Abstract
Background
Central nervous system (CNS) primitive neuroectodermal tumors (PNETs) are malignant primary brain tumors that occur in young infants. Using current standard therapy, up to 80% of the children still dies from recurrent disease. Cellular immunotherapy might be key to improve overall survival. To achieve efficient killing of tumor cells, however, immunotherapy has to overcome cancer-associated strategies to evade the cytotoxic immune response. Whether CNS-PNETs can evade the immune response remains unknown.
Methods
We examined by immunohistochemistry the immune response and immune evasion strategies in pediatric CNS-PNETs.
Results
Here, we show that CD4+, CD8+, γδ-T-cells, and Tregs can infiltrate pediatric CNS-PNETs, although the activation status of cytotoxic cells is variable. Pediatric CNS-PNETs evade immune recognition by downregulating cell surface MHC-I and CD1d expression. Intriguingly, expression of SERPINB9, SERPINB1, and SERPINB4 is acquired during tumorigenesis in 29%, 29%, and 57% of the tumors, respectively.
Conclusion
We show for the first time that brain tumors express direct granzyme inhibitors (serpins) as a potential mechanism to overcome cellular cytotoxicity, which may have consequences for cellular immunotherapy.
Introduction
Embryonal tumors of the central nervous system (CNS), i.e. medulloblastoma, atypical teratoid rhabdoid tumor, and CNS primitive neuroectodermal tumors (PNET), are the most common malignant primary brain cancers in children and account for approximately 20% of all pediatric brain tumors [1]. Histologically they appear as small round blue progenitor cell tumors, but biologically and molecularly they are distinct entities [2, 3]. CNS-PNETs have an annual incidence of 0.62 per 1,000,000 children in the USA [4]. They are treated like high-risk medulloblastomas, resulting in a 5-year disease free survival of 15–50%, which is worse than medulloblastomas (5-year disease free survival of ~80%) [5–7]. In analogy to other brain tumors, like gliomas, immunotherapy might be key to improve survival in CNS-PNETs. Therefore, it is of importance to understand the immune response against CNS-PNETs. Efficient killing of CNS-PNETs during immunotherapeutic protocols can only be achieved when potential tumor-associated mechanisms to evade recognition or killing by the immune system are overcome. It has been well established that cancers employ multiple mechanisms to evade our immune system, making them less susceptible for immunotherapy [8]. Evidence for the existence of immune evasion strategies in brain tumors comes from gliomas and medulloblastomas, showing that subtypes downregulate MHC-I expression pointing to evasion from T cell-mediated anti-tumor immunity [9, 10] or lack CD1d expression to evade NKT cell recognition [11]. Moreover, expression of intracellular apoptosis inhibitors (e.g. caspase inhibitors) to escape from death receptor-induced apoptosis and granzyme-mediated killing pathways [8] predicts a worse clinical outcome and poor response to cellular immunotherapy [12, 13]. Whether CNS-PNETs can evade the immune response remains to be elucidated. The aim of this study is to survey several cases of pediatric CNS-PNET for tumor-infiltrating lymphocytes and immune evasion molecules, allowing to facilitate prediction of the tumor response to immunotherapy.
Materials and Methods
Patients
We examined by immunohistochemistry the cytotoxic immune response and immune evasion strategies in seven primary pediatric CNS-PNETs operated between 1998–2014 at the University Medical Center Utrecht (Utrecht, The Netherlands). Patient characteristics are shown in Table 1. The study material was derived from the archive of the Department of Pathology of the University Medical Center Utrecht, Utrecht, The Netherlands and distributed by the Biobank of the Department of Pathology. The biobank is overseen by the institutional medical ethical review board.
Table 1. Patient characteristics.
| Case | Gender | Age (years) | Location | Histology† | Survival (months) | GFAP* | NeuN* | Synaptophysin* | Ki-67* | Ini1* | β-catenin |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Female | 2 | Frontal lobe bilateral | CNS PNET, NOS | Died (21) | 0 | 0 | 100 | 75 | 100 | Cytoplasmic |
| 2 | Female | 2 | Insula left | CNS PNET, NOS | Died (2) | <1 | 0 | 90 | 50 | 100 | Cytoplasmic |
| 3 | Female | 2 | Frontal-temporal lobe right | CNS PNET, NOS | Died (10) | 0 | 0 | <1 | 95 | 100 | Cytoplasmic |
| 4 | Male | 9 | Frontal lobe right | CNS PNET, NOS | Died (5) | <1 | 0 | 90 | 65 | 100 | Cytoplasmic |
| 5 | Female | 17 | Frontal lobe/ regio pinealis | CNS PNET, pineoblastoma | Alive (50) | 0 | 0 | 100 | 10 | 100 | Cytoplasmic |
| 6 | Female | 7 | Parieto-ocipital lobe right | CNS PNET, Ependymoblastoma | Died (25) | 40 | 5 | 30 | 5 | 100 | Cytoplasmic |
| 7 | Female | 2 | Insula left | CNS PNET, Ependymoblastoma | Died (4) | 75 | <1 | 0 | 75 | 100 | Cytoplasmic |
†Tumors were reclassified according to the 4th edition of the WHO classification of tumors of the central nervous system.
*Values are displayed as percentage positive tumor cells.
Since we are using archival pathology material which does not interfere with patient care and does not involve physical involvement of the patient, no ethical approval is required according to Dutch legislation [14]. Use and storage of anonymous or coded left over material for scientific purposes is part of the standard treatment contract with patients and therefore informed consent procedure was not required according to our institutional medical ethical review board, this has also been described by van Diest [15].
Immunohistochemistry
Immunohistochemistry was carried out on 4μm thick formalin fixed paraffin embedded consecutive sections. For tumor classification, all stainings (GFAP, Synaptophysin, Neu-N, Ini1, β-catenin, Ki-67) were repeated using an automated immunostainer (Benchmark Ultra, Ventana, Roche). All other stainings were performed manually, except CD4 and SerpinB1 that were stained using the immunostainer. After deparaffination and rehydration, endogenous peroxidase activity was blocked for 15 min in a buffer solution pH5.8 containing 0.3% hydrogen peroxide. After antigen retrieval, i.e. boiling for 20 min in 10 mM citrate pH6.0, or Tris/EDTA pH9.0, a cooling off period of 30 min preceded the primary antibody incubation. All primary antibodies were diluted in PBS containing 2% BSA and incubated for 1h at room temperature (NKp46 and SERPINB4 were incubated o/n at 4°C). Antibody dilutions can be found in Table 2. The signal was amplified using Brightvision poly-HRP anti-mouse, rabbit, rat (DPVO-HRP, Immunologic) or in case of NKp46 with rabbit anti-goat HRP (DAKO), or in case of SERPINB4 the Novolink kit (Leica), and developed with diaminobenzidine followed by counterstaining with haematoxylin, dehydration in alcohol and mounting. The γδ-TCR staining was performed by boiling in 10 mM citrate pH6.0 for 2 min in a pressure cooker, followed by washing with TBS-T for 5 min (DAKO) and blocking with 5% Human serum in PBS for 30 min and avidin-biotin blocking (DAKO) for 20 min prior to antibody incubation. Signal amplification was performed using the REAL Detection System, Alkaline Phosphatase/RED, Rabbit/mouse (DAKO) followed by counterstaining with haematoxylin and mounting. Appropriate positive and negative controls were included in all stainings.
Table 2. Overview of used antibodies.
| Antigen retrieval | clone | Company | dilution | |
|---|---|---|---|---|
| GFAP | EDTA | 27G12 | Novocastra | 1:200 |
| Synaptophysin | EDTA | 6F2 | Dako | 1:1,000 |
| Neu-N | EDTA | Mab377 | Chemicon | 1:500 |
| Ini1 | EDTA | CL25/Baf47 | BD Biosciences | 1:100 |
| β-catenin | EDTA | 17C2 | Novocastra | 1:20 |
| Ki-67 | EDTA | M7240 | Dako | 1:100 |
| HLA-A | Citrate | HCA2 | Ref. [29] | 1:100 |
| HLA-B | EDTA | HC10 | Ref. [29] | 1:200 |
| CD1d | EDTA | NOR3.2 | Thermo Scientific | 1:100 |
| β2-microglobulin | None | A072 | Dako | 1:600 |
| CD3 | EDTA | A452 | Dako | 1:100 |
| CD4 | EDTA | SP35 | CellMarque | 1:50 |
| CD8 | Citrate | M7103 | Dako | 1:50 |
| CD20 | Citrate | M0755 | Dako | 1:800 |
| FOXP3 | EDTA | 150D/E4 | Ebioscience | 1:100 |
| NKp46 | EDTA | AF1850 | R&D Systems | 1:200 o/n |
| γTCR | Citrate | Gamma3.20 | Thermo Scientific | 1:40 |
| CD34 | Citrate | QBEnd10 | Immunotech | 1:800 |
| Bcl-2 | Citrate | M0887 | Dako | 1:200 |
| Survivin | Citrate | 71G4B7 | Cell Signaling | 1:400 |
| SERPINB1 | Citrate | Ab47731 | Abcam | 1:800 |
| SERPINB4 | EDTA | 10C12 | Santa Cruz | 1:50 o/n |
| SERPINB9 | Citrate | Clone 17 | Ref. [30] | 1:400 |
| Granzyme B | Citrate | GB7 | Ref. [31] | 1:250 |
Scoring of immunohistochemistry
Reclassification of cases was performed independently by two experienced neuropathologists (WGSS and WVH). All scoring was done blinded to patient characteristics and results of other staining by three independent observers (JFV, WGSS, WVH). Analysis of the immune influx was performed on whole slides at 20x magnification. Immune influx was corrected for the size of tissue on the slide and the tumor percentage as calculated with the manufacturers algorithm based on digitalized immunochemical slides using a digital slide scanner (Aperio Technologies Inc.). Serpin expression was scored as present (+) or absent (-), because serpins were uniformly expressed throughout the tumor.
Statistics
Statistical analysis was performed using IBM SPSS version 21 (SPSS Inc.). Descriptive statistics were examined as median and inter quartile range (IQR) taking all patients into account. No statistical tests or survival analyses were performed due to the number of patients included in this study.
Results and Discussion
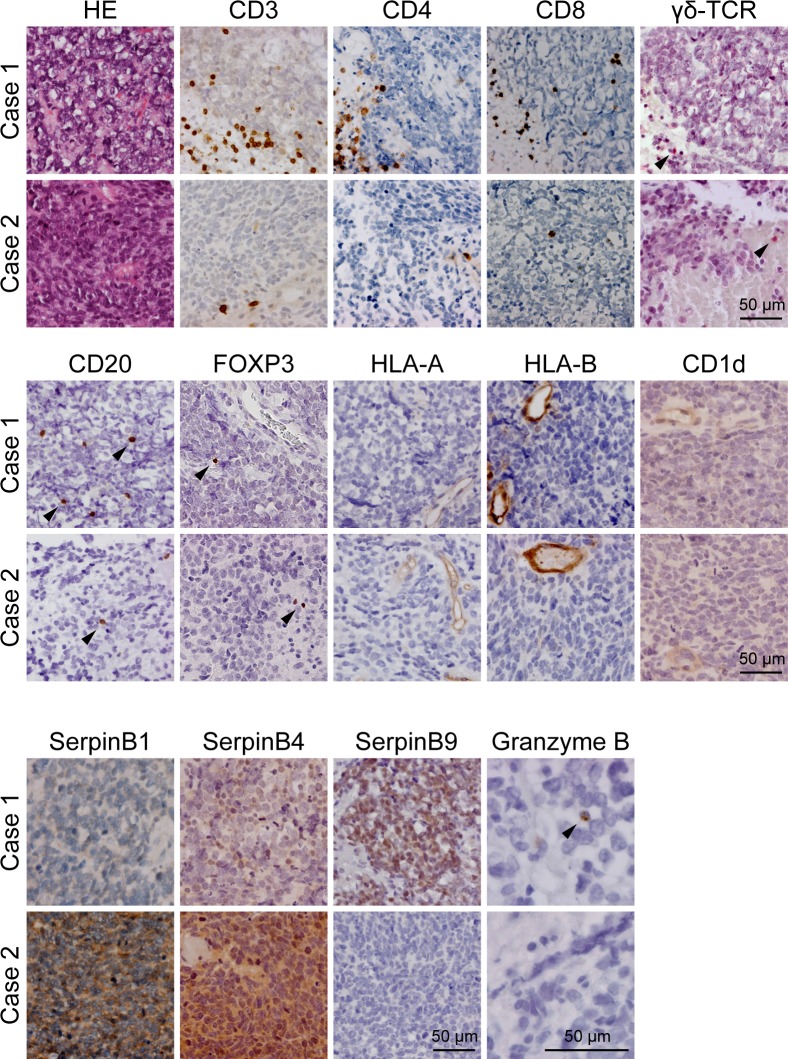
We found a substantial and highly variable influx of immune cells from the (tumor-associated) vasculature into the tumor tissue, i.e. 28.5 (43.7) [median (IQR)] CD3+ T-cells and 6.4 (13.3) CD20+ B-cells per 2mm2 tumor tissue. Normal brain parenchyma did not contain CD3+ T-cells or CD20+ B-cells. Data on individual patients is shown in Table 3. The CD3/CD20 ratio in the tumor tissue was 7.0 (12.6). The immune cell influx was independent of the vascular density. Leucocytosis or leucocytopenia prior to surgery, as determined by routine laboratory blood tests, was absent in all patients. The CD3+ T-cell population consisted of 9.6 (27.8) CD8+ T-cells and 8.7 (16.1) CD4+ T-cells per 2mm2 tumor tissue [CD8+ /CD4+ T-cell ratio of 1.2 (0.3)]. Next, we studied the influx of γδ-T-cells, an additional cytotoxic lymphocyte subset [16, 17]. We detected low numbers of γδ-T-cells in CNS-PNET [0.1 (0.2)]. Recruitment of NKp46+ NK-cells could not be detected in CNS-PNET, which is in line with results in other CNS tumors [18, 19]. The activity of cytotoxic tumor-infiltrating lymphocytes was examined by granzyme B (GrB) expression, resulting in a GrB-positive CTL fraction of 8.4% (8.4%). One patient (Case 1, Fig 1) had 29.0% GrB positive CTLs whereas all the other patients had <10% GrB positive CTLs (Case 2 is shown as an example, Fig 1).
Table 3. Results on infiltrating immune cells and Granzyme inhibitor expression of the individual patients.
| Case | CD3+ | CD4+ | CD8+ | CD20+ | FOXP3+ | NKp46+ | γTCR+ | CD3/CD20 ratio | CD8/CD4 ratio | GrB+ CTL fraction | SERPINB1 | SERPINB4 | SERPINB9 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 15.92 | 5.41 | 6.37 | 6.39 | 0.33 | 0 | 0.74 | 2.49 | 1.18 | 0.29 | - | - | + |
| 2 | 11.14 | 4.55 | 3.37 | 1.11 | 0.32 | 0 | 0.31 | 10.00 | 0.74 | 0.066 | + | + | - |
| 3 | 6.41 | 2.55 | 3.59 | 10.81 | 0.061 | 0 | 0.061 | 0.59 | 1.41 | 0.014 | - | + | - |
| 4 | 110.03 | 44.22 | 51.06 | 15.78 | 0.14 | 0 | 0.24 | 6.97 | 1.15 | 0.099 | + | + | - |
| 5 | 54.86 | 20.63 | 31.40 | 3.95 | 1.30 | 0 | n.a. | 13.88 | 1.52 | 0.084 | - | - | + |
| 6 | 38.83 | 15.27 | 16.27 | 2.51 | 0.23 | 0 | 0.028 | 15.45 | 1.07 | 0.015 | - | - | - |
| 7 | 28.46 | 8.70 | 9.57 | 21.85 | 0.17 | 0 | 0.26 | 1.30 | 1.10 | 0.099 | - | + | - |
Values are displayed as number of immune cells per 2mm2 tumor tissue.
+ and - indicates presence or absence of expression of SERPINs, respectively
Fig 1. Immune (evasion) markers in cases of CNS-PNET.
Immunohistochemical staining of immune markers in two CNS-PNET cases. Note that SerpinB9 expression coincides with high numbers of activated GrB + CTLs in case 1 versus low numbers of activated GrB + CTLs in case 2. Size bar equals 50μm.
Given the modest cytotoxic lymphocyte activation, we wondered whether CNS-PNETs downregulate MHC-I (HLA-A and HLA-B) and/or CD1d to avoid CTL, NKT, and/or CD1d-restricted γδ-T-cell [20] recognition. Whereas normal brain tissue, blood vessels, and infiltrating immune cells readily express these HLA molecules and CD1d, we found that HLA-A, HLA-B, and CD1d expression was not detectable in all CNS-PNET cases (Fig 1). In addition, β2-microglobulin expression was decreased concordantly (data not shown). We detected low numbers of FOXP3+ regulatory T-cells [0.2 (0.3) per 2mm2 tumor tissue], which may contribute to attenuation of immune activity. Together, these data suggest that pediatric CNS-PNETs may evade recognition by cytotoxic immune cells.
Granzymes are the major tumor killing molecules secreted by cytotoxic cells. In humans, five granzymes (i.e. GrA, GrB, GrH, GrK, and GrM) exist with distinct substrate specificities and only partially overlapping routes of apoptosis induction [21]. Certain tumors can express serine protease inhibitors (serpins) to directly block granzyme activity. It has been well established that SERPINB9 (GrB inhibitor also called PI-9) expression in melanomas correlates with worse clinical outcome and poor response to immunotherapy [13]. For brain tumors in general, it remains unknown whether granzyme inhibitors are expressed. Intriguingly, we now show that 29% of CNS-PNETs had expression of the GrB inhibitor SERPINB9 (Fig 1). We found that SERPINB9 expression was absent in the normal brain parenchyma, indicating that SERPINB9 expression is acquired during tumorigenesis. Remarkably, high SERPINB9 expression was constrained to the case with high cytotoxic lymphocyte activation. We also addressed the expression of the GrH and GrM inhibitors (SERPINB1 [22] and SERPINB4 [23], respectively) in CNS-PNETs. Like SERPINB9, expression of SERPINB1 and SERPINB4 was acquired in CNS-PNETs. We found SERPINB4 expression in four CNS-PNETs, of which two cases turned out to be also SERPINB1 positive (Fig 1, Table 1). These data suggest that SERPINB1, SERPINB4, and SERPINB9 are differentially expressed in pediatric CNS-PNETs. Interestingly, besides these serpins, all tumors had high expression of Survivin (caspase-3 inhibitor) and Bcl-2 (cytochrome c release inhibitor), which are both downstream inhibitors of granzyme-induced apoptotic pathways.
The molecular mechanisms and physiological relevance of intracellular serpin expression in pediatric brain tumors remains unknown. SERPINB9, B4, and B1 are known to inhibit granzyme B, M, and H, respectively, and are therefore likely to contribute to evasion of granzyme-induced cytotoxicity [22–24]. However, we cannot exclude that these serpins also play other roles in tumorigenesis. Recently, Valiente et al showed that expression of neuroserpin and SERPINB2 are essential for developing brain metastases in patients with lung and breast cancer. Expression of these serpins inhibited plasminogen activator and FAS-L induced cytotoxic cell death by reactive astrocytes and is therefore a marker for poor prognosis [25]. Furthermore, SERPINB1 expression in glioma and glioblastoma cell lines seems to be a marker for good prognosis, because it inhibits tumor cell migration and invasion [26]. Finally, SERPINB4 expression in patients with squamous cell carcinomas is associated poor prognosis and SERPINB4 can inhibit both radiation- and TNF-induced apoptosis, probably by inhibition of the p38 MAPK pathway and the proteolytic activity of endogenous cathepsin G, respectively [27, 28]. Whether CNS-PNETs with high serpin expression are more prone to be aggressive and more resistant towards (immuno)therapies requires further study,
Conclusion
In conclusion, we have demonstrated that several immune cell subsets can infiltrate pediatric CNS-PNETs, although the activation status of the cytotoxic cells (granzyme B) is variable. Pediatric CNS-PNETs might evade immune recognition by downregulating cell surface MHC-I and CD1d expression. We show that brain tumors can acquire expression of SERPINB1, SERPINB4, and SERPINB9 as a potential mechanism to resist granzyme-induced cytotoxicity. Although the mechanistic insights remain to be elucidated. This study hints to the putative implications of serpin expression for the success rate of immunotherapy in CNS-PNET patients. To predict clinical outcome and response to immunotherapy, further study is required in larger pediatric CNS-PNET cohorts as wells as in the currently running clinical trial of pediatric medulloblastomas/CNS-PNET immunotherapy, in which dendritic cell vaccination and adoptive cellular immunotherapy with cytotoxic lymphocytes is employed [Vaccine Immunotherapy for Recurrent Medulloblastoma and Primitive Neuroectodermal Tumor (Re-MATCH), University of Florida, NCT01326104].
Data Availability
All relevant data are within the paper.
Funding Statement
This work was supported by a research grant from Cancer Foundation Koppie-Au. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.De Braganca KC, Packer RJ. Treatment Options for Medulloblastoma and CNS Primitive Neuroectodermal Tumor (PNET). Curr Treat Options Neurol. 2013;15(5):593–606. 10.1007/s11940-013-0255-4 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Taylor MD, Northcott PA, Korshunov A, Remke M, Cho YJ, Clifford SC, et al. Molecular subgroups of medulloblastoma: the current consensus. Acta Neuropathol. 2012;123(4):465–72. 10.1007/s00401-011-0922-z . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Picard D, Miller S, Hawkins CE, Bouffet E, Rogers HA, Chan TS, et al. Markers of survival and metastatic potential in childhood CNS primitive neuro-ectodermal brain tumours: an integrative genomic analysis. Lancet Oncol. 2012;13(8):838–48. 10.1016/S1470-2045(12)70257-7 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Smoll NR, Drummond KJ. The incidence of medulloblastomas and primitive neurectodermal tumours in adults and children. J Clin Neurosci. 2012;19(11):1541–4. 10.1016/j.jocn.2012.04.009 . [DOI] [PubMed] [Google Scholar]
- 5.Johnston DL, Keene DL, Lafay-Cousin L, Steinbok P, Sung L, Carret AS, et al. Supratentorial primitive neuroectodermal tumors: a Canadian pediatric brain tumor consortium report. J Neurooncol. 2008;86(1):101–8. 10.1007/s11060-007-9440-1 . [DOI] [PubMed] [Google Scholar]
- 6.Timmermann B, Kortmann RD, Kuhl J, Rutkowski S, Meisner C, Pietsch T, et al. Role of radiotherapy in supratentorial primitive neuroectodermal tumor in young children: results of the German HIT-SKK87 and HIT-SKK92 trials. J Clin Oncol. 2006;24(10):1554–60. 10.1200/JCO.2005.04.8074 . [DOI] [PubMed] [Google Scholar]
- 7.Packer RJ, Zhou T, Holmes E, Vezina G, Gajjar A. Survival and secondary tumors in children with medulloblastoma receiving radiotherapy and adjuvant chemotherapy: results of Children's Oncology Group trial A9961. Neuro Oncol. 2013;15(1):97–103. 10.1093/neuonc/nos267 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Igney FH, Krammer PH. Immune escape of tumors: apoptosis resistance and tumor counterattack. J Leukoc Biol. 2002;71(6):907–20. . [PubMed] [Google Scholar]
- 9.Raffaghello L, Nozza P, Morandi F, Camoriano M, Wang X, Garre ML, et al. Expression and functional analysis of human leukocyte antigen class I antigen-processing machinery in medulloblastoma. Cancer Res. 2007;67(11):5471–8. 10.1158/0008-5472.CAN-06-4735 . [DOI] [PubMed] [Google Scholar]
- 10.Gerosa MA, Amadori G, Semenzato P, Gasparotto G, Carteri A. Immunobiology of primary CNS tumors in infancy and childhood. B- and T-cell dependent immunity and cytotoxicity and cell kinetic evaluation. Childs Brain. 1980;6(2):92–102. . [DOI] [PubMed] [Google Scholar]
- 11.Liu D, Song L, Brawley VS, Robison N, Wei J, Gao X, et al. Medulloblastoma expresses CD1d and can be targeted for immunotherapy with NKT cells. Clin Immunol. 2013;149(1):55–64. 10.1016/j.clim.2013.06.005 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sapoznik S, Hammer O, Ortenberg R, Besser MJ, Ben-Moshe T, Schachter J, et al. Novel anti-melanoma immunotherapies: disarming tumor escape mechanisms. Clin Dev Immunol. 2012;2012:818214 10.1155/2012/818214 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.van Houdt IS, Oudejans JJ, van den Eertwegh AJ, Baars A, Vos W, Bladergroen BA, et al. Expression of the apoptosis inhibitor protease inhibitor 9 predicts clinical outcome in vaccinated patients with stage III and IV melanoma. Clin Cancer Res. 2005;11(17):6400–7. 10.1158/1078-0432.CCR-05-0306 . [DOI] [PubMed] [Google Scholar]
- 14.CCMO website:. Central Committee on Research involving Human Subjects (Centrale Commissie Mensgebonden Onderzoek) (text in Dutch): http://www.ccmo.nl/nl/uw-onderzoek-wmo-plichtig-of-niet [2015 September 2].
- 15.van Diest PJ. No consent should be needed for using leftover body material for scientific purposes. For. BMJ. 2002;325(7365):648–51. [PubMed] [Google Scholar]
- 16.Brandes M, Willimann K, Moser B. Professional antigen-presentation function by human gammadelta T Cells. Science. 2005;309(5732):264–8. 10.1126/science.1110267 . [DOI] [PubMed] [Google Scholar]
- 17.Chien YH, Meyer C, Bonneville M. gammadelta T cells: first line of defense and beyond. Annu Rev Immunol. 2014;32:121–55. 10.1146/annurev-immunol-032713-120216 . [DOI] [PubMed] [Google Scholar]
- 18.Vaquero J, Coca S, Oya S, Martinez R, Ramiro J, Salazar FG. Presence and significance of NK cells in glioblastomas. J Neurosurg. 1989;70(5):728–31. 10.3171/jns.1989.70.5.0728 . [DOI] [PubMed] [Google Scholar]
- 19.Poli A, Kmiecik J, Domingues O, Hentges F, Blery M, Chekenya M, et al. NK cells in central nervous system disorders. J Immunol. 2013;190(11):5355–62. 10.4049/jimmunol.1203401 . [DOI] [PubMed] [Google Scholar]
- 20.Uldrich AP, Le Nours J, Pellicci DG, Gherardin NA, McPherson KG, Lim RT, et al. CD1d-lipid antigen recognition by the gammadelta TCR. Nat Immunol. 2013;14(11):1137–45. 10.1038/ni.2713 . [DOI] [PubMed] [Google Scholar]
- 21.Bovenschen N, Kummer JA. Orphan granzymes find a home. Immunol Rev. 2010;235(1):117–27. 10.1111/j.0105-2896.2010.00889.x . [DOI] [PubMed] [Google Scholar]
- 22.Wang L, Li Q, Wu L, Liu S, Zhang Y, Yang X, et al. Identification of SERPINB1 as a physiological inhibitor of human granzyme H. J Immunol. 2013;190(3):1319–30. 10.4049/jimmunol.1202542 . [DOI] [PubMed] [Google Scholar]
- 23.de Koning PJ, Kummer JA, de Poot SA, Quadir R, Broekhuizen R, McGettrick AF, et al. Intracellular serine protease inhibitor SERPINB4 inhibits granzyme M-induced cell death. PLoS One. 2011;6(8):e22645 10.1371/journal.pone.0022645 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Medema JP, de Jong J, Peltenburg LT, Verdegaal EM, Gorter A, Bres SA, et al. Blockade of the granzyme B/perforin pathway through overexpression of the serine protease inhibitor PI-9/SPI-6 constitutes a mechanism for immune escape by tumors. Proceedings of the National Academy of Sciences of the United States of America. 2001;98(20):11515–20. 10.1073/pnas.201398198 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Valiente M, Obenauf AC, Jin X, Chen Q, Zhang XH, Lee DJ, et al. Serpins promote cancer cell survival and vascular co-option in brain metastasis. Cell. 2014;156(5):1002–16. 10.1016/j.cell.2014.01.040 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Huasong G, Zongmei D, Jianfeng H, Xiaojun Q, Jun G, Sun G, et al. Serine protease inhibitor (SERPIN) B1 suppresses cell migration and invasion in glioma cells. Brain research. 2015;1600:59–69. 10.1016/j.brainres.2014.06.017 . [DOI] [PubMed] [Google Scholar]
- 27.McGettrick AF, Barnes RC, Worrall DM. SCCA2 inhibits TNF-mediated apoptosis in transfected HeLa cells. The reactive centre loop sequence is essential for this function and TNF-induced cathepsin G is a candidate target. European journal of biochemistry / FEBS. 2001;268(22):5868–75. . [DOI] [PubMed] [Google Scholar]
- 28.Murakami A, Suminami Y, Hirakawa H, Nawata S, Numa F, Kato H. Squamous cell carcinoma antigen suppresses radiation-induced cell death. British journal of cancer. 2001;84(6):851–8. 10.1054/bjoc.2000.1683 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stam NJ, Vroom TM, Peters PJ, Pastoors EB, Ploegh HL. HLA-A- and HLA-B-specific monoclonal antibodies reactive with free heavy chains in western blots, in formalin-fixed, paraffin-embedded tissue sections and in cryo-immuno-electron microscopy. Int Immunol. 1990;2(2):113–25. . [DOI] [PubMed] [Google Scholar]
- 30.Bladergroen BA, Strik MC, Bovenschen N, van Berkum O, Scheffer GL, Meijer CJ, et al. The granzyme B inhibitor, protease inhibitor 9, is mainly expressed by dendritic cells and at immune-privileged sites. J Immunol. 2001;166(5):3218–25. . [DOI] [PubMed] [Google Scholar]
- 31.Kummer JA, Kamp AM, Tadema TM, Vos W, Meijer CJ, Hack CE. Localization and identification of granzymes A and B-expressing cells in normal human lymphoid tissue and peripheral blood. Clin Exp Immunol. 1995;100(1):164–72. . [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the paper.