Abstract
Background:
Asian women have a younger age at onset of breast cancer and a lower body mass index (BMI) than Western women. The link between obesity and risk of breast cancer in Asian women is still elusive. We aimed to investigate the effect of BMI on the risk of incident breast cancer in Taiwanese women.
Methods:
A total of 1 393 985 women who had been cancer-free before recruitment and attended a nation-wide Taiwanese breast cancer-screening program between 1999 and 2009 were enrolled using a prospective cohort study. Obesity and other relevant variables (such as menopause status and other biochemical markers) were collected through in-person interviews, anthropometric measurements and blood samples at first screen. Incident breast cancers during follow-up were ascertained through the linkage of the cohort with the National Cancer Registry and the National Death Certification System.
Results:
A total of 6969 and 7039 incident breast cancer cases were identified among women enrolled before and after menopause, respectively. Compared with a BMI range of 18.5–23.9 kg m−2, the incremental level of BMI in the enrolled women before menopause revealed a lack of statistically significant association with the risk of incident breast cancer (adjusted hazard ratio=0.94, 0.98, 1.02, 1.01 and 0.82 for BMI <18.5, 24–26.9, 27–29.9, 30–34.9 and ⩾35, respectively), but the incremental level of BMI in the enrolled women after menopause led to a statistically significant incremental increase in the risk of breast cancer (adjusted hazard ratio=0.78, 1.19, 1.31, 1.53 and 1.65 for BMI <18.5, 24–26.9, 27–29.9, 30–34.9 and ⩾35, respectively) after adjusting for other explanatory risk factors.
Conclusion:
Obesity acts mainly as an influential promoter of the development of late-onset breast cancer after menopause in Taiwanese women.
Introduction
Breast cancer is the most commonly diagnosed cancer in women worldwide1 and has recently increased markedly in Taiwan.2 Excess body weight, an emerging problem worldwide, has been reported to be associated with elevated risks of many non-communicable chronic diseases.3 Although body mass index (BMI), which is generally used to define overweight or obese, varies among ethnicities and cannot completely reflect adiposity, excess body weight is one of the most important contributors to mortality worldwide4 and is considered an established factor for several types of cancer,5, 6 including breast cancer. The evidence showing that high BMI has significant negative and positive associations with risk of breast cancer among pre- and post-menopausal women, respectively, is mainly from Western populations.5, 7 However, inconclusive results have been reported from Asian populations such as Taiwanese women partly because the data used in the previous studies are too sparse and partly because the epidemiological profiles are different across ethnic groups, specifically in that the incidence of breast cancer in Asian women peaks at age 40–50 years, whereas it peaks at age 60–70 years in Western women.8 Socio-economic profiles, lifestyles, cultures and genetic backgrounds related to occurrence of breast cancer in Asian population are also at odds with those in Western populations.8, 9 Therefore, a better understanding of the similarities and differences between Asian and Western women in major breast cancer risk factors (such as BMI) could potentially be of great benefit to designing and providing more effective screening and primary prevention programs.
High BMI is associated with an elevated risk of breast cancer in post-menopausal women with consistent evidence.5, 7, 10, 11, 12, 13, 14, 15, 16, 17, 18 However, the association between obesity and breast cancer risk is controversial in pre-menopausal women,7, 19, 20 which may be attributed to different anthropometric measurements of body composition presentation (including BMI, body height or waist-to-hip ratio) and different study designs (such as cohort studies or case–control studies). As Asian people have been reported to have higher levels of body fat, more abdominal fat and less-lean mass than the other ethnic groups for a given BMI,19, 20, 21 such findings motivate us to test the postulate, ‘Is the effect of BMI on breast cancer risk greater in Asian women?'.
In this study, we aimed to investigate the effect of current BMI on the risk of incident breast cancer in Taiwanese pre-menopausal and post-menopausal women using a large population-based cohort study. We also examined the effect of BMI on the age at breast cancer diagnosis during follow-up among women recruited in this cohort study.
Materials and methods
Study cohort
A nation-wide prospective non-selective breast cancer-screening program has been conducted in Taiwan since 1999 using three stepwise stages. The first population cohort launched in 1999, the second cohort launched in 2002, and the third cohort launched in 2005. The recruitment and follow-up of the first two cohorts have been previously described.22 In brief, in cohort I (n=897 806), women aged 35 years or older at screening were invited via a governmental publicity campaign to enroll in this nation-wide cohort between 1999 and 2001. In cohort II (n=301 181), women aged 50–69 years were invited to enroll in the program between 2002 and 2004. In the first two cohorts, all participants were screened via physical examination by public health nurses or by questionnaire, respectively, to exclude women at high risk of breast cancer prior to further ultrasonography and mammography. In cohort III (n=595 410), women aged 40 years and older were invited between 2005 and 2009 to participate in the nation-wide breast cancer-screening program, which offered mammography every 2 years. Women (n=311 832) who were repeatedly recruited in at least two of the three cohorts were identified, and only their first screen was retained in the final analyses. We excluded subjects who had not gone through menopause by age 60, those with incomplete data for height, weight, BMI or menopausal status, and subjects who at baseline were menopausal owing to surgical reasons. All enrolled subjects were considered to be free of breast cancer. A total of 1 393 985 women were included in the following analyses. All the subjects gave informed consent, and this nation-wide cancer-screening program was supported and approved by the Department of Health, Executive Yuan (No.1039900137).
All women recruited in these three cohorts were free of symptoms and underwent face-to-face interviews with public health nurses or health-care providers at recruitment for the collection of basic personal data including anthropometric measurements, menstrual and reproductive history, and family and medical history. BMI was calculated as weight (kilograms) divided by squared height (square meters) and obtained only at entry into the study. Values of BMI were grouped as follows according to recommendations for Taiwanese adults from the Department of Health, Executive Yuan: underweight (<18.5), normal-weight (18.5–23.9), overweight (24–26.9), mild obesity (27–29.9), moderate obesity (30–34.9) and morbid obesity (35 or more). Information on hormone usage was included in the questionnaires for cohorts II and III, but not for cohort I.
Follow-up and identification of cancer cases
All enrolled women were followed from the start of screening until 26 October 2012.2 The incident breast cancer during follow-up was ascertained using the National Cancer Registry and the National Death Certification System. All hospitals in Taiwan have a legal obligation to actively report cases of treated or diagnosed cancer to the National Cancer Registry. In addition, any migration or death must be registered with the local household registration office in Taiwan; therefore, all deceased residents in Taiwan were included in the computerized national death certificate data. Regardless of emigration, we could trace the vital status of all participants through data linkage with the household registration and death certification systems. To investigate the relationship between baseline BMI and subsequent breast cancer cases in the breast cancer-screening program cohort and to identify breast cancers that may have already developed but would not be identified by screening, we further differentiated breast cancer diagnosed during follow-up as prevalent and incident breast cancer. Prevalent breast cancer cases were defined as subjects who had a positive screening result and were diagnosed with breast cancer. Other breast cancer cases diagnosed during follow-up were regarded as incident cases.
Statistical analysis
The data are presented as the number of patients along with the percentage, as shown in Table 1. The time to occurrence of breast cancer was calculated from the date of the first screen to the diagnosis of incident breast cancer, death, loss to follow-up or the end of the study, whichever came first. The life-table method was used to show the actual number of breast cancer cases and their percent distribution according to BMI at enrollment and age of diagnosis of breast cancer for pre- and post-menopausal women. Cox proportional hazards regression models were used to assess the association between incident breast cancer and BMI, age at recruitment, family history of breast cancer, history of hormone usage, and reproductive factors including age at menarche, number of births, age at first full-term pregnancy and breast-feeding history. Hazard ratios were estimated using univariate and multi-variable regression models for all explanatory variables, including BMI, age at recruitment, family history of breast cancer, age at menarche, number of births, age at first full-term pregnancy and history of breastfeeding. Trends analyses were also performed for the level of BMI and other variables. All statistical analyses were performed using the PC version of the Statistical Analysis System (SAS, version 9.1; SAS Institute, Inc., Cary, NC, USA). All programming codes for the statistical analyses are available upon request (Chiou S-T and Chen H-H).
Table 1. The demographic and hormone-related characteristics of all recruited women.
| Factors |
Pre-menopause N=503 007 |
Post-menopause N=890 978 |
||||
|---|---|---|---|---|---|---|
| Free of breast cancer N(%) | Prevalence breast cancer N(%) | Incidence breast cancer N(%) | Free of breast cancer N(%) | Prevalence breast cancer N(%) | Incidence breast cancer N(%) | |
| Age at recruitment | ||||||
| <40 | 121 968(24.67) | 141(8.80) | 1702(24.42) | 1005(0.11) | 0(0.00) | 11(0.16) |
| 40–49 | 225 429(45.59) | 450(28.09) | 3962(56.85) | 21 032(2.39) | 39(1.05) | 258(3.67) |
| 50–59 | 147 039(29.74) | 1011(63.11) | 1305(18.73) | 450 445(51.17) | 2236(60.08) | 3772(53.59) |
| 60–69 | 0(0.00) | 0(0.00) | 0(0.00) | 31 8301(36.16) | 1353(36.35) | 2522(35.83) |
| ⩾70 | 0(0.00) | 0(0.00) | 0(0.00) | 89 434(10.16) | 94(2.53) | 476(6.76) |
| BMI | ||||||
| <18.5 | 15 384(3.22) | 36(2.29) | 224(3.34) | 19331(2.46) | 84(2.40) | 103(1.71) |
| 18.5–23.9 | 283 602(59.36) | 936(59.58) | 4161(62.02) | 375 549(47.70) | 1593(45.61) | 2578(42.80) |
| 24–26.9 | 114 707(24.01) | 377(24.00) | 1518(22.63) | 237 766(30.20) | 1093(31.29) | 1939(32.19) |
| 27–29.9 | 43 546(9.11) | 154(9.80) | 562(8.38) | 105 322(13.38) | 490(14.03) | 923(15.32) |
| 30–34.9 | 17 532(3.67) | 62(3.95) | 216(3.22) | 42 716(5.43) | 196(5.61) | 417(6.92) |
| ⩾35 | 2993(0.63) | 6(0.38) | 28(0.42) | 6599(0.84) | 37(1.06) | 63(1.05) |
| Age at menarche | ||||||
| ⩽13 | 134 295(28.32) | 526(33.80) | 2091(31.41) | 159 981(18.65) | 950(25.75) | 1345(19.70) |
| 14 | 138 451(29.19) | 440(28.28) | 2008(30.16) | 189 723(22.12) | 977(26.48) | 1578(23.12) |
| 15 | 98 623(20.80) | 290(18.64) | 1303(19.57) | 173 794(20.26) | 731(19.81) | 1429(20.93) |
| ⩾16 | 102 866(21.69) | 300(19.28) | 1256(18.86) | 334 368(38.95) | 1032(27.97) | 2474(36.24) |
| Birth | ||||||
| No | 22 378(4.57) | 136(8.57) | 399(5.81) | 35 302(4.02) | 306(8.23) | 399(5.70) |
| Yes | 467 736(95.43) | 1451(91.43) | 6471(94.19) | 842 123(95.98) | 3414(91.77) | 6600(94.30) |
| No. of birtha | ||||||
| 1 | 35 762(7.65) | 156(10.75) | 643(9.94) | 33 909(4.03) | 255(7.47) | 315(4.77) |
| 2 | 186 266(39.82) | 653(45.00) | 2884(44.57) | 159 867(18.98) | 989(28.97) | 1318(19.97) |
| ⩾3 | 245 708(52.53) | 642(44.25) | 2944(45.50) | 648 347(76.99) | 2170(63.56) | 4967(75.26) |
| Age at full-term pregnancya | ||||||
| ⩽22 | 92 818(26.33) | 111(18.17) | 1091(19.09) | 328 738(39.86) | 958(28.47) | 2283(35.23) |
| 23–25 | 107 326(30.44) | 181(29.62) | 1642(28.73) | 274 274(33.26) | 1089(32.36) | 2116(32.65) |
| 26–29 | 104 786(29.72) | 202(33.06) | 1914(33.48) | 161 333(19.56) | 885(26.30) | 1459(22.51) |
| ⩾30 | 47 605(13.50) | 117(19.15) | 1069(18.70) | 60 316(7.31) | 433(12.87) | 623(9.61) |
| Breast feedinga | ||||||
| No | 211 953(44.72) | 854(55.17) | 3104(47.58) | 193 792(22.44) | 1382(37.62) | 1626(23.98) |
| Yes | 261 997(55.28) | 694(44.83) | 3420(52.42) | 66 9749(77.56) | 2292(62.38) | 5155(76.02) |
| Family history | ||||||
| No | 472 375(96.52) | 1473(92.41) | 6573(95.27) | 844 882(96.77) | 3444(92.71) | 6633(95.03) |
| Yes | 17045(3.48) | 121(7.59) | 326(4.73) | 28220(3.23) | 271(7.29) | 347(4.97) |
| Hormone therapy | ||||||
| No | 99 652(91.75) | 845(92.86) | 508(88.04) | 366 358(81.96) | 2444(82.71) | 1718(77.11) |
| Yes | 8963(8.25) | 65(7.14) | 69(11.96) | 80 664(18.04) | 511(17.29) | 510(22.89) |
Among parous women.
Results
Among the 1 393 985 women enrolled in total, 503 007 women were pre-menopausal and 890 978 women were post-menopausal. A total of 8571 (including 1602 prevalent and 6969 incident cases of breast cancer) and 10 761 (including 3722 prevalent and 7039 incident cases of breast cancer) newly diagnosed cases of breast cancer were recorded during follow-up among pre- and post-menopausal women, respectively. Baseline demographic data are shown in Table 1.
Table 2 presents the associations between the baseline explanatory variables and the development of incident breast cancer according to menopausal status at recruitment. Only incident breast cancer cases were included in the final analyses. As expected, breast cancer risks were significantly higher in women with a family history of breast cancer and among those who had used hormones, and risks were significantly lower among those who had delayed menarche and those who had given birth. Among women with a history of childbirth, breastfeeding and high-order parity were associated with lower risks of breast cancer, whereas older age at first delivery was associated with increased risk. All associations remained significant in the baseline pre- and post-menopausal groups after adjusting for the explanatory factors with each other.
Table 2. Cox proportional hazards regression analyses for the crude HR and multiple variable-adjusted HR for risk of breast cancer in women recruited before and after menopause.
| Factors |
Pre-menopause |
Post-menopause |
||||
|---|---|---|---|---|---|---|
| Crude HR |
aHR |
Crude HR |
aHR |
|||
| (95% CI) | (95% CI) | P-value | (95% CI) | (95% CI) | P-value | |
| BMI (vs 18.5–23.9) | ||||||
| <18.5 | 0.94(0.82,1.07) | 0.94(0.81,1.10) | 0.9999a | 0.79(0.65,0.97) | 0.78(0.63,0.96) | <0.0001a |
| 24–26.9 | 0.95(0.90,1.01) | 0.98(0.91,1.04) | 1.13(1.06,1.20) | 1.19(1.12,1.27) | ||
| 27–29.9 | 0.96(0.87,1.04) | 1.02(0.93,1.13) | 1.22(1.13,1.31) | 1.31(1.21,1.41) | ||
| 30–34.9 | 0.93(0.81,1.06) | 1.01(0.86,1.18) | 1.41(1.27,1.56) | 1.53(1.38,1.71) | ||
| ⩾35 | 0.71(0.49,1.03) | 0.82(0.54,1.24)b | 1.50(1.17,1.92) | 1.65(1.27,2.13) | ||
| Age at recruitment (vs <40) | ||||||
| 40–49 | 1.26(1.19,1.34) | 1.39(1.30,1.48) | <0.0001a | 1.11(0.61,2.03) | 0.96(0.49,1.88) | <0.0001a |
| 50–59 | 1.39(1.29,1.49) | 1.72(1.56,1.90) | 1.34(0.74,2.42) | 1.25(0.65,2.41) | ||
| 60–69 | — | 1.07(0.59,1.93) | 1.21(0.63,2.33) | |||
| ⩾70 | — | 0.59(0.33,1.08) | 0.73(0.37,1.41) | |||
| Age at menarche (vs ⩽13) | ||||||
| 14 | 0.91(0.85,0.97) | 0.96(0.90,1.03) | <0.0001a | 0.88(0.82,0.95) | 0.94(0.87,1.02) | <0.0001a |
| 15 | 0.83(0.83,0.89) | 0.89(0.82,0.96) | 0.83(0.77,0.90) | 0.92(0.85,1.00) | ||
| ⩾16 | 0.76(0.76,0.82) | 0.82(0.76,0.89) | 0.66(0.62,0.71) | 0.78(0.72,0.84) | ||
| Birth (vs no) | ||||||
| Yes | 0.73(0.66,0.81) | 0.81(0.62,1.06) | 0.1186 | 0.62(0.56,0.69) | 0.67(0.54,0.83) | 0.0003 |
| No. of birthc (vs 1) | ||||||
| 2 | 0.86(0.79,0.94) | 0.91(0.82,1.00) | <0.0001a | 0.89(0.79,1.01) | 0.96(0.83,1.10) | <0.0001a |
| ⩾3 | 0.66(0.60,0.71) | 0.76(0.69,0.85) | 0.59(0.53,0.66) | 0.80(0.70,0.92) | ||
| Age at first full-term pregnancyc (vs ⩽22) | ||||||
| 23–25 | 1.29(1.20,1.39) | 1.28(1.18,1.39) | <0.0001a | 1.20(1.13,1.27) | 1.15(1.08,1.23) | <0.0001a |
| 26–29 | 1.54(1.43,1.66) | 1.46(1.35,1.58) | 1.57(1.47,1.68) | 1.33(1.23,1.44) | ||
| ⩾30 | 1.89(1.74,2.06) | 1.69(1.54,1.87) | 1.87(1.72,2.05) | 1.51(1.36,1.68) | ||
| Breast feedingc (vs no) | ||||||
| Yes | 0.86(0.82,0.91) | 0.94(0.89,0.99) | 0.0243 | 0.67(0.63,0.71) | 0.86(0.80,0.92) | <0.0001 |
| Family history (vs no) | ||||||
| Yes | 1.57(1.41,1.76) | 1.39(1.22,1.59) | <0.0001 | 2.02(1.81,2.24) | 1.68(1.48,1.90) | <0.0001 |
| Hormone therapy (vs no) | ||||||
| Yes | 1.25(0.97,1.61) | — | 1.25(1.13,1.38) | — | ||
Abbreviations: BMI, body mass index; CI, confidence interval; HR, hazards ratio. aHR: adjusted hazard ratio calculated by multiple variable Cox proportional hazards regression model for the risk of breast cancer after adjustment for all the variables include BMI, age, age at menarche, birth history, number of birth, age at the first full-term pregnancy, breast-feeding history and family history of breast cancer.
P-value for trend.
P-value=0.3575 for testing BMI ⩾35 vs BMI<35 (HR=0.82, 95% CI=0.54–1.25).
Among parous women.
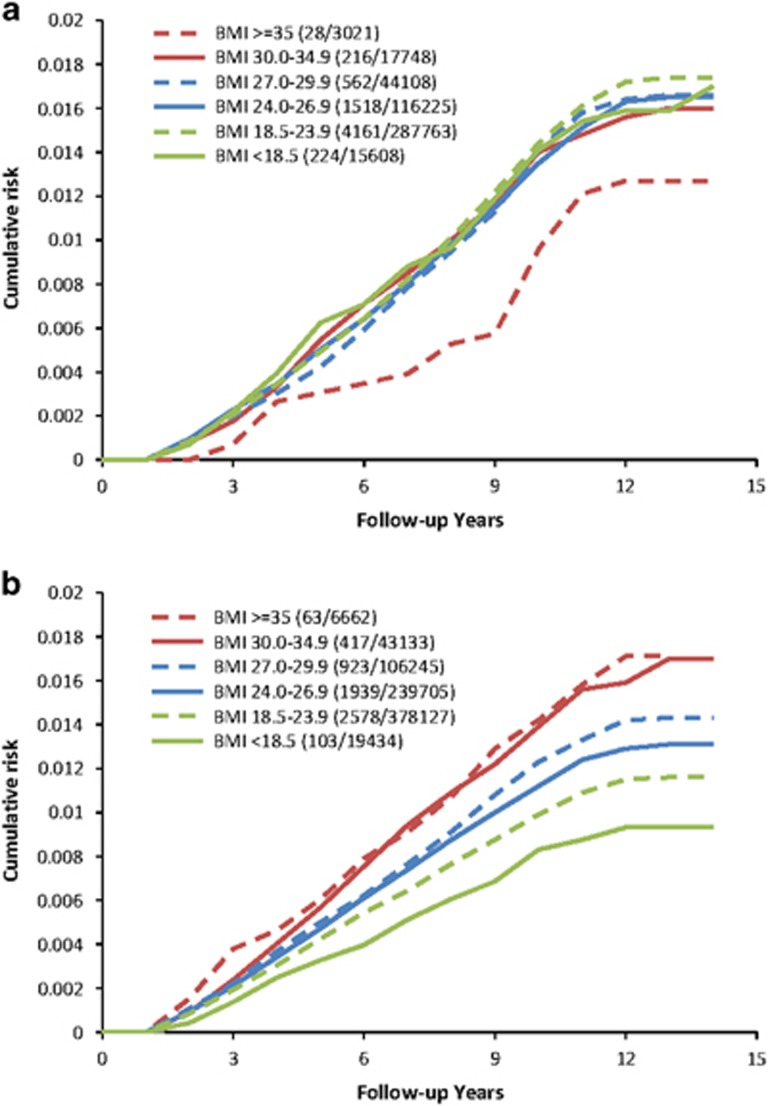
The relationship between baseline BMI and risk of incident breast cancer during follow-up is shown in Table 2 and Figure 1. High BMI was associated with increased risk of breast cancer in post-menopausal women, and this association remained after adjusting for all explanatory variables. A total of 6969 and 7039 incident breast cancer cases were identified among the enrolled women before and after menopause, respectively. Compared with the reference subgroup of BMI within 18.5–23.9 kg m−2 that contained the largest number of enrolled subjects among all BMI subgroups, the incremental level of BMI at recruitment in the enrolled women before menopause was not statistically significantly associated with the risk of incident breast cancer (adjusted hazard ratio=0.94, 0.98, 1.02, 1.01 and 0.82 for BMI <18.5, 24–26.9, 27–29.9, 30–34.9 and ⩾35, respectively), but the incremental level of BMI at recruitment in the enrolled women after menopause led to a statistically significant incremental increase in the risk of incident breast cancer (adjusted hazard ratio=0.78, 1.19, 1.31, 1.53 and 1.65 for BMI <18.5, 24–26.9, 27–29.9, 30–34.9 and ⩾35, respectively) after adjusting for other explanatory risk factors. Although morbidly obese (BMI ⩾35 kg m−2) women who were pre-menopausal at recruitment had a lower risk of developing incident breast cancer, this association was not statistically significant. Figures 1a and b show the cumulative incidence of breast cancer during follow-up by BMI among women who were pre- and post-menopausal at recruitment, respectively. The morbidly obese women recruited before menopause had a trend of lower cumulative incidence of breast cancer during the follow-up period (Figure 1a). The cumulative incidence of new breast cancers during follow-up increased with greater baseline BMI among women who were menopausal at recruitment (Figure 1b).
Figure 1.
(a) The cumulative risk of breast cancer by six different BMI levels in women recruited before menopause. (b) The cumulative risk of breast cancer by six different BMI levels in women recruited after menopause.
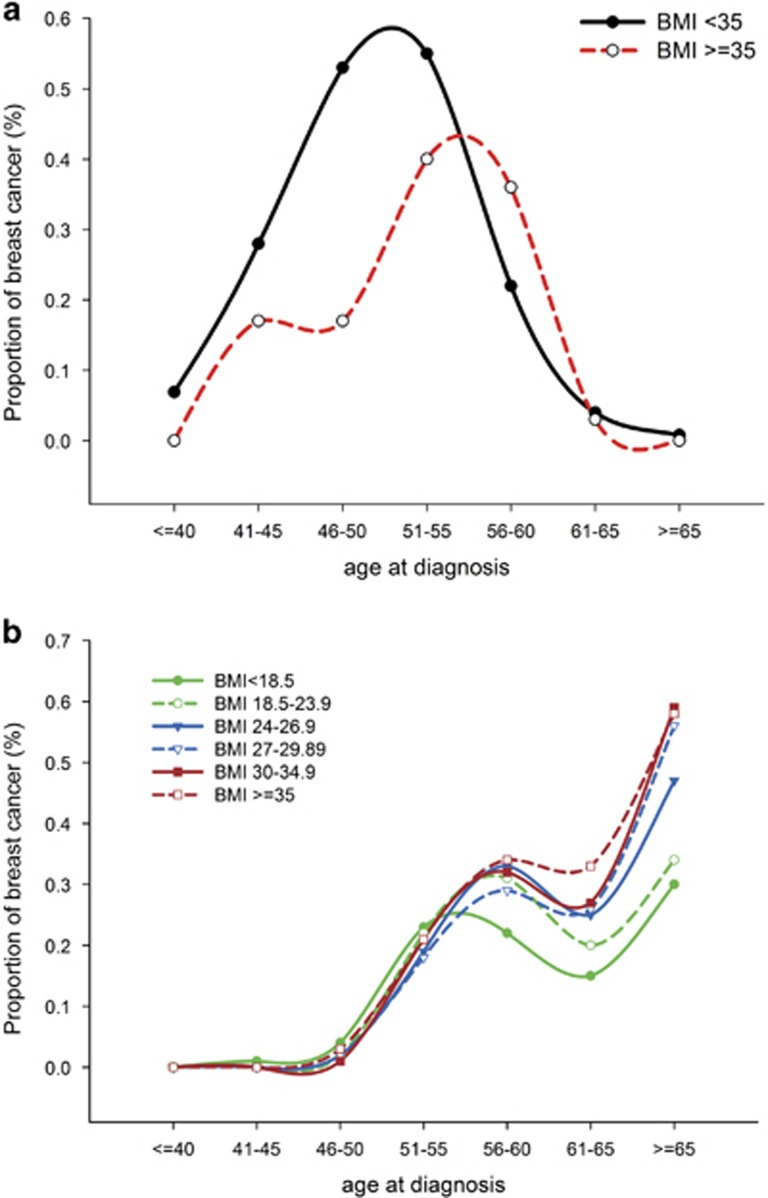
To further investigate the effects of baseline BMI on the age at diagnosis of breast cancer among pre- and post-menopausal women, we stratified all subjects according to baseline BMI and plotted the proportion of breast cancer diagnosed at different age bands during follow-up. As shown in Figure 2a, the peak percentage of breast cancer diagnosed at each age subgroup in pre-menopausal women with preceding morbidly obese (BMI ⩾35 kg m−2) tended to occur at an older age than those with lower baseline BMI. For women who were post-menopausal at recruitment, as shown in Figure 2b, the percentage of breast cancer increased with the incremental level of BMI.
Figure 2.
(a) The proportion of breast cancer diagnosed at seven age subgroups in women with and without preceding morbid obesity recruited before menopause. (b) The proportion of breast cancer diagnosed at seven age subgroups among different preceding BMI levels in women recruited after menopause.
Discussion
Because Asian women generally have lower BMI23 and an earlier peak age of breast cancer incidence than Western women,8 it is therefore worthwhile to investigate the effect of BMI on the risk of incident breast cancer for pre-menopausal and post-menopausal Taiwanese women using a large prospective cohort study like our study design. We found BMI was a strong predictor of breast cancer for post-menopausal but not for pre-menopausal Taiwanese women. Obesity seems to mainly exert its effects on breast cancer among older women.
The precipitating effect of adiposity and obesity on the risk of breast cancer in post-menopausal women had been well established in all ethnicities.5, 6, 7, 17 Such an association seems stronger in Asian populations than among Caucasian women in meta-analyses of previous studies.5, 19, 20, 24 In this study, we not only confirmed the positive association between BMI and risk of breast cancer in the enrolled women after menopause, but also revealed that the risk of incident breast cancer was nearly twofold (adjusted odds ratio=1.65) in morbidly obese women compared with women of normal-weight enrolled after menopause. Hence, the effect of BMI on the risk of breast cancer in Taiwanese women seems much higher than in women in Western countries.5, 7, 20, 24 The higher impact of high BMI on the risk of breast cancer in Asian women, as shown in this study, might be explained by the greater adiposity in Asian women than in other ethnicities for a given BMI.19 Therefore, the WHO-recommended BMI level for overweight and obesity for Asians is quite different from the recommended level for Caucasians.23
The biological mechanisms linking obesity to elevated risk of breast cancer have been explained by the higher rate of conversion of androgenic precursors to estrogens through the peripheral aromatization in adipose tissue.20, 25 The high levels of insulin and insulin-like growth factor in response to obesity and increased estrogens levels have been found to stimulate the development and growth of cancer cells in both pre- and post-menopausal women.20, 26 A trend of more frequent estrogen receptor-positive and hormone-dependent subtypes of breast cancer in post-menopausal women14, 27 provides strong evidence to support the association between high BMI and risk of incident breast cancer among post-menopausal women.
The association between BMI and breast cancer risk among pre-menopausal women of different ethnicities remains controversial,5, 6, 7 especially among Asian women. Although some studies have reported an inverse relationship between BMI and breast cancer risk among Indian and Asian–American women,16, 17, 28 most studies among pre-menopausal Asian women from Japan, China, Hong Kong and Taiwan have suggested no association or a positive association between BMI and breast cancer risk.5, 6, 12, 13, 14, 15, 18, 29, 30 The main criticism of these previous Asian studies15, 17, 21, 28, 29, 31, 32 is the use of a case–control study design, small sample size, the failure of considering age onset of breast cancer and the narrow range of BMI, all of which could be solved by using a large population-based cohort study design as in the current study.
It is very interesting to note that morbidly obese women had a lower incidence of breast cancer before menopause, which was consistent with the previous finding that greater BMI during earlier periods of life may be inversely related to breast cancer risk.33, 34, 35 In our cohort, though morbidly obese women who were enrolled prior to menopause tended to be at lower odds of having early-onset breast cancer; however, this protective effect of morbid obesity disappeared and inversed at advanced age, which is upheld by growing evidence that the hormone receptor status of breast cancer leads to differential breast cancer risk based on race, obesity and age.36, 37 Younger women (⩽50 years) with obesity (BMI ⩾30 kg m−2) have a higher prevalence of aggressive and hormone receptor-negative breast cancer,36 whereas older women (>50 years) with obesity have increased risk of hormone receptor-positive breast cancer.14, 36 Moreover, it has been reported that greater body fatness and BMI during childhood, adolescence and young adulthood are associated with higher prevalence of anovulatory disorders such as polycystic ovary syndrome and infertility,38, 39, 40 resulting in lower estrogen levels, which, in turn, leads to lower breast cancer risk in women throughout life.41, 42, 43 However, anovulation itself cannot completely explain the reduced breast cancer risk in obese young women.33 Recently, obesity has been reported to be associated with rapid decline in ovarian reserve44 and early menopause.45 Further studies are needed to investigate the relationship between histology, obesity and ovarian function on the risk of breast cancer.
Our study has some limitations. Although we found that morbidly obese women enrolled both before and after menopause have higher incidence of breast cancer diagnosed at advanced age, particularly from 56 years of age onward as shown in Figure 2, this might imply the association between adiposity and estrogen-dependent breast cancer diagnosed after menopause. However, the data on BMI at the time of breast cancer diagnosis, age of menopause, status of menopause at the time of breast cancer diagnosis and breast cancer histology (hormone receptor status) were not available in this study. Moreover, the influence of BMI at the time of breast cancer diagnosis and change in adiposity on the risk of breast cancer could also not be investigated in the present study. Therefore, these might limit the interpretation of the potential impact of BMI and obesity on the hormone-dependent subtype of breast cancer and its association with menopausal status in this study. Some individuals with breast cancer might have long-term survival or may not have early diagnosis using current screening methods. Therefore, to investigate the causal relationship between baseline BMI levels and risk of breast cancer, and to avoid bias from over-representation of breast cancer cases, we only included incident breast cancer in all analyses. Another concern pertains to the sparsity of breast cancer cases among morbidly obese pre-menopausal women that precludes us from reaching the statistically significant result as shown in Table 2, suggesting further study with a larger sample size is needed to clarify the result.
Using a large prospective Taiwanese cohort study, we found that baseline BMI was not significantly associated with risk of incident breast cancer in women enrolled before menopause, but the higher the level of BMI, the higher the risk for incident breast cancer in women enrolled after menopause. Although morbid obesity seems to have a protective effect on the risk of breast cancer, especially in early-onset breast cancer in women enrolled before menopause, it was not statistically significant when confined to incident breast cancer cases. Our findings suggest that excess weight may act as an influential promoter for the late-stage development of post-menopausal breast cancer among Taiwanese women.
Acknowledgments
All authors thank the hospital, physicians, public health nurses and health-care providers involved in this national screening project. This work was supported by the Health Promotion Administration, Ministry of Health and Welfare (A1011119 and A1021227).
Author contributions
All authors made substantial contribution to the conception and design, analysis, and interpretation of data and to critical review of the manuscript. MJC carried out the design of the study, interpretation of the results and drafted the manuscript. WYYW performed the statistical analysis and helped to design the study and draft the manuscript. AMFY, JCYF, SLSC and SYHC helped in the data acquisition, interpretation of the data, conception and design of study and statistical analysis. HHC conceived and designed the study, coordinated the data collection and analysis, and revised the manuscript. STC carried out the administrative, technical and material support. All authors read and approved the final manuscript.
The authors declare no conflict of interest.
References
- Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin 2015; 65: 87–108. [DOI] [PubMed] [Google Scholar]
- Department of HealthCancer Registry Annual Report 2010. In: Department of Health, Executive Yuan: Taipei, Taiwan, 2013.
- WHOGlobal Health Risks: Mortality and Burden of Disease Attributable to Selected Major Risks. In: World Health Organization: Geneva, Switzerland, 2009.
- Ezzati M, Lopez AD, Rodgers A, Vander Hoorn S, Murray CJ. Selected major risk factors and global and regional burden of disease. Lancet 2002; 360: 1347–1360. [DOI] [PubMed] [Google Scholar]
- Renehan AG, Tyson M, Egger M, Heller RF, Zwahlen M. Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Lancet 2008; 371: 569–578. [DOI] [PubMed] [Google Scholar]
- Parr CL, Batty GD, Lam TH, Barzi F, Fang X, Ho SC et al. Body-mass index and cancer mortality in the Asia-Pacific Cohort Studies Collaboration: pooled analyses of 424,519 participants. Lancet Oncol 2010; 11: 741–752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van den Brandt PA, Spiegelman D, Yaun SS, Adami HO, Beeson L, Folsom AR et al. Pooled analysis of prospective cohort studies on height, weight, and breast cancer risk. Am J Epidemiol 2000; 152: 514–527. [DOI] [PubMed] [Google Scholar]
- Leong SP, Shen ZZ, Liu TJ, Agarwal G, Tajima T, Paik NS et al. Is breast cancer the same disease in Asian and Western countries? World J Surg 2010; 34: 2308–2324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhoo-Pathy N, Yip CH, Hartman M, Uiterwaal CS, Devi BC, Peeters PH et al. Breast cancer research in Asia: adopt or adapt Western knowledge? Eur J Cancer 2013; 49: 703–709. [DOI] [PubMed] [Google Scholar]
- Lahmann PH, Hoffmann K, Allen N, van Gils CH, Khaw KT, Tehard B et al. Body size and breast cancer risk: findings from the European Prospective Investigation into Cancer And Nutrition (EPIC). Int J Cancer 2004; 111: 762–771. [DOI] [PubMed] [Google Scholar]
- Tehard B, Clavel-Chapelon F. Several anthropometric measurements and breast cancer risk: results of the E3N cohort study. Int J Obes (Lond) 2006; 30: 156–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuriyama S, Tsubono Y, Hozawa A, Shimazu T, Suzuki Y, Koizumi Y et al. Obesity and risk of cancer in Japan. Int J Cancer 2005; 113: 148–157. [DOI] [PubMed] [Google Scholar]
- Kawai M, Minami Y, Kuriyama S, Kakizaki M, Kakugawa Y, Nishino Y et al. Adiposity, adult weight change and breast cancer risk in postmenopausal Japanese women: the Miyagi Cohort Study. Br J Cancer 2010; 103: 1443–1447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suzuki R, Orsini N, Saji S, Key TJ, Wolk A. Body weight and incidence of breast cancer defined by estrogen and progesterone receptor status—a meta-analysis. Int J Cancer 2009; 124: 698–712. [DOI] [PubMed] [Google Scholar]
- Chow LW, Lui KL, Chan JC, Chan TC, Ho PK, Lee WY et al. Association between body mass index and risk of formation of breast cancer in Chinese women. Asian J Surg 2005; 28: 179–184. [DOI] [PubMed] [Google Scholar]
- Mathew A, Gajalakshmi V, Rajan B, Kanimozhi V, Brennan P, Mathew BS et al. Anthropometric factors and breast cancer risk among urban and rural women in South India: a multicentric case-control study. Br J Cancer 2008; 99: 207–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu AH, Yu MC, Tseng CC, Pike MC. Body size, hormone therapy and risk of breast cancer in Asian-American women. Int J Cancer 2007; 120: 844–852. [DOI] [PubMed] [Google Scholar]
- Wu MH, Chou YC, Yu JC, Yu CP, Wu CC, Chu CM et al. Hormonal and body-size factors in relation to breast cancer risk: a prospective study of 11,889 women in a low-incidence area. Ann Epidemiol 2006; 16: 223–229. [DOI] [PubMed] [Google Scholar]
- Amadou A, Ferrari P, Muwonge R, Moskal A, Biessy C, Romieu I et al. Overweight, obesity and risk of premenopausal breast cancer according to ethnicity: a systematic review and dose-response meta-analysis. Obes Rev 2013; 14: 665–678. [DOI] [PubMed] [Google Scholar]
- Amadou A, Hainaut P, Romieu I. Role of obesity in the risk of breast cancer: lessons from anthropometry. J Oncol 2013; 2013: 906495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rush EC, Freitas I, Plank LD. Body size, body composition and fat distribution: comparative analysis of European, Maori, Pacific Island and Asian Indian adults. Br J Nutr 2009; 102: 632–641. [DOI] [PubMed] [Google Scholar]
- Wu GH, Chen LS, Chang KJ, Hou MF, Chen SC, Liu TJ et al. Evolution of breast cancer screening in countries with intermediate and increasing incidence of breast cancer. J Med Screen 2006; 13 (Suppl 1): S23–S27. [PubMed] [Google Scholar]
- Consultation WHOE. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004; 363: 157–163. [DOI] [PubMed] [Google Scholar]
- Cheraghi Z, Poorolajal J, Hashem T, Esmailnasab N, Doosti Irani A. Effect of body mass index on breast cancer during premenopausal and postmenopausal periods: a meta-analysis. PloS One 2012; 7: e51446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Renehan AG, Roberts DL, Dive C. Obesity and cancer: pathophysiological and biological mechanisms. Arch Physiol Biochem 2008; 114: 71–83. [DOI] [PubMed] [Google Scholar]
- Endogenous HBreast Cancer Collaborative G, Key TJ, Appleby PN, Reeves GK, Roddam AW. Insulin-like growth factor 1 (IGF1), IGF binding protein 3 (IGFBP3), and breast cancer risk: pooled individual data analysis of 17 prospective studies. Lancet Oncol 2010; 11: 530–542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang WY, Newman B, Millikan RC, Schell MJ, Hulka BS, Moorman PG. Hormone-related factors and risk of breast cancer in relation to estrogen receptor and progesterone receptor status. Am J Epidemiol 2000; 151: 703–714. [DOI] [PubMed] [Google Scholar]
- Ziegler RG, Hoover RN, Nomura AM, West DW, Wu AH, Pike MC et al. Relative weight, weight change, height, and breast cancer risk in Asian-American women. J Natl Cancer Inst 1996; 88: 650–660. [DOI] [PubMed] [Google Scholar]
- Shu XO, Jin F, Dai Q, Shi JR, Potter JD, Brinton LA et al. Association of body size and fat distribution with risk of breast cancer among Chinese women. Int J Cancer 2001; 94: 449–455. [DOI] [PubMed] [Google Scholar]
- Li HL, Gao YT, Li Q, Liu DK. [Anthropometry and female breast cancer: a prospective cohort study in urban Shanghai]. Zhonghua liu xing bing xue za zhi 2006; 27: 488–493. [PubMed] [Google Scholar]
- Chie WC, Chen CF, Lee WC, Chen CJ. Body size and risk of pre- and post-menopausal breast cancer in Taiwan. Anticancer Res 1996; 16: 3129–3132. [PubMed] [Google Scholar]
- Chie WC, Li CY, Huang CS, Chang KJ, Lin RS. Body size as a factor in different ages and breast cancer risk in Taiwan. Anticancer Res 1998; 18: 565–570. [PubMed] [Google Scholar]
- Michels KB, Terry KL, Willett WC. Longitudinal study on the role of body size in premenopausal breast cancer. Arch Intern Med 2006; 166: 2395–2402. [DOI] [PubMed] [Google Scholar]
- Magnusson C, Baron J, Persson I, Wolk A, Bergstrom R, Trichopoulos D et al. Body size in different periods of life and breast cancer risk in post-menopausal women. Int J Cancer 1998; 76: 29–34. [DOI] [PubMed] [Google Scholar]
- Le Marchand L, Kolonel LN, Earle ME, Mi MP. Body size at different periods of life and breast cancer risk. Am J Epidemiol 1988; 128: 137–152. [DOI] [PubMed] [Google Scholar]
- Yang XR, Chang-Claude J, Goode EL, Couch FJ, Nevanlinna H, Milne RL et al. Associations of breast cancer risk factors with tumor subtypes: a pooled analysis from the Breast Cancer Association Consortium studies. J Natl Cancer Inst 2011; 103: 250–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desantis C, Ma J, Bryan L, Jemal A. Breast cancer statistics, 2013. CA Cancer J Clin 2013; 64: 52–62. [DOI] [PubMed] [Google Scholar]
- Tworoger SS, Eliassen AH, Missmer SA, Baer H, Rich-Edwards J, Michels KB et al. Birthweight and body size throughout life in relation to sex hormones and prolactin concentrations in premenopausal women. Cancer Epidemiol Biomarkers Prev 2006; 15: 2494–2501. [DOI] [PubMed] [Google Scholar]
- Talmor A, Dunphy B. Female obesity and infertility. Best Pract Res Clin Obstet Gynaecol 2015; 29: 498–506. [DOI] [PubMed] [Google Scholar]
- Anderson AD, Solorzano CM, McCartney CR. Childhood obesity and its impact on the development of adolescent PCOS. Semin Reprod Med 2014; 32: 202–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baer HJ, Tworoger SS, Hankinson SE, Willett WC. Body fatness at young ages and risk of breast cancer throughout life. Am J Epidemiol 2010; 171: 1183–1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berkey CS, Frazier AL, Gardner JD, Colditz GA. Adolescence and breast carcinoma risk. Cancer 1999; 85: 2400–2409. [DOI] [PubMed] [Google Scholar]
- Hilakivi-Clarke L, Forsen T, Eriksson JG, Luoto R, Tuomilehto J, Osmond C et al. Tallness and overweight during childhood have opposing effects on breast cancer risk. Br J Cancer 2001; 85: 1680–1684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Su HI, Sammel MD, Freeman EW, Lin H, DeBlasis T, Gracia CR. Body size affects measures of ovarian reserve in late reproductive age women. Menopause 2008; 15: 857–861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sowers MR, McConnell D, Yosef M, Jannausch ML, Harlow SD, Randolph JF Jr. Relating smoking, obesity, insulin resistance, and ovarian biomarker changes to the final menstrual period. Ann N Y Acad Sci 2010; 1204: 95–103. [DOI] [PMC free article] [PubMed] [Google Scholar]