Abstract
Zika virus is an emerging flavivirus that is following the path of dengue and chikungunya. The three Aedes-borne viruses cause simultaneous outbreaks with similar clinical manifestations which represents a diagnostic challenge in ill returning travellers. We report the first Zika virus infection case imported to Switzerland and present a diagnostic algorithm.
Keywords: Chikungunya, dengue, diagnostic algorithm, outbreak, Zika
On 19 November 2015 a 29-year-old woman attended our clinic with a 4-day flulike syndrome after a trip in Colombia from 30 October to 15 November. During her trip home, she developed a feverish feeling with diarrhoea; 24 hours later, she noted a pruritic rash on her trunk. Over the coming days, she presented retro-orbital headache and arthralgia involving her wrists and interphalangeal joints. Physical examination revealed a maculopapular rash on her trunk and limbs. Full blood count was normal. Because of her stay in a region with concurrent arbovirus epidemics, as well as clinical presentation and incubation time, the differential diagnosis included dengue, chikungunya and Zika virus infection. Given the absence of concerning clinical signs, the patient received symptomatic treatment and was followed up as an outpatient. Blood smear, malaria (SD Bioline Malaria Ag P.f/Pan) and dengue rapid tests (SD Bioline Dengue Duo IgG/IgM/NS1Ag) were negative. On serum collected on 20 November (5 days after onset of symptoms), chikungunya IgM/IgG (immunofluorescence commercial test chikungunya (Euroimmun, Germany)) was negative, but real-time Zika reverse transcription (RT) PCR was positive (38 Ct; method developed by National Reference Center for Arboviruses, Service de Santé des Armées, Marseille, France). Urine collected 12 days after symptom onset was positive for Zika by real-time RT-PCR with a higher virus load than in serum collected 7 days before (34 Ct). At the last medical visit, 20 days after symptom onset, she described progressive relief from the arthralgia, and urine real-time RT-PCR was negative. This was the first imported case of Zika infection in Switzerland.
Clinical manifestations of Zika infection are similar to dengue and chikungunya (fever, exanthema, conjunctivitis, retro-orbital headache and arthralgia) [1]. Identification of the virus has specific management implications for clinicians. In the case of dengue, a close follow-up for thrombocytes and haematocrit should be done. In the case of chikungunya, the high prevalence of chronic arthralgia should be discussed. In the presence of Zika, potential sexual and maternal-foetal transmission (with risk of congenital microcephaly) should be presented [2].
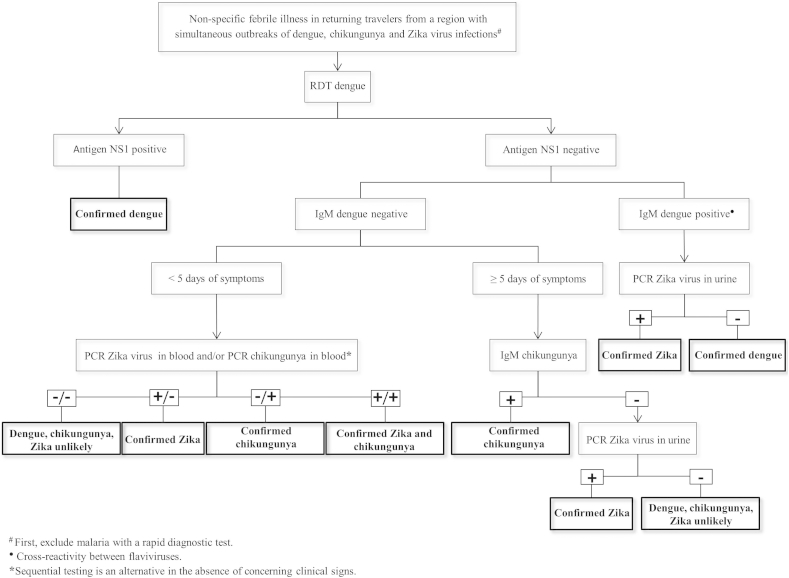
A reliable immunochromatographic rapid diagnostic test makes dengue infection easy to rule out in acutely ill travellers [3]. NS1 antigen is highly specific but in the presence of dengue IgM only, cross-reactivity between the two flaviviruses—dengue and Zika—has been described [4]. Chikungunya can be detected by PCR in blood, and serology by immunofluorescence is expected to be positive after ≥5 days of symptoms. Cross-reactivity between flaviviruses limits the use of serology for Zika diagnosis, which relies on virus RNA detection by PCR in blood, preferably fewer than 5 days after symptom onset (short viraemic period 3–5 days). As illustrated in our case, virus RNA in urine persists for longer periods (15–20 days) and can be useful to confirm infection [5]. Virus can also be detected in saliva during the viraemic period [6]. To support clinicians in their diagnostic workup, we present in Fig. 1 a diagnostic algorithm for travellers with nonspecific febrile illness returning from regions experiencing simultaneous outbreaks of dengue, chikungunya and Zika.
Fig. 1.
Diagnostic algorithm for travellers with nonspecific febrile illness returning from regions experiencing simultaneous outbreaks of dengue, chikungunya and Zika virus infections. RDT, rapid diagnostic test.
Acknowledgements
We thank J. Helfer from the medical outpatient clinic for clinical care. We are grateful to S. De Vallière and B. Genton for their critical reviews. We thank I. Leparc Goffart for the development of the Zika PCR.
Conflict of Interest
None declared.
References
- 1.Cardoso C.W., Paploski I.A., Kikuti M., Rodrigues M.S., Silva M.M., Campos G.S. Outbreak of exanthematous illness associated with Zika, chikungunya, and dengue viruses, Salvador, Brazil. Emerg Infect Dis. 2015;21:2274–2276. doi: 10.3201/eid2112.151167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fauci A.S., Morens D.M. Zika virus in the Americas—yet another arbovirus threat. N Engl J Med. 2016;374:601–604. doi: 10.1056/NEJMp1600297. [DOI] [PubMed] [Google Scholar]
- 3.Fry S.R., Meyer M., Semple M.G., Simmons C.P., Sekaran S.D., Huang J.X. The diagnostic sensitivity of dengue rapid test assays is significantly enhanced by using a combined antigen and antibody testing approach. PLoS Negl Trop Dis. 2011;5:e1199. doi: 10.1371/journal.pntd.0001199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lanciotti R.S., Kosoy O.L., Laven J.J., Velez J.O., Lambert A.J., Johnson A.J. Genetic and serologic properties of Zika virus associated with an epidemic, Yap State, Micronesia, 2007. Emerg Infect Dis. 2008;14:1232–1239. doi: 10.3201/eid1408.080287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gourinat A.C., O'Connor O., Calvez E., Goarant C., Dupont-Rouzeyrol M. Detection of Zika virus in urine. Emerg Infect Dis. 2015;21:84–86. doi: 10.3201/eid2101.140894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Musso D., Roche C., Nhan T.X., Robin E., Teissier A., Cao-Lormeau V.M. Detection of Zika virus in saliva. J Clin Virol. 2015;68:53–55. doi: 10.1016/j.jcv.2015.04.021. [DOI] [PubMed] [Google Scholar]