Abstract
Background
Current research attention has been moving toward the needs of patients and their consequences for the quality of life (QoL). Self-stigma is a maladaptive psychosocial phenomenon disturbing the QoL in a substantial number of psychiatric patients. In our study, we examined the relationship between demographic data, the severity of symptoms, self-stigma, and QoL in patients with schizophrenia spectrum disorder.
Methods
Probands who met International Classification of Diseases-10 criteria for schizophrenia spectrum disorder (schizophrenia, schizoaffective disorder, or delusional disorder) were recruited in the study. We studied the correlations between the QoL measured by the QoL Satisfaction and Enjoyment Questionnaire, self-stigma assessed by the Internalized Stigma of Mental Illness, and severity of the disorder measured by the objective and subjective Clinical Global Impression severity scales in this cross-sectional study.
Results
A total of 109 psychotic patients and 91 healthy controls participated in the study. Compared with the control group, there was a lower QoL and a higher score of self-stigmatization in psychotic patients. We found the correlation between an overall rating of self-stigmatization, duration of disorder, and QoL. The level of self-stigmatization correlated positively with total symptom severity score and negatively with the QoL. Multiple regression analysis revealed that the overall rating of objective symptom severity and the score of self-stigma were significantly associated with the QoL.
Conclusion
Our study suggests a negative impact of self-stigma level on the QoL in patients suffering from schizophrenia spectrum disorders.
Keywords: quality of life, self-stigma, schizophrenia, schizoaffective disorder, delusional disorder
Introduction
Schizophrenia spectrum disorders are chronic and highly debilitating psychiatric disorders characterized by impairment of thinking, feeling, behavior, and global functioning. Because of the wide spectrum of impairment with persistent cognitive dysfunction, many patients with this condition fail to gain occupation or maintain a marriage.1–3 Although significant progress has been made in the development of drugs used to treat schizophrenia spectrum disorders, investigation in this area has often focused only on the management of psychotic symptoms and the assessment of side effects. These objectives are essential facets of psychopharmacological research, but they do not cover all important factors that influence pharmacological treatment of patients with schizophrenia spectrum disorder. Current research has started focusing on the broader needs of patients.
Recently, as a consequence of an increased focus on patients’ experiences and their needs, the idea of quality of life (QoL) has been taken into consideration in the research of mental disorders, such as schizophrenia.4–10 If one of the main goals of treatment of schizophrenia is to recover patient’s adaptive functioning and QoL, then determining the efficacy or improvement of treatment should also include assessment of the QoL. The measurement of QoL offers complementary information that contributes to a multidimensional approach in both research and treatment of schizophrenia.11
In patients with schizophrenia, QoL has been recognized as the main result of treatment.12–14 There were concerns about the reliability of self-report measures in patients with schizophrenia,14 but many investigations have shown that these concerns are not very legitimate.11 Much earlier, Lehman15 demonstrated that the QoL data received from subjective QoL assessment of patients with schizophrenia were reliable. Although QoL is considered to be important for research on treatment outcome in schizophrenia, the evaluation of QoL in clinical practice remains underused.16
Self-stigma is a maladaptive psychosocial phenomenon disturbing a substantial number of psychiatric patients.17 Patients with a high level of self-stigma accept the societal prejudices about people with mental illness and thus are convinced of their inferiority or untreatability of their mental problems.18 Self-stigma often leads to dysphoria and decline in self-esteem and QoL.19 Social isolation or other forms of potentially maladaptive behavior are also common. Self-stigma might also lead to suicide.20 The negative impact of self-stigma on the treatment efficacy in mental disorders may also be present.21,22
The aims of this study were to investigate the QoL and self-stigma in outpatients with schizophrenia and to find out how the QoL and self-stigma are related to each other and which demographic and clinical data could influence them.
Methods
The study group consisted of mentally ill people with schizophrenia and related psychotic disorders according to the International Classification of Diseases, Tenth Revision.23 One hundred and forty psychiatrists in Czech Republic received a letter with a request for collaboration. Twenty psychiatrists from different towns who agreed to cooperate received the questionnaires. Psychiatrists made an assessment with the patients during regular sessions, which lasting ~40 minutes. The research was realized between March 2014 and November 2015. The inclusion criteria were age between 18 years and 60 years, both sexes, diagnosis of schizophrenia, schizoaffective disorder, or delusional disorder. The exclusion criteria were severe acute symptomatology and comorbidity with substance abuse.
Measurements
The patients completed several questionnaires during their routine psychiatric control.
The Quality of Life Satisfaction and Enjoyment Questionnaire (Q-LES-Q7) with 93 questions is divided into eight domains to measure. The probands assess each domain by choosing one number from a five-point Likert scale according to their level of satisfaction with the domain. The completion takes from 20 to 30 minutes. Patients complete the domains of physical health, feelings, leisure, household, work, school/study, social relations, general, and a sum of the QoL. The Czech Republic version of the Q-LES-Q was validated by Müllerova.24
The Internalized Stigma of Mental Illness (ISMI25) scale includes 29 statements with a four-point Likert scale that measures the level of the agreement. The scale assesses five facets of self-stigma: alienation, perceived discrimination, stereotype endorsement, social withdrawal, and resistance to the stigma.25 The questionnaire was standardized in Czech Republic by Ociskova et al.26
Clinical Global Impression (CGI27) is a simple scale used for global assessment of the severity of psychopathology. The CGI severity rating is based on symptoms, behaviors, and functioning over the past 7 days, both reported and observed. It is assessed on the seven-point scale ranging from 1 (normal) to 7 (among the most extremely ill patients). The first evaluation is performed by the patient’s psychologist or psychiatrist using the objective form of the scale (objCGI). The patient also evaluates himself/herself by the subjective version (subCGI), which includes seven levels of severity of psychopathology.27
The demographic questionnaire contained basic information such as sex, age, employment status, pension status, education, age of disease onset, duration of attendance at the outpatient clinic, number of underwent psychiatric hospitalizations, time since the last hospitalization, number of visited psychiatrists in outpatient practice, current medication, and discontinuation of medication in the past (recommended by a psychiatrist or arbitrarily).
Statistical analysis and ethics
The statistical software packages Prism3 and SPSS 17.0 were used for statistical analysis. Demographic data and average total scores on the particular scales were assessed using descriptive statistics. Mean, median, standard deviation, and the distribution of data were defined. The Shapiro–Wilk W-test determined the Gaussian distribution of the demographic and QoL variables. The t-tests of the Mann–Whitney U-tests and unpaired t-test were used for the comparisons of the means. The relationships between particular categories were analyzed using the correlation coefficients (Pearson or Spearman according to the data distribution) and linear regression. The Fisher’s exact test or chi-square test verified the connection between alternative variables (sex, marital status, and education). Multiple stepwise regression analysis was used to analyze the significance of the correlations of the particular factors. The 5% level of significance was considered to be acceptable for all statistical tests. The ethics committee of the University Hospital Olomouc approved the study. The investigation was conducted in agreement with the latest version of the Declaration of Helsinki and standards of Good Clinical Practice.28 All the patients signed an informed consent.
Results
Subjects
A total of 109 outpatients (62.4% females) with a mean age of 42.00±10.42 years attended the study. The distribution of diagnosis was as follows: schizophrenia (n=71), schizoaffective disorder (n=31), and delusional disorder (n=8). One hundred and three patients completed all the questionnaires, and based on those, the analysis was performed (Table 1). There were 91 subjects in the control group (50.5% females) with a mean age of 36.23±13.40 years.
Table 1.
Description of the sample, demographic, and clinical data
| Variable | Patients (n=103) | Controls (n=91) | Statistics |
|---|---|---|---|
| Age | 41.96±10.231 | 36.23±13.40 | MW test; U=3,519; P<0.0005 |
| Sex (male:female) | 41:62 | 36:55 | Fisher’s exact test (ns) |
| Age of disease onset | 26.12±8.974 | ||
| Lifetime duration of treatment | 15.38±9.519 | ||
| Number of hospitalizations | 4.13±3.968 | ||
| Psychiatric heredity | |||
| Same disorder | 15 (14.6%) | ||
| Other disorder | 39 (37.9%) | ||
| Without | 47 (45.6%) | ||
| Education | Pearson’s chi-squared test (ns) | ||
| Elementary | 9 (8.7%) | 1 (0.9%) | |
| Vocational training | 25 (24.3%) | 3 (2.8%) | |
| Secondary school | 52 (50.5%) | 38 (34.9%) | |
| University | 16 (15.5%) | 9 (8.3%) | |
| Not completed | 1 (0.01%) | 40 (0.44%) | |
| Marital status | Pearson’s chi-squared test (ns) | ||
| Single | 61 (59.0%) | 28 (25.7%) | |
| Married | 24 (23.1%) | 21 (19.3%) | |
| Divorced | 15 (14.3%) | 1 (0.9%) | |
| Widowed | 1 (0.9%) | 1 (0.9%) | |
| Not completed | 3 (2.7%) | 40 (0.44%) | |
| Employment (yes/no) | 33/70 | ||
| objCGI severity | 4.14±0.971 | ||
| subCGI severity | 2.75±1.392 | ||
| objCGI–subCGI severity | 1.67±1.56 | ||
| Physical health (max 65p) | 41.81±9.74 | 43.53±10.43 | Unpaired t-test: t=4.098; df=180; P<0.0001 |
| Feelings (max 70p) | 46.33±10.63 | 52.36±9.70 | Unpaired t-test: t=4.107; df=192; P<0.0001 |
| Work (max 65p) | 27.82±18.13 | 37.78±19.47 | MW test: U=3,377; P<0.001 |
| Household (max 50p) | 34.99±9.04 | 33.84±13.72 | Unpaired t-test: t=0.6997; df=192; ns |
| School/study (max 50p) | 13.47±8.77 | 20.05±12.97 | MW test: U=3,451; P<0.005 |
| Leisure (max 30p) | 20.15±5.42 | 25.22±4.05 | Unpaired t-test: t=7.290; df=191; P<0.0001 |
| Social activities (max 55p) | 35.69±9.22 | 43.02±8.24 | Unpaired t-test: t=5.808; df=192; P<0.0001 |
| General (max 80p) | 51.49±12.08 | 56.88±9.69 | Unpaired t-test: t=3.400; df=192; P<0.001 |
| Sum of Q-LES-Q (max 465p) | 271.5±58.03 | 312.68±46.11 | Unpaired t-test: t=5.419; df=192; P<0.0001 |
| Sum of Q-LES-Q in percent | 58.42%±12.47% | 67.24%±9.91% | Unpaired t-test: t=5.401; df=192; P<0.0001 |
| Alienation | 13.31±3.89 | ||
| Stereotype agreement | 14.01±3.42 | ||
| Perceived discrimination | 11.01±3.30 | ||
| Social withdrawal | 13.03±3.77 | ||
| Stigma resistance | 12.63±2.34 | ||
| Overall score | 63.98±13.74 |
Note: Data are presented as mean ± SD or n (%).
Abbreviations: CGI, Clinical Global Impression; df, degrees of freedom; max, maximum; MW test, Mann–Whitney test; ns, non significant; objCGI, objective CGI; p, points; Q-LES-Q, Quality of Life Satisfaction and Enjoyment Questionnaire; subCGI, subjective CGI.
Approximately one of three (n=33) patients were employed. In total, 76 (69.7%) patients received disability benefits: the most frequent were full disability benefits (n=65; 59.6%), followed by partial disability benefits (n=20; 18.3%) and retirement (n=8; 7.3%).
The average number of the hospitalizations in the past was 4.22±4.01. One hundred and one (92.7%) patients were hospitalized at least once. Only seven (6.4%) of the whole sample managed their problems on an outpatient basis without any hospitalization.
In the demographic questionnaire, the patient reported the subjective experienced social support. More than 60% of respondents believed that their social support is very good or relative good. Only nine patients described their social support as not sufficient, and three patients considered their social support to be catastrophic – they were fully isolated. The current mood of the patients was rated as “normal, not very good” (n=66; 60.6%), followed by patients with very good mood (n=33; 30.3%) and very bad mood (n=10; 9.2%).
Treatment
One hundred and seven (98.2%) patients reported that they used antipsychotics. Most of the patients indicated that they were using the medication in prescribed dosages regularly (89.9%), two reported using higher dosages than were prescribed, and eight (7.3%) patients reported taking the medication irregularly. Two patients (1.8%) stated that they did not use the medication at all. The mean duration of the psychiatric treatment was 15.69±9.66 years.
Severity of the disorder
Psychiatrists evaluated the actual severity of the disorder in their patients using objCGI severity scores. In average, the objCGI score was 4.13±0.95. The average rating of subCGI was 2.73±1.36. The average difference between objCGI severity rating and subCGI rating was 1.69±1.55 (Table 1).
Self-stigma
A total of 108 patients completed the ISMI questionnaire, and only one patient did not complete it.
Relation between self-stigma and demographic and clinical variables
“Overall score of ISMI” did not statistically significantly correlate with the age of patients and the age of the onset of the disorder (Table 2). However, the age of onset of the disorder was statistically significantly negatively correlated with the ISMI subscale “perceived discrimination” (Table 2). It means that if the mental disorder started at an earlier age, the patients perceived more intense discriminative behavior from others. Spearman’s correlation coefficient did not exhibit a statistically significant correlation between the overall score of ISMI and the number of hospitalizations (Table 2), but the positive relationship was between the number of hospitalizations and subscale perceived discrimination. Pearson’s correlation coefficient found no statistically significant association between the overall score of ISMI and duration of disorder, but statistical significance stayed close to fixed level. The duration of the course of mental illness is in a weak significant positive correlation with the “alienation” subscale. This could mean the longer a mental illness lasts, the more one can feel socially alienated and different. The trend shows a correlation between the duration of disorder and the perceived discrimination subscale (Table 2).
Table 2.
Relations between self-stigma and demographic and clinical variables
| Variable | Overall score | Alienation | Stereotype agreement | Perceived discrimination | Social withdrawal | Stigma resistance |
|---|---|---|---|---|---|---|
| Pearson’s or Spearman’s correlations | ||||||
| Age | 0.007 | −0.039 | 0.046 | −0.090 | 0.035 | 0.067 |
| Onset | −0.125 | −0.188 | −0.068 | −0.274* | −0.092 | 0.087 |
| Length | 0.181** | 0.190* | 0.163 | 0.188*** | 0.163 | 0.048 |
| Hospitalizations | 0.121 | 0.143 | 0.011 | 0.277**** | 0.139 | −0.091 |
| objCGI severity | 0.154 | 0.072 | 0.103 | 0.211* | 0.136 | 0.149 |
| subCGI severity | 0.520***** | 0.466***** | 0.475***** | 0.319***** | 0.482***** | 0.339***** |
| objCGI–subCGI severity | −0.374***** | −0.375***** | −0.338**** | −0.209* | −0.363***** | −0.138 |
| Unpaired t-test comparisons between subgroups | ||||||
| Male/female | 65.29±13.13 | 13.32±3.86 | 14.34±3.37 | 11.63±3.51 | 13.20±3.44 | 12.80±2.11 |
| 63.04±13.71 | 13.31±3.85 | 13.72±3.37 | 10.69±3.09 | 12.90±3.87 | 12.60±2.46 | |
| Unpaired t-test: t=0.84; df=106; ns | Unpaired t-test: t=0.005; df=106; ns | Unpaired t-test: t=0.94; df=106; ns | Unpaired t-test: t=1.47; df=106; ns | Unpaired t-test: t=0.41; df=106; ns | Unpaired t-test: t=0.45; df=106; ns | |
| Employment (yes/no) | 59.42±13.30 | 12.45±3.91 | 12.85±3.13 | 10.09±2.86 | 11.70±3.19 | 12.73±2.56 |
| 65.8±13.16 | 13.69±3.78 | 14.44±3.37 | 11.47±3.36 | 13.59±3.77 | 12.65±2.27 | |
| Unpaired t-test: t=−2; df=106; P<0.05 | Unpaired t-test: t=−1.56; df=106; ns | Unpaired t-test: t=−2.3; df=106; P<0.05 | Unpaired t-test: t=−2.04; df=106; P<0.05 | Unpaired t-test: t=−2.51; df=106; P<0.05 | Unpaired t-test: t=0.15; df=106; ns | |
| One-way ANOVA comparisons between subgroups | ||||||
| Education | 66.00±16.04 | 12.80±4.07 | 14.80±3.99 | 12.00±4.87 | 14.20±4.36 | 13.20±2.53 |
| Elementary (n=10) | 65.48±14.12 | 14.11±4.02 | 13.96±3.47 | 11.22±3.66 | 13.04±4.13 | 13.19±1.92 |
| Vocational training (n=28) | 64.23±12.86 | 13.68±3.54 | 14.25±3.36 | 10.96±2.88 | 13.25±3.38 | 12.34±2.49 |
| Secondary school (n=53) | 59.35±13.32 | 11.47±3.92 | 12.35±2.58 | 10.47±2.89 | 11.47±3.45 | 12.82±2.09 |
| University (n=17) | One-way ANOVA; F=0.849; df=3; ns | One-way ANOVA; F=1.972; df=3; ns | One-way ANOVA; F=1.646; df=3; ns | One-way ANOVA; F=0.849; df=3; ns | One-way ANOVA; F=0.485; df=3; ns | One-way ANOVA; F=1.405; df=3; ns |
| Marital | 63.94±14.84 | 13.41±4.11 | 13.88±3.57 | 11.38±3.50 | 13.05±3.92 | 12.39±2.45 |
| Single (n=54) | 61.71±10.13 | 12.63±3.21 | 13.54±2.82 | 10.29±2.81 | 12.29±2.84 | 12.96±1.65 |
| Married (n=24) | 69.50±10.98 | 14.69±3.48 | 15.31±3.05 | 11.63±2.73 | 14.81±3.21 | 13.13±2.36 |
| Divorced (n=16) | 42.00±0.00 | 7.00±0.00 | 8.00±0.00 | 6.00±0.00 | 8.00±0.00 | 13.00±0.00 |
| Widowed (n=1) | One-way ANOVA; F=1.685, df=2; ns | One-way ANOVA; F=1.39; df=2; ns | One-way ANOVA; F=1.51; df=2; ns | One-way ANOVA; F=1.16; df=2; ns | One-way ANOVA; F=2.42; df=2; ns | One-way ANOVA; F=0.980; df=2; ns |
Notes: Statistically significant relation is marked by *:
P<0.05;
P=0.06;
P=0.052;
P<0.01;
P<0.001.
Abbreviations: ANOVA, analysis of variance; CGI, Clinical Global Impression; df, degrees of freedom; ns, non significant; objCGI, objective CGI; subCGI, subjective CGI.
Spearman’s correlation coefficient calculated the relation of self-stigmatization and current severity of psychopathology rated by CGI. There was a strong significant positive relationship between the overall degree of self-stigma and subCGI (Table 2). The patients with more severe psychopathology evaluated themselves as more self-stigmatized in all subscales of ISMI. We have also found a statistically significant relationship between the overall score and all the subscores of self-stigma and subCGI severity (Table 2). objCGI severity was only in a weak significant positive correlation with the perceived discrimination subscale.
There were no differences between sex in the overall score of ISMI and subscores of ISMI (Table 2). Regarding marital status, the overall score of ISMI, and scores of subscales of ISMI, there were no differences between groups of married, unmarried, and divorced patients. There were also no differences in the overall rating of ISMI and its subscores between patients with a different level of education. Nevertheless, there was a statistically significant difference in the overall rating of ISMI between employed and unemployed patients. Patients who had a job (n=33) stigmatized themselves less than those who did not (n=75). This difference also occurs in the following subscales: stereotype agreement, perceived discrimination, and social withdrawal (Table 2).
Quality of life
A total of 103 patients completed the Q-LES-Q. From the maximum of 465 possible points, patients received 271.5+58.03; the mean relative sum of the QoL was 58.4%±12.47%. The healthy controls reached 312.68±46.11 points in average, and the maximum of relative sum of the QoL was 67.24%±9.91%. This difference is of high statistical significance (Table 1).
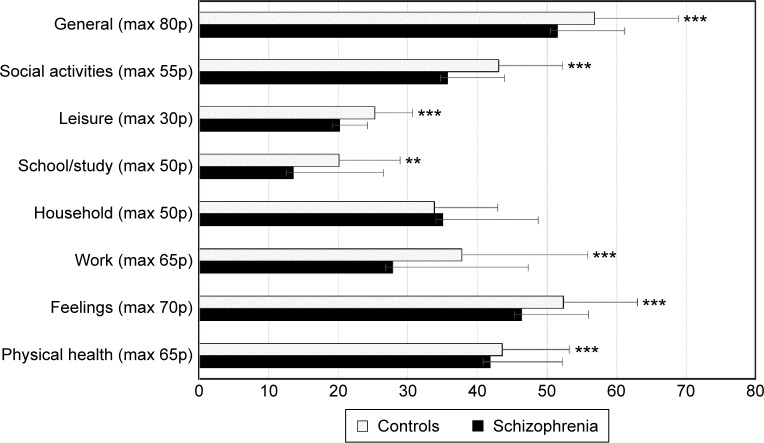
The groups of the patients and controls statistically differ in the mean age (controls were younger) but did not differ in sex ratio or the level of education. There were a statistically significant lower number of individuals without a partner and occupation in the patients group than in the control group (Table 1). The QoL was statistically significantly lower in domains such as physical health, feelings, work, school/study, leisure time, social activities, and general of Q-less-Q questionnaire in patients than in controls (Table 1 and Figure 1). The groups did not significantly differ only in the “household” domain. There was also a statistically significant difference between the sum of Q-LES-Q evaluated by the percentage of the maximum in patients with schizophrenia compared with the healthy control group (Table 1).
Figure 1.
Q-LES-Q domains in the controls and the patients.
Notes: Statistically significant relation is marked by *: **P<0.01; ***P<0.001.
Abbreviations: max, maximum; p, points; Q-LES-Q, Quality of Life Satisfaction and Enjoyment Questionnaire.
Relation between the QoL and demographic and clinical variables
The sum of Q-LES-Q and most of the domains of Q-LES-Q (the domain “school/study” was the only exception) correlated only with the objective and subjective assessment of the severity of the disorder (objCGI and subCGI) but not with other demographic or clinical variables such as age, age of the onset of the disorder, duration of the disorder, or the number of previous psychiatric hospitalizations (Table 3).
Table 3.
Correlations between quality of life and demographic and clinical variables
| Domain | Age | Onset | Length | objCGI | subCGI | objCGI–subCGI | Hospital |
|---|---|---|---|---|---|---|---|
| Physical health | −0.87 | 0.126 | −0.217* | −0.315*** | −0.478*** | 0.256* | 0.047 |
| Feelings | 0.12 | 0.108 | −0.112 | −0.307** | −0.540*** | 0.343** | 0.029 |
| Work | −0.173 | −0.087 | −0.095 | −0.279** | −0.383*** | 0.193 | −0.109 |
| Household | −0.071 | 0.004 | −0.128 | −0.327*** | −0.416*** | 0.259* | −0.150 |
| School/study | −0.147 | −0.105 | −0.098 | 0.059 | −0.169 | 0.104 | −0.044 |
| Leisure | 0.042 | 0.108 | −0.072 | −0.289** | −0.374*** | 0.167 | −0.088 |
| Social activities | −0.089 | 0.090 | −0.166 | −0.374*** | −0.369*** | −0.002 | −0.102 |
| General | 0.043 | 0.184 | −0.137 | −0.377*** | −0.492*** | 0.226* | −0.017 |
| Sum of Q-LES-Q | −0.101 | 0.059 | −0.180 | −0.423*** | −0.581*** | 0.279** | −0.075 |
Notes: Statistically significant relation is marked by*:
P<0.05;
P<0.01;
P<0.001.
Abbreviations: CGI, Clinical Global Impression; objCGI, objective CGI; Q-LES-Q, Quality of Life Satisfaction and Enjoyment Questionnaire; subCGI, subjective CGI.
Relation between self-stigma and demographic factors
The overall score of self-stigma correlated statistically significantly with the subCGI and was on the border of significance with the length of the disorder. From the subscales of ISMI, the perceived discrimination subscale correlates significantly with the onset of the disorder (negatively: earlier onset – more perceived discrimination) and with a number of hospitalizations, objective and subjective global impression about the severity of the disorder (all positively). subCGI correlates with all subscales of ISMI (Table 2). The statistically significant negative relation was found between subjective and objective actual severity of psychopathology and self-stigmatization. The larger difference in the assessment of the current severity of psychopathology between patient and doctor leads to lower self-stigmatization by patients.
Relation between QoL and self-stigma
The overall score of ISMI correlated highly significantly with all domains of Q-LES-Q except school/study (there were only a few students). The same situation was with all subscales of ISMI except domain work. There were two subscales, namely, perceived discrimination and stigma resistance, that both did not correlate (Table 4).
Table 4.
Relation between Q-LES-Q domains and facets of ISMI
| Domain | Overall score of ISMI | Alienation | Stereotype agreement | Perceived discrimination | Social withdrawal | Stigma resistance |
|---|---|---|---|---|---|---|
| Physical health | −0.496*** | −0.397*** | −0.509*** | −0.372*** | −0.454*** | −0.349*** |
| Feelings | −0.633*** | −0.535*** | −0.588*** | −0.469*** | −0.561*** | −0.413*** |
| Work | −0.261** | −0.202* | −0.246* | −0.141 | −0.258** | −0.106 |
| Household | −0.355*** | −0.278** | −0.350*** | −0.294** | −0.311*** | −0.268** |
| School/study | −0.099 | −0.069 | −0.073 | −0.078 | −0.103 | −0.100 |
| Leisure | −0.457*** | −0.430*** | −0.411*** | −0.347*** | −0.410*** | −0.293** |
| Social activities | −0.507*** | −0.391*** | −0.438*** | −0.390*** | −0.555*** | −0.235* |
| General | −0.550*** | −0.487*** | −0.487*** | −0.444*** | −0.504*** | −0.316*** |
| Sum of Q-LES-Q | −0.581*** | −0.477*** | −0.540*** | −0.429*** | −0.548*** | −0.355*** |
Notes:
P<0.05;
P<0.01;
P<0.001.
Abbreviations: ISMI, Internalized Stigma of Mental Illness; Q-LES-Q, Quality of Life Satisfaction and Enjoyment Questionnaire.
Regression analysis
Because of the numerous aspects significantly related to the overall score of Q-LES-Q, a multiple regression analysis was performed to identify the most important factors connected to the QoL in patients with schizophrenia. The dependent variable was the overall score of the Q-LES-Q. The independent variables were the overall objective severity of mental disorder, objCGI, subCGI, difference between objCGI and subCGI, overall rating of ISMI, age, length, onset, and the number of underwent psychiatric hospitalizations. The method we applied was a stepwise regression analysis. The most significant factors connected to the overall QoL measured by Q-LES-Q were the overall score of self-stigma by ISMI, objective overall severity of mental disorder measured by objCGI, subjective overall severity of the disorder measured by subCGI, and the age of the onset of the disorder, which totally explained 49.2% of the Q-LES-Q scores (P<0.001; Table 5).
Table 5.
Multiple regression analysis with the overall score of Q-LES-Q as a dependent variable
| Regressors | B (regression coefficient) | SE | Beta | Significance |
|---|---|---|---|---|
| ISMI | −2.574 | 0.404 | −0.600 | P<0.001 |
| objCGI | −19.425 | 5.714 | −0.302 | P<0.001 |
| subCGI | −11.698 | 5.192 | −0.260 | P<0.05 |
| Onset of disorder | −1.316 | 0.606 | −0.187 | P<0.05 |
Abbreviations: CGI, Clinical Global Impression; ISMI, Internalized Stigma of Mental Illness; objCGI, objective CGI; Q-LES-Q, Quality of Life Satisfaction and Enjoyment Questionnaire; SE, standard error; subCGI, subjective CGI.
Discussion
The aim of the study was to compare the QoL in patients with schizophrenia spectrum disorder and healthy controls. Like in other investigations, the sum of the QoL in patients was lower than in healthy controls.9,29 This result has the limitation; there is the different mean age of the patients and controls in our study. Age could be a factor, which can influence the QoL according to some authors.30 On the other hand, there is no correlation between patient age and the sum of Q-LES-Q or any domains of the Q-LES-Q in our sample (Table 3). Statistical analysis revealed differences in all the Q-LES-Q domains except the household domain. This result was partly in agreement with the outcome of the study by Sidlova et al,9 where patients with schizophrenia reported lower QoL in the domains such as physical health, feelings, leisure, and general. The aforementioned study did not report the differences in domains of “social activities”, what we found contrary in our study. The discrepancies in the results can be explained by the higher mean age of the patients in the present study (but in linear regression analysis, there were no correlations between the age of our patients and level of Q-LES-Q) or by lower level of education in patients reported in the study by Sidlova et al.9 The other possible explanation for the different results could be the fact that in the study by Sidlova et al.9 There were not enough patients for an adequate detection of the differences in the mentioned domains (the mean scores were considerably higher in controls).
The second aim was to search the relation between the QoL and self-stigma. The results show that the level of the self-stigma was significantly negatively correlated with the QoL. The same result was described by Tang and Wu31 in the same population. The authors found that self-stigma of patients with schizophrenia negatively correlated with all domains of the QoL. The question is, if the QoL is changed by self-stigma, or it leads to the decrease in the QoL, or if the low QoL predicts a higher level of self-stigma. Longitudinal studies are needed to answer this question.
The QoL also highly depended on the degree of severity of the disorder. The self-stigma and severity of disorder markedly positively correlated with each other. The stepwise regression analysis was used to understand the influence of these two factors. The stepwise regression analysis showed that these factors together explained 47% of the variance of the sum of the QoL.
The level of self-stigma in patients with schizophrenia spectrum disorders was similar to the level in patients suffering from other mental disorders in which it was measured.26 In the context of self-stigma, there was no evidence of a relationship between the age of the onset of disease, duration of disorder (which only indicated a trend), the number of previous hospitalizations (however, a subscale of ISMI “perceived discrimination” significantly correlated), sex, marital status, and education. These findings partly correspond with the findings of Vrbová et al32 and Gerlinger et al,33 which showed that sex, partnership, heredity, and education are not statistically significantly related to the degree of self-stigma. Kamaradova et al34 found that the level of self-stigma among men and women does not differ, what is also confirmed in the present study. The rate of self-stigma was significantly associated with the employment. Unemployed people showed a higher degree of self-stigma (groups with and without job differed in the subscales such as agreement with stereotypes, perceived discrimination, and social withdrawal). These results are in agreement with the findings of Tiggemann and Winefield,35 the study of rates of depression, negative mood, and lower self-esteem in unemployment patients. The results of our study are also in agreement with the outcome of a study by Adewuya et al.36 The authors suggested that the high degree of the self-stigma was significantly linked to the unemployment status of the people with mental disorders.
There was no significant relationship between actual severity of the disorder and an overall score of self-stigma, but the score of perceived discrimination subscale positively correlated with an objCGI as well as a subCGI rating of disorder severity. The latter means that people who perceived themselves as discriminated evaluated their disorder as more severe, or conversely, people with higher severity of disorder felt more discriminated. An important connection was found between subjectively assessed severity of the illness and all subscales of ISMI (mostly in agreement with stereotypes, social withdrawal, and alienation). Patients who evaluated their current severity of the disease as more serious stigmatized themselves more than patients who evaluated their disorder as less severe. It is hard to say the direction of these relations from the correlation study. Both directions are possible – patients who feel themselves more seriously ill can consequently believe that others look on them in the same way and that is why they are critical to them, which may lead to isolation from the people. The opposite direction could be that isolated patients who agree with the stereotypes feel themselves as more seriously disordered.
Other findings pointed to the difference between subCGI, objCGI, and self-stigmatization. The larger difference in the assessment of the current severity of psychopathology between patient and doctor leads to the lower self-stigmatization by patients. These finding could be explained by feeling healthier with denial of the current condition or lower insight, which is reflected in lower recognition of the severity of the disorder, measured by the subjective severity of the disorder by subCGI. This could result in self-stigmatization of patients and greater differences between subCGI and objCGI scores, which was evaluated by the psychiatrist.
Our data revealed that many factors correlated with Q-LES-Q scores. The stepwise regression analysis showed that the overall rating of ISMI, objCGI, subCGI, and the onset of the disorder correlated with Q-LES-Q score to the highest extent.
There was also a significant relationship between QoL and self-stigma. Individuals, who perceived themselves as more stigmatized, evaluated their QoL as lower and vice versa. However, it is not possible to precisely explain the relationships between these two variables within the cross-sectional design of this study.
Limitations
The main limitation of the study is using the self-report scales and questionnaires, since filling the questionnaire can be significantly affected by the current state of the patient. This applies mainly to the questionnaire evaluating the QoL. In addition, the severity of illness was assessed only by the global clinical evaluation, using no symptom-specific objective assessment instruments. Finally, the research consists of a small sample size. Nevertheless, the results shed light on the important topic of the QoL for the patients suffering from schizophrenia spectrum disorders.
Conclusion
Self-stigma and QoL could be reflected as important factors for patients who suffer from schizophrenia spectrum disorders, their caregivers, and mental health specialists. The outcomes of the study showed a lower level of QoL in patients compared with healthy controls in almost all measured domains. Patients with a higher degree of self-stigma reported a lower standard of QoL and a greater degree of the severity of the disorder. Subjects with early onset of disorder perceived higher discrimination from others. Our data suggest the importance of the subsequent research and longitudinal evaluation of psychopathological symptoms and their influence on the subjectively perceived QoL during the disorder. In addition, answering the question, whether and how the QoL could change after the therapy, remains the significant challenge for research in the future.
Acknowledgments
The authors thank the willing cooperation of Engineer Miloš Čejka from Hradec Králové, Master Václav Holub from Liberec, Dr Jiří Rozkoš from Prostějov, Dr Jan Flídr from Kralupy nad Vltavou, Dr Jana Matějková from Prague, Dr Simona Papežové from Prague, Dr Pavel Tautermann from Prague, Dr Markéta Zemanová from Havlíčkův Brod, Dr Markéta Dobrá from Hrabyně, Dr Zuzana Kozáková from Trutnov (RIAPS association), Dr Tibor Miklóš from Prague, Dr Michaela Zapletalová from Chomutov, Dr Jana Novosadová from Blansko, Dr Jiří Trska from Týn nad Vltavou, Dr Zdeněk Holoubek from Nymburk, Dr Iva Ondráčková from Prague, Dr Andrea Bryčková from Hořice, Dr Jindřiška Masnerová from Beroun, Dr Petr Pastucha from Prostějov, and Dr Hana Lemanová from Brno.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Marwaha S, Johnson S. Schizophrenia and employment – a review. Soc Psychiatry Psychiatr Epidemiol. 2004;39(5):337–349. doi: 10.1007/s00127-004-0762-4. [DOI] [PubMed] [Google Scholar]
- 2.Karagianis J, Novick D, Pecenak J, et al. Worldwide-schizophrenia outpatient health outcomes (W-SOHO): baseline characteristics of pan-regional observational data from more than 17,000 patients. Int J Clin Pract. 2009;63(11):1578–1588. doi: 10.1111/j.1742-1241.2009.02191.x. [DOI] [PubMed] [Google Scholar]
- 3.Remberk B, Hintze B, Rybakowski F. Executive functioning improves after remission of psychosis and may not deteriorate at short follow-up in early-onset schizophrenia. Neuro Endocrinol Lett. 2015;36(2):153–160. [PubMed] [Google Scholar]
- 4.Browne S, Roe M, Lane A, et al. Quality of life in schizophrenia: relationship to sociodemographic factors, symptomatology, and tardive dyskinesia. Acta Psychiatr Scand. 1996;94:118–124. doi: 10.1111/j.1600-0447.1996.tb09835.x. [DOI] [PubMed] [Google Scholar]
- 5.Skantze K, Malm U, Dencker SJ, May PR, Corrigan P. Comparison of the quality of life with standard of living in schizophrenic out-patients. Br J Psychiatry. 1992;161:797–801. doi: 10.1192/bjp.161.6.797. [DOI] [PubMed] [Google Scholar]
- 6.Wegener S, Redoblado-Hodge MA, Lucas S, Fitzgerald D, Harris A, Brennan J. Relative contributions of psychiatric symptoms and neuropsychological functioning to quality of life in first-episode psychosis. Aust N Z J Psychiatry. 2005;39:487–492. doi: 10.1080/j.1440-1614.2005.01608.x. [DOI] [PubMed] [Google Scholar]
- 7.Ritsner M, Kurs R, Gibel A, Ratner Y, Endicott J. Validity of an abbreviated quality of life enjoyment and satisfaction questionnaire (Q-LES-Q-18) for schizophrenia, schizoaffective, and mood disorder patients. Qual Life Res. 2005;14:1693–1703. doi: 10.1007/s11136-005-2816-9. [DOI] [PubMed] [Google Scholar]
- 8.Yamauchi K, Aki H, Tomotake M, et al. Predictors of subjective and objective quality of life in outpatients with schizophrenia. Psychiatry Clin Neurosci. 2008;62:404–411. doi: 10.1111/j.1440-1819.2008.01818.x. [DOI] [PubMed] [Google Scholar]
- 9.Sidlova M, Prasko J, Jelenova D, et al. The quality of life of patients suffering from schizophrenia – a comparison with healthy controls. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2011;155(2):173–180. doi: 10.5507/bp.2011.010. [DOI] [PubMed] [Google Scholar]
- 10.Latalova K, Prasko J, Diveky T, Kamaradova D, Velartova H. Quality of life in patients with bipolar disorder – a comparison with schizophrenic patients and healthy controls. Psychiatr Danub. 2011;23(1):21–26. [PubMed] [Google Scholar]
- 11.Herrman H, Hawthorne G, Thomas R. Quality of life assessment in people living with psychosis. Soc Psychiatry Psychiatr Epidemiol. 2002;37(11):510–518. doi: 10.1007/s00127-002-0587-y. [DOI] [PubMed] [Google Scholar]
- 12.Karow A, Naber D. Subjective well-being and quality of life under atypical antipsychotic treatment. Psychopharmacology (Berl) 2002;162(1):3–10. doi: 10.1007/s00213-002-1052-z. [DOI] [PubMed] [Google Scholar]
- 13.Awad AG, Voruganti LNP. The impact of atypical antipsychotics on quality of life in patients with schizophrenia. CNS Drugs. 2004;18(13):877–893. doi: 10.2165/00023210-200418130-00004. [DOI] [PubMed] [Google Scholar]
- 14.Awad AG, Voruganti LNP. Measuring quality of life in patients with schizophrenia: an update. Pharmacoeconomics. 2012;30(3):183–195. doi: 10.2165/11594470-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 15.Lehman AF. The effects of psychiatric symptoms on quality of life assessments among the chronic mentally ill. Eval Program Plann. 1983;6:143–151. doi: 10.1016/0149-7189(83)90028-9. [DOI] [PubMed] [Google Scholar]
- 16.Boyer L, Baumstarck K, Boucekine M, Blanc J, Lançon C, Auquier P. Measuring quality of life in patients with schizophrenia: an overview. Expert Rev Pharmacoecon Outcomes Res. 2013;13(3):343–349. doi: 10.1586/erp.13.15. [DOI] [PubMed] [Google Scholar]
- 17.Livingston JD, Boyd JE. Correlates and consequences of internalized stigma for people living with mental illness: a systematic review and meta-analysis. Soc Sci Med. 2010;71:2150–2161. doi: 10.1016/j.socscimed.2010.09.030. [DOI] [PubMed] [Google Scholar]
- 18.Corrigan PW, Rafacz J, Rüsch N. Examining a progressive model of self-stigma and its impact on people with serious mental illness. Psychiatry Res. 2011;189:339–343. doi: 10.1016/j.psychres.2011.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Corrigan PW, Watson AC, Barr L. Understanding the self-stigma of mental illness. J Soc Clin Psychol. 2006;25:875–884. [Google Scholar]
- 20.Schulze B, Angermeyer MC. Subjective experiences of stigma: a focus group study of schizophrenic patients, their relatives, and mental health professionals. Soc Sci Med. 2003;56:299–312. doi: 10.1016/s0277-9536(02)00028-x. [DOI] [PubMed] [Google Scholar]
- 21.Ritsher JB, Phelan JC. Internalized stigma predicts the erosion of morale among psychiatric outpatients. Psychiatry Res. 2004;129:257–265. doi: 10.1016/j.psychres.2004.08.003. [DOI] [PubMed] [Google Scholar]
- 22.Tsang HW, Fung KM, Chung RC. Self-stigma and stages of change as predictors of treatment adherence of individuals with schizophrenia. Psychiatry Res. 2010;180(1):10–15. doi: 10.1016/j.psychres.2009.09.001. [DOI] [PubMed] [Google Scholar]
- 23.World Health Organization . The ICD-10 Classification of Mental and Behavioral Disorders: Diagnostic Criteria for Research. Geneva: World Health Organization; 1993. [Google Scholar]
- 24.Müllerova H. Mezikulturní přenos a validace dotazníku kvality života Q-LES-Q [Transcultural transmission and validation of the quality life questionnaire Q-LES-Q] Psychiatrie. 2001;5:80–87. [Google Scholar]
- 25.Ritsner M, Ben-Avi I, Ponizovsky A, Timinsky I, Bistrov E, Modai I. Quality of life and coping with schizophrenia symptoms. Qual Life Res. 2003;12(1):1–9. doi: 10.1023/a:1022049111822. [DOI] [PubMed] [Google Scholar]
- 26.Ociskova M, Prasko J, Vrbova K, Kamaradova D, Jelenova D, Latalova K. Stigma and self-stigma in patients with schizophrenia. Česká Slov Psychiatr. 2014;110(5):250–258. [Google Scholar]
- 27.Guy W. ECDEU Assessment Manual for Psychopharmacology. Rockville, MD: US Department of Health, Education, and Welfare; 1976. [Google Scholar]
- 28.WMA Declaration of Helsinki - Ethical Principles for Medical Research Involving Human Subjects [webpage on the Internet] 64th WMA General Assembly, Fortaleza, Brazil, October 2013. World Medical Association, Inc; 2016. Available from: http://www.wma.net/en/30publications/10policies/b3/ [Google Scholar]
- 29.Bobes J, Garcia-Portilla MP, Bascaran MT, Saiz PA, Bousoño M. Quality of life in schizophrenic patients. Dialogues Clin Neurosci. 2007;9(2):215–226. doi: 10.31887/DCNS.2007.9.2/jbobes. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Evans S, Huxley P, Priebe S. A comparison of the quality of life of severely mentally ill people in UK & German samples. Int J Soc Psychiatry. 2000;46(1):47–56. doi: 10.1177/002076400004600106. [DOI] [PubMed] [Google Scholar]
- 31.Tang IC, Wu HC. Quality of life and self-stigma in individuals with schizophrenia. Psychiatr Q. 2012;83(4):497–507. doi: 10.1007/s11126-012-9218-2. [DOI] [PubMed] [Google Scholar]
- 32.Vrbová K, Kamarádová D, Látalová K, et al. Self-stigma and adherence to medication in patients with psychotic disorders – cross-sectional study. Neuro Endocrinol Lett. 2014;35(7):645–652. [PubMed] [Google Scholar]
- 33.Gerlinger G, Hauser M, De Hert M, Lacluyse K, Wampers M, Correll CU. Personal stigma in schizophrenia spectrum disorders: a systematic review of prevalence rates, correlates, impact and interventions. World Psychiatry. 2013;12:155–164. doi: 10.1002/wps.20040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kamaradova D, Latalova K, Prasko J, et al. Sebestigmatizace, adherence kléčbě a vysazování medikace u psychických poruch – průřezová studie [Self-stigma, adherence to treatment and withdrawal of medication in psychiatric disorders – a cross-sectional study] Psychiatrie. 2015;19(4):175–183. [Google Scholar]
- 35.Tiggemann M, Winefield AH. The effects of unemployment on the mood, self-esteem, locus of control, and depressive affect of school-leavers. J Occup Psychol. 2011;57(1):33–42. [Google Scholar]
- 36.Adewuya AO, Owoeye AO, Erinfolami AO, Ola BA. Correlates of self-stigma among outpatients with mental illness in Lagos, Nigeria. Int J Soc Psychiatry. 2011;57(4):418–427. doi: 10.1177/0020764010363522. [DOI] [PubMed] [Google Scholar]