Abstract
Objective
Point-of-care ultrasound (POCUS) is a vital tool for diagnosis and management of critically ill patients, particularly in resource-limited settings where access to diagnostic imaging may be constrained. We aimed to develop a novel POCUS training curriculum for surgical practice in the United States and in resource-limited settings in low- and middle-income countries and to determine its effect on surgical resident self-assessments of efficacy and confidence.
Design
We conducted an observational cohort study evaluating a POCUS training course that comprised 7 sessions of 2 hours each with didactics and proctored skills stations covering ultrasound applications for trauma (Focused Assessement with Sonography for Trauma (FAST) examination), obstetrics, vascular, soft tissue, regional anesthesia, focused echocardiography, and ultrasound guidance for procedures. Surveys on attitudes, prior experience, and confidence in point-of-care ultrasound applications were conducted before and after the course.
Setting
General Surgery Training Program in Seattle, Washington.
Participants
A total of 16 residents participated in the course; 15 and 10 residents completed the precourse and postcourse surveys, respectively.
Results
The mean composite confidence score from pretest compared with posttest improved from 23.3 (±10.2) to 37.8 (±6.7). Median confidence scores (1-6 scale) improved from 1.5 to 5.0 in performance of FAST (p < 0.001). Residents reported greater confidence in their ability to identify pericardial (2 to 4, p = 0.009) and peritoneal fluid (2 to 4.5, p < 0.001), to use ultrasound to guide procedures (3.5 to 4.0, p = 0.008), and to estimate ejection fraction (1 to 4, p = 0.004). Both before and after training, surgical residents overwhelmingly agreed with statements that ultrasound would improve their US-based practice, make them a better surgical resident, and improve their practice in resource-limited settings.
Conclusions
After a POCUS course designed specifically for surgeons, surgical residents had improved self-efficacy and confidence levels across a broad range of skills.
Keywords: education, ultrasound
Introduction
In interdisciplinary settings throughout the United States, point-of-care ultrasound (POCUS) use has grown tremendously over the past 2 decades. Initially developed for specific indications such as the Focused Assessment with Sonography for Trauma (FAST) examination or in the evaluation of obstetric patients, portable ultrasound has expanded to be used in virtually every clinical environment.1-3 Given its utility and prevalence, and with the recognition that ultrasound proficiency is operator dependent, some specialties have developed rigorous training requirements in point-of-care ultrasound.
In emergency medicine, the Residency Review Committee (RRC) and Council of Residency Directors (CORD) have mandated minimum standards for ultrasound training during residency, which includes a core lecture series and an ultrasound rotation of 2-4 weeks with dedicated hands-on experience.4,5 Other specialties have developed ultrasound curricula for critical care physicians focused on chest and procedural ultrasound, as well as ultrasound for patients in shock.2 Several medical schools have undergraduate curricula integrating ultrasound into the preclinical years, with the belief that early exposure to ultrasound may improve understanding of functional anatomy and familiarize students with the clinical utility of point-of-care ultrasound.6,7 Like emergency medicine and critical care physicians, general surgeons frequently use ultrasound in their practice for both diagnostic purposes (such as hemoperitoneum and abscesses) and procedural guidance (such as placement of a central venous catheter or paracentesis).8
Recognizing the importance of ultrasound training for surgeons, in 1996, the American College of Surgeons developed an educational program specifically for ultrasound use for trauma, vascular surgery, head and neck surgery, and intraoperative applications.1 The ACS course is an opportunity for surgeons to develop their hands-on skills, and 65% of participants surveyed reported using ultrasound in their practice after the course.1 Additionally, several studies have demonstrated that surgeons can effectively perform and interpret ultrasound examination results after POCUS training programs.9-11 Despite the increasing use of POCUS within surgical practice, there are no standardized training recommendations from accreditation bodies for general surgery residencies.
Within the United States, surgical residents identify ultrasound as crucial for their training.12,13 General surgery residents increasingly indicate an interest in working in resource-limited settings, where ultrasound proficiency is invaluable.14,15 POCUS skills, although important in the United States, are even more crucial in resource-limited settings where ultrasound is often the only diagnostic imaging modality available to evaluate patients presenting with conditions related to trauma, pregnancy, and acute undifferentiated abdominal pain. The World Health Organization has stated that plain radiography and ultrasound could be used to meet two-thirds of all imaging needs in resource-limited settings.16
In light of the increase in surgical residents interested in working in resource-limited settings and the value of ultrasound across settings, we sought to develop a novel POCUS course specifically designed for surgical residents interested in working in resource-limited settings, modeled off of similar courses in emergency medicine as well as the core curriculum taught to general practitioners in resource-limited settings, and to evaluate resident confidence with point-of-care ultrasound for a variety of applications. The curriculum represents one of only a handful of POCUS courses designed for surgical residents. It was novel in its focus on ultrasound modalities of particular use in resource-limited settings, and in that, it was designed and taught by a multidisciplinary faculty group.
Methods
Study Design
We conducted a prospective observational cohort study to test the hypothesis that a novel POCUS training program composed of didactic training and hands-on practice would improve confidence of general surgical residents in their facility with ultrasound for a variety of clinical applications.
Setting and Population
The study was conducted at an urban academic general surgical training program, using a convenience sample of 16 interested general surgery residents (R1-R5). The only previous ultrasound training that residents had was training in ultrasound guidance for central venous catheter placement and a brief FAST training session for senior residents. Training was provided by a multidisciplinary faculty with expertise in point-of-care ultrasound from the Departments of Surgery, Radiology, and Anesthesia and the Division of Emergency Medicine.
Intervention and Outcome
Residents completed a precourse survey regarding their confidence in using ultrasound for different applications. Participants then attended 7 sessions of 2 hours each over the course of 3 months. Sessions included lecture-based didactics by faculty instructors, immediately followed by proctored hands-on workshops using live models. Course topics included ultrasound physics and artifacts, the FAST examination, skin and soft tissue ultrasound, obstetrical ultrasound (early and late pregnancy), focused echocardiography and volume assessment (using aorta: inferior vena cava (IVC) ratio and collapsibility index), ultrasound for procedural guidance (paracentesis, thoracentesis, and pericardiocentesis), vascular ultrasound (evaluation of the abdominal aorta and diagnosis of deep vein thrombosis), and ultrasound-guided regional anesthesia (Table 1).
Table 1. Overview of the POCUS Training Curriculum.
| Lecture Topic | Content | Time |
|---|---|---|
| Introduction/physics | Introduction to ultrasound principles: gain, depth, knobology, machine safety, ALARA principle, and common artifacts | 30-minute lecture |
| eFAST examination | Identification of hemoperitoneum, hemopericardium, hemothorax, and pneumothorax | 45-minute lecture 2 hours hands-on |
| Focused cardiac ultrasound | Identification of pericardial effusion, assessment of ejection fraction, and volume assessment | 45-minute lecture 90 minutes hands-on |
| Focused obstetric ultrasound | First trimester: identification of early intrauterine pregnancy and signs of ectopic pregnancy | 1-hour lecture 1 hour hands-on |
| Late pregnancy: fetal heart rate, fetal lie, and estimation of gestational age | ||
| Skin and soft tissue ultrasound | Differentiation of cellulitis from abscess | 30-minute lecture 1 hour hands-on |
| Vascular ultrasound | Identification of abdominal aortic aneurysm and lower extremity deep venous thrombosis | 30-minute lecture 75 minutes hands-on |
| Ultrasound-guided procedures | Peripheral IV placement, assessment of fluid collections in paracentesis, thoracentesis, and pericardiocentesis | 45-minute lecture 75 minutes hands-on |
| Ultrasound-guided regional anesthesia | Principles of needle guidance; axillary and femoral nerve blocks | 1-hour lecture 1 hour hands-on |
ALARA, as low as reasonably achievable.
The primary outcome was the change in self-assessment scores on a series of measures regarding attitudes, confidence, and assessment of the value of ultrasound before and after the educational intervention. The self-assessment scores were measured using a 6-point Likert scale for each question. This study was approved by the University of Washington's Institutional Review Board.
Analysis
Scores for each question were summarized using medians and interquartile ranges. Composite scores were calculated for each participant, and both paired and unpaired analyses were conducted. Comparisons were performed using non-parametric tests for individual questions, given the small sample size. These comparisons were made using a Wilcoxon rank sum test. Among individuals whose presurvey and postsurvey results could be matched, composite scores were compared using a paired Student t test. All analyses were performed using STATA Version 12.1 (StataCorp, College Station, TX).
Results
A total of 16 residents participated in the course; 15 residents completed the precourse survey and 10 completed the postcourse survey. Owing to missing study identification numbers on the surveys, only 6 participants were able to have their presurvey and postsurvey matched.
Skill Confidence Scores
Median confidence scores (1-6 scale) improved for nearly all skills (Fig. 1). Residents stated that their ability to use ultrasound to formulate a diagnosis improved after the course, with statistically significant greater confidence scores in identifying pericardial and peritoneal fluid, procedural guidance, and estimation of cardiac ejection fraction (Fig. 1). There was no statistically significant difference in median confidence scores for understanding the limitations of the FAST examination or in the ability to use ultrasound to distinguish cellulitis and abscess. Residents reported greater confidence in performing the FAST examination, specifically indicating that they could perform it in less than 2 minutes and be the primary FAST sonographer in a trauma scenario.
Figure 1.
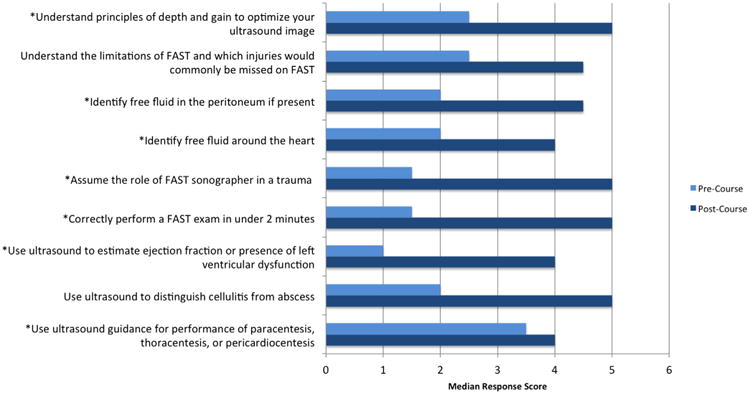
Precourse and postcourse surveys' median confidence scores. (*Indicates statistically significant; N = 10.)
In our paired analysis comparing presurvey and post-survey composite confidence scores, we found that there was a significant difference between the precomposite and postcomposite scores (23.3 ± 10.2 vs 37.8 ± 6.7, p = 0.03; maximum composite score = 68).
Utility of Ultrasound
Both before and after training, residents overwhelming agreed with statements that ultrasound would improve their US-based practice, make them a better surgical resident, and improve their practice in resource-limited settings, with median scores of 6 both before and after the course on all the 3 measures. All residents agreed with the statement that the ultrasound course helped them improve their point-of-care ultrasound knowledge and skills (median = 5, IQR = 1.25). All residents indicated that the course should be integrated into the formal surgical curriculum (median = 6, IQR = 1.25).
Discussion
Point-of-care ultrasound is increasingly used in the evaluation and management of patients in the United States and is of even greater importance in resource-limited settings where it is often the only imaging modality available. We found that a novel point-of-care ultrasound curriculum for surgical residents resulted in increased confidence in the ability to use and interpret ultrasound images for various applications. Residents participating in the study also overwhelmingly agree that ultrasound is important for their practice in the United States and in resource-limited settings.
Our course highlighted a number of different applications where POCUS might be a useful adjunct to clinical history and physical examination—obstetrics, volume assessment, echocardiography, and guidance for procedures. These applications were selected because of their relevance in caring for patients in resource-limited settings. Some applications such as skin and soft tissue ultrasound or FAST examination are natural POCUS applications for surgeons to learn. Others such as obstetrics or volume assessment are less obvious. In resource-limited settings, where a general surgeon is frequently the only surgical provider, emergency obstetrical care is a cornerstone of surgical practice. Ultrasound has been shown to be associated with faster recognition of ectopic pregnancy in the United States, accurate diagnosis of intrauterine growth retardation (IUGR) in Egypt, and prompt evaluation of fetal heart rate and fetal positioning in Tanzania.17-19
Acute diarrhea accounts for 17% of pediatric deaths worldwide, mainly due to severe dehydration.20 Ultrasound is increasingly used to diagnose and manage severe dehydration. POCUS is accurate and reliable for the diagnosis of severe dehydration in the United States.21 In resource-limited settings, such as Rwanda, assessment of dehydration using aorta to IVC ratio has a sensitivity of 93% and a specificity of 59%, making it superior to clinical assessment alone using the World Health Organization dehydration scale.22
In resource-limited settings, the lack of diagnostic equipment and trained personnel remains a major barrier to health care delivery. In this context, point-of-care ultrasound is a sustainable high-impact technology; it is easily learned, can confirm diagnoses, and can change clinical decision making. Point-of-care ultrasound skills are readily transferrable to midlevel providers, such as midwives.18,23 In an assessment of 345 scans performed in rural Rwanda, ultrasound use changed management plans in 43% of patients. The most frequent change in clinical management was the decision to proceed with a surgical procedure, such as a cesarean section, biopsy, or minor surgical intervention.24 The effect of POCUS extends to other health care settings, including a tertiary care hospital in Liberia, the Amazon jungle, and ambulatory clinics in Ghana.25-27
The results of this study must be interpreted in the context of study design. Firstly, our study had a small sample size, with just 16 participating residents. Only 10 residents completed both the precourse and postcourse surveys, and only 6 could be matched. As such, the sample size is a significant limitation of our findings. Secondly, residents volunteered to participate in this course and in the study; consequently, there may be a selection bias. These factors may limit the generalizability of our findings. Thirdly, in this study, we only assessed resident confidence in the use of ultrasound applications and not their actual skill or competence. We also did not measure the effect of the intervention on residents' skills in a resource-limited environment, where the setting and challenges may be different.
Conclusion
Our study confirms that a dedicated point-of-care ultrasound course improves confidence in using ultrasound among surgical residents. The skills learned in this course may prove beneficial for residents practicing in the United States and may be valuable in resource-limited settings where ultrasound is central in the evaluation of patients with various clinical presentations. As point-of-care ultrasound increases in utility and portability, we anticipate that its role in surgical practice would continue to grow. Regardless of the clinical setting, integration of POCUS training into general surgical residency curricula is of increasing importance.
Acknowledgments
Dr. Kotagal was supported by a University of Washington Department of Surgery T32 training fellowship grant from the National Institute of Diabetes & Digestive & Kidney Diseases (Grant number 5T32DK070555-03).
Footnotes
Competencies: Medical Knowledge
References
- 1.Staren ED, Knudson MM, Rozycki GS, Harness JK, Wherry DC, Shackford SR. An evaluation of the American College of Surgeons' ultrasound education program. Am J Surg. 2006;16(4):489–496. doi: 10.1016/j.amjsurg.2005.10.023. [DOI] [PubMed] [Google Scholar]
- 2.Neri L, Storti E, Lichetenstein D. Toward an ultrasound curriculum for critical care medicine. Crit Care Med. 2007;35(5):S290–S304. doi: 10.1097/01.CCM.0000260680.16213.26. [DOI] [PubMed] [Google Scholar]
- 3.Rozycki GS. Surgeon-performed ultrasound: its use in clinical practice. Ann Surg. 1998;228(1):16–28. doi: 10.1097/00000658-199807000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Heller MB, Mandavia D, Tayal VS, et al. Residency training in emergency ultrasound: fulfilling the mandate. Acad Emerg Med. 2002;9(8):835–839. doi: 10.1111/j.1553-2712.2002.tb02174.x. [DOI] [PubMed] [Google Scholar]
- 5.Akhtar S, Theodoro D, Gaspari R, et al. Resident training in emergency ultrasound: consensus recommendations from the 2008 Council of Emergency Medicine Residency Directors Conference. Acad Emerg Med. 2009;16(suppl 2):S32–S36. doi: 10.1111/j.1553-2712.2009.00589.x. [DOI] [PubMed] [Google Scholar]
- 6.Gogalniceanu P, Sheena Y, Kashef E, Purkayastha S, Darzi A, Paraskeva P. Is basic emergency ultrasound training feasible as part of standard undergraduate medical education? J Surg Ed. 2010;67(3):152–156. doi: 10.1016/j.jsurg.2010.02.008. [DOI] [PubMed] [Google Scholar]
- 7.Hoppmann RA, Rao VV, Poston MB, et al. An integrated ultrasound curriculum (iUSC) for medical students: 4 year experience. Crit Ultrasound J. 2011;3(1):1–12. doi: 10.1007/s13089-011-0052-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moore CL, Copel JA. Point-of-care ultrasonography. N Engl J Med. 2011;364(8):749–757. doi: 10.1056/NEJMra0909487. [DOI] [PubMed] [Google Scholar]
- 9.Forster R, Pillasch J, Zielke A, et al. Ultrasonography in blunt abdominal trauma: influence of the investigators' experience. J Trauma. 1993;34(2):264–269. [PubMed] [Google Scholar]
- 10.Rozycki GS, Oschner MG, Jaffin JH, et al. Prospective evaluation of surgeons' use of ultrasound in the evaluation of trauma patients. J Trauma. 1993;34(4):516–527. doi: 10.1097/00005373-199304000-00008. [DOI] [PubMed] [Google Scholar]
- 11.Wherrett LJ, Boulanger BR, McLellelan BL, et al. Hypotension after blunt abdominal trauma: the role of emergent abdominal sonography in surgical triage. J Trauma. 1996;41(5):815–820. doi: 10.1097/00005373-199611000-00008. [DOI] [PubMed] [Google Scholar]
- 12.Han DC, Rozycki GS, Schmidt JA, et al. Ultrasound training during ATLS: an early start for surgical interns. J Trauma. 1996;41(2):208–213. doi: 10.1097/00005373-199608000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Rozycki GS, Kraut EJ. Ultrasound: what every trauma surgeon should know. J Trauma. 1996;40(1):1–4. doi: 10.1097/00005373-199601000-00001. [DOI] [PubMed] [Google Scholar]
- 14.Jayaraman SP, Ayzengart AL, Goetz LH, Ozgediz D, Farmer DL. Global health in general surgery residency: a national survey. J Am Coll Surg. 2009;208(3):426–433. doi: 10.1016/j.jamcollsurg.2008.11.014. [DOI] [PubMed] [Google Scholar]
- 15.Leow JJ, Kingham P, Casey KM, Kushner AL. Global surgery: thoughts on an emerging surgical subspecialty for students and residents. J Surg Ed. 2010;67(3):143–148. doi: 10.1016/j.jsurg.2010.03.002. [DOI] [PubMed] [Google Scholar]
- 16.Aide-memoire for diagnostic imaging services. Geneva: World Health Organization; 2009. Accessed at Available at: 〈 http://whqlibdoc.who.int/aide-memoire/a71903.pdf〉. [Google Scholar]
- 17.Mateer JR, Valley VT, Aiman EJ, Phelan MB, Thoma ME, Kefer MP. Outcome analysis of a protocol including bedside endovascular sonography in patients at risk for ectopic pregnancy. Ann Emerg Med. 1996;27(3):283–289. doi: 10.1016/s0196-0644(96)70260-3. [DOI] [PubMed] [Google Scholar]
- 18.Mahran M, Omran M. The impact of diagnostic ultrasound on the prediction of intrauterine growth retardation in developing countries. Int J Gynaecol Obstet. 1988;26(3):375–378. doi: 10.1016/0020-7292(88)90332-3. [DOI] [PubMed] [Google Scholar]
- 19.Stein W, Katunda I, Butoto C. A two-level ultrasono-graphic service in a maternity care unit of a rural district hospital in Tanzania. Trop Doct. 2008;38(2):125–126. doi: 10.1258/td.2007.070045. [DOI] [PubMed] [Google Scholar]
- 20.World Health Organization. World Health Report 2005: Making Every Mother and Child Count: Statistical Annex. Geneva: World Health Organization; 2005. [Google Scholar]
- 21.Chen L, Hsiao A, Langhan M, Riera A, Santucci KA. Use of bedside ultrasound to assess degree of dehydration in children with gastroenteritis. Acad Emerg Med. 2010;17:1042–1047. doi: 10.1111/j.1553-2712.2010.00873.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Levine AC, Shah SP, Umulisa I, et al. Ultrasound assessment of severe dehydration in children with diarrhea and vomiting. Acad Emerg Med. 2010;17(10):1035–1041. doi: 10.1111/j.1553-2712.2010.00830.x. [DOI] [PubMed] [Google Scholar]
- 23.Kimberly HH, Murray A, Mennicke M, et al. Focused maternal ultrasound by midwives in rural Zambia. Ultrasound Med Biol. 2010;36(8):1267–1272. doi: 10.1016/j.ultrasmedbio.2010.05.017. [DOI] [PubMed] [Google Scholar]
- 24.Shah SP, Epino H, Bukhman G, et al. Impact of the introduction of ultrasound services in a limited resource setting: rural Rwanda 2008. BMC Int Health Hum Rights. 2009;9(9):4. doi: 10.1186/1472-698X-9-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Spencer JK, Adler RS. Utility of portable ultrasound in a community in Ghana. J Ultrasound Med. 2008;27(12):1735–1742. doi: 10.7863/jum.2008.27.12.1735. [DOI] [PubMed] [Google Scholar]
- 26.Kotlyar S, Moore CL. Assessing the utility of ultrasound in Liberia. J Emerg Trauma Shock. 2008;1(1):10–14. doi: 10.4103/0974-2700.41785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Blaivas M, Kuhn W, Reynolds B, Brannam L. Change in differential diagnosis and patient management with the use of portable ultrasound in a remote setting. Wilderness Environ Med. 2005;16(1):38–41. doi: 10.1580/1080-6032(2005)16[38:ciddap]2.0.co;2. [DOI] [PubMed] [Google Scholar]


