Abstract
Background
Cross-sectional population-based surveys are essential surveillance tools for tracking changes in HIV epidemics. In 2007, Kenya implemented the first AIDS Indicator Survey [Kenya AIDS Indicator Survey (KAIS) 2007)], a nationally representative, population-based survey that collected demographic and behavioral data and blood specimens from individuals aged 15–64 years. Kenya’s second AIDS Indicator Survey (KAIS 2012) was conducted to monitor changes in the epidemic, evaluate HIV prevention, care, and treatment initiatives, and plan for an efficient and effective response to the HIV epidemic.
Methods
KAIS 2012 was a cross-sectional 2-stage cluster sampling design, household-based HIV serologic survey that collected information on households as well as demographic and behavioral data from Kenyans aged 18 months to 64 years. Participants also provided blood samples for HIV serology and other related tests at the National HIV Reference Laboratory.
Results
Among 9300 households sampled, 9189 (98.8%) were eligible for the survey. Of the eligible households, 8035 (87.4%) completed household-level questionnaires. Of 16,383 eligible individuals aged 15–64 years and emancipated minors aged less than 15 years in these households, 13,720 (83.7%) completed interviews; 11,626 (84.7%) of the interviewees provided a blood specimen. Of 6302 eligible children aged 18 months to 14 years, 4340 (68.9%) provided a blood specimen. Of the 2094 eligible children aged 10–14 years, 1661 (79.3%) completed interviews.
Conclusions
KAIS 2012 provided representative data to inform a strategic response to the HIV epidemic in the country.
Keywords: HIV, Kenya, AIDS Indicator Survey, surveillance
INTRODUCTION
In 2011, an estimated 1.6 million people were living with HIV in Kenya, representing 6.8% of the HIV burden in sub-Saharan Africa.1 The adult prevalence of HIV in Kenya has remained stable over the past 5 years at approximately 6%.2 To monitor the epidemic, assess the impact of HIV prevention, care, and treatment programs, and to plan interventions, the country uses findings from Demographic and Health Surveys, AIDS Indicator Surveys, HIV sentinel surveillance in antenatal clinics, behavioral surveys in high-risk populations, and HIV estimates and projections from mathematical modeling. However, continuous improvement on the collection of detailed information on the HIV-infected, at-risk groups, and the general population is needed for the Government of Kenya to plan for and evaluate its HIV prevention, care, and treatment programs adequately.
In 2007, Kenya conducted its first national comprehensive, population-based HIV serologic survey, the Kenya AIDS Indicator Survey (KAIS 2007), among persons aged 15–64 years. KAIS 2007 found that adult HIV prevalence was 7.1% (95% confidence interval: 6.5 to 7.7); married or cohabitating partners were at high risk for HIV transmission compared with those who had never married or cohabitated3,4; uncircumcised men were more likely to be infected with HIV compared with circumcised men5; the vast majority of HIV-infected individuals were unaware of their infection6,7; and there was unmet need for HIV-related care, including antiretroviral therapy (ART).3 Also, for the first time, HIV prevalence among older adults (aged 50–64 years) was measured. In response to these findings, the government increased opportunities for voluntary medical male circumcision and expanded HIV testing strategies, programs to prevent perinatal HIV transmission, and HIV treatment and care services throughout the country.8
Although Kenya has made great strides in its national response to the HIV epidemic, information gaps in critical populations remain. For example, while there is evidence of unmet need for HIV medical care among children, no nationally representative data exist to confirm the prevalence of HIV infection among children.1 Additionally, surveys conducted among select high-risk groups such as female sex workers, men who have sex with men, and persons who inject drugs have been conducted, but estimates on the size of these key populations have not been well validated.9
The second Kenya AIDS Indicator Survey (KAIS 2012), conducted between October 29, 2012 and February 5, 2013, enabled the Government of Kenya to monitor progress on indicators collected in KAIS 2007 and also collected new indicators to address information gaps. KAIS 2012 included children aged 18 months to 14 years and persons aged 15 to 64 years. In addition, the survey also provided home-based testing and counseling (HBTC), and for persons found to be HIV-positive in HBTC, in–home measurement of CD4+ T-cell counts. Data from KAIS 2012 allowed for analysis of trends in HIV prevalence, risk behaviors, and coverage of and unmet need for HIV prevention, care, and treatment services in both the general population and key populations at high-risk of HIV infection. We describe the design and methods of the survey, results of the household and participant recruitment, and respondent characteristics.
METHODS
Sample Size and Study Design
The survey sample size was calculated to estimate HIV prevalence for men and women aged 15 to 64 years and children aged 18 months to 14 years for the main geographic domains of interest: urban, rural, regional, and national. For children, the domain of interest was the national-level only. It was estimated that a sample of 9300 households within 372 clusters would provide a representative sample of women and men aged 15 to 64 years and children aged 18 months to 14 years.
The survey used a 2-stage stratified cluster sampling design. The first stage involved selection of 372 of a total of 5360 clusters from the Kenya National Bureau of Statistics household-based sampling frame (NASSEP V) using a systematic random sampling method.10 The NASSEP V frame was developed using the 47 counties and further stratified into residential areas (urban and rural) within clusters. In the second stage, a sample of 25 households was selected in each cluster using equal probability systematic sampling methods. Because half of the households were required for the child sample, we selected every other household after random selection of the first household to recruit children.
Community Mobilization
To gain support and awareness for the survey at the cluster, regional, and national levels, we undertook a series of activities that included a high-level national launch targeting national and regional leaders and development of print, radio, and television materials that described the survey. During data collection, we focused on district and cluster-level mobilization, where field staff worked directly with local leaders and key organizations to gain access and acceptability in the sampled clusters and disseminated information on the survey before the arrival of field teams into those clusters.
Eligibility Criteria, Recruitment, and Consent Procedures
The survey population was persons aged 18 months to 64 years who were usual household residents or persons who had been present in the household on the night before the survey. We excluded adults or children with cognitive or hearing disabilities that would prohibit them from effectively participating in the survey. Emancipated minors aged 17 years or younger were included in the survey and completed adult questionnaires. KAIS 2012 defined an emancipated minor as a person aged less than 18 years who was married, pregnant, or a parent and allowed these individuals to provide consent for survey participation.
The head of household, defined as an adult aged 18 years or older who was a resident of the household and recognized as a decision maker by other household members, provided verbal consent for his or her household to participate in the survey and subsequently completed the household interview. In the absence of an adult household member, an emancipated minor living in the home was selected as the household head for the purposes of the survey. Enumeration of household members was obtained through the household interview. If a household was contacted and a head of household was not available or it was not convenient for household members to be interviewed, the survey team would reschedule a maximum of 3 return visits while proceeding to the next selected household.
Eligible adults aged 18 years and above or emancipated minors provided verbal consent for interview, collection of a blood specimen for biologic testing at the National HIV Reference Laboratory (NHRL), storage of blood samples at the NHRL, and future testing that would include recent HIV infection and other unspecified tests. Verbal consent from parents or parents or guardians was required for minors aged 17 years and below to participate; we also obtained verbal assent from children aged 10–17 years whose parents or guardians had consented to their participation. Participants could also consent or assent to HBTC in their homes and for those testing HIV-positive through HBTC, a point-of-care (POC) CD4+ T-cell count test was offered.
Survey Instruments
Trained interviewers conducted face-to face interviews in a private area in the participants’ home. Names of participants were collected to facilitate interviews; however, these were not retained in the survey data set. Data were captured on netbook computers (Mirus innovations, Mississauga, Ontario, Canada) using a data entry software application that was programmed with automated skip patterns and recognition of invalid responses.11 In addition to providing information on eligible participants, the household questionnaire collected information regarding support of orphans and vulnerable children within the household, the physical and sanitary condition of the home, and household possessions. Based on household characteristics (water source, sanitation facilities, and household construction material) and household possessions, a wealth score was calculated for each household and used to divide households into quintiles that represented a wealth index of the poorest to the wealthiest households.12 The household questionnaire also collected data using a validated Household Hunger Scale to measure food security at the household level.13 The Household Hunger Scale was used to tabulate a score for each household based on responses about the occurrence and frequency of food insecurity and intake. Based on the scores, we derived 3 household hunger categories: little to no household hunger, moderate household hunger, and severe household hunger.
Interviewers administered questionnaires to persons aged 15–64 years and emancipated minors that collected information on demographic characteristics, reproductive and children’s health (for households with children aged 18 months to 14 years), sexual behavior, HIV-related knowledge and attitudes, HIV testing, exposure to blood transfusions and medical injections, tuberculosis and other health issues, male circumcision, health service utilization, nonprescription drug use, and migration. New elements in KAIS 2012 included an expansion of questions pertaining to programs that prevent perinatal HIV transmission, HIV care and treatment modules that asked comprehensive questions around entry into HIV care, retention in care, use of cotrimoxazole and ART, and adherence to treatment, questions to describe sexual concurrency, and prevalence of high-risk behaviors such as anal sex, transactional sex, and injecting drug use. The children’s questionnaire was administered to respondents aged 10–14 years and collected information on demographics, HIV-related knowledge and attitudes, HIV risk perception, exposure to HIV prevention interventions, male circumcision, HIV testing, social norms about sex, alcohol and drug use, and HIV stigma. Information on sexual behavior in the children’s questionnaire was limited to respondents aged 12–14 years to correspond with the age of sex education in Kenyan schools.
Sample Collection
Laboratory technicians collected venous blood from participants in CD4 stabilization tubes (Becton Dickinson Vacutainer Systems, Franklin Lakes, NJ). If a participant was willing to be interviewed but refused to provide a venous blood sample, a dried capillary blood spot (DBS) sample from a finger prick was requested. DBS samples were also collected in cases where venipuncture was not feasible or unsuccessful. Laboratory technicians prepared up to 4 S&S 903 DBS cards (Schleicher & Schuell Bioscience Inc., Keene, NH) for every participant at the end of each day using venous blood samples. DBS cards were labeled with study identification numbers that matched their corresponding venous blood tube. DBS cards were dried overnight in the field laboratory and packaged for transport to the NHRL for biologic testing and storage. Field teams shipped participant blood tubes and DBS cards to the NHRL at room temperature through ground courier several times a week.
HIV Home-Based Testing and Counseling and Point-of-Care CD4+ T-Cell Count Testing
Eligible survey participants who completed the survey were given the opportunity to receive their HIV test results within their home using rapid HIV tests based on the national HIV testing algorithm.14 Blood specimens were tested in a parallel testing algorithm with Determine HIV-1/2 (Inverness Medical, Waltham, MA) and Unigold (Trinity Biotech PLC, Bray, Ireland) rapid test kits. Specimens that tested positive on both test kits were reported positive as the final result. Specimens testing negative on both test kits were reported negative as the final result. Specimens that tested positive on 1 kit and negative on the other were determined to be discrepant and reported indeterminate as the final result. Participants with indeterminate results were referred to a health facility for retesting. CD4+ T-cell count testing was performed within the home using the PIMA CD4 Analyzer (Alere Inc., Waltham, MA) for participants with HIV-positive test results.
Adults were offered the opportunity to receive their HIV test results as an individual or as a couple. The parents or guardians of children aged 18 months to 9 years received the results on the child’s behalf and were counseled by the HBTC service provider on how to disclose results to the child. Children aged 10–14 years received results in the presence of their parent or guardian, whereas children aged 15–17 years could receive their results without a parent or guardian present, provided the parent or guardian consented to this. All HIV-positive participants were provided with a KAIS 2012 referral card and referred for care.
Central Laboratory Procedures and Specimen Repository
At the NHRL, specimens were tested for HIV antibody using the Vironostika HIV-1/2 UNIF II Plus O Enzyme Immunoassay (bioMérieux, Marcy d’Etoile, France). HIV antibody–positive results were confirmed using the Murex HIV.1.2.O HIV Enzyme Immunoassay (DiaSorin, SpA, Saluggia, Italy). Repeat testing was performed for discordant results, and if results remained discordant, final results were obtained using polymerase chain reaction (Cobas Amplicor HIV-1 Monitor Test, version 1.5, Roche Molecular Diagnostics, Pleasanton, CA). We measured CD4+ T-cell counts and percentages (for children aged less than 5 years) using BD FACSCalibur flow cytometer (Becton Dickinson BioSciences, San Jose, CA). To quantify CD4+ T-cell count reference values, we measured CD4+ T-cell counts from a 10% random sample of HIV-negative specimens. All confirmed HIV-positive blood specimens were measured for HIV RNA concentration (Abbott M2000 Real-Time HIV-1 Assay, Abbott Laboratories, Abbott Park, IL). Specimens with HIV RNA concentrations of under 1000 copies per milliliter were classified as clinically suppressed; specimens with HIV RNA concentrations of less than 550 copies per milliliter, the minimum concentration detectable on the assay, were classified as virologically suppressed.15,16 Samples remaining after HIV, CD4, and viral load testing were completed were stored at 270°C for future tests for recent HIV infection and other unspecified biologic testing.
Data Management, Weighting, and Statistical Analysis
Survey data were transmitted from field teams on a daily basis to the KAIS 2012 central server using a secure virtual private network. Where wireless networks were not available, national-level survey supervisors would visit the teams on a monthly basis, collect the data, and upload the data to the central server in Nairobi. Because the KAIS 2012 design was not self-weighted, sampling weights were computed to take into account the sampling probability and survey nonre-sponse. Design weights included the probability of selection of the 372 KAIS 2012 clusters in the NASSEP V sampling frame. Weights were adjusted for household nonresponse (both for the adult and child sample) and individual non-response (both for the interview and blood draw). Because of overrepresentation of females in the sample, a poststratification adjustment was applied to the weights to refiect the expected distribution of sex across geographic regions based on the projected 2012 population distribution in the 2009 Kenya Population and Housing Census.17 In each cluster, separate weights were calculated for the type of interview or blood draw conducted, including household interview, adult interview, child interview, parent or guardian’s pediatric interview, adult blood draw, and child blood draw. When reporting proportions and mean values, weights were normalized to the survey’s sample size and had a mean of 1.0. When reporting regional and national estimates of the total number of adults and children with select characteristics in the population, non-normalized weights based on the 2012 projected population data in the 2009 Kenya Population and Housing Census were applied.17 We performed data cleaning and analyses using STATA version 12.0 (STATA Corporation, College Station, TX) and SAS version 9.3 (SAS Institute Inc., Cary, NC).
Ethical Approval
The KAIS 2012 protocol was reviewed and approved by the Ethical Review Board of the Kenya Medical Research Institute, the Institutional Review Board of the US Centers for Disease Control and Prevention, and the Committee on Human Research of the University of California, San Francisco.
RESULTS
Survey Response Rates
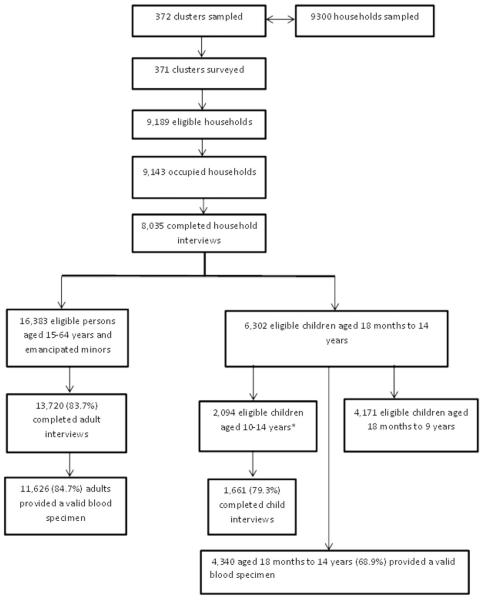
Because of regional insecurity, the North Eastern region was not included in the NASSEP V from which KAIS 2012 clusters were sampled. The North Eastern region contributes to approximately 6% of Kenya’s total population, and HIV prevalence in North Eastern region was 0.8% in 2007 accounting for 0.4% of the overall HIV burden in the country.3,17 A total of 372 clusters were sampled for KAIS 2012; however, 1 cluster in Tana River region was excluded because of security issues during the survey period. The final number of surveyed clusters was 371. Of the 9300 households sampled, 9189 (98.8%) were eligible for the survey and 9143 (98.3%) were occupied by house-hold members at the time of the survey (Fig. 1). Of the eligible households, 8035 (87.4%) completed a household interview. Of 16,383 eligible individuals aged 15–64 years and emancipated minors in these households, 13,720 (83.7%) completed individual interviews, and 11,626 (84.7%) provided a blood specimen. There were a total of 6302 children aged 18 months to 14 years who were eligible for the blood draw, and of these 4340 (68.9%) provided a blood specimen. There were a total of 2094 children aged 10–14 years eligible for interview, and of these, 1661 (79.3%) completed child interviews.
FIGURE 1.
Clusters, households, and individuals in the Kenya AIDS Indicator Survey 2012.
Rural households had higher household interview response rates (89.3%) compared to urban households (84.7%, P < 0.0001) (Table 1). Response rates for adult interviews (respondents aged 15–64 years) were higher among women (89.1%) than men (77.4%; P < 0.0001) and similar between urban (83.4%) and rural (84.0%) residents. A greater proportion of women (85.4%) than men (83.9%, P = 0.0200) provided blood specimens. Participants who were aged younger than 35 years (P = 0.0030), residing in urban areas (P < 0.0001) and in the highest wealth index (P < 0.0001) were less likely to provide a blood sample than their older, rural, and poorer counterparts. Among children aged 10–14 years, interview response rates were similar among girls and boys (79.3% vs. 79.2%, P = 0.3100) and among urban and rural residents (79.7% vs. 79.2%, P = 0.5000) (Table 2). The overall blood response rate among all children aged 18 months to 14 years was 68.9%.
TABLE 1.
Interview and Blood Response Rates Among Households and Individuals Aged 15–64 Years and Emancipated Minors, KAIS 2012
| Total Eligible, N |
Interviewed, N |
Interview Response Rate, % |
P | Provided Blood Sample, N |
Blood Response Rate, % |
P | |
|---|---|---|---|---|---|---|---|
| Households | N = 9189 | N = 8035 | N/A | ||||
| Rural | 5506 | 4915 | 89.3 | — | — | — | |
| Urban | 3683 | 3120 | 84.7 | <0.0001 | — | — | — |
| Individuals aged 15–64 years and emancipated minors |
N = 16,383 | N = 13,720 | N = 11,626 | ||||
| Sex | |||||||
| Men | 7452 | 5766 | 77.4 | 4836 | 83.9 | ||
| Women | 8931 | 7954 | 89.1 | <0.0001 | 6790 | 85.4 | 0.0200 |
| Age group, yrs* | |||||||
| 15–24 | 5708 | 4546 | 79.6 | 3828 | 84.2 | ||
| 25–34 | 4519 | 3863 | 85.5 | 3228 | 83.6 | ||
| 35–44 | 3021 | 2590 | 85.7 | 2211 | 85.4 | ||
| 45–54 | 1929 | 1684 | 87.3 | 1446 | 85.9 | ||
| 55–64 | 1139 | 1037 | 91.0 | <0.0001 | 913 | 88.0 | 0.0030 |
| Residence | |||||||
| Rural | 10,290 | 8638 | 84.0 | 7501 | 86.8 | ||
| Urban | 6093 | 5082 | 83.4 | 0.3700 | 4125 | 81.2 | <0.0001 |
| Region | |||||||
| Central | 1757 | 1580 | 89.9 | 1423 | 90.1 | ||
| Coast | 1971 | 1712 | 86.9 | 1462 | 85.4 | ||
| Eastern | 3381 | 2684 | 79.4 | 2321 | 86.5 | ||
| Nairobi | 2098 | 1745 | 83.2 | 1314 | 75.3 | ||
| Nyanza | 2146 | 1834 | 85.5 | 1631 | 88.9 | ||
| Rift Valley | 3109 | 2484 | 79.9 | 2067 | 83.2 | ||
| Western | 1921 | 1681 | 87.5 | <0.0001 | 1408 | 83.8 | <0.0001 |
| Wealth index | |||||||
| Poorest | 3570 | 2850 | 79.8 | 2434 | 85.4 | ||
| Second | 3358 | 2857 | 85.1 | 2497 | 87.4 | ||
| Middle | 3091 | 2675 | 86.5 | 2318 | 86.7 | ||
| Fourth | 3056 | 2580 | 84.4 | 2177 | 84.4 | ||
| Richest | 3308 | 2758 | 83.3 | <0.0001 | 2200 | 79.8 | <0.0001 |
Excludes 67 eligible emancipated minors younger than aged 15 years who were not interviewed.
TABLE 2.
Interview and Blood Response Rates Among Children Aged 18 Months to 14 Years, KAIS 2012
| Total Eligible | Boy | Girl | P | Rural | Urban | P | |
|---|---|---|---|---|---|---|---|
| Number eligible for blood draw (18 months to 14 years) | 6302 | 3196 | 3106 | — | 1682 | 4620 | — |
| Blood draw response rate (%) (18 months to 14 years) | 68.9 | 69.1 | 68.6 | 0.6600 | 62.8 | 71.1 | <0.0001 |
| Number eligible for interview (10–14 yrs) | 2094 | 1037 | 1057 | — | 543 | 1551 | — |
| Interview response rate (%) (10–14 yrs) | 79.3 | 79.2 | 79.3 | 0.3100 | 79.2 | 79.7 | 0.5000 |
Among participants aged 15–64 years and emancipated minors who completed an interview, more than half were women, and close to half were persons aged 15–29 years (Table 3). Married or cohabiting participants accounted for almost 60% of survey respondents. The majority of participants resided in rural areas with Rift Valley region having the highest representation of all respondents. About half of the subjects were currently employed and two-thirds were Protestant Christian. The distribution of sociodemographic characteristics among KAIS 2007 and KAIS 2012 survey respondents was similar with respect to age, sex, marital status, and regional distribution.
TABLE 3.
Demographic Characteristics of Individuals* Aged 15–64 Years and Emancipated Minors, KAIS 2007 and KAIS 2012
| KAIS 2012 |
||||||
|---|---|---|---|---|---|---|
| Characteristic | Men (N = 5766) Unweighted, n |
Weighted % (95% CI) |
Women (N = 7954) Unweighted, n |
Weighted % (95% CI) |
Total (N = 13,720) Unweighted, n |
Weighted % (95% CI) |
| Age group, yrs | ||||||
| 15–19 | 1073 | 18.2 (16.8 to 19.7) | 1220 | 15.3 (14.2 to 16.5) | 2293 | 16.8 (15.8 to 17.7) |
| 20–24 | 846 | 14.9 (13.7 to 16.0) | 1403 | 17.6 (16.5 to 18.7) | 2249 | 16.3 (15.4 to 17.1) |
| 25–29 | 828 | 14.6 (13.5 to 15.8) | 1313 | 16.6 (15.6 to 17.6) | 2141 | 15.6 (14.8 to 16.4) |
| 30–34 | 716 | 12.2 (11.3 to 13.2) | 981 | 12.4 (11.5 to 13.4) | 1697 | 12.3 (11.7 to 13.0) |
| 35–39 | 583 | 10.4 (9.6 to 11.3) | 833 | 10.4 (9.6 to 11.2) | 1416 | 10.4 (9.8 to 11.0) |
| 40–44 | 493 | 8.6 (7.8 to 9.4) | 669 | 8.4 (7.7 to 9.0) | 1162 | 8.5 (8.0 to 9.0) |
| 45–49 | 357 | 6.1 (5.5 to 6.8) | 492 | 6.3 (5.7 to 7.0) | 849 | 6.2 (5.8 to 6.7) |
| 50–54 | 372 | 6.4 (5.7 to 7.0) | 473 | 5.9 (5.3 to 6.5) | 845 | 6.1 (5.7 to 6.6) |
| 55–59 | 277 | 4.7 (4.0 to 5.3) | 320 | 4.0 (3.5 to 4.5) | 597 | 4.3 (3.9 to 4.8) |
| 60–64 | 221 | 3.8 (3.2 to 4.4) | 250 | 3.1 (2.6 to 3.5) | 471 | 3.4 (3.0 to 3.8) |
| 15–24 | 1919 | 33.1 (31.5 to 34.8) | 2622 | 32.9 (31.7 to 34.2) | 4541 | 33.0 (32.0 to 34.1) |
| 15–49 | 4896 | 85.1 (84.0 to 86.3) | 6910 | 87.1 (86.1 to 88.0) | 11,806 | 86.1 (85.2 to 87.0) |
| 50–64 | 870 | 14.9 (13.7 to 16.0) | 1043 | 12.9 (12.0 to 13.9) | 1913 | 13.9 (13.0 to 14.7) |
| Highest educational attainment | ||||||
| No primary | 381 | 3.8 (2.9 to 4.8) | 1197 | 10.6 (8.8 to 12.4) | 1578 | 7.3 (6.0 to 8.6) |
| Incomplete primary | 450 | 6.7 (5.4 to 7.9) | 710 | 8.4 (7.3 to 9.5) | 1160 | 7.6 (6.7 to 8.4) |
| Complete primary | 1893 | 32.5 (30.6 to 34.4) | 2423 | 32.1 (30.3 to 33.9) | 4316 | 32.3 (30.9 to 33.7) |
| Secondary or higher | 3042 | 57.0 (54.6 to 59.3) | 3624 | 48.9 (46.8 to 50.9) | 6666 | 52.8 (51.1 to 54.6) |
| Marital status | ||||||
| Never married/never cohabited | 2256 | 38.7 (37.0 to 40.4) | 2015 | 25.5 (24.1 to 26.9) | 4271 | 32.0 (30.7 to 33.2) |
| Ever widowed | 49 | 0.8 (0.5 to 1.1) | 561 | 7.0 (6.3 to 7.7) | 610 | 4.0 (3.6 to 4.3) |
| Separated/divorced | 219 | 3.8 (3.2 to 4.4) | 439 | 5.4 (4.8 to 6.0) | 658 | 4.7 (4.2 to 5.1) |
| Married/cohabiting- polygamous |
239 | 3.8 (3.1 to 4.5) | 691 | 8.2 (7.1 to 9.3) | 930 | 6.0 (5.2 to 6.8) |
| Married/cohabiting- monogamous |
2999 | 52.8 (51.1 to 54.4) | 4242 | 53.8 (52.3 to 55.4) | 7241 | 53.3 (52.1 to 54.6) |
| Living with partner/spouse | ||||||
| Yes | 2780 | 85.7 (83.6 to 87.9) | 3818 | 78.0 (76.3 to 79.8) | 6598 | 81.6 (80.1 to 83.1) |
| Residence | ||||||
| Rural | 3531 | 61.4 (58.5 to 64.2) | 5107 | 64.5 (62.1 to 66.8) | 8638 | 62.9 (60.5 to 65.4) |
| Urban | 2235 | 38.6 (35.8 to 41.5) | 2847 | 35.5 (33.2 to 37.9) | 5082 | 37.1 (34.6 to 39.5) |
| Region | ||||||
| Nairobi | 796 | 11.6 (10.3 to 13.0) | 949 | 10.3 (9.2 to 11.4) | 1745 | 11.0 (9.9 to 12.0) |
| Central | 654 | 13.2 (11.1 to 15.3) | 926 | 13.2 (11.7 to 14.7) | 1580 | 13.2 (11.5 to 14.9) |
| Coast | 714 | 9.4 (8.0 to 10.9) | 998 | 9.1 (7.6 to 10.7) | 1712 | 9.3 (7.9 to 10.7) |
| Eastern | 1089 | 15.2 (13.1 to 17.3) | 1595 | 15.6 (14.0 to 17.2) | 2684 | 15.4 (13.7 to 17.1) |
| Nyanza | 774 | 13.4 (11.5 to 15.2) | 1060 | 14.7 (13.0 to 16.3) | 1834 | 14.0 (12.4 to 15.7) |
| Rift Valley | 1058 | 26.7 (23.6 to 29.9) | 1426 | 25.7 (23.1 to 28.4) | 2484 | 26.2 (23.5 to 29.0) |
| Western | 681 | 10.4 (8.9 to 11.9) | 1000 | 11.3 (9.9 to 12.7) | 1681 | 10.9 (9.5 to 12.2) |
| Employment | ||||||
| Employed in last week | 3331 | 59.0 (56.7 to 61.4) | 2836 | 37.9 (35.9 to 39.9) | 6167 | 48.2 (46.4 to 50.1) |
| Wealth index | ||||||
| Poorest | 1131 | 18.1 (15.4 to 20.9) | 1719 | 20.2 (17.5 to 23.0) | 2850 | 19.2 (16.6 to 21.8) |
| Second | 1162 | 20.2 (18.1 to 22.2) | 1695 | 21.4 (19.5 to 23.4) | 2857 | 20.8 (18.9 to 22.7) |
| Middle | 1135 | 20.0 (17.9 to 22.0) | 1540 | 19.7 (17.8 to 21.6) | 2675 | 19.8 (17.9 to 21.7) |
| Fourth | 1195 | 21.1 (18.7 to 23.5) | 1385 | 17.6 (15.6 to 19.6) | 2580 | 19.3 (17.2 to 21.4) |
| Richest | 1143 | 20.6 (17.8 to 23.5) | 1615 | 21.0 (18.3 to 23.8) | 2758 | 20.8 (18.1 to 23.6) |
| Religion | ||||||
| Roman Catholic | 1318 | 24.2 (21.9 to 26.4) | 1733 | 23.0 (20.8 to 25.3) | 3051 | 23.6 (21.6 to 25.6) |
| Protestant/other Christian | 3487 | 64.4 (61.9 to 67.0) | 5088 | 68.4 (65.8 to 71.0) | 8575 | 66.5 (64.1 to 68.8) |
| Muslim | 610 | 5.8 (4.2 to 7.4) | 835 | 5.5 (3.8 to 7.3) | 1445 | 5.6 (4.0 to 7.3) |
| No religion | 240 | 4.5 (3.3 to 5.6) | 182 | 2.0 (1.2 to 2.8) | 422 | 3.2 (2.5 to 4.0) |
| Other | 110 | 1.2 (0.4 to 1.9) | 113 | 1.0 (0.6 to 1.4) | 223 | 1.1 (0.6 to 1.6) |
| Nationality | ||||||
| Kenyan | 5729 | 99.4 (99.2 to 99.7) | 7898 | 99.4 (99.2 to 99.6) | 13,627 | 99.4 (99.3 to 99.6) |
| Non-Kenyan | 37 | 0.6 (0.3 to 0.8) | 56 | 0.6 (0.4 to 0.8) | 93 | 0.6 (0.4 to 0.7) |
|
| ||||||
|
KAIS 2007
|
||||||
| Characteristic |
Men (N = 7701)
Weighted % (95% CI) |
Women (N = 10,239)
Weighted % (95% CI) |
Total (N = 17,940)
Weighted % (95% CI) |
|||
|
| ||||||
| Age group, yrs | ||||||
| 15–19 | 18.6 (17.3 to 19.8) | 15.5 (14.7 to 16.3) | 16.8 (16.1 to 17.6) | |||
| 20–24 | 15.7 (14.7 to 16.6) | 17.8 (16.9 to 18.8) | 16.9 (16.1 to 17.7) | |||
| 25–29 | 12.6 (11.7 to 13.6) | 15.0 (14.2 to 15.9) | 14.0 (13.3 to 14.7) | |||
| 30–34 | 11.3 (10.4 to 12.1) | 12.3 (11.5 to 13.1) | 11.9 (11.2 to 12.5) | |||
| 35–39 | 10.1 (9.4 to 10.9) | 10.7 (10.0 to 11.4) | 10.5 (9.9 to 11.0) | |||
| 40–44 | 8.2 (7.4 to 8.9) | 8.2 (7.5 to 8.8) | 8.2 (7.6 to 8.7) | |||
| 45–49 | 7.7 (7.1 to 8.4) | 7.9 (7.3 to 8.5) | 7.8 (7.4 to 8.3) | |||
| 50–54 | 5.5 (5.0 to 6.1) | 5.2 (4.7 to 5.7) | 5.3 (4.9 to 5.7) | |||
| 55–59 | 5.6 (5.0 to 6.2) | 4.7 (4.1 to 5.2) | 5.1 (4.7 to 5.5) | |||
| 60–64 | 4.7 (4.2 to 5.3) | 2.7 (2.3 to 3.0) | 3.5 (3.2 to 3.9) | |||
| 15–24 | 34.2 (32.8 to 35.7) | 33.4 (32.4 to 34.4) | 33.7 (32.8 to 34.7) | |||
| 15–49 | 84.1 (83.2 to 85.1) | 87.5 (86.6 to 88.3) | 86.1 (85.4 to 86.8) | |||
| 50–64 | 15.9 (14.9 to 16.8) | 12.5 (11.7 to 13.4) | 13.9 (13.2 to 14.6) | |||
| Highest educational attainment | ||||||
| No primary | 6.5 (5.5 to 7.5) | 15.0 (13.6 to 16.4) | 11.4 (10.3 to 12.5) | |||
| Incomplete primary | 29.3 (27.5 to 31.2) | 29.6 (28.1 to 31.2) | 29.5 (28.0 to 31.0) | |||
| Complete primary | 24.5 (23.1 to 25.8) | 24.8 (23.6 to 25.9) | 24.6 (23.6 to 25.6) | |||
| Secondary or higher | 39.7 (37.5 to 42.0) | 30.5 (28.5 to 32.6) | 34.5 (32.5 to 36.4) | |||
| Marital status | ||||||
| Never married/never cohabited | 37.1 (35.5 to 38.6) | 23.1 (21.8 to 24.4) | 29.1 (27.9 to 30.2) | |||
| Ever widowed | 1.4 (1.0 to 1.7) | 7.4 (6.8 to 8.0) | 4.8 (4.4 to 5.2) | |||
| Separated/divorced | 4.2 (3.7 to 4.8) | 6.8 (6.0 to 7.5) | 5.7 (5.2 to 6.2) | |||
| Married/cohabiting-polygamous | 4.6 (4.0 to 5.2) | 8.3 (7.5 to 9.2) | 6.7 (6.1 to 7.4) | |||
| Married/cohabiting-monogamous | 52.7 (51.2 to 54.2) | 54.4 (52.8 to 55.9) | 53.7 (52.4 to 54.9) | |||
| Living with partner/spouse | 83.5 (81.4 to 85.6) | 72.7 (71.1 to 74.2) | 77.1 (75.7 to 78.5) | |||
| Residence | ||||||
| Rural | 77.6 (74.9 to 80.3) | 76.1 (72.8 to 79.5) | 76.8 (73.8 to 79.7) | |||
| Urban | 22.4 (19.7 to 25.1) | 23.9 (20.5 to 27.2) | 23.2 (20.3 to 26.2) | |||
| Region | ||||||
| Nairobi | 9.3 (7.8 to 10.8) | 9.8 (8.5 to 11.2) | 9.6 (8.4 to 10.9) | |||
| Central | 14.5 (13.1 to 16.0) | 14.4 (12.9 to 15.8) | 14.4 (13.1 to 15.8) | |||
| Coast | 7.6 (6.5 to 8.8) | 8.1 (6.7 to 9.5) | 7.9 (6.7 to 9.1) | |||
| Eastern | 18.5 (16.2 to 20.9) | 17.4 (15.7 to 19.2) | 17.9 (16.0 to 19.8) | |||
| Nyanza | 15.5 (13.7 to 17.4) | 15.7 (14.1 to 17.3) | 15.6 (14.0 to 17.3) | |||
| Rift Valley | 22.5 (20.1 to 24.8) | 22.6 (19.4 to 25.7) | 22.5 (19.8 to 25.3) | |||
| Western | 12.0 (10.5 to 13.5) | 12.0 (10.6 to 13.4) | 12.0 (10.7 to 13.3) | |||
| Employment | ||||||
| Employed in last week | 80.8 (79.5 to 82.1) | 63.3 (61.9 to 64.8) | 70.8 (69.7 to 71.9) | |||
| Wealth index | ||||||
| Poorest | 15.4 (13.3 to 17.4) | 15.6 (13.8 to 17.4) | 15.5 (13.7 to 17.3) | |||
| Second | 17.8 (16.1 to 19.5) | 17.6 (16.1 to 19.2) | 17.7 (16.1 to 19.3) | |||
| Middle | 19.9 (18.3 to 21.5) | 19.6 (18.2 to 21.1) | 19.7 (18.3 to 21.2) | |||
| Fourth | 21.3 (19.3 to 23.3) | 21.5 (19.8 to 23.3) | 21.4 (19.7 to 23.2) | |||
| Richest | 25.6 (22.9 to 28.4) | 25.6 (22.7 to 28.5) | 25.6 (22.9 to 28.3) | |||
| Religion | ||||||
| Roman Catholic | 28.0 (25.8 to 30.2) | 24.8 (22.9 to 26.7) | 26.1 (24.2 to 28.0) | |||
| Protestant/other Christian | 60.7 (58.3 to 63.0) | 65.8 (63.8 to 67.9) | 63.6 (61.6 to 65.7) | |||
| Muslim | 6.5 (5.6 to 7.5) | 7.1 (6.1 to 8.1) | 6.9 (5.9 to 7.8) | |||
| No religion | 4.1 (3.3 to 4.8) | 1.7 (1.2 to 2.2) | 2.7 (2.2 to 3.2) | |||
| Other | 0.7 (0.4 to 1.1) | 0.6 (0.2 to 1.1) | 0.7 (0.4 to 1.0) | |||
| Nationality | ||||||
| Kenyan | — | — | — | |||
| Non-Kenyan | — | — | — | |||
The sums for individual variables may not add up to the totals in the column headings because of missing data.
CI, confidence interval.
The median age of surveyed children aged 10–14 years was 12 years (Table 4). Sex was equally distributed among interviewed children, with 49.7% girls compared with 50.3% boys. Most children were rural residents (75.6%) and were surveyed in the Rift Valley region (29.9%).
TABLE 4.
Demographic Characteristics of Children Aged 10–14 Years, KAIS 2012
| Characteristic | Crude, n | Weighted % (95% CI) |
|---|---|---|
| Total | 1661 | |
| Median age (yrs) | 12 | — |
| Sex | ||
| Boy | 822 | 50.3 (47.5 to 53.1) |
| Girl | 839 | 49.7 (46.9 to 52.5) |
| Residence | ||
| Rural | 1236 | 75.6 (71.8 to 79.5) |
| Urban | 425 | 24.4 (20.5 to 28.2) |
| Region | ||
| Nairobi | 111 | 6.1 (4.8 to 7.3) |
| Central | 181 | 10.5 (8.7 to 12.3) |
| Coast | 227 | 9.4 (7.0 to 11.7) |
| Eastern | 349 | 16.1 (12.5 to 19.7) |
| Nyanza | 231 | 14.9 (12.3 to 17.5) |
| Rift Valley | 306 | 29.9 (24.7 to 35.1) |
| Western | 256 | 13.1 (10.9 to 15.4) |
| Wealth index | ||
| Poorest | 453 | 28.2 (22.3 to 34.1) |
| Second | 419 | 25.5 (22.0 to 29.0) |
| Middle | 366 | 22.2 (18.8 to 25.6) |
| Fourth | 237 | 13.3 (10.6 to 16.1) |
| Richest | 186 | 10.8 (8.5 to 13.1) |
CI, confidence interval.
A total of 16,807 DBS specimens and 14,993 venous blood specimens were received at the NHRL. Of the venous blood specimens received, 1254 were not suitable for CD4+ T-cell testing primarily because of hemolysis of the blood during transport. Furthermore, of 15,979 participants who gave a blood sample, 1135 provided a DBS only (as opposed to venous sample) from which we could not measure CD4+ T-cell counts. Because of this, less than half (46.2%) of HIV antibody–positive specimens had a valid CD4+ T-cell test result from the national laboratory.
DBS specimens that were not used for primary testing at NHRL were stored for future anticipated testing for recent HIV infection and other unspecified biologic testing. Overall, HBTC services were requested by 72% of survey participants.18 Among participants who had an HBTC HIV test result and a central laboratory HIV test result, the overall agreement of results was 99% (data not shown).
DISCUSSION
KAIS 2012 provided data for monitoring HIV prevalence and HIV-related behaviors among the general population. Although KAIS 2007 had a larger sample size, the distribution and sociodemographic characteristics of respondents in the 2 surveys were similar. KAIS 2012 included several new elements to enhance the utility of data collected from a national HIV serologic survey to inform Kenya’s national strategy for prevention, care, and treatment. Data from KAIS 2012 permited analysis of sexual concurrency in relationships, HIV testing patterns within sexual partnerships, and same sex partnerships; previously, these had not been examined. The survey collected information to calculate national size estimates for populations at high risk for HIV infection. Behavioral and clinical data on HIV-infected persons, including knowledge of HIV infection, use of ART, CD4+ T-cell count, and viral load, enabled us to construct a clinical cascade describing the continuum of care among HIV-infected persons in the country, following persons from HIV infection to diagnosis, entry and retention in care, use of and adherence to ART, and virologic suppression.
For the first time, a national household survey in Kenya included an assessment of HIV prevalence, correlates of HIV infection, sociodemographic characteristics, sexual norms, HIV risk perception, and HIV-related stigma among children. Another innovation was the pairing of HBTC services with POC CD4 testing, allowing study participants to receive their CD4+ T-cell counts at the time of testing within their homes. This also provided data for comparison of POC results to CD4 test results from the national laboratory. KAIS 2012 used up-to-date technology for data collection and transmission, allowing for real-time monitoring of survey progress and response rates, maximizing data quality and minimizing time for data entry and data cleaning, thereby facilitating rapid dissemination of key findings.
KAIS 2012 had several limitations. The survey response rate was lower than expected for both interview and blood draw response rates, which we had a priori estimated to be 90% based on results from KAIS 2007. The household interview, individual interview, and blood draw response rates were lower than documented in KAIS 2007, where the household and individual interview rates were above 90% and blood draw response rate was 88%.3 Lower participation in the blood draw could introduce selection bias if participation was associated with knowledge of HIV infection, potentially leading to an underestimate of national HIV prevalence.19 Participation of children aged 10–14 years was lower than expected because many were away at school during the survey. Infants younger than 18 months of age were excluded because of logistical difficulties in conducting polymerase chain reaction tests in the field and returning these results back to participants. Consequently, KAIS 2012 data excluded potential cases of HIV infection in this age group, underscoring an important gap in the ability to provide a comprehensive assessment of HIV infection and need for services for all children in Kenya. In addition, we were unable to survey North Eastern region because of regional security concerns. In KAIS 2007, North Eastern region had the fewest number of participants and the lowest HIV prevalence.3 Therefore, it is unlikely that omission of North Eastern region contributed to underestimation of national HIV prevalence in KAIS 2012. Finally, approximately half of HIV-positive samples did not have corresponding CD4+ T-cell count data, limiting our ability to comprehensively estimate eligibility for ART and ART coverage among treatment eligible persons. To limit bias, we weighted our estimates of ART need and coverage to account for missing CD4+ T-cell count data among HIV-positive persons.
Despite this the overall sample sizes for adults and children were large enough to provide adequately robust regional and national estimates of HIV prevalence. Findings from this survey will be used to validate and calibrate existing surveillance data and guide the country’s HIV programs in strengthening prevention, treatment, care, and surveillance initiatives. Kenya’s recent transition into a devolved government system also necessitates that these data be sufficiently detailed to assist planning, budgeting, and programming up to regional and subregional levels.
In generalized epidemics, population-based surveys of the general population are critical for obtaining information for monitoring epidemic trends, guiding programmatic responses, and evaluating key initiatives.8,20 Data from KAIS 2007 had substantial influence in determining and refining Kenya’s response to HIV/AIDS over the past 5 years.8 As the new Kenya National AIDS Strategic Plan is being formed, important political and programmatic impact is expected from the results of KAIS 2012.
ACKNOWLEDGMENTS
The authors thank the fieldworkers and supervisors for their excellent work during KAIS 2012 data collection. They also gratefully acknowledge all the children and families who participated in this national survey. The authors would like to thank George Rutherford, Kevin DeCock, Janet Lee, and Joy Mirjahangir for reviewing and providing input on the article; Ray Shiraishi, Eddas Bennett, and Paul Stupp for their input on weighting of the data set; and the KAIS 2012 Study Group for their contribution to the design of the survey and collection of the data set: Willis Akhwale, Sehin Birhanu, John Bore, Angela Broad, Robert Buluma, Thomas Gachuki, Jennifer Galbraith, Anthony Gichangi, Beth Gikonyo, Margaret Gitau, Joshua Gitonga, Mike Grasso, Malayah Harper, Andrew Imbwaga, Muthoni Junghae, Mutua Kakinyi, Samuel Mwangi Kamiru, Nicholas Owenje Kandege, Lucy Kanyara, Yasuyo Kawamura, Timothy Kellogg, George Kichamu, Andrea Kim, Lucy Kimondo, Davies Kimanga, Elija Kinyanjui, Stephen Kipkerich, Danson Kimutai Koske, Boniface O. K’Oyugi, Veronica Lee, Serenita Lewis, William Maina, Ernest Makokha, Agneta Mbithi, Joy Mirjahangir, Ibrahim Mohamed, Rex Mpazanje, Nicolas Muraguri, Patrick Murithi, Lilly Muthoni, James Muttunga, Jane Mwangi, Mary Mwangi, Sophie Mwanyumba, Silas Mulwa, Francis Ndichu, Anne Ng’ang’a, James Ng’ang’a, John Gitahi Ng’ang’a, Lucy Ng’ang’a, Carol Ngare, Bernadette Ng’eno, Inviolata Njeri, David Njogu, Bernard Obasi, Macdonald Obudho, Edwin Ochieng, Linus Odawo, Jacob Odhiambo, Caleb Ogada, Samuel Ogola, David Ojakaa, James Kwach Ojwang, George Okumu, Patricia Oluoch, Tom Oluoch, Kenneth Ochieng Omondi, Osborn Otieno, Yakubu Owolabi, Bharat Parekh, George Rutherford, Sandra Schwarcz, Shahnaaz Sharrif, Victor Ssempiijja, Lydia Tabuke, Yuko Takanaka, Mamo Umuro, Brian Eugene Wakhutu, Celia Wandera, John Wanyungu, Wanjiru Waruiru, Anthony Waruru, Paul Waweru, Larry Westerman, and Kelly Winter.
Kenya AIDS Indicator Survey (KAIS) 2012 was supported by the National AIDS and STI Control Programme (NASCOP), Kenya National Bureau of Statistics (KNBS), National Public Health Laboratory Services (NPHLS), National AIDS Control Council (NACC), National Council for Population and Development (NCPD), Kenya Medical Research Institute (KEMRI), US Centers for Disease Control and Prevention (CDC/Kenya, CDC/Atlanta), United States Agency for International Development (USAID/Kenya), University of California, San Francisco (UCSF), Joint United Nations Team on HIV/AIDS, Japan International Cooperation Agency (JICA), Elizabeth Glaser Paediatric AIDS Foundation (EGPAF), Liverpool Voluntary Counselling and Testing (LVCT), African Medical and Research Foundation (AMREF), World Bank, and Global Fund. This publication was made possible by support from the US President’s Emergency Plan for AIDS Relief through cooperative agreements (PS001805, GH000069, and PS001814) from the US Centers for Disease Control and Prevention, Division of Global HIV/AIDS. This work was also funded in part by support from the Global Fund, World Bank, and the Joint United Nations Team for HIV/AIDS.
Footnotes
The authors have no conflicts of interest to disclose.
The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the US Centers for Disease Control and Prevention and the Government of Kenya.
REFERENCES
- 1.National AIDS Control Council (NACC) The Kenya AIDS Epidemic Update, 2011. NACC; Nairobi, Kenya: 2012. Available at: http://www.unaids.org/en/dataanalysis/knowyourresponse/countryprogressreports/2012countries. Accessed May 20, 2013. [Google Scholar]
- 2.oint United Nations Programme on HIV/AIDS (UNAIDS) Global AIDS Report 2012. UNAIDS; Geneva, Switzerland: 2012. Available at: http://www.unaids.org/en/dataanalysis/datatools/aidsinfo. Accessed June 19, 2013. [Google Scholar]
- 3.National AIDS and STI Control Programme (NASCOP) 2007 Kenya AIDS Indicator Survey Final Report. NASCOP; Nairobi, Kenya: 2009. Available at: http://nascop.or.ke. Accessed May 20, 2013. [Google Scholar]
- 4.Kaiser R, Bunnell R, Hightower A, et al. Factors associated with HIV infection in married or cohabitating couples in Kenya: results from a nationally representative study. PLoS One. 2011;6:e17842. doi: 10.1371/journal.pone.0017842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mwandi Z, Bunnell R, Cherutich P, et al. Male circumcision programmes in Kenya: lessons from the Kenya AIDS Indicator Survey 2007. Bull World Health Organ. 2012;90:642–651. doi: 10.2471/BLT.11.096412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cherutich P, Kaiser R, Galbraith J, et al. Lack of knowledge of HIV status a major barrier to HIV prevention, care and treatment efforts in Kenya: results from a nationally representative study. PLoS One. 2012;7:e36797. doi: 10.1371/journal.pone.0036797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mwangi M, Bunnell R, Nyoka R, et al. Unsafe sex among HIV-infected adults in Kenya: results of a nationally representative survey. J Acquir Immune Defic Syndr. 2011;58:80–88. doi: 10.1097/QAI.0b013e3182251001. [DOI] [PubMed] [Google Scholar]
- 8.Maina WK, Kim AA, Rutherford G, et al. Kenya AIDS Indicator Surveys 2007 and 2012: implications for public health policies for HIV prevention and treatment. J Acquir Immune Defic Syndr. 2014;66(suppl 1):S130–S137. doi: 10.1097/QAI.0000000000000123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.National AIDS and STI Control Programme (NASCOP) and Population Council . 2010-2011 Integrated Biological and Behavioural Survey Among Most-at-Risk Populations in Nairobi and Kisumu, Kenya. NASCOP; Nairobi, Kenya: 2013. [Google Scholar]
- 10.Kenya National Bureau of Statistics (KNBS) National Sample Survey and Evaluation Programme (NASSEP) V Frame. Nairobi, Kenya: 2012. Available at: http://www.knbs.or.ke. Accessed June 19, 2013. [Google Scholar]
- 11.Ojwang’ JK, Lee VC, Waruru A, et al. Using information and communications technology in a national population-based survey: the Kenya AIDS Indicator Survey 2012. J Acquir Immune Defic Syndr. 2014;66(suppl 1):S123–S129. doi: 10.1097/QAI.0000000000000116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rutstein SO, Johnson K. The DHS Wealth Index. DHS Comparative Reports No. 6. ORC Macro; Calverton, Maryland: 2004. [Google Scholar]
- 13.Ballard T, Coates J, Swindale A, et al. Household Hunger Scale: Indicator Definition and Measurement Guide. Food and Nutrition Technical Assistance II Project (FANTA-2) Bridge. Vol. 360. FHI; Washington, DC: 2011. [Google Scholar]
- 14.National AIDS and STI Control Programme (NASCOP) National Guidelines for HIV Testing and Counseling in Kenya, 2nd ed. NASCOP; Nairobi, Kenya: 2010. Available at: http://www.nascop.or.ke. Accessed June 14, 2013. [Google Scholar]
- 15.Redondo M, Garrido C, Parkin N, et al. Comparison of HIV-1 RNA measurements obtained by using plasma and dried blood spots in the automated abbott real-time viral load assay. J Clin Microbiol. 2012;50:569–572. doi: 10.1128/JCM.00418-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.National AIDS and STI Control Programme (NASCOP) Guidelines for Antiretroviral Therapy in Kenya. 4th. NASCOP; Nairobi, Kenya: 2011. Available at: http://www.nascop.or.ke. Accessed June 14, 2013. [Google Scholar]
- 17.Kenya National Bureau of Statistics (KNBS) 2009 Population and Housing Census. KNBS; Nairobi, Kenya: 2010. Available at: http://www.knbs.or.ke. Accessed June 19, 2013. [Google Scholar]
- 18.Ng’ang’a A, Waruiru W, Ngare C, et al. The status of HIV testing and counseling in Kenya: results from a nationally representative population-based survey. J Acquir Immune Defic Syndr. 2014;66(suppl 1):S27–S36. doi: 10.1097/QAI.0000000000000102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Floyd S, Molesworth A, Dube A, et al. Underestimation of HIV prevalence in surveys when some people already know their status, and ways to reduce the bias. AIDS. 2013;27:233–242. doi: 10.1097/QAD.0b013e32835848ab. [DOI] [PubMed] [Google Scholar]
- 20.Joint United Nations Program on HIV/AIDS and World Health Organization . Guidelines for Second Generation HIV Surveillance. UNAIDS; Geneva, Switzerland: 2000. Available at: http://www.unaids.org/en/media/unaids/contentassets/dataimport/publications/irc-pub01/jc370-2ndgeneration_en.pdf. Accessed May 24, 2013. [Google Scholar]