Abstract
Increased APP (amyloid precursor protein) processing causes β-amyloid (Aβ) accumulation in autosomal dominant Alzheimer's disease (AD), but it is unclear if it also affects sporadic Aβ accumulation. We tested healthy controls and patients with mild cognitive symptoms (N=331) in the BioFINDER study, using cerebrospinal fluid (CSF) Aβ40 as a surrogate for amyloidogenic APP processing. We find that levels of brain Aβ fibrils (measured by 18F-flutemetamol PET) are independently associated with high CSF Aβ40 (P<0.001) and APOE ɛ4 (P<0.001). The association between CSF Aβ40 and brain Aβ is stronger in APOE ɛ4-negative than in positive people (P=0.0080). The results are similar for CSF Aβ38 and for a combination of CSF Aβ38 and CSF Aβ40. In conclusion, sporadic Aβ accumulation may be partly associated with increased amyloidogenic APP production, especially in APOE ɛ4-negative subjects. The risk for sporadic AD may consequently depend on increased Aβ production, in addition to decreased Aβ clearance.
 Autosomal dominant Alzheimer's disease is thought to be caused by increased amyloidogenic APP processing. Mattson et al. show that association between brain Aβ and cerobrospinal fluid Aβ40 levels is stronger in APOE ɛ4 negative people, suggesting that increased processing may also underlie sporadic disease.
Autosomal dominant Alzheimer's disease is thought to be caused by increased amyloidogenic APP processing. Mattson et al. show that association between brain Aβ and cerobrospinal fluid Aβ40 levels is stronger in APOE ɛ4 negative people, suggesting that increased processing may also underlie sporadic disease.
Brain accumulation of amyloid β (Aβ) is a hallmark of Alzheimer's disease (AD) which may precede dementia by up to two decades1,2,3 and be quantified by cerebrospinal fluid (CSF) biomarkers or positron emission tomography (PET) imaging4,5. Aβ accumulation is thought to be caused by an imbalance of Aβ production and clearance from the brain6. The APOE ɛ4 allele is the main genetic susceptibility factor for late-onset AD and sporadic Aβ pathology7. This is likely because the APOE ɛ4 gene product apoE4 has reduced capacity to clear Aβ peptides from the brain8. However, Aβ accumulation also occurs in the absence of APOE ɛ4 (ref. 7) and ∼40–50% of AD patients lack the APOE ɛ4 allele9. In autosomal dominant forms of AD, Aβ pathology is believed to be caused by increased amyloidogenic processing of APP (amyloid precursor protein), that is, increased Aβ production10 but variations in APP processing have not been thoroughly explored as risk factors in ‘sporadic' AD. Using a large cohort of non-demented subjects, the aim of this study was to test if APOE ɛ4 and biomarker surrogates of amyloidogenic APP processing were independently associated with brain Aβ accumulation. We used CSF levels of Aβ40 to estimate amyloidogenic APP processing. The rationale for this was that Aβ40 is a major Aβ isoforms produced by neurons by concerted β- and γ-secretase cleavages of APP (the same processing pathway that results in Aβ42)11 but is generally not related to Aβ plaque pathology (in contrast to CSF Aβ42, which is reduced in the presence of Aβ plaques12). Note that previous studies testing the correlation between CSF Aβ40 and PET Aβ have not co-varied for the presence of APOE ɛ4. We hypothesized that there would be independent correlations between Aβ accumulation and the predictors APOE ɛ4 and CSF Aβ40, and that increased amyloidogenic APP processing would be related to Aβ accumulation mainly in APOE ɛ4-negative subjects. We also hypothesized that CSF Aβ40 would not be associated with APOE ɛ4 (that is, CSF Aβ40 would not be affected by apoE4-mediated impaired Aβ clearance). Finally, we hypothesized to see similar results when using CSF Aβ38 instead of CSF Aβ40 to estimate amyloidogenic APP processing.
Our results confirmed our hypothesis. We show that 18F-flutemetamol PET levels are independently associated with high CSF Aβ40 (P<0.001) and APOE ɛ4 (P<0.001) and that the association between CSF Aβ40 and brain Aβ is stronger in APOE ɛ4-negative than in positive people (P=0.0080). The results are similar when using CSF Aβ38 or a combination of CSF Aβ38 and CSF Aβ40 to estimate amyloidogenic APP production. We conclude that sporadic Aβ accumulation may be partly associated with increased amyloidogenic APP production, especially in APOE ɛ4-negative subjects. Thus, the risk for sporadic AD may partly depend on increased Aβ production, in addition to decreased Aβ clearance.
Results
Cohort characteristics
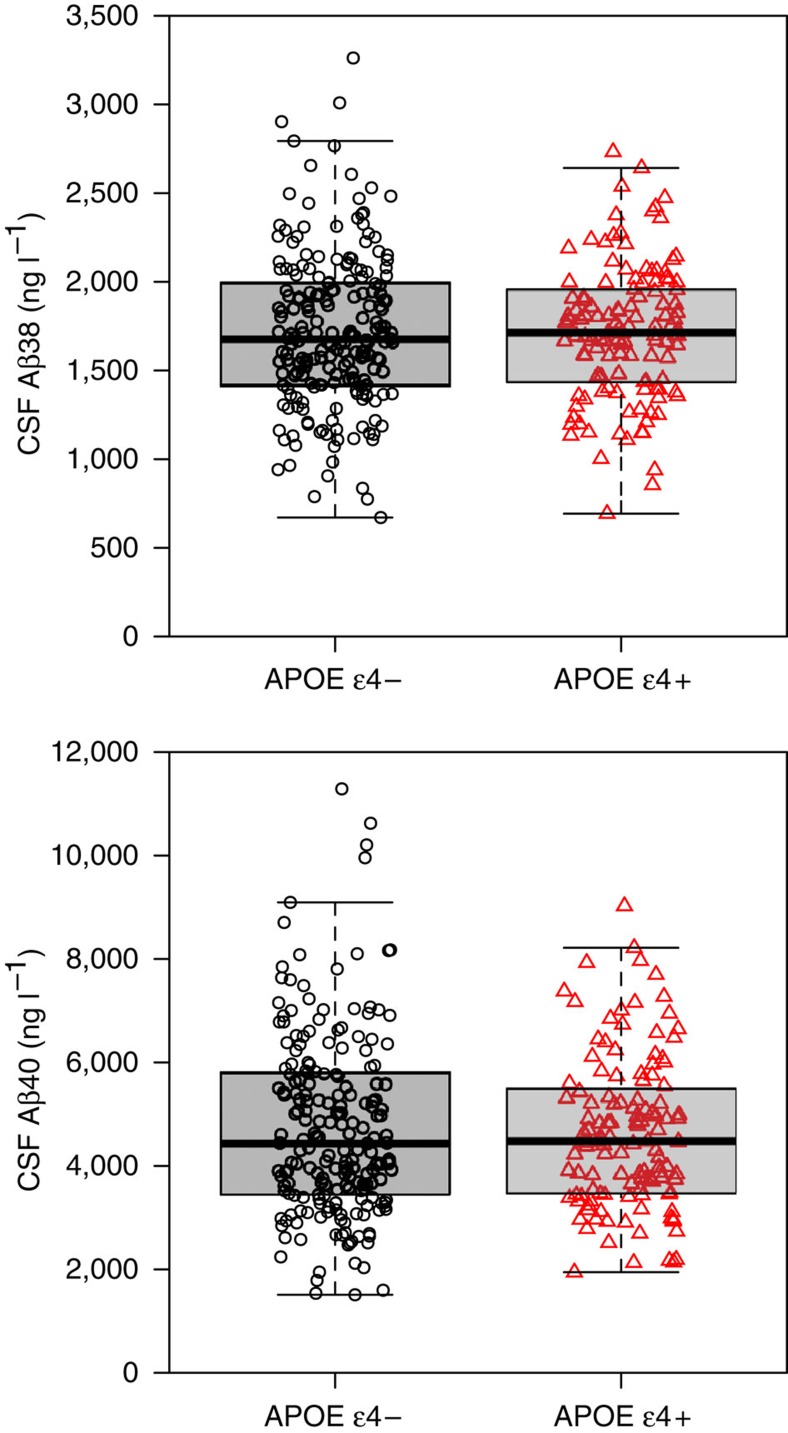
The cohort consisted of 331 participants (cognitively normal controls (CN) 121, subjective cognitive decline (SCD) 102 and mild cognitive impairment (MCI) 108). Demographics and data on cognition and biomarkers are summarized in Table 1 (see Table 2 for demographics stratified by APOE status). In sum, APOE ɛ4 positivity was more common in SCD and MCI than in CN, CSF Aβ42 levels were lower in MCI compared with the other groups, and the frequency of PET Aβ positivity was lowest in CN and highest in MCI. CSF Aβ38 and CSF Aβ40 did not differ between the diagnostic groups. APOE ɛ4 was not associated with CSF Aβ40 or with CSF Aβ38 (Fig. 1). The lack of association between APOE ɛ4 and CSF Aβ40 and CSF Aβ38 supports our assumption that these CSF Aβ peptides are unaffected by apoE4-mediated clearance of Aβ.
Table 1. Demographics.
| CN | SCD | MCI | All | P value | |
|---|---|---|---|---|---|
| N | 121 | 102 | 108 | 331 | |
| Age (y) | 73.7 (4.5) | 70.2 (5.6) | 71.2 (5.6) | 71.8 (5.4) | <0.001 |
| Sex (F) | 63% | 51% | 40% | 52% | 0.0023 |
| Education (y) | 11.5 (3.28) | 12.7 (3.28) | 11.3 (3.38) | 11.8 (3.39) | 0.0038 |
| MMSE (points) | 29.0 (0.92) | 28.5 (1.47) | 27.2 (1.69) | 28.3 (1.57) | <0.001 |
| ADAS-cog, delayed recall (points) | 2.1 (2.0) | 3.3 (2.2) | 6.4 (2.2) | 3.9 (2.8) | <0.001 |
| APOE ɛ4 (% +) | 28% | 42% | 43% | 37% | 0.028 |
| PET Aβ (% +) | 19% | 37% | 61% | 38% | <0.001 |
| PET Aβ (SUVR) | 1.30 (0.28) | 1.41 (0.38) | 1.70 (0.53) | 1.46 (0.44) | <0.001 |
| CSF Aβ38 (ng l−1) | 1,742 (404) | 1,722 (421) | 1,686 (421) | 1,718 (414) | 0.51 |
| CSF Aβ40 (ng l−1) | 4,510 (1526) | 4,893 (1852) | 4,812 (1809) | 4,727 (1728) | 0.35 |
| CSF Aβ42 (ng l−1) | 538 (187) | 584 (251) | 475 (216) | 532 (221) | 0.0031 |
ADAS-cog, Alzheimer's Disease Assessment Scale-cognitive subscale; CN, cognitively normal; CSF, cerebrospinal fluid; MCI, mild cognitive impairment; MMSE, mini-mental state examination; PET, positron emission tomography; SCD, subjective cognitive decline; SUVR, standardized uptake value ratio.
Continuous data are mean (s.d.). APOE e4+ is defined as at least one e4 allele. PET Aβ positivity is defined as >1.42 SUVR (ref. 13). MMSE ranges from 0 to 30. ADAS-cog delayed recall ranges from 0 to 10 (word list learning test from the ADAS-cog battery, points indicate number of missed items). P values are for comparisons between diagnostic groups (using Kruskal–Wallis test for continuous variables and X2-test for categorical variables).
Table 2. Demographics by diagnostic group and APOE ɛ4.
|
CN |
SCD |
MCI |
All |
|||||
|---|---|---|---|---|---|---|---|---|
| N |
121 |
102 |
108 |
331 |
||||
| APOE ɛ4− | APOE ɛ4+ | APOE ɛ4− | APOE ɛ4+ | APOE ɛ4− | APOE ɛ4+ | APOE ɛ4− | APOE ɛ4+ | |
| 87 | 34 | 59 | 43 | 61 | 47 | 207 | 124 | |
| Age (y) | 73.5 (4.4) | 74.1 (4.7) | 70.1 (6.0) | 70.3 (5.0) | 71.0 (6.1) | 71.5 (5.0) | 71.8 (5.6) | 71.8 (5.1) |
| Sex (F) | 63% | 62% | 53% | 49% | 41% | 38% | 54% | 48% |
| Education (y) | 11.6 (3.3) | 11.5 (3.3) | 12.9 (3.5) | 12.4 (2.9) | 11.3 (3.4) | 11.3 (3.3) | 11.9 (3.5) | 11.7 (3.2) |
| MMSE (points) | 29.0 (0.97) | 29.2 (0.78) | 28.4 (1.55) | 28.6 (1.35) | 27.2 (1.75) | 27.2 (1.62) | 28.3 (1.58) | 28.2 (1.57) |
| ADAS-cog, delayed recall (points) | 2.2 (2.1) | 1.7 (1.9) | 3.2 (2.3) | 3.5 (2.0) | 6.0 (2.3) | 6.9 (2.0) | 3.6 (2.7) | 4.3 (2.9) |
| PET Aβ (% +) | 10% | 41% | 20% | 61% | 38% | 91% | 21% | 67% |
| PET Aβ (SUVR) | 1.22 (0.16) | 1.48 (0.41) | 1.27 (0.29) | 1.59 (0.42) | 1.51 (0.51) | 1.95 (0.45) | 1.32 (0.35) | 1.70 (0.47) |
| CSF Aβ38 (ng l−1) | 1,741 (420) | 1,742 (365) | 1,735 (457) | 1,705 (367) | 1,670 (436) | 1,707 (405) | 1,719 (435) | 1,716 (380) |
| CSF Aβ40 (ng l−1) | 4,573 (1,655) | 4,348 (1,135) | 5,076 (2,051) | 4,643 (1,527) | 4,792 (1,969) | 4,838 (1,599) | 4,781 (1,871) | 4,636 (1,461) |
| CSF Aβ42 (ng l−1) | 571 (179) | 454 (181) | 673 (240) | 462 (213) | 559 (211) | 365 (168) | 596 (212) | 423 (192) |
ADAS-cog, Alzheimer's Disease Assessment Scale-cognitive subscale; CN, cognitively normal; CSF, cerebrospinal fliuid; MCI, mild cognitive impairment; MMSE, mini-mental state examination; PET, or positron emission tomography; SCD, subjective cognitive decline; SUVR, standardized uptake value ratio.
Continuous data are mean (s.d.). APOE ɛ4+ is defined as at least one ɛ4 allele. PET Aβ positivity is defined as>1.42 SUVR (ref. 13).
Figure 1. CSF Aβ38 and Aβ40 in APOE ɛ4- and APOE ɛ4+ subjects.
Observed data for CSF Aβ38 and CSF Aβ40 by APOE ɛ4 status. The individual observations are overlaid on boxplots (thick lines are medians, box limits are 25th and 75th percentiles). APOE ɛ4 did not affect levels of CSF Aβ38 (Mann–Whitney U-test, P=0.75; t-test, P=0.95; linear regression adjusted for age, sex and diagnosis, P=0.99) or CSF Aβ40 (Mann–Whitney U-test, P=0.84; t-test, P=0.43; linear regression adjusted for age, sex and diagnosis, P=0.26). This supports the notion that CSF Aβ38 and Aβ40 are unaffected by APOE ɛ4-mediated changes in Aβ clearance.
APOE ɛ4 and high CSF Aβ40 independently predict PET Aβ
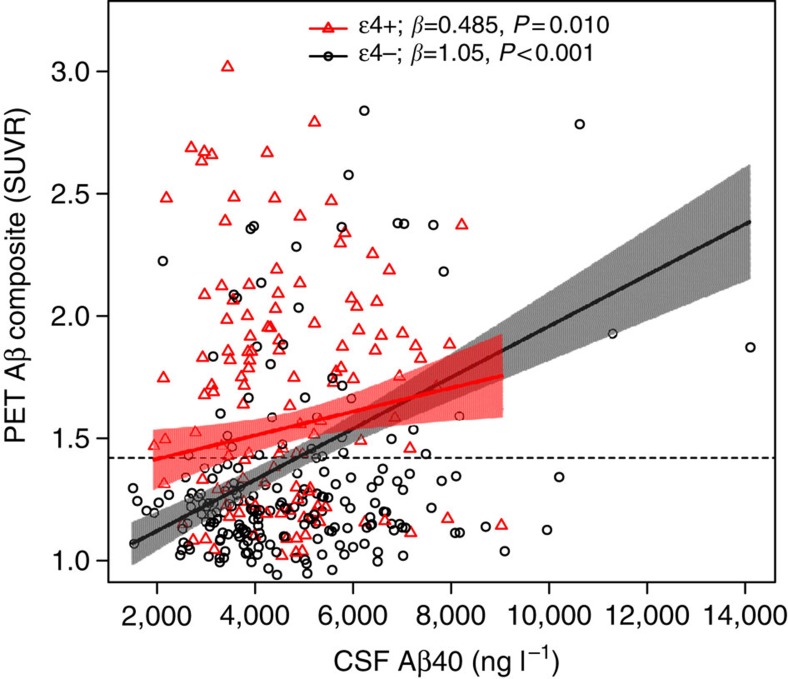
Figure 2 shows the observed PET Aβ and CSF Aβ40 data, with estimated slopes in the APOE ɛ4-positive and -negative groups. In a linear regression model with PET Aβ as the dependent variable, high levels of CSF Aβ40 (β=1.05 × 10−4, P<0.001), APOE ɛ4-positivity (β=0.406, P<0.001) and the interaction between APOE ɛ4 and CSF Aβ40 (β=−5.61 × 10−5, P=0.0080) were all significant predictors of continuous PET Aβ. Note that since APOE ɛ4 and CSF Aβ40 were both included as predictors the main effect of CSF Aβ40 indicates the effect within APOE ɛ4-negative subjects. The significant interaction between CSF Aβ40 and APOE ɛ4 indicates that the correlation between CSF Aβ40 and brain Aβ was stronger in APOE ɛ4-negative than in positive people (as seen in Fig. 2). The correlation between CSF Aβ40 and PET Aβ in the APOE ɛ4-positive group was weaker than in the APOE ɛ4-negative group, but remained significant (β=0.485 × 10−4, P=0.010). The results support the hypotheses that high CSF Aβ40 and APOE ɛ4 are independent predictors of PET Aβ, and that the relationship between CSF Aβ40 and PET Aβ varies with APOE ɛ4 carrier status. As expected, CSF Aβ42 was a significant covariate (low CSF Aβ42 was correlated with PET Aβ, β=−0.00120, P<0.001), but CSF Aβ40, APOE ɛ4 and the interaction between CSF Aβ40 and APOE ɛ4 remained significant also when not adjusting for CSF Aβ42 (CSF Aβ40: P=0.0089; APOE ɛ4: P<0.001; interaction: P=0.026). Age (β=0.0082, P=0.0094) and diagnosis (SCD, β=0.137, P=0.0011; MCI, β=0.299, P<0.001) were also significant predictors of PET Aβ, but sex was not (P=0.23). White matter lesions (WML) were evaluated as a covariate, but were not significant (P=0.68) and were therefore excluded from the final model. We also evaluated plasma levels of Aβ40 as a covariate to exclude the possibility that the results depended on peripheral APP processing. Plasma Aβ40 was not a significant covariate (P=0.99) and including it in the model did not change the other estimates.
Figure 2. PET Aβ as a function of CSF Aβ40 and APOE ɛ4.
Observed PET and CSF Aβ40 data. Slopes are modelled from a linear regression adjusted for CSF Aβ42, sex, age and diagnostic group. The shaded areas indicate 95% confidence intervals for the slopes. The dotted line indicates a cutoff for clinically significant PET Aβ load (1.42 SUVR). β-coefficients (divided by 10−4) and P values for the slopes within APOE ɛ4-positive and separately for APOE ɛ4-negative subjects are shown in the legend. The interaction between CSF Aβ40 and APOE ɛ4 is significant, indicating that the correlation between CSF Aβ40 and PET Aβ differs by APOE ɛ4 status (P=0.0080). The results did not change significantly when removing outliers (CSF Aβ40>10,000 ng l−1).
To further examine if clinically significant Aβ accumulation (defined as a composite standardized uptake value ratio (SUVR) >1.42 (ref. 13) was associated with CSF Aβ40, we evaluated a logistic regression model with PET Aβ positivity as the dependent variable. CSF Aβ40 (log odds=9.18 × 10−4, P<0.001) was a significant predictor in this model but APOE ɛ4 (P=0.13), and the interaction between CSF Aβ40 and APOE ɛ4 were not (P=0.73). Age and sex (P=0.13–0.14) were not significant but CSF Aβ42 (P<0.001) and diagnosis (SCD, P=0.0016; MCI, P<0.001) remained significant covariates. When CSF Aβ42 was excluded from the model, CSF Aβ40 (P=0.014) and APOE ɛ4 (P<0.001) were both significant predictors of PET Aβ positivity.
CSF Aβ38 as an independent predictor of PET Aβ
To corroborate our findings, we repeated the analyses using CSF Aβ38 instead of CSF Aβ40, with very similar results. When predicting continuous PET Aβ, the effects of CSF Aβ38 (β=4.04 × 10−4, P<0.001), APOE ɛ4 (β=0.72, P<0.001) and the interaction between APOE ɛ4 and CSF Aβ38 (β=−3.40 × 10−4, P<0.001) were all significant, and CSF Aβ42 was a significant covariate (β=−0.00112, P<0.001). CSF Aβ38 (P=0.017), APOE ɛ4 (P<0.001) and the interaction between APOE ɛ4 and CSF Aβ38 (P=0.015) remained significant when removing CSF Aβ42 from the model. When predicting PET Aβ positivity using logistic regression, CSF Aβ38 (log odds=0.00332, P<0.001) and APOE ɛ4 (log odds=4.47, P=0.0075) were independent predictors and there was a tendency for significant interaction between APOE ɛ4 and CSF Aβ38 (P=0.061). Again, CSF Aβ42 was a significant covariate (log odds=−0.0119, P<0.001).
We also used a combination of CSF Aβ40 and CSF Aβ38 based on their molar amounts (CSF Aβ, mol l−1). Again, the results were very similar. When predicting continuous PET Aβ, the effects of CSF Aβ (β=3.70 × 108, P<0.001), APOE ɛ4 (β=0.470, P<0.001) and the interaction between APOE ɛ4 and CSF Aβ (β=−2.20 × 108, P=0.0030) were all significant predictors. CSF Aβ42 remained a significant covariate (β=−0.00120, P<0.001). CSF Aβ (P=0.0090), APOE ɛ4 (P<0.001) and the interaction between APOE ɛ4 and CSF Aβ (P=0.021) remained significant when removing CSF Aβ42 from the model. When predicting PET Aβ positivity using logistic regression, CSF Aβ (log odds=3.15 × 109, P<0.001) was a significant predictor and CSF Aβ42 remained a significant covariate (log odds=−0.0129, P<0.001).
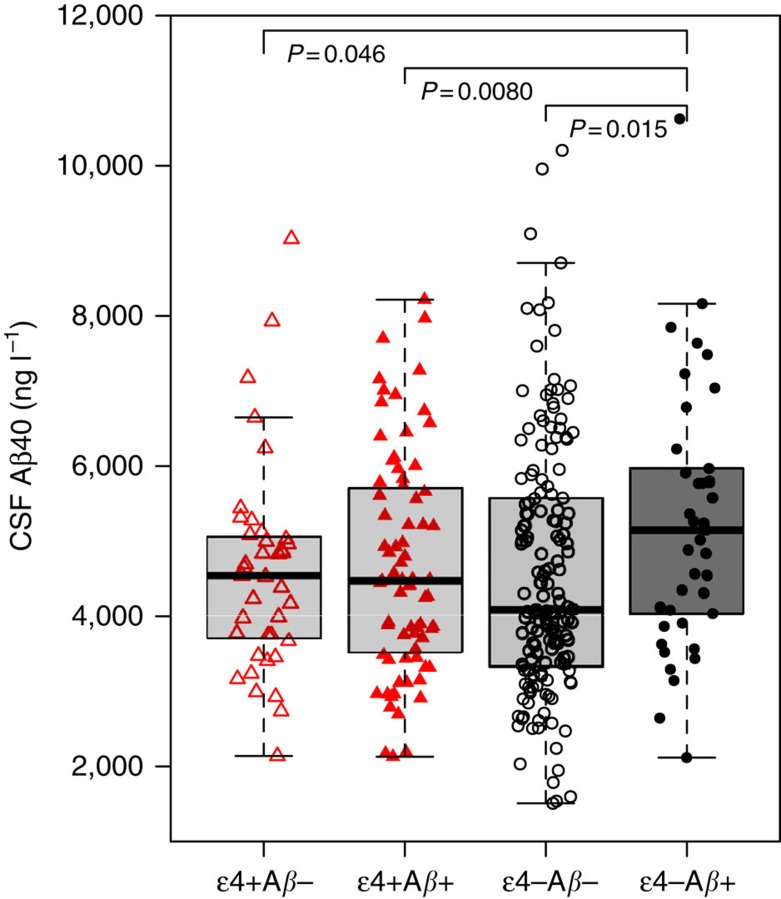
CSF Aβ40 is highest in APOE ɛ4− PET Aβ+ subjects
In a linear regression model with CSF Aβ40 as the dependent variable and a four level combination of PET Aβ and APOE as the independent variable, the overall highest CSF Aβ40 levels were seen in the PET Aβ+ & APOE ɛ4− group (β=732, P=0.015, compared with the reference category PET Aβ- & APOE ɛ4−, Fig. 3). PET Aβ+ & APOE ɛ4− subjects had 19% higher mean level of CSF Aβ40 (and 26% higher median level) compared with PET Aβ- & APOE ɛ4− subjects. The model was adjusted for WML (β=−18.8, P=0.00013), age (β=46.1, P=0.015), sex (female sex, β=−322, P=0.094) and diagnostic group (SCD, β=570, P=0.019; MCI, β=421, P=0.11). When also adjusting for CSF Aβ42 as a covariate the effect of PET Aβ & APOE ɛ4 was even stronger, with higher CSF Aβ40 in the PET Aβ+ & APOE ɛ4− group compared with PET Aβ- & APOE ɛ4− (P<0.001) and PET Aβ- & APOE ɛ4+ (P<0.001) but no significant difference compared with the PET Aβ+ & APOE ɛ4+ group (P=0.45).
Figure 3. CSF Aβ40 in different combinations of PET Aβ and APOE ɛ4.
Observed CSF Aβ40 for different combinations of APOE ɛ4 and PET Aβ positivity and negativity. The individual observations are overlaid on boxplots (thick lines are medians, box limits are 25th and 75th percentiles). CSF Aβ40 was significantly increased in the PET Aβ+ & APOE ɛ4− group compared with PET Aβ- & APOE ɛ4−, which was the reference category (P=0.015, using linear regression adjusted for age, sex, diagnosis and WML). No other group had significant different CSF Aβ40 compared with the PET Aβ- & APOE ɛ4− group (P=0.62–0.90). The groups were PET Aβ- & APOE ɛ4−, N=158; PET Aβ- & APOE ɛ4+, N=39; PET Aβ+ & APOE ɛ4−, N=41; and PET Aβ+ & APOE ɛ4+, N=75. The total N=313 for this analysis was smaller than the total study population (N=331) due to missing data for WML in 18 subjects (but the main results did not differ when WML was not included and the analysis was done on the whole study population). One data point is excluded from the graph for visual clarity (CSF Aβ40 14110, ng l−1, PET Aβ+ & APOE ɛ4−).
Discussion
We tested the hypothesis that biomarker surrogates of amyloidogenic APP processing (CSF Aβ40 and Aβ38) and APOE ɛ4 were independent predictors of brain Aβ fibril accumulation. In accordance with our hypotheses, CSF Aβ40 (and Aβ38 in a secondary analysis) and APOE ɛ4 were independent predictors of PET Aβ, and the effect of CSF Aβ40 was strongest in the APOE ɛ4-negative individuals. To our knowledge, this is the first study showing that increased Aβ production are associated with increased risk for sporadic brain Aβ accumulation. These novel results provide indirect evidence that brain Aβ pathology in humans may arise from two pathways, where one involves the APOE ɛ4 allele (likely causing reduced apoE4-mediated Aβ42 clearance), and the other involves increased amyloidogenic processing of APP. This may correspond to two pathways to sporadic AD, namely reduced clearance and increased production of Aβ peptides.
The amyloid cascade hypothesis postulates that Aβ pathology arises due to an imbalance between Aβ production and clearance6. It has been suggested that sporadic AD is mainly caused by poor clearance of peptides from the brain, whereas autosomal dominant AD is mainly caused by increased Aβ production, especially the Aβ42 variant. This is supported by a metabolic labelling study showing reduced Aβ clearance in sporadic AD dementia14, and studies showing increased amyloidogenic APP processing in early stages of autosomal dominant AD10. The main cause of reduced Aβ clearance in sporadic AD is likely APOE ɛ4, since the apoE4 protein isoform has reduced capacity to clear Aβ peptides compared with other apoE isoforms8, although it is possible that APOE ɛ4 may also contribute to increased AD risk by other mechanisms, for example, by affecting inflammation and neuronal repair15,16. However, one APP gene polymorphism which reduces Aβ production is associated with reduced risk of AD in the general population17, which provides genetic evidence that variations in APP processing may also affect the risk for sporadic AD.
The main limitation of this paper was that we used an indirect measure of APP processing, which was estimated by CSF Aβ40. The rationale for this approach was that Aβ40 is a major Aβ isoform produced by neurons11, which is not directly influenced by the presence of Aβ plaque pathology12, and is not influenced by APOE ɛ4-mediated impaired Aβ clearance. The later was demonstrated by our finding that there was no overall difference in CSF Aβ40 depending on APOE ɛ4 status (Fig. 1). Alterations in CSF Aβ40 are therefore more likely to reflect differences in amyloidogenic APP processing rather than differences in Aβ clearance. However, we acknowledge that there may be variations in APP processing that are not captured by CSF Aβ40. We also performed analyses using CSF Aβ38 (another highly expressed Aβ isoform) and a combination of CSF Aβ38 and CSF Aβ40 (based on their molar amounts), with very similar results as when using CSF Aβ40 alone, which support our findings. A more direct estimate of Aβ production may be done by metabolic labelling14, but such methods are liable to bias due to the longitudinal drift of CSF biomarkers during continuous CSF sampling that depends on sampling frequency and volume18. Another limitation is that there may be other factors affecting CSF Aβ40 besides variations in APP processing. For example, reduced CSF Aβ40 is associated with chronic WML19, and WML may also be associated with Aβ pathology (although this is more common in MCI20 and AD dementia20 than in non-demented people21). It is not clear if the association between CSF Aβ40 and WML is due to a direct link between Aβ production and WML or if lower CSF Aβ40 levels reflect reduced neuronal Aβ secretion due to decreased brain activity in the presence of WML. Importantly, our results remained significant when adjusting for WML. Theoretically, CSF Aβ40 could also be influenced by peripheral APP processing, but our results were stable when adjusting for plasma Aβ40, suggesting that the effects did not depend on peripheral APP processing. We did not measure all other possible factors besides increased amyloidogenic APP that may contribute to Aβ deposition in APOE ɛ4-negative subjects. For example, other AD risk genes (including CLU and CR1) may impact Aβ clearance in APOE ɛ4-negative subjects22. We included several different diagnostic groups, including a SCD group. We noted that the frequency of Aβ positivity in our SCD subjects (37%) was higher than in a recent large meta-analysis by Jansen et al.3 where ∼22% of SCD subjects were Aβ-positive, compared with ∼25% of CN subjects. The reason for this difference is not clear, but we noted that our SCD subjects were on average 6 years older than the Jansen subjects, which may contribute to higher frequency of Aβ pathology. Furthermore, all our SCD subjects were referred to specialized memory clinics because of cognitive symptoms, while some of the Jansen SCD subjects may have been seen at other health care facilities, opening for the possibility that they had less severe complaints than the SCD subjects in our study. Another recent study on PET Aβ positivity in memory clinic SCD subjects found that 57% of SCD subjects were Aβ-positive compared with 31% of CN, which more resembles the findings in our cohort23. Finally, we did not include an AD dementia group, since we know from a previous study that patients with severe AD dementia have lower CSF Aβ40 than patients with mild dementia (this may reflect reduced capacity to produce Aβ peptides as the disease progresses)24. Including an AD dementia group in this study would therefore risk confounding the relationship between CSF Aβ40 and PET Aβ.
Until now, there have been few attempts to examine the independent roles of APOE ɛ4 and APP processing in the development of brain Aβ pathology in non-demented subjects. Previous studies did not find correlations between CSF Aβ40 (or Aβ38) and PET Aβ (ref. 12). This is likely because they did not co-vary for APOE ɛ4 (and/or CSF Aβ42). Adjusting for APOE ɛ4 is important since the relationship between CSF Aβ40 and PET Aβ differs between APOE ɛ4-positive and -negative individuals. Furthermore, adjusting for APOE ɛ4 and CSF Aβ42 reduces the residual errors of the models, and some of this error may contribute to the variance of CSF Aβ40. Once this error is removed the correlation between CSF Aβ40 and PET Aβ can be better estimated. Our results add novel information and point to different possible pathways to Aβ pathology in humans. In sum, our results support the idea that sporadic Aβ accumulation may be partly associated with increased amyloidogenic APP production, especially in APOE ɛ4-negative subjects. The risk for sporadic AD may consequently depend on increased Aβ production, in addition to decreased Aβ clearance. This provides novel insight into disease mechanisms in AD and may be important for development of drugs targeting Aβ metabolism in early stages of AD.
Methods
Study population
The study population came from the Swedish BioFINDER study (Biomarkers For Identifying Neurodegenerative Disorders Early and Reliably). All available CN and non-demented patients with mild cognitive symptoms characterized as having SCD or MCI were included.
CN subject were originally enrolled from the population-based EPIC cohort. The inclusion criteria were: age ≥60 years old, MMSE 28-30, and fluent in Swedish. Exclusion criteria were: presence of subjective cognitive impairment, significant neurologic disease (for example, stroke, Parkinson's disease, multiple sclerosis), severe psychiatric disease (for example, severe depression or psychotic syndromes), dementia or MCI. All CN subjects underwent a thorough clinical assessment, including neurological, psychiatric and cognitive testing all performed by a medical doctor, in addition to MRI of the brain and relevant blood tests. The cognitive battery included MMSE, ADAS-cog (items 1–3), Trail Making A & B, Symbol Digit modalities, A quick test of cognitive speed, clock drawing, cube coping, letter S fluency and animals fluency. The medical doctor made a global assessment of whether the individual was cognitively healthy based on the test results in relation to education and age. All CN subjects had a Clinical Dementia Rating scale score of 0.
The SCD and MCI cases were recruited consecutively and were thoroughly assessed by physicians with special competence in dementia disorders. The inclusion criteria were: referred to a memory clinic due to possible cognitive impairment, not fulfilling the criteria for dementia, MMSE 24–30, age 60–80 years and, fluent in Swedish. The exclusion criteria were: cognitive impairment that without doubt could be explained by another condition (other than prodromal dementia); severe somatic disease; and refusing lumbar puncture or neuropsychological investigation. The classification in SCD or MCI was based on a neuropsychological battery and the clinical assessment of a senior neuropsychologist. The battery included tests for verbal ability (including A multiple-choice vocabulary test (SRB:1 (ref. 25) and semantic verbal fluency (Condition 2, D-KEFS (ref. 26), episodic memory (including Rey Auditory Verbal Learning Test (RAVLT (ref. 27), and Rey Complex Figure Test (RCFT (ref. 28)), visuospatial construction ability (including Block design (WAIS (ref. 29) and The copy trial of Rey Complex Figure Test), attention and executive functions (including Trail Making Test (D-KEFS (ref. 26) and Letter Verbal Fluency, Condition 1 (D-KEFS (ref. 26)). A senior neuropsychologist stratified all patients into those with SCD (no measurable cognitive deficits) or MCI according to the consensus criteria for MCI suggested by Petersen30.
The Regional Ethics Committee in Lund, Sweden, approved the study. All subjects gave written informed consent. For more details, see ref. 13 and www.biofinder.se.
PET analysis
Brain Aβ was measured using 18F-flutemetamol PET (refs 31, 32). PET/CT scanning was conducted at two sites using the same type of scanner, a Philips Gemini TF 16. PET sum images from 90 to 110 min post injection were generated for the average uptake. MRI results were not used since this does not improve the quantification of 18F-flutemetamol data33. The images were analysed using the NeuroMarQ software provided by GE Healthcare. A volume of interest template was applied for nine bilateral regions (prefrontal, parietal, lateral temporal, medial temporal, sensorimotor, occipital, anterior cingulate and posterior cingulate/precuneus), combined in a global neocortical composite signal33. The SUVR was the global composite tracer uptake, normalized for the mean uptake in the cerebellar cortex (note that Thurfjell et al.35 found that 18F-flutemetamol PET SUVR had >98% concordance with visual reads independent of which reference region that was used). Most analyses in this study used continuous PET Aβ but when indicated a previously defined cutoff for Aβ positivity was used (>1.42 SUVR, based on mixture modelling analysis13).
Cerebrospinal fluid analysis
All subjects underwent lumbar CSF sampling at baseline, following the Alzheimer's Association Flow Chart35. Samples were stored in 1 ml polypropylene tubes at −80 °C until analysis. CSF Aβ38, Aβ40 and Aβ42 were analysed by ELISA assays (EUROIMMUN AG, Lübeck, Germany). All analyses were performed by board-certified laboratory technicians who were blinded for clinical data and diagnoses. The CSF samples were randomized to avoid group bias. The analyses were performed during two different runs in batch, plates 1–20 using lot no. E140224AB for Aβ38, E130611AA for Aβ40 and E130607AA for Aβ42, and plates 21–24 using lot no. E150522BK for Aβ38, E150302A1 for Aβ40 and E150522AZ for Aβ42. Aliquots of two different pools of CSF were used as internal control samples, with CVs of 13.8% for Aβ38 for the first control with a mean of 695 pg ml−1 and 7.9% for Aβ38 for the second control with a mean of 1596, pg ml−1; 17.9% for Aβ40 for the first control with a mean of 1951, pg ml−1 and 11.1% for Aβ40 for the second control with a mean of 3992, pg ml−1; and 16.3% for Aβ42 for the first control with a mean of 227 pg ml−1 and 15.1% for Aβ42 for the second control with a mean of 216 pg ml−1. To assure consistency in levels between the two runs, 40 CSF samples from the first run were re-analysed in the second run.
Plasma analysis
For plasma collection, blood was drawn into tubes containing EDTA as anticoagulant. After centrifugation (2000g, +4 °C, 10 min), plasma samples were aliquoted into polypropylene tubes and stored at −80 °C pending biochemical analyses. Plasma Aβ40 was analysed using Simoa immunoassay (Quanterix, Lexington, MA, USA).
White matter lesions
All patients were examined using a single 3T MR scanner (Trio, Siemens). Automated segmentation of WML was performed using the Lesion Segmentation Tool implemented in SPM8 (http://www.applied-statistics.de/lst.html), generating a total WML volume. Before this, manual segmentation for reference of WML was performed on FLAIR images co-registered to the native MPRAGE in four MCI patients, with the segmented volume ranging from 0.5 to 106.3 ml; the resulting optimal κ based on the Dice coefficient was 0.4 (ref. 36) and was used in the subsequent automated segmentation for all participants.
Statistical analysis
We tested correlations between CSF Aβ40 and PET Aβ in different regression models. The main model was a linear regression model where the dependent variable was PET Aβ and the independent variables were CSF Aβ40, APOE ɛ4 (dichotomous), and the interaction between CSF Aβ40 and APOE ɛ4. Second, we tested the correlation between clinically significant PET Aβ accumulation and CSF Aβ40 and APOE ɛ4 in a logistic regression model with PET Aβ positivity as the dependent variable. Third, we tested a linear regression model with CSF Aβ40 as the dependent variable and a four level combination of PET Aβ and APOE ɛ4 as the independent variable (PET Aβ- & APOE ɛ4−, PET Aβ- & APOE ɛ4+, PET Aβ+ & APOE ɛ4− and PET Aβ+ & APOE ɛ4+). All models were adjusted for age (years), sex and diagnostic group. We also adjusted for CSF Aβ42 to test if CSF Aβ40 was associated with PET Aβ beyond CSF Aβ42, and to reduce the residual error of the model, allowing a better estimate of the correlation between CSF Aβ40 and PET Aβ. We adjusted for WML (ml) except for when WML was clearly nonsignificant, as detailed in the results section. The primary analyses were done using CSF Aβ40, but we also performed analyses using CSF Aβ38 and a combination of CSF Aβ38 and Aβ40 (based on their molar weights, Aβ38: 4129.012 g mol−1; and Aβ40: 4327.148 g mol−1 (ref. 37). Statistical significance was determined at P<0.05. All analyses were done using R (v. 3.0.1, The R Foundation for Statistical Computing).
Additional information
How to cite this article: Mattsson, N. et al. Increased amyloidogenic APP processing in APOE ɛ4-negative individuals with cerebral β-amyloidosis. Nat. Commun. 7:10918 doi: 10.1038/ncomms10918 (2016).
Acknowledgments
We are very grateful to all study participants in the Swedish BioFINDER study. We also thank the collaborators of this study and the entire Swedish BioFINDER study (www.biofinder.se), including Susanna Vestberg for neuropsychological assessments, Christer Nilsson, Katarina Nägga and Per Johansson for clinical evaluations, Per Wollmer and Douglas Hägerström for [18F]-flutemetamol PET imaging. N.M. and O.H. had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. This study was supported by the European Research Council, the Swedish Research Council, the Strategic Research Area MultiPark (Multidisciplinary Research in Parkinson's disease) at Lund University, the Crafoord Foundation, the Swedish Brain Foundation, The Swedish Alzheimer foundation, the Torsten Söderberg Foundation at the Royal Swedish Academy of Sciences, the Knut and Alice Wallenberg Foundation, Frimurarestiftelsen and the Swedish federal government under the ALF agreement. The funding sources had no role in the design and conduct of the study; in the collection, analysis, interpretation of the data; or in the preparation, review, or approval of the manuscript. Doses of [18F]flutemetamol injection were sponsored by GE Healthcare.
Footnotes
N.M., P.S.I., S.P., E.S., L.H. and O.H. report no conflicts of interest. K.B. has served as a consultant for Eli Lilly, Novartis, Roche Diagnostics and Sanofi-Aventis, and at Advisory Boards for IBL International and lecturing for Fujirebio Europe and Lundbeck. K.B. and H.Z. are co-founders of Brain Biomarker Solutions in Gothenburg AB, a GU Holding-based platform company at the University of Gothenburg.
Author contributions N.M. and O.H. had the full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design was formulated by N.M. and O.H. Acquisition, analysis or interpretation of data were done by N.M., P.S.I., S.P., H.Z., K.B., E.S., L.M. and O.H. Drafting of the manuscript was done by N.M. Critical revision of the manuscript for important intellectual content was done by P.S.I., S.P., E.S., L.M., H.Z., K.B. and O.H. Statistical analysis was done by N.M. and P.S.I. N.M. and O.H. obtained funding for this study. Administrative, technical or material support was provided by S.P., H.Z., K.B., E.S., L.M. and O.H. Study was done under the supervision of N.M. and O.H.
References
- Bateman R. J. et al. Clinical and biomarker changes in dominantly inherited Alzheimer's disease. N. Engl. J. Med. 367, 795–804 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villemagne V. L. et al. Amyloid β deposition, neurodegeneration, and cognitive decline in sporadic Alzheimer's disease: a prospective cohort study. Lancet Neurol. 12, 357–367 (2013). [DOI] [PubMed] [Google Scholar]
- Jansen W. J. et al. Prevalence of cerebral amyloid pathology in persons without dementia: a meta-analysis. JAMA. 313, 1924–1938 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klunk W. E. et al. Imaging brain amyloid in Alzheimer's disease with Pittsburgh Compound-B. Ann. Neurol. 55, 306–319 (2004). [DOI] [PubMed] [Google Scholar]
- Blennow K., Mattsson N., Schöll M., Hansson O. & Zetterberg H. Amyloid biomarkers in Alzheimer's disease. Trends Pharmacol. Sci. 36, 297–309 (2015). [DOI] [PubMed] [Google Scholar]
- Hardy J. & Selkoe D. J. The amyloid hypothesis of Alzheimer's disease: progress and problems on the road to therapeutics. Science 297, 353–356 (2002). [DOI] [PubMed] [Google Scholar]
- Morris J. C. et al. APOE predicts amyloid-beta but not tau Alzheimer pathology in cognitively normal aging. Ann. Neurol. 67, 122–131 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castellano J. M. et al. Human apoE isoforms differentially regulate brain amyloid-beta peptide clearance. Sci. Transl. Med. 3, 89ra57 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward A. et al. Prevalence of apolipoprotein E4 genotype and homozygotes (APOE e4/4) among patients diagnosed with Alzheimer's disease: a systematic review and meta-analysis. Neuroepidemiology 38, 1–17 (2012). [DOI] [PubMed] [Google Scholar]
- Reiman E. M. et al. Brain imaging and fluid biomarker analysis in young adults at genetic risk for autosomal dominant Alzheimer's disease in the presenilin 1 E280A kindred: a case-control study. Lancet Neurol. 11, 1048–1056 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore S. et al. APP metabolism regulates tau proteostasis in human cerebral cortex neurons. Cell Rep. 11, 689–696 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fagan A. M. et al. Cerebrospinal fluid tau and ptau(181) increase with cortical amyloid deposition in cognitively normal individuals: implications for future clinical trials of Alzheimer's disease. EMBO Mol. Med. 1, 371–380 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palmqvist S. et al. Accuracy of brain amyloid detection in clinical practice using cerebrospinal fluid β-amyloid 42: a cross-validation study against amyloid positron emission tomography. JAMA Neurol. 71, 1282–1289 (2014). [DOI] [PubMed] [Google Scholar]
- Mawuenyega K. G. et al. Decreased clearance of CNS beta-amyloid in Alzheimer's disease. Science 330, 1774 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michaelson D. M. APOE ɛ4: the most prevalent yet understudied risk factor for Alzheimer's disease. Alzheimers Dement. 10, 861–868 (2014). [DOI] [PubMed] [Google Scholar]
- Yu J.-T., Tan L. & Hardy J. Apolipoprotein E in Alzheimer's disease: an update. Annu. Rev. Neurosci. 37, 79–100 (2014). [DOI] [PubMed] [Google Scholar]
- Jonsson T. et al. A mutation in APP protects against Alzheimer's disease and age-related cognitive decline. Nature 488, 96–99 (2012). [DOI] [PubMed] [Google Scholar]
- Li J. et al. Effect of human cerebrospinal fluid sampling frequency on amyloid-β levels. Alzheimers Dement. 8, 295–303 (2012). [DOI] [PubMed] [Google Scholar]
- Selnes P. et al. Effects of cerebrovascular disease on amyloid precursor protein metabolites in cerebrospinal fluid. Cerebrospinal. Fluid. Res. 7, 10 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brun A. & Englund E. A white matter disorder in dementia of the Alzheimer type: a pathoanatomical study. Ann. Neurol. 19, 253–262 (1986). [DOI] [PubMed] [Google Scholar]
- Hedden T. et al. Disruption of functional connectivity in clinically normal older adults harboring amyloid burden. J. Neurosci. 29, 12686–12694 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambert J.-C. & Amouyel P. Genetics of Alzheimer's disease: new evidences for an old hypothesis? Curr. Opin. Genet. Dev. 21, 295–301 (2011). [DOI] [PubMed] [Google Scholar]
- Snitz B. E. et al. Amyloid-β Imaging in Older Adults Presenting to a Memory Clinic with Subjective Cognitive Decline: A Pilot Study. J. Alzheimers Dis. 48, (Suppl 1): S151–S159 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosen C. et al. Cerebrospinal fluid profiles of amyloid beta-related biomarkers in Alzheimer's disease. Neuromolecular. Med. 14, 65–73 (2012). [DOI] [PubMed] [Google Scholar]
- Nilsson L.-G. et al. The betula prospective cohort study: memory, health, and aging. Neuropsychol. Dev. Cogn. B Aging Neuropsychol. Cogn. 4, 1–32 (1997). [Google Scholar]
- Delis D. C., Kaplan E. & Kramer J. H. Delis-Kaplan executive function system TM: Examiner's Manual The Psychological Corporation (2001). [Google Scholar]
- Strauss E., Sherman E. M. & Spreen O. A Compendium of Neuropsychological Tests. Administration, Norms, and Commentary – third edition Oxford University Press (2006). [Google Scholar]
- Meyers J. E. & Meyers K. R. Rey Complex Figure Test and Recognition Trial Psychological Resources, Inc. (1995). [Google Scholar]
- Wechsler D. Wechsler Adult Intelligence Scale 4th edn, (ed. Psykologiförlaget A. B.) (Pearson, Inc., 2008; Harcourt Assessment, Swedish version, 2010).
- Petersen R. C. Mild cognitive impairment as a diagnostic entity. J. Intern. Med. 256, 183–194 (2004). [DOI] [PubMed] [Google Scholar]
- Koole M. et al. Whole-body biodistribution and radiation dosimetry of 18F-GE067: a radioligand for in vivo brain amyloid imaging. J. Nucl. Med. 50, 818–822 (2009). [DOI] [PubMed] [Google Scholar]
- Nelissen N. et al. Phase 1 study of the Pittsburgh compound B derivative 18F-flutemetamol in healthy volunteers and patients with probable Alzheimer disease. J. Nucl. Med. 50, 1251–1259 (2009). [DOI] [PubMed] [Google Scholar]
- Lundqvist R. et al. Implementation and validation of an adaptive template registration method for 18F-flutemetamol imaging data. J. Nucl. Med. 54, 1472–1478 (2013). [DOI] [PubMed] [Google Scholar]
- Thurfjell L. et al. Automated quantification of 18F-flutemetamol PET activity for categorizing scans as negative or positive for brain amyloid: concordance with visual image reads. J. Nucl. Med. 55, 1623–1628 (2014). [DOI] [PubMed] [Google Scholar]
- Blennow K., Hampel H., Weiner M. & Zetterberg H. Cerebrospinal fluid and plasma biomarkers in Alzheimer disease. Nat. Rev. Neurol. 6, 131–144 (2010). [DOI] [PubMed] [Google Scholar]
- Schmidt P. et al. An automated tool for detection of FLAIR-hyperintense white-matter lesions in multiple sclerosis. NeuroImage 59, 3774–3783 (2012). [DOI] [PubMed] [Google Scholar]
- Brinkmalm G. et al. An online nano-LC-ESI-FTICR-MS method for comprehensive characterization of endogenous fragments from amyloid beta and amyloid precursor protein in human and cat cerebrospinal fluid. J. Mass. Spectrom. 47, 591–603 (2012). [DOI] [PubMed] [Google Scholar]