Abstract
BACKGROUND:
Airway foreign bodies (AFBs) is an interdisciplinary area between emergency medicine, pediatrics and otolaryngology. It is a life-threatening condition that is not infrequently seen; however, it is poorly covered in medical literature. Accidental aspiration of an element into airways is a widespread clinical scenario among children under 3 years, predominantly males. Moreover, it is the leading cause of infantile deaths and the fourth one among preschool children.
DATA RESOURCES:
A systemic search was conducted in July 2015 using PubMed/PubMed Central Database of The National Center for Biotechnology Information (NCBI) (http://www.ncbi.nlm.nih.gov/). A total of 1 767 articles were identified and most of them were meta-analyses, systematic reviews, and case series. Those thoroughly discussing assessment and management of AFBs were retrieved.
RESULTS:
AFBs episodes may be either witnessed or missed. Presence of a witness for the inhalation is diagnostic. The later usually present with persistent active cough. A classical triad of paroxysmal cough, wheezing, and dyspnoea/decreased air entry was reported, though many presentations have inconsistent findings. Hence, diagnosis requires high index of clinical suspicion. Flexible fibro-optic bronchoscopy is the gold standard of diagnosis, whereas inhaled objects are best retrieved by rigid bronchoscopes.
CONCLUSIONS:
Close supervision of pediatrics is the hallmark of prevention. Caregivers should ensure a safe surrounding milieu, including the toys their offspring play with. Immediate complications result from direct obstruction or injury by the inhaled object. Alternatively, prolonged lodging traps air and induces inflammatory response causing atelectesis and pneumonia, respectively.
KEY WORDS: Airway foreign bodies, Aspiration/inhalation, Airway obstruction, Café coronary syndrome, Breathing difficulties
INTRODUCTION
Accidental impaction of objects in the respiratory tract, known as airway foreign bodies (AFBs), is a potentially life-threatening emergency; however, it is a poorly covered topic in textbooks. The most common site for that is the right lower bronchus or its bronchus intermedius as it is more vertical, shorter and wider.[1]
Historically, Haugen[2] was the first to report a series of deaths in restaurants in 1963. Café coronary is a fatal upper airway obstruction that occurs to adults who spontaneously swallow large pieces of meat while they laugh or chat. Such cases were successfully managed in 1897 using bronchoscopic extraction by the pioneer Gustav Killian.[3]
Figure 1.
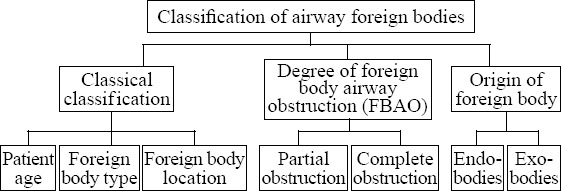
Classification of airway foreign bodies.
Classification
Despite of its importance, no standard classification system for AFBs exists. Rather, there are several items to categorize them, here are the most important three. In classical classification, cases are differentiated according to patient age, foreign body category, and the impaction site.[4] According to the degree of foreign body airway obstruction (FBAO), there are two types, partial and complete obstruction. The former has mild to moderate effects compared to consequences of complete occlusion. Regarding the origin of foreign bodies it is either internal or external. Examples of endogenous sources include mucus masses (mucocoele)[5] and bronchial casts of plastic bronchitis. Exogenous bodies are like industrial items, e.g. plastic bags, small items, etc and food particles as peanuts that are seen in 40% of all cases.[6]
Epidemiology
Thus so far, statistic data are mainly retrieved from single center studies. Larger cohorts and national wide analysis have just started.[7] These studies estimate the incidence of FBAO to be 0.66 per 100 000.[8] In the USA, 17 000 emergency visits in children under 14 years were attributed to foreign bodies inhalation during 2000.[9] Moreover, it is the leading cause of accidental infantile deaths and the fourth one among preschool children (≤5 years).[10]
AFBs have very unique demography. 80% of cases are below 3 years, of which the peak frequency occurs in 1–2 years age group.[11] In a review of 81 cases, Asif et al found that 77.8% of foreign bodies are aspirated by children under 5 years, 16% by children between 5–15 years, and 6.2% by those above 15 years. Similarly, Reilly et al[12] highlighted that ≤4 years pediatrics are more vulnerable to inhale bodies as they are driven by oral exploration behavior using their molar-free mouths and they lack well-coordinated swallowing reflex. The smaller diameter of their airways allows the inhaled body to obstruct the tract.[13] Additionally, Yadav et al[14] and Brkić and Umihanić[15] demonstrated that 46% and 65.2% of their sample were ≤3 years, respectively.
Male sex predominance is another characteristic feature of this condition.[16] Their adventurous and impulsive behavior may justify that.[17] In a study done by Cohen et al,[18] male to female ratio was 1.4:1.0. Kaur et al[19] and Hughes et al[20] found it to be 1.5:1.0 and 1.7:1.0, respectively. Furthermore, Shlizerman et al[21] reported that up to two thirds of their patients were boys. The incidence in Arab children was significantly higher than that in their Jewish peers in Israel (P=0.001). To the best of our knowledge, this is the first study to report racial differences.
The socioeconomic status has a limited impact on the burden of AFBs, rather, it is associated with a high incidence of serious complications seen in high (10%) and low-middle income countries (20%).[22]
Type of inhaled foreign body has global variation. For example, 91% of western patients inhaled organic materials, peanuts account for half of that.[23] However, bones were the most common AFBs in southeast Asia and China.[24,25] Similarly, seeds of watermelons, sunflowers, and pumpkins are more prevalent in Egypt, Turkey, and Greece, respectively.[26]
This is because of differences in food habits that reflect a cultural impact. Moreover, religion and associated habits have some role to play. Ragab et al[27] reported 20 Muslim females who accidently aspired scarf pins held between their lips while wearing Hijab. Obviously, treating pins orally, rather than Hijab itself, was the why.
Etiology
Causes vary greatly depending on age. While children tend to explore their surroundings, they may engulf some inappropriate objects. For instance, toys, coins, etc should not be treated by mouth. Some types of food require higher level of skills to deal with which makes it age-restricted, i.e. peanuts for preschool children who lack the necessary skills of mastication.
Children are chocked by food while moving or talking relatively resembles the scenario of café coronary in adults. Pediatrics are known for their physical activity, this may disrupt their concentration and increase both respiratory rate and depth leading the food into the respiratory passages.
Finally, AFBs may occur because of misdirecting of solid food or liquid fluids into the airways rather than the gastrointestinal tract during the second stage of deglutition, the pharyngeal stage.[28] Alternatively, an endogenous source may obstruct airways as seen in case of mucoid impaction or bronchial casts formation characterizing plastic bronchitis.[29] The exact pathophysiological mechanism is unknown, but it is commonly seen in chronic asthmatics, adults with cardiac and pericardial diseases, and children with congenital heart deformities.[30]
Pathophysiology
Nature of the foreign body determines the degree of inflammatory response. Metallic objects cause minimal reaction, while lipophilic materials stimulate intense chemo-inflammation in a response to its fatty acid content.[31] Starchy food adsorbs water, turning partial obstruction into complete one.[32]
Clinical features
Onset of symptoms is predominantly sudden. These presenting complaints depend widely on the location where the body lodged. Nasal objects tend to cause unilateral, offensive, and chronic discharge that is usually unexplained.[33] Rarely, cases of halitosis, chronic sinusitis and recurrent epistaxis have been reported.[34–37]
Inhaled foreign objects induce prompt gagging, chocking, and distress as they pass down through the vocal cords and epiglottis.[33] Tracheal bodies have this clinical triad: asthmatoid wheeze, audible slap from the rubbed trachea, and palpable thud.[38] Penetration syndrome, i.e. chocking and intractable coughing followed by vomiting characterizes endobronchial bodies.[30]
Clinical features vary according to the wide range of symptoms. The suggested clinical triad of paroxysmal cough, wheezing and decreased air entry was seen in 35% and 39% of patients reported by Mehta et al[39] and Denny et al[40], respectively. Furthermore, Pinzoni et al[41] demonstrated that cough and dyspnoea were the most presenting complaints. Likewise, the most frequent symptomatic triad according to Chiu et al[17] was cough (72%), dyspnoea (64%) and wheezing (60%). The former acts as a protective reflex that keeps the inhaled body from advancing further.
In a study by Pinto et al[42], a higher proportion of patients complained of cough (87.1%), whereas choking, fever and cyanosis were seen in 85.1%, 22.6% and 16.1%, respectively. According to Chew and Tan,[43] the former two constituted 61.5% and 46.2%, respectively. They noted that, choking is usually missed or downplayed by parents as a principal complaint. Despite its low incidence, interestingly, choking showed a sensitivity of 81% and a specificity of 33%, when compared with persistent coughing (a sensitivity of 78% and a specificity of 37%).[44] Even though, another study found choking values to be as high as 97% for the sensitivity and 63% for the specificity.[45] Occasionally, AFBs precipitate anxiety and ptyalism as a result of sympathetic stimulation and psychoactive drive.[46]
Notably, physical examination of symptomatic patients has a sensitivity of 90%.[47] Clinical findings include raspy respiration, hypopnea, and dyspnea,[48] accordingly, hypoxia, hypercapnia, and cyanosis develop. Additionally, ipsilateral wheezes may be appreciated on auscultation. Sonorous rhonchi, a special high pitched wheeze, indicates aspiration of a large foreign body.[49] Interestingly, AFBs have a unique type of stridor that is expiratory and it indicates a lower tract obstruction.[50]
Differential diagnoses
A long list of differentials should be considered. These diseases could be categorized according to the site of obstruction. Laryngeal bodies partially resemble subglottic laryngitis and epiglottitis.[51] Presentations of foreign bodies lodging in the trachea mimic that of croup, tracheal and paratracheal compressing mass lesions, tracheomalacia, and tracheal stenosis. Bronchial obstructing bodies resemble congenital cystic adenomatoid malformation (CCAM), bronchial compression, and plastic bronchitis, also known as fibrinous, pseudomembranous, Hoffman’s, or cast bronchitis.[52] Bronchioles obstructing diseases as bronchiolitis, bronchiectasis, bronchiolitis obliterans, and bronchiolitis obliterans with organizing pneumonia (BOOP) should be considered. Lobar obstruction may be overseen as asthma and atelectasis.
Diagnosis
Diagnosis of AFBs is a real dilemma. Recently, Heyer et al[53] developed diagnostic criteria. Two out of the following three are considered diagnostic and recommend bronchoscopy for confirmation: foal hyperinflation (β=45.4; 95%CI 5.3–390.5, P=0.001), witnessed chocking crisis (β=18.6; 95%CI 4.7–73.0, P=0.001), leukocytosis>10 000 (β=4.2; 95%CI 1.2–14.7, P=0.026).
Another diagnostic tool is the scoring system created by Kadmonet et al.[54] Significant parameters are: age (10–24 months); history of presence of an object in patient’s mouth followed by severe respiratory symptoms; signs of stridor, dyspnea or hypoxia during acute phase; unilateral abnormal breathing sounds on auscultation; abnormal tracheal radiogram; and positive chest X-ray (CXR).
Only 16% of AFBs are spot diagnosed on CXR as they are radiopaque.[55] Accordingly, a negative film does not exclude aspiration, rather, it may contain one of the signs detected in 72% of the cases.[56] This ratio was 67.7% in the study conducted by Svedstrom et al.[57] Such radiological findings include unilateral atelectasis, local hyperinflation or obstructive emphysema. Usually, inspiratory-expiratory film in anterior-posterior (AP) view is likely to reveal the overinflation as a hyperlucency best during expiration.[58] Although, lateral decubitus is routinely obtained, a recent study has demonstrated its limited role in diagnosis with only a sensitivity of 27% and a specificity of 67% (95%CI 0.1–5.2; P=0.57).[59] Virk et al[60] recommended addition of lateral soft tissue neck X-ray in case of laryngeal bodies.
Chest fluoroscopy is valuable in detecting mediastinal shift and paradoxical diaphragmatic respiration; however, its false negative rate of 53% is considerably high.[61] Although, the diagnostic yield of CT scan is superior to that of CXR particularly for radiolucent bodies (a sensitivity of 100% and a specificity of 66.7%),[62,63] it is the last resolve as it contradicts the contemporary approach for minimizing ionizing irradiation exposure. High quality scans require movement restriction, which makes it impractical choice for AFBs pediatric patients under respiratory distress. Hence, flexible fibro-optic bronchoscopy remains the gold standard for diagnosis. Baseline investigations, as complete blood count (CBC) and serum electrolytes, are useful in assessing patient’s general condition. Pulse oximetry and arterial blood gases are of help in determining arterial blood oxygen saturation (SaO2).
The key to reach a definitive diagnosis lies in a detailed history that identifies risk factors, an examination that elicits important signs, and supportive CXR findings. Diagnostic bronchoscopy should be performed when any one of the above modalities is positive. Otherwise, both examination and radiography should be repeated 24 hours apart given a negative history and inconclusive initial examination and imaging in a stable patient.[64]
Management
The management plan depends on many factors that include the general condition of the patient, clinical settings, and policy guidelines of the health facility. American Academy of Pediatrics recommendations offer a comprehensive approach to improve anticipatory measures.[65] Caregivers must know the best ways of supervising their kids in a safe milieu. However, when precautions fail and aspiration is suspected or witnessed, parents should call 911 (ambulance service) asking for help. Meanwhile, basic life support manoeuvres should be started. Both European Resuscitation Council and American Heart Association guidelines are combined in Figure 2.[66,67]
Figure 2.
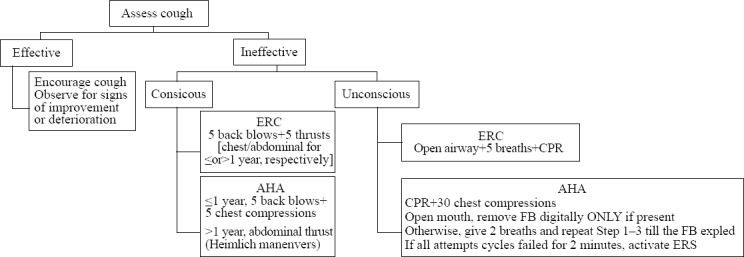
AFB emergency algorithm following ERC and AHA guidelines. ERC: European Resuscitation Council; AHA: American Heart Association; FB: foreign bodies; CPR: cardiopulmonary resuscitation; ERS: emergency response system.
In hospital, while the above measures are checked, emergency bronchoscopy should be prepared. Flexible bronchoscope is used primarily for diagnosis. However, new studies defined a new role for them in treatment, particularly, when combined with ureteral stone baskets and forceps.[68] When done by expertise hands, objects are retrieved in more than 90% of cases.[69,70] Both Ramírez-Figueroa et al[71] and Tang et al[72] found this to be 91.3% in their two separate studies.
Rigid bronchoscopy is the modality of choice in extracting AFBs. It offers adequate visualization making them overweigh flexible ones by being dual-purpose, diagnosis and management. Moreover, it is specially-designed to enable anesthetists of administering oxygen and inhalational agents through the side arms. Additionally, it can be used with a wide range of instruments, like Roth nets and endoscopic baskets, to achieve better outcome.[73] Its success rates range from 95% to 99%.[74–76] Solanki et al[77] suggested use of Heimlich’s maneuver in tandem with bronchoscopy when it fails. Invasive operations such as tracheostomy, thoracotomy and bronchostomy are the options for the remaining 0.3%–4%.[78–79]
Type of anesthesia is another issue of controversy. There is a wide consensus on using sevoflurane or halothane as inhalational agents for induction of anesthesia and spontaneous breathing as a maintenance technique of choice.[80] This is usually done by connecting Ayre’s T-piece (Mapleson F) to bronchoscope’s sidearm. Alternatively, a single trial found positive pressure ventilation after paralysing the patient to be superior since fewer episodes of coughing and desaturation were reported.[81]
Postoperative hospitalization depends on clinical situation. According to Hidaka et al,[82] the nature of inhaled body was the only predictor of recovery and subsequently hospital stay. For instance, patients who underwent bronchoscopic extraction of peanuts or animal materials were hospitalized longer than others (OR 5.80; 95%CI 1.12–30.43). In contrast, age, sex, and length of duration precedes intervention have no association.
Complications
Williams et al[83] classified complications into minor complications such as arterial oxygen desaturation, bradycardia, and bronchospasm. Major consequences include laryngeal edema, pneumothorax, and cardiac arrests. Early diagnosis and adequate management are essential in preventing progression into serious consequences.[84] Sharp objects cause serious injuries and subsequently hemoptysis. Prolonged airways obstruction precipitates hypoxia and hypercapnia. Recurrent irritation of alveolar epithelium develops edema that may be superadded by secondary bacterial infection. Longstanding inflammation leads to abscess formation, recurrent pneumonia, bronchiectasis, and bronchial strictures. Bronchial granulomas commonly surround vegetable matters and can be distinguished microscopically by presence of foreign body giant cells.[85]
Reports on frequencies of complications and mortalities are of great variety. This may be a result of their frequent underestimation in many studies.[86] Inflammatory responses, localized edema, and bronchospasm are the most common consequences for AFBs. The 59.4% of patients reported by de Sousa et al[87] had localized inflammations, whereas laryngeal edema and pneumonia were seen in 18.9%. The mortality rate was zero. A recent study found that pneumonia (32.2%), granuloma (26.9%) and mucosal erosion (16.11%) were the most common complications.[88]
Kaur et al[89] reported that 10% of subjects developed complications predominantly as bronchospasm (8%) and subglottic edema (2%). They reported a death rate of 2% which was higher than that (0.42%) reported by Fidowski et al.[90] Other complications have been shown in a huge meta-analysis of 1 699 papers.[91] Among the complications reported in 15% of patients, laryngeal edema (9.3%), cardiac arrest (2.1%), and pneumothorax (0.7%) were the most serious. Rarely reported complications include brain abscess[92,93] and pulmonary botryomycosis.[94]
In conclusion, global population explosion and pacing lifestyle strongly favour AFBs. Careful supervision of children is the root reason of preventing inhalation. However, when precautions fail, a prompt intervention will minimize long-term complications. AFBs should be considered as a differential in any young child with unexplained cough.
ACKNOWLEDGEMENTS
The authors thank Dr. Khalid M. A\Allah, Pediatrics Sr. Consultant, Pediatric Emergency Centre, HMC, Qatar for his endless scientific and editorial contributions. They would also like to thank Dr. Mohammed B. Al-Nayer, Paediatrics Sr. Specialist, Pediatric Emergency Centre, HMC, Qatar for their guidance and support throughout the preparation of this article. Their continuous enthusiasm and encouragement are greatly appreciated.
Footnotes
Funding: None.
Ethical approval: Not needed.
Conflicts of interest: The authors declare that they have no competing interests.
Contributors: Salih AM proposed the study and wrote the first draft. All authors read and approved the final manuscript.
REFERENCES
- 1.Limper AH, Prakash UB. Tracheobronchial foreign bodies in adults. Ann Intern Med. 1990;112:604–609. doi: 10.7326/0003-4819-112-8-604. [DOI] [PubMed] [Google Scholar]
- 2.Haugen RK. The cafécoronary: sudden deaths in restaurants. JAMA. 1963;186:142–143. doi: 10.1001/jama.1963.63710020011017. [DOI] [PubMed] [Google Scholar]
- 3.Fleischer K. Erkennung und Entfernung Von. Bronchial-frem-dkorpern-einstJetzt. TherGgegenw. 1974;113:348–358. [PubMed] [Google Scholar]
- 4.Robinson CLN, Mushin WW. Inhaled foreign bodies. Br Med J. 1956;2:324–328. doi: 10.1136/bmj.2.4988.324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.El-Munshid HA. Gastrointestinal Physiology. In: Sukkar MY, El-Munshid HA, Ardawi MSM, editors. Concise Human Physiology. 2nd Ed. Oxford: Blackwell; 2000. p. 159. [Google Scholar]
- 6.Park JY, Elshami AA, Kang DS, Jung TH. Plastic bronchitis. Eur Respir J. 1996;9:612–614. doi: 10.1183/09031936.96.09030612. [DOI] [PubMed] [Google Scholar]
- 7.Passàli D, Lauriello M, Bellussi L, Passali GC, Passali FM, Gregori D. Foreign body inhalation in children: an update. Acta Otorhinolaryngol Ital. 2010;30:27–32. [PMC free article] [PubMed] [Google Scholar]
- 8.Hughes CA, Baroody FM, Marsh BR. Pediatric tracheobronchial foreign bodies: Historical review from the Johns Hopkins Hospital. Ann Otol Rhinol Laryngol. 1996;105:555–561. doi: 10.1177/000348949610500712. [DOI] [PubMed] [Google Scholar]
- 9.Centres for Disease Control and Prevention (CDC) Nonfatal choking-related episodes among children-United States, 2001. MMWR Morb Mortal Wkly Rep. 2002;51:945. [PubMed] [Google Scholar]
- 10.Doody DP. Foreign body aspiration. In: Grillo HC, editor. Surgery of the Trachea and Bronchi. 1st Ed. Ontario: BC Decker Inc; 2004. pp. 707–718. [Google Scholar]
- 11.Ciftci AO, Bingöl-Koloğlu M, Senocak ME, Tanyel FC, Büyükpamukçu N. Bronchoscopy for evaluation of foreign body aspiration in children. J Pediatr Surg. 38:1170–1176. doi: 10.1016/s0022-3468(03)00263-x. [DOI] [PubMed] [Google Scholar]
- 12.Reilly JS, Cook SP, Stool D, Rider G. Prevention and management of aerodigestive foreign body injuries in childhood. Pediatr Clin North Am. 1996;43:1403–1411. doi: 10.1016/s0031-3955(05)70525-3. [DOI] [PubMed] [Google Scholar]
- 13.Smith GA, Gardner HG, Baum CR, Dowd MD, Durbin DR, Lichenstein R, et al. Prevention of chocking among children. Pediatrics. 2010;125:601–607. [Google Scholar]
- 14.Yadav SP, Singh J, Aggarwal N, Goel A. Airway foreign bodies in children: experience of 132 cases. Singapo Med J. 2007;48:850–853. [PubMed] [Google Scholar]
- 15.Brkić F, Umihanić S. Tracheobronchial foreign bodies in children. Experience at ORL clinic Tuzla, 1954-2004. Int J Pediatr Otorhinolaryngol. 2007;71:909–915. doi: 10.1016/j.ijporl.2007.02.019. [DOI] [PubMed] [Google Scholar]
- 16.Shivakumar AM, Naik AS, Prashanth KB, Shetty KD, Praveen DS. Tracheobronchial foreign bodies. Indian J Pediatr. 2003;70:793–797. doi: 10.1007/BF02723797. [DOI] [PubMed] [Google Scholar]
- 17.Chiu CY, Wong KS, Lai SH, Hsia SH, Wu CT. Factors predicting early diagnosis of foreign body aspiration in children. Pediatr Emerg Care. 2005;21:161–164. [PubMed] [Google Scholar]
- 18.Cohen SR, Herbert WI, Lewis GB, Jr, Geller KA. Foreign bodies in the airway - 6 year retrospective study with special reference to management. Ann Otol Rhinol Laryngol. 1980;89:437–442. doi: 10.1177/000348948008900513. [DOI] [PubMed] [Google Scholar]
- 19.Kaur K, Sonkhya N, Bapna AS. Foreign bodies in the tracheobronchial tree: a prospective study of fifty cases. Indi J Otolaryngol Head Nec Surg. 2002;54:30–34. doi: 10.1007/BF02911002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hughes C, Anthony E. Paediatric tracheobronchial foreign bodies - historical review from the John Hopkins Hospital. Ann Otol Rhinol Laryngol. 1996;105:555–561. doi: 10.1177/000348949610500712. [DOI] [PubMed] [Google Scholar]
- 21.Shlizerman L, Ashkenazi D, Mazzawi S, Harefuah RY. Foreign body aspiration in children: ten-years experience at the Ha’Emek Medical Center. Harefuah. 2006;145:569–571. 631. [PubMed] [Google Scholar]
- 22.Foltran F, Ballali S, Rodriguez H, Bvan A, Desiderio A, Desiderio P, et al. Inhaled foreign bodies in children: a global perspective on their epidemiological, clinical, and preventive aspects. Pediatr Pulmonol. 2013;48:344–351. doi: 10.1002/ppul.22701. [DOI] [PubMed] [Google Scholar]
- 23.Baharloo F, Veyckemans F, Francis C, Biettlot MP, Rodenstein DO. Tracheobronchial foreign bodies: presentation and management in children and adults. Chest. 1999;115:1357–1362. doi: 10.1378/chest.115.5.1357. [DOI] [PubMed] [Google Scholar]
- 24.Lan RS. Non asphyxiating tracheobronchial foreign bodies in adults. Eur Respir J. 1994;7:510–514. doi: 10.1183/09031936.94.07030510. [DOI] [PubMed] [Google Scholar]
- 25.Patel S, Kazeroonl EA. Case 31: foreign body aspiration-chicken vertebra. Radiol. 2001;218:523–525. doi: 10.1148/radiology.218.2.r01fe49523. [DOI] [PubMed] [Google Scholar]
- 26.Vijayasekaran D, Sambandam AP, Gowrishankar NC. Acute plastic bronchitis. Indian Paediatr. 2004 Dec 17;41:1257–1259. [PubMed] [Google Scholar]
- 27.Ragab A, Ebied OM, Zalat S. Scarf pins sharp metallic tracheobronchial foreign bodies: presentation and management. Int J Pediatr Otorhinolaryngol. 2007;71:769–773. doi: 10.1016/j.ijporl.2007.01.018. [DOI] [PubMed] [Google Scholar]
- 28.Review of inhaled foregin body. Amsterdam: Elsevier Inc; 2007. Aug 24, Available from: http://www.mdconsult.com/ [Google Scholar]
- 29.Alfageme I, Reyes N, Merino M. Aspirated foreign body. Int J Pulmon Med. 2007;7:5–6. [Google Scholar]
- 30.Webb WA. Management of foreign bodies of the upper gastrointestinal tract. Gastrointest Endosc. 1995;41:39–51. doi: 10.1016/s0016-5107(95)70274-1. [DOI] [PubMed] [Google Scholar]
- 31.Ganong WF. Review of Medical Physiology. 22th Ed. London: McGraw-Hill; 2005. p. 678. [Google Scholar]
- 32.Inhaled foregin body. Florida: DSHI Systems Inc; 2009. Apr 27, Available from: http://www.freemd.com/ [Google Scholar]
- 33.Poirier M. Foreign bodies of the respiratory tract. Intern J Emerg Med. 2003;2:1–12. [Google Scholar]
- 34.Brownstein D, Hodge D. Foreign bodies of the eye, ear, and nose. Pediatr Emerg Care. 1988;4:215–218. doi: 10.1097/00006565-198809000-00016. [DOI] [PubMed] [Google Scholar]
- 35.Baker M. Foreign bodies of the ears and nose in childhood. Pediatr Emerg Care. 1987;3:67–70. doi: 10.1097/00006565-198706000-00001. [DOI] [PubMed] [Google Scholar]
- 36.Bennett J. An unexplained cause of halitosis. J R Army Med Corps. 1988;134:151–152. doi: 10.1136/jramc-134-03-10. [DOI] [PubMed] [Google Scholar]
- 37.Fireman P. Diagnosis of sinusitis in children: emphasis on the history and physical examination. J A Clin Immunol. 1992;90:433–436. doi: 10.1016/0091-6749(92)90164-w. [DOI] [PubMed] [Google Scholar]
- 38.Jackson C, Jackson CL. Diseases of the Air and Food Passages of Foreign Body Origin. 1st Ed. Philadelphia, PA: Elsevier Saunders; 1936. [Google Scholar]
- 39.Mehta S, Mehta N, Suri M, Khajura R. Guidelines for removal of foreign bodies in pediatric airway. JK Practiti. 2006;13:18–22. [Google Scholar]
- 40.Denny MK, Berkas EM, Snider TH. Foreign body bronchiectasis. Dis Chest. 1968;53:613–616. doi: 10.1378/chest.53.5.613. [DOI] [PubMed] [Google Scholar]
- 41.Pinzoni F, Boniotti C, Molinaro SM, Baraldi A, Berlucchi M. Inhaled foreign bodies in pediatric patients: review of personal experience. Int J Pediatr Otorhinolaryngol. 2007;71:1897–1903. doi: 10.1016/j.ijporl.2007.09.002. [DOI] [PubMed] [Google Scholar]
- 42.Pinto A, Scaglione M, Pinto F, Guidi G, Pepe M, Del Prato B, Grassi R, et al. Tracheobronchial aspiration of foreign bodies: current indications for emergency plain chest radiography. Radiol Med. 2006;111:497–506. doi: 10.1007/s11547-006-0045-0. [DOI] [PubMed] [Google Scholar]
- 43.Chew HS, Kiaang Tan HK. Airway foreign body in children. Int J Clin Med. 2012;3:655–660. [Google Scholar]
- 44.Hoeve LJ, Rombout J, Pot DJ. Foreign body aspiration in children. The diagnostic value of signs, symptoms and preoperative examination. Clin Otolaryngol. 1993;18:55–57. doi: 10.1111/j.1365-2273.1993.tb00810.x. [DOI] [PubMed] [Google Scholar]
- 45.Fontoba JEB, Gutierrez C, Lluna J, Vila JJ, Poquet J, Ruiz-Company S. Bronchial foreign body: should bronchoscopy be performed in all patients with a chocking crisis? Pediatr Surg Int. 1997;12:118–120. doi: 10.1007/s003830050080. [DOI] [PubMed] [Google Scholar]
- 46.Merghani TH. The core of medical physiology. 1st Ed. Khartoum: Khartoum University Printing Press; 2008. [Google Scholar]
- 47.Agarwal RK, Banerjee G, Shembish N, Jamal B, Kareemullah C, Swaleh ABV. Foreign bodies in the tracheobronchial tree: a review of 102 cases in Benghazi, Libya. Ann Trop Pediatr. 1988;8:213–216. doi: 10.1080/02724936.1988.11748573. [DOI] [PubMed] [Google Scholar]
- 48.Singh B, Kantu M, Har-El G, Lucente FE. Complications associated with 327 foregin bodies of the pharynx, larynx, & esophagus. Ann Otol Rhinol Laryngol. 1997;106:301–304. doi: 10.1177/000348949710600407. [DOI] [PubMed] [Google Scholar]
- 49.Sapira JD, Orient JM. Sapira’s art & science of bedside diagnosis. Hagerstwon: Lippincott Williams & Wilkins; 2000. [Google Scholar]
- 50.Zerellaab JT, Dimlerab M, McGillab LC, Pippus KJ. Foreign body aspiration in children: Value of radiography and complications of bronchoscopy. J Pediatr Surg. 1998;33:1651–1654. doi: 10.1016/s0022-3468(98)90601-7. [DOI] [PubMed] [Google Scholar]
- 51.Ginsberg GG. Management of ingested foreign objects & food bolus impactions. Gastrointest Endosc. 1995;41:33–38. doi: 10.1016/s0016-5107(95)70273-3. [DOI] [PubMed] [Google Scholar]
- 52.Hoeve LJ, Rombout J, Pot DJ. Foreign body aspiration in children: The diagnostic value of signs, symptoms and pre-operative examination. Clin Otolaryngo & Allie Scien. 1993;18:55–57. doi: 10.1111/j.1365-2273.1993.tb00810.x. [DOI] [PubMed] [Google Scholar]
- 53.Heyer CM, Bollmeier ME, Rossler L, Nuesslein TG, Stephan V, Bauer TT, et al. Evaluation of clinical, radiologic, and laboratory prebronchoscopy findings in children with suspected foreign body aspiration. J Pediatr Surg. 2006;41:1882–1888. doi: 10.1016/j.jpedsurg.2006.06.016. [DOI] [PubMed] [Google Scholar]
- 54.Kadmon G, Stern Y, Bron-Harlev E, Nahum E, Battat E, Schonfeld T. Computerized scoring system for the diagnosis of foreign body aspiration in children. Ann Otol Rhinol Laryngol. 2008;117:839–843. doi: 10.1177/000348940811701108. [DOI] [PubMed] [Google Scholar]
- 55.Cantaneo AJ, Reibscheid SM, Ruiz RL, Junior, Ferrari GF. Foreign body in the tracheobronchial tree. Clin Pediatr. 1997;36:701–706. doi: 10.1177/000992289703601206. [DOI] [PubMed] [Google Scholar]
- 56.Loo CM, Hsu AAL, Eng P, Ong YY. Case series of bronchoscopic removal of tracheobronchial foreign body in six adults. Ann Acad Med Singapore. 1998;27:849–853. [PubMed] [Google Scholar]
- 57.Svedstrom E, Puhakka H, Kero P. How accurate is chest radiography in the diagnosis of tracheobronchial foreign bodies in children? Pediatr Radiol. 1989;19:521–522. doi: 10.1007/BF02389562. [DOI] [PubMed] [Google Scholar]
- 58.Griffiths DM, Freeman NV. Expiratory chest X-ray examination in the diagnosis of inhaled foreign bodies. Br Med J. 1984;288:1074–1075. doi: 10.1136/bmj.288.6423.1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Assefa D, Amin N, Stringel G, Dozor AJ. Use of Decubitus radiographs in the diagnosis of foreign body aspiration in young children. Pediatr Emerg Care Mar. 2007;23:154–157. doi: 10.1097/PEC.0b013e3180328cd8. [DOI] [PubMed] [Google Scholar]
- 60.Virk J, Pang J, Okhovat S, Lingam R, Singh A. Analysis lateral soft tissue neck radiographs. Emerg Radiol. 2012;19:255–260. doi: 10.1007/s10140-012-1026-3. [DOI] [PubMed] [Google Scholar]
- 61.Even L, Heno N, Talmon Y, Samet E, Zonis Z, Kugelman A. Diagnostic evaluation of foreign body aspiration in children: a prospective study. J Pediatr Surg. 2005;40:1122–1127. doi: 10.1016/j.jpedsurg.2005.03.049. [DOI] [PubMed] [Google Scholar]
- 62.Hong SJ, Goo HW, Roh JL. Utility of Spiral and cine CT scans in pediatric patients suspected of aspirating radiolucent foreign bodies. Otolaryngol Head Neck Surg. 2008;138:576–580. doi: 10.1016/j.otohns.2007.12.039. [DOI] [PubMed] [Google Scholar]
- 63.Donnellyl F, Frush DP, Risset GS. The multiple presentations of foreign bodies in children. Am J Roentgenol. 1998;170:471–477. doi: 10.2214/ajr.170.2.9456967. [DOI] [PubMed] [Google Scholar]
- 64.Tokar B, Ozkan R, Ilhan H. Tracheobronchial foreign bodies in children: importance of accurate history and plain chest radiography in delayed presentation. Clin Radiol. 2004;59:609–615. doi: 10.1016/j.crad.2004.01.006. [DOI] [PubMed] [Google Scholar]
- 65.Hagan JF, Shaw JS, Duncan PM. Bright Future: Guidelines for Health Supervision of Infants, Children, and Adolescents. 3rd Ed. Elk Grove Village, IL: American Academy of Pediatrics; 2008. [Google Scholar]
- 66.Biarent D, Bingham R, Eich C, López-Herce J, Maconochie I, Rodríguez-Núñez A, et al. European Resuscitation Council Guidelines for Resuscitation 2010: Section 6, Paediatric life support. Resuscita. 2010;31:1364–88. doi: 10.1016/j.resuscitation.2010.08.012. [DOI] [PubMed] [Google Scholar]
- 67.Berg MD, Schexnayder SM, Chameides L, Terry M, Donoghue A, Hickey RW, et al. Part 13: Pediatric Basic Life Support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122:S862–S875. doi: 10.1161/CIRCULATIONAHA.110.971085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Swanson KL, Prakash UBS, Midthun DE, Edell ES, Utz JP, McDougall JC, et al. Flexible Bronchoscopic Management of Airway Foreign Bodies in Children. Chest. 2003;121:1695–700. doi: 10.1378/chest.121.5.1695. [DOI] [PubMed] [Google Scholar]
- 69.Swanson KL, Parkash USB, McDougall JC. Airway foreign bodies in adults. J Bronchol. 2003;10:107–111. [Google Scholar]
- 70.Surka A, Chin R, Conforti J. Bronchoscopic myths and legends: airway foreign bodies. Clin Pulm Med. 2006;3:209–211. [Google Scholar]
- 71.Ramírez-Figueroa JL, Gochicoa-Rangel LG, Ramírez-San Juan DH, Vargas MH. Foreign body removal by flexible fiberoptic bronchoscopy in infants and children. Pediatr Pulmonol. 2005;40:392–397. doi: 10.1002/ppul.20242. [DOI] [PubMed] [Google Scholar]
- 72.Tang LF, Xu YC, Wang YS, Wang CF, Zhu GH, Bao XE, et al. Airway foreign body removal by flexible bronchoscopy: experience with 1027 children during 2000–2008. World J Pediatr. 2009;5:191–195. doi: 10.1007/s12519-009-0036-z. [DOI] [PubMed] [Google Scholar]
- 73.Sepehr A, Albers GC, Armstrong WB. Aspiration of a capsule endoscope and description of a unique retrieval technique. Otolaryngol Head Neck Surg. 2007;137:965–966. doi: 10.1016/j.otohns.2007.09.011. [DOI] [PubMed] [Google Scholar]
- 74.Steen KH, Zimmermann T. Tracheobronchial aspiration of foreign bodies in children: a study of 94 cases. Laryngoscop. 1990;100:925–930. doi: 10.1288/00005537-199005000-00016. [DOI] [PubMed] [Google Scholar]
- 75.Elhassani NB. Tracheobronchial foreign bodies in the Middle East: A Baghdad study. J Thorac Cardiovasc Surg. 1988;96:621–625. [PubMed] [Google Scholar]
- 76.Hsu Wc, Sheen Ts, Lin Cd, Tan Ct, Yeh Th, Lee Sy. Clinical experiences of removing foreign bodies in the airway and esophagus with a rigid endoscope: a seies of 3217 cases from 1970 to 1996. Otolaryngol Head Neck Surg. 2000;122:450–454. doi: 10.1016/S0194-5998(00)70063-5. [DOI] [PubMed] [Google Scholar]
- 77.Solanki SL, Bansal S, Khare A, Jain A. Heimlich’s maneuver-assisted bronchoscopic removal of airway foreign body. Anesth Essays Res. 2011;5:201–203. doi: 10.4103/0259-1162.94779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ulku R, Onen A, Onat S, Ozcelik C. The value of surgical approaches for aspirated pen caps. J Pediatr Surg. 2005;40:1780–1783. doi: 10.1016/j.jpedsurg.2005.07.028. [DOI] [PubMed] [Google Scholar]
- 79.Zhijun C, Fugao Z, Niankai Z, Jingjing C. Therapeutic experience from 1420 patients with pediatric tracheobronchial foreign body. J Pediatr Surg. 2008;43:718–721. doi: 10.1016/j.jpedsurg.2007.10.010. [DOI] [PubMed] [Google Scholar]
- 80.Weir PM. Foreign body aspiration. In: Stoddart PA, Lauder GR, editors. Problems in Anaesthesia: Paediatric Anaesthesia. 1st Ed. London: Taylor & Francis Books Ltd; 2004. pp. 163–166. [Google Scholar]
- 81.Soodan A, Pawar D, Subramanium R. Anaesthesia for removal of inhaled foreign bodies in children. Pediatr Anaesth. 2004;14:947–952. doi: 10.1111/j.1460-9592.2004.01309.x. [DOI] [PubMed] [Google Scholar]
- 82.Hidaka H, Obara T, Kuriyama S, Kurosawa S, Katori Y, Kobayashi T. Logistic regression analysis of risk factors for prolonged pulmonary recovery in children from aspirated foreign body. Int J Pediat Otorhinolaryngol. 2013;77:1677–1682. doi: 10.1016/j.ijporl.2013.07.024. [DOI] [PubMed] [Google Scholar]
- 83.Williams A, George C, Atul PS, Sam S, Shukla S. An audit of morbidity and mortality associated with foreign body aspiration in children from a tertiary level hospital in Northern India. Afr J Paediatr Surg. 2014;11:287–292. doi: 10.4103/0189-6725.143129. [DOI] [PubMed] [Google Scholar]
- 84.Foreign body aspiration-Diagnosis-Best Practice [homepage on the Internet] London: BMJ Publishing Group; 2010. Available from: http://www.bestpractice.bmj.com/ [Google Scholar]
- 85.MacSween RNM, Whaley K. Muir’s Textbook of Pathology. 13th Ed. London: Arnold; 1992. [Google Scholar]
- 86.Oliveira CF, Almeida JFL, Troster EJ, Costa Vaz FA. Complications of tracheobronchial foreign body aspiration in children: report of 5 cases and review of the literature. Rev Hosp Clin. 2002;57:108–111. doi: 10.1590/s0041-87812002000300005. [DOI] [PubMed] [Google Scholar]
- 87.de Sousa ST, Ribeiro VS, de Menezes Filho JM, dos Santos AM, Barbieri MA, de Figueiredo Neto JA. Foreign body aspiration in children and adolescents: experience of a Brazilian referral center. J Bras Pneumol. 2009;35:653–659. doi: 10.1590/s1806-37132009000700006. [DOI] [PubMed] [Google Scholar]
- 88.Rodríguez H, Cuestas G, Botto H, Nieto M, Cocciaglia A, Passali D, et al. Complications in children from foreign bodies in the airway. Acta Otorrinolaringol Esp. 2015 Apr 6; doi: 10.1016/j.otorri.2015.01.003. pii: S0001-6519(15)00031-X. doi: 10.1016/j.otorri.2015.01.003. [DOI] [PubMed] [Google Scholar]
- 89.Kaur K, Sonkhya N, Bapna AS. Foreign bodies in the tracheobronchial tree: A prospective study of fifty cases. Indian J Otolaryngol Head Neck Surg. 2002;54:30–34. doi: 10.1007/BF02911002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Fidkowski CW, Zheng H, Firth PG. The anesthetic considerations of tracheobronchial foreign bodies in children: A literature review of 12 979 cases. Anesth Analg. 2010;111:1016–1025. doi: 10.1213/ANE.0b013e3181ef3e9c. [DOI] [PubMed] [Google Scholar]
- 91.Foltran F, Ballali S, Passali FM, Kern E, Morra B, Passali GC, et al. Foreign bodies in the airways: A meta-analysis of published papers. Int J Pediatr Otorhinolaryngol. 2012;76S:S12–S19. doi: 10.1016/j.ijporl.2012.02.004. [DOI] [PubMed] [Google Scholar]
- 92.Sane SM, Faerber EN, Belani KK. Respiratory foreign bodies and Eikenella corrodens brain abscess in two children. Pediatr Radiol. 1999;29:327–330. doi: 10.1007/s002470050600. [DOI] [PubMed] [Google Scholar]
- 93.Roberts J, Bartlett AH, Giannoni CM, Valdez TA. Airway foreign bodies and brain abscesses: report of two cases and review of the literature. Int J Pediatr Otorhinolaryngol. 2008;72:265–269. doi: 10.1016/j.ijporl.2007.10.006. [DOI] [PubMed] [Google Scholar]
- 94.Tuggey JM, Hosker HSR, DaCosta P. Primary pulmonary botryomycosis: a late complication of foreign body aspiration. Thorax. 2000;55:1068–1069. doi: 10.1136/thorax.55.12.1068. [DOI] [PMC free article] [PubMed] [Google Scholar]


