys. 2007;68:479–484. doi: 10.1016/j.ijrobp.2006.12.015. [DOI] [PubMed] [Google Scholar]
- 24.Chen CT, Valicenti RK, Lu J, et al. Does hormonal therapy influence sexual function in men receiving 3D conformal radiation therapy for prostate cancer? Int J Radiat Oncol Biol Phys. 2001;50:591–595. doi: 10.1016/s0360-3016(01)01504-8. [DOI] [PubMed] [Google Scholar]
- 25.D'Amico AV, Manola J, Loffredo M, et al. 6-month androgen suppression plus radiation therapy vs. radiation therapy alone for patients with clinically localized prostate cancer: A randomized controlled trial. JAMA. 2004;292:821–827. doi: 10.1001/jama.292.7.821. [DOI] [PubMed] [Google Scholar]
- 26.Kratzik CW, Schatzl G, Lunglmayr G, et al. The impact of age, body mass index and testosterone on erectile dysfunction. J Urol. 2005;174:240–243. doi: 10.1097/01.ju.0000162049.95483.51. [DOI] [PubMed] [Google Scholar]
- 27.Rosenberg MT. Diagnosis and management of erectile dysfunction in the primary care setting. Int J Clin Pract. 2007;61:1198–1208. doi: 10.1111/j.1742-1241.2007.01418.x. [DOI] [PubMed] [Google Scholar]