Abstract
Study Objective
To investigate whether Type O blood group status is associated with increased intraoperative blood loss and requirement of blood transfusion in extensive spine surgery.
Design
Retrospective comparative study.
Setting
University-affiliated, non-profit teaching hospital.
Measurements
Data from 1,050 ASA physical status 1, 2, 3, 4, and 5 patients who underwent spine surgeries involving 4 or more vertebral levels were analyzed. Patients with Type O blood were matched to similar patients with other blood types using propensity scores, which were estimated via demographic and morphometric data, medical history variables, and extent of surgery. Intraoperative estimated blood loss (EBL) was compared among matched patients using a linear regression model; intraoperative transfusion requirement in volume of red blood cells, fresh frozen plasma, platelet, cryoprecipitate, cell salvaged blood, volume of intraoperative infusion of hetastarch, 5% albumin, crystalloids, and hospital length of hospital (LOS) were compared using Wilcoxon rank-sum tests.
Main Results
Intraoperative EBL and requirement of blood product transfusion were similar in patients with Type O blood group and those with other blood groups.
Conclusion
There was no association between Type O blood and increased intraoperative blood loss or blood transfusion requirement during extensive spine surgery, with similar hospital LOS in Type O and non-O patients.
Keywords: Blood loss, surgical; Blood salvage, intraoperative; Hemodilution; Transfusion; Type O blood
1. Introduction
Individuals with Type O blood have smaller amounts of circulating factor VIII/von Willebrand Factor (vWF) than those with other blood groups [1,2]. Quiroga et al [3] investigated more than 500 patients who presented with mucocutaneous hemorrhage and reported that the proportion of individuals with Type O blood was higher in those patients than in the normal population. Similarly, Type O blood has been associated with decreased risk of venous thromboembolism [4].
In complex spine surgery accompanied by large blood loss, significant hemodilution occurs as a result of intravascular volume replacement with crystalloid and colloid solutions. Because of its initially lower concentration, vWF concentration may decrease to levels that impair hemostasis in patients with Type O blood compared with those of other blood types [5]. Therefore, patients with Type O blood may plausibly lose more blood than those with other blood types, and consequently require more blood product transfusion.
It was hypothesized that intraoperative estimated blood loss (EBL) during extensive spine surgery is greater in patients who have Type O blood than in those of other blood groups. Secondary hypotheses were that patients with Type O blood required more intraoperative packed red blood cell (PRBC) transfusion, fresh frozen plasma (FFP) transfusion, and cryoprecipitate transfusion, platelet transfusion, and required longer hospitalization than those of other blood groups.
2. Materials and methods
With Institutional Review Board (IRB) approval from the Cleveland Clinic, the Perioperative Health Documentation System at the Cleveland Clinic was queried for all patients who had extensive spine surgery (≥ 4 levels) between April 1, 2005 and August 17, 2011. The requirement for written, informed consent was waived by the IRB. A manual chart review was conducted for patients in whom blood type, EBL, or demographic/morphometric data (aside from laboratory measurements) were missing from our registry. Patients with missing data in both the registry and charts were excluded from analysis.
2.1. Statistical analysis
Each Type O patient was matched to a similar patient with any other blood type via exact matching on propensity score, rounded to the nearest 0.01. The propensity scores were estimated via a multivariable logistic regression model that included year of surgery, age, gender, race (African American, Caucasian, or other), body mass index, ASA physical status, emergency status, number of levels operated on, surgical approach (anterior vs posterior), previous spine surgery, and various medical history variables (hypertension, chronic obstructive pulmonary disease, coronary artery disease, congestive heart failure, diabetes mellitus, renal insufficiency, and cerebrovascular accident). The number of vertebral levels operated was divided into 4–8 levels and ≥ 9 levels because it was the categorization used by Perioperative Health Documentation System at the Cleveland Clinic. Baseline laboratory measurements were not included in the propensity matching procedure due to the high incidence of missing data; however, a sensitivity analysis was performed that did include these measurements in the matching.
In the primary comparison of EBL among matched patients, a linear regression model was used to adjust for any of the above-listed baseline variables (excluding laboratory variables) that were not adequately balanced after the propensity matching procedure. Balance was assessed using absolute standardized difference (ASD) scores, which were defined as the difference in means, mean rankings, or proportions, divided by a pooled estimate of standard deviation. Variables exhibiting an ASD greater than 0.1 standard deviations (SDs) between the two groups after matching were included for adjustment in the linear regression model.
The authors anticipated that the distribution of EBL was right-skewed; as such, patients with large amounts of blood loss may unduly influence regression parameter estimates. A common approach to minimizing the over-influence of outlying observations with respect to EBL is to use a normalizing transformation. With right-skewed variables, the logarithmic transformation is often used. The EBL outcomes were transformed using the logarithm prior to modeling so as to correct for skewness in the distribution. This had the effect of changing the interpretation of the treatment effect of interest from one estimating the difference in arithmetic mean EBL between blood type groups to one estimating the percentage difference in geometric means between blood type groups.
Secondary outcomes were summarized among the matched patients using univariable descriptive statistics and evaluated for group differences using Wilcoxon rank-sum tests.
R statistical software version 2.14.1 (R Foundation for Statistical Computing, Vienna, Austria) was used to perform the analysis. The Type I error rate for all hypotheses was fixed at 0.05. Post-hoc power analysis indicated that we had 90% power to detect a percentage difference in geometric means of 24% or greater between Type O patients and patients with other blood types.
3. Results
After the manual chart review, blood type remained unavailable for two patients, and EBL remained unavailable for another. Similarly, certain demographic and medical history data remained unavailable for 23 additional patients. Thus, 1,296 patients were available for propensity score matching (Fig. 1).
Fig. 1.
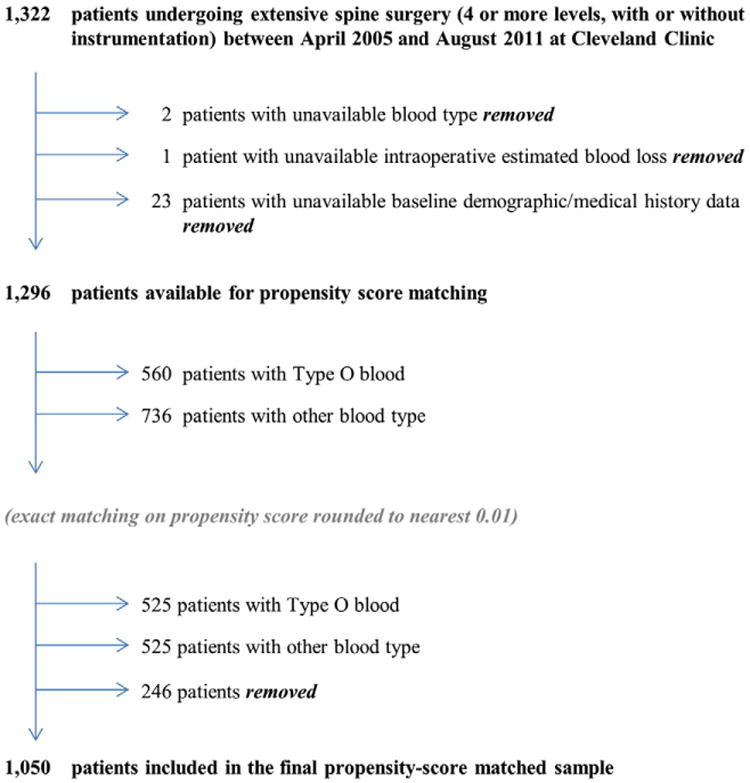
Study flow diagram.
The propensity score matching procedure yielded 525 successful matched pairs, with 35/560 (6.3%) of Type O patients removed from the analysis for lack of a comparable control patient. Baseline and operative variables were excellently balanced among the matched subset (Table 1), as evidenced by the fact that variables included in the propensity score model had an ASD of < 0.1 SD. Propensity scores were 0.44 ± 0.06 in both groups after matching; these values were similar to propensity scores prior to matching (0.44 ± 0.07 and 0.42 ± 0.07), and being close to 0.5 was indicative of general lack of potential confounding of data.
Table 1. Balance of baseline characteristics before and after propensity score matching.
| Factor | All patients | Matched patients | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Type O | Other | ASD | Type O | Other | ASD | |
|
|
|
|
|
|||
| (N=560) | (N=736) | (N=525) | (N=525) | |||
| Year of surgery | 2008.0 ± 1.7 | 2008.3 ± 1.7 | 0.16 | 2008.0 ± 1.7 | 2008.1 ± 1.6 | 0.03 |
| Age (yrs) | 49 ± 23 | 50 ± 23 | 0.06 | 49 ± 22 | 49 ± 23 | 0.01 |
| Male gender | 44.6 | 45.2 | 0.01 | 43.6 | 44.8 | 0.02 |
| Race | ||||||
| African American | 13.6 | 9.9 | 0.15 | 11.2 | 12 | 0.03 |
| Caucasian | 81.4 | 87 | 85.5 | 84.4 | ||
| Other | 5 | 3.1 | 3.2 | 3.6 | ||
| BMI (kg/m2) | 27 ± 7 | 27 ± 7 | 0.03 | 27 ± 7 | 27 ± 7 | 0.08 |
| ASA physical status | ||||||
| 1/2 | 44 | 42 | 0.09 | 45 | 45 | 0.07 |
| 3 | 52 | 52 | 51 | 50 | ||
| 4/5 | 4 | 5 | 4 | 6 | ||
| Emergency surgery | 2 | 2 | 0.05 | 2 | 2 | 0.04 |
| Levels, n (≥ 9 vs 4–8 levels) | 26 | 23 | 0.06 | 25 | 24 | 0.02 |
| Surgical approach (posterior vs anterior) | 96 | 95 | 0.07 | 96 | 94 | 0.08 |
| Reoperation | 10 | 9 | 0.03 | 10 | 10 | 0.01 |
| Preop Hct (%) a | 41 ± 4 | 41 ± 4 | 0.00 | 41 ± 4 | 41 ± 4 | 0.04 |
| Preop Hb (g/dL) a | 13.4 ± 1.7 | 13.4 ± 1.6 | 0.01 | 13.4 ± 1.7 | 13.5 ± 1.6 | 0.02 |
| Preop platelets (×109/L) a | 250 [211, 300] | 251 [206, 305] | 0.02 | 250 [210, 299] | 252 [205, 309] | 0.01 |
| Preop PT (sec) a | 10.9 [10.5, 11.3] | 10.9 [10.6, 11.3] | 0.05 | 10.9 [10.5, 11.3] | 10.9 [10.6, 11.3] | 0.09 |
| Preop aPTT (sec) a | 30 [28, 31] | 28 [27, 30] | 0.33 | 30 [28, 31] | 29 [27, 31] | 0.28 |
| Preop PT (INR)a | 1.0 [0.9, 1.0] | 1.0 [0.9, 1.0] | 0.10 | 1.0 [0.9, 1.0] | 1.0 [0.9, 1.0] | 0.13 |
| Preop WBC count (×109/L)a | 6.7 [5.5, 8.2] | 6.9 [5.7, 8.4] | 0.10 | 6.7 [5.5, 8.2] | 6.8 [5.6, 8.4] | 0.08 |
| Preop creatinine (mg/dL) a | 0.8 [0.7, 0.9] | 0.8 [0.7, 1.0] | 0.04 | 0.8 [0.7, 0.9] | 0.8 [0.6, 0.9] | 0.02 |
| Preop BUN (mg/dL) a | 15 [11, 19] | 15 [12, 20] | 0.07 | 15 [11, 19] | 15 [11, 19] | 0.00 |
| Hypertension history | 41 | 45 | 0.08 | 42 | 42 | 0.02 |
| COPD history | 16 | 13 | 0.09 | 14 | 14 | 0.00 |
| CAD history | 9 | 14 | 0.16 | 9 | 8 | 0.03 |
| CHF history | 3 | 4 | 0.07 | 3 | 3 | 0.03 |
| Diabetes Mellitus history | 11 | 14 | 0.10 | 11 | 12 | 0.04 |
| Renal insufficiency history | 5 | 5 | 0.00 | 5 | 4 | 0.04 |
| CVA history | 2 | 2 | 0.03 | 2 | 2 | 0.06 |
| Propensity score | 0.44 ± 0.07 | 0.42 ± 0.07 | 0.29 | 0.44 ± 0.06 | 0.44 ± 0.06 | 0.00 |
Summary statistics for each group are presented as means (±SD) medians (1st and 3rd quartiles), or numbers (%), as appropriate. Absolute standardized difference (ASD) scores, defined as the difference in means, mean rankings, or proportions divided by a pooled estimate of standard deviation, are given both before and after matching. No variable included in the propensity score model was more than 0.1 standard deviations apart (ASD > 0.1) after matching. Many baseline laboratory measurements (which were excluded from the propensity score model due to high frequency of missing values) were well balanced. BMI=body mass index, preop=preoperative, Hct=hematocrit, Hb=hemoglobin, PT=prothrombin time, aPTT=activated partial thromboplastin time, INR=international normalized ratio, WBC=white blood cells, BUN=blood, urea, nitrogen, COPD=chronic obstructive pulmonary disease, CAD=coronary artery disease, CHF=congestive heart failure, CVA=cerebrovascular accident.
Variables excluded from the matching procedure.
Geometric mean EBL [95% confidence interval (CI)] was 762 [690 – 841] mL for matched Type O patients and 727 [658 – 803] mL for matched patients with other blood types, corresponding to an estimated percent difference in means [95% CI] of +4.8% [−8.9%, +20.6%] (P = 0.51, Wald test). In the sensitivity analysis, which incorporated laboratory measurements in the propensity matching procedure, similar results occurred (estimated percent difference in means of +4.3% [−14.2% +26.8%] among 320 matched pairs). Secondary outcomes were similar between matched Type O patients and matched patients with other blood types (Table 2).
Table 2. Selected quantiles of secondary outcomes by group (in mL unless otherwise noted), and associated Wilcoxon rank-sum test P-values.
| Fluid Type | Min | 1st decile | 2nd decile | 3rd decile | 4th decile | Median decile | 6th decile | 7th decile | 8th decile | 9th decile | Max | P-value | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| RBCs | Type O | 0 | 0 | 0 | 0 | 0 | 0 | 320 | 426 | 731 | 1224 | 4030 | |
| Other | 0 | 0 | 0 | 0 | 0 | 0 | 284 | 372 | 692 | 1060 | 4700 | 0.49 | |
| FFP | Type O | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 251 | 2785 | |
| Other | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1499 | 0.35 | |
| Platelets | Type O | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1006 | |
| Other | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 937 | 0.71 | |
| Cryoprecipitate | Type O | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 265 | |
| Other | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 242 | 0.99 | |
| Cell Saver | Type O | 0 | 0 | 0 | 0 | 0 | 0 | 143 | 425 | 715 | 1151 | 4569 | |
| Other | 0 | 0 | 0 | 0 | 0 | 0 | 133 | 303 | 589 | 1073 | 4533 | 0.13 | |
| Hetastarch | Type O | 0 | 0 | 0 | 500 | 500 | 1000 | 1000 | 1000 | 1000 | 1500 | 2000 | |
| Other | 0 | 0 | 0 | 500 | 500 | 500 | 1000 | 1000 | 1000 | 1500 | 2000 | 0.51 | |
| Albumin 5% | Type O | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 500 | 750 | 1000 | 2500 | |
| Other | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 500 | 500 | 1000 | 2500 | 0.67 | |
| Total crystalloids | Type O | 300 | 2400 | 2900 | 3200 | 3900 | 4300 | 4900 | 5500 | 6200 | 7130 | 16700 | |
| Other | 640 | 2500 | 3000 | 3400 | 3800 | 4200 | 4700 | 5100 | 6000 | 7070 | 13200 | 0.67 | |
| Hospital LOS (days) | Type O | 0.6 | 2.7 | 3.4 | 4.3 | 4.7 | 5.4 | 6.2 | 6.7 | 7.5 | 10.3 | 46.1 | |
| Other | 0.4 | 2.6 | 3.5 | 4.3 | 4.7 | 5.4 | 6.2 | 6.8 | 7.6 | 10.1 | 35.5 | 0.78 |
RBCs = red blood cells, FFP = fresh frozen plasma, Cell Saver® (Haemoneutics, Braintree, MA, USA), LOS = length of stay.
4. Discussion
The current study indicates that intraoperative requirement of blood products transfusion and EBL were not significantly different between blood Type O patients and those with other blood types undergoing extensive spine surgery. This study is the largest to date to evaluate this hypothesis, and based on the relatively narrow width of CIs, the likelihood that the authors did not detect a clinically important difference in EBL was low.
Two previous studies compared blood loss and transfusion requirement in patients with Type O and other blood types in spine surgery. Choi et al [6] studied lumbar spine surgery involving three or fewer vertebral levels with infusion of hydroxyethyl starch (HES) 15 mL/kg given at a rate of 10 mL/kg/hr. Factor VIII activity was lower and activated partial thromboplastin time (aPTT) was slightly prolonged in Type O patients compared with those with other blood types both at baseline and after infusion of HES. Intraoperative blood loss was 25% greater in patients with Type O blood; these patients required twice as much intraoperative red blood cell transfusion, although the differences did not reach statistical significance.
Kang et al [5] studied spine surgery consisting of more than two vertebral levels accompanied by acute normovo-lemic hemodilution with approximately 1,000 mL of blood deposition and roughly the same volume replacement with HES within one hour. At baseline, aPTT was slightly prolonged in Type O patients, and factor VIII activity and vWF antigen were lower at baseline and further decreased below normal range after acute normovolemic hemodilution in Type O patients. More blood was lost in patients with vWF antigen < 50%, but blood loss was similar in patients with Type O and other blood types.
Results from the current study were also consistent with Huraux et al [7], who studied 40 patients having abdominal surgeries ranging from herniorrhaphy to esophagectomy, in which blood loss varied from 0 to 1,800 mL, with no difference in postoperative blood loss between Type O patients and those with other blood types. However, the small number of patients in this study and the wide range of surgeries may have affected the accuracy with which the association between O blood type and blood loss was estimated. Welsby et al [8] also failed to show a significant difference in blood loss between Type O and non-O patients undergoing cardiac surgery, where hemodilutional and consumptive coagulopathy due to the use of cardiopulmonary bypass [9] is substantial. The study's results and available literature thus suggest that patients with Type O blood are not at special risk of bleeding.
After propensity score matching, surgical factors that affected bleeding were well balanced between patients with blood Type O and those with other blood types. Sensitivity analysis based on laboratory values did not suggest that they contribute substantively to our conclusions.
Patients included in the current study all had extensive surgery and typically were given intravenous fluids equaling their entire blood volume. Thus, they surely experienced substantial hemodilution, which presumably reduced circulating concentrations of factor VIII/vWF. Factor VIII/vWF may have been further reduced by the administration of HES [10,11], which stabilizes endothelial membranes, thus preventing vWF release and consequently reducing factor VIII [12]. The patients in the current study generally received only 500 to 1,000 mL of HES, which is less than in previous studies [5,6] and thus likely provoked less hemodilution of clotting factors. On the other hand, patients were given 6% HES (670/0.75), which decreases factor VIII activity and vWF antigen concentration more than 6% HES (130/0.4) [13]. Because of the retrospective nature of the study, the authors cannot determine whether factor VIII activity and vWF antigen concentration decreased by clinically important amounts in the patients.
Heterozygotes of O allele (genotypes AO and BO) have slightly lower concentrations of vWF antigen than non-O-carriers (genotype AA, BB, and AB), and homozygotes (genotype OO) have markedly lower concentrations [14]. Stratifying groups according to genotypes rather than phenotypes thus might better characterize the effects of vWF antigen level on surgical blood loss.
There are limitations to the current study. Due to the retrospective nature of the study, the potential confounding effect of other characteristics potentially influencing blood loss and transfusion practices that were not available in the registry were not included in propensity matching. Vertebral levels operated on were only categorized into two (ie, 4–8 and ≥ 9) levels, so that the possibility of imbalance in extent of surgery between the groups still remains. This was a single-center study of a specific type of surgery; results may differ in other settings and in other populations.
4.1. Conclusion
In summary, there was no association between Type O blood and increased intraoperative blood loss or blood transfusion requirement during extensive spine surgery, with similar hospital length of stay noted for Type O and non-O patients.
Footnotes
Supported by departmental funding only.
References
- 1.Souto JC, Almasy L, Muñiz-Diaz E, et al. Functional effects of the ABO locus polymorphism on plasma levels of von Willebrand factor, factor VIII, and activated partial thromboplastin time. Arterioscler Thromb Vasc Biol. 2000;20:2024–8. doi: 10.1161/01.atv.20.8.2024. [DOI] [PubMed] [Google Scholar]
- 2.O'Donnell J, Boulton FE, Manning RA, Laffan MA. Amount of H antigen expressed on circulating von Willebrand factor is modified by ABO blood group genotype and is a major determinant of plasma von Willebrand factor antigen levels. Arterioscler Thromb Vasc Biol. 2002;22:335–41. doi: 10.1161/hq0202.103997. [DOI] [PubMed] [Google Scholar]
- 3.Quiroga T, Pérez M, Rodríguez S, et al. Skin and mucous membrane hemorrhages: clinical assessment, study sequence and relative frequency of hereditary diseases of the hemostasis in a Chilean population. Rev Med Chil. 1997;125:409–18. [PubMed] [Google Scholar]
- 4.Ohira T, Cushman M, Tsai MY, et al. ABO blood group, other risk factors and incidence of venous thromboembolism: the Longitudinal Investigation of Thromboembolism Etiology (LITE) J Thromb Haemost. 2007;5:1455–61. doi: 10.1111/j.1538-7836.2007.02579.x. [DOI] [PubMed] [Google Scholar]
- 5.Kang JG, Ahn HJ, Kim GS, et al. The hemostatic profiles of patients with Type 0 and non-0 blood after acute normovolemic hemodilution with 6% hydroxyethyl starch (130/0.4) Anesth Analg. 2006;103:1543–8. doi: 10.1213/01.ane.0000244533.81152.7a. [DOI] [PubMed] [Google Scholar]
- 6.Choi SJ, Ahn HJ, Lee JI. Comparison of coagulation factors and blood loss between O and non-O blood types following hydroxyethyl starch infusion. Korean J Anesthesiol. 2010;58:344–50. doi: 10.4097/kjae.2010.58.4.344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Huraux C, Ankri A, Eyraud D, et al. Hemostatic changes in patients receiving hydroxyethyl starch: the influence of ABO blood group. Anesth Analg. 2001;92:1396–401. doi: 10.1097/00000539-200106000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Welsby IJ, Jones R, Pylman J, et al. Cardiothoracic Anesthesiology Research Endeavours (C.A.R.E.), Department of Anesthesiology, Duke University Medical Center. ABO blood group and bleeding after coronary artery bypass graft surgery. Blood Coagul Fibrinolysis. 2007;18:781–5. doi: 10.1097/MBC.0b013e3282f1029c. [DOI] [PubMed] [Google Scholar]
- 9.Gelb AB, Roth RI, Levin J, et al. Changes in blood coagulation during and following cardiopulmonary bypass: lack of correlation with clinical bleeding. Am J Clin Pathol. 1996;106:87–99. doi: 10.1093/ajcp/106.1.87. [DOI] [PubMed] [Google Scholar]
- 10.Treib J, Baron JF, Grauer MT, Strauss RG. An international view of hydroxyethyl starches. Intensive Care Med. 1999;25:258–68. doi: 10.1007/s001340050833. [DOI] [PubMed] [Google Scholar]
- 11.Treib J, Haass A, Pindur G. Coagulation disorders caused by hydroxyethyl starch. Thromb Haemost. 1997;78:974–83. [PubMed] [Google Scholar]
- 12.Collis RE, Collins PW, Gutteridge CN, et al. The effect of hydroxyethyl starch and other plasma volume substitutes on endothelial cell activation; an in vitro study. Intensive Care Med. 1994;20:37–41. doi: 10.1007/BF02425053. [DOI] [PubMed] [Google Scholar]
- 13.Gandhi SD, Weiskopf RB, Jungheinrich C, et al. Volume replacement therapy during major orthopedic surgery using Voluven (hydroxyethyl starch 130/0.4) or hetastarch. Anesthesiology. 2007;106:1120–7. doi: 10.1097/01.anes.0000265422.07864.37. [DOI] [PubMed] [Google Scholar]
- 14.Shima M, Fujimura Y, Nishiyama T, et al. ABO blood group genotype and plasma von Willebrand factor in normal individuals. Vox Sang. 1995;68:236–40. doi: 10.1111/j.1423-0410.1995.tb02579.x. [DOI] [PubMed] [Google Scholar]


