Abstract
Objective
The objective is to describe the utility of prevention of parent-to-child transmission tracking tool in terms of the in-depth information that it provides for better decision making to improve the services.
Methods
The excel-based tracking tool is initiated by 578 Integrated Counselling and Testing Centre (ICTC) Counsellor and shared with 70 antiretroviral treatment (ART) centres. Between April and September 2014, total of 1118 HIV-infected pregnant women were registered in the tool. The secondary data for this period that is captured in the prevention of parent-to-child transmission tracking tool has been analyzed and presented in this descriptive study.
Results
Of the total 1118 HIV-positive pregnant women, registered in the tool, 760 (68%) were newly detected with HIV infection and 358 (32%) had already been detected before their current pregnancy. In total, 1095 (98%) pregnant women were registered at ART centre out of which 1007 (91%) were initiated on lifelong ART. The average time delay between HIV detection and registration at ART centre was 12 days (n = 844). In this cohort of 1118 pregnant women, 45% delivered live babies, 7% underwent medical termination of pregnancy, 2% were stillbirths and abortions, and 46% were yet to deliver. Only 29 infants were tested for HIV at 6 weeks of age and six were found reactive.
Conclusion
The tracking tool provides in-depth information regarding the pregnant women registered in the program and in the tracking tool. The information throws more light on the characteristics of the registered women and the various services provided to them and highlight key areas where the program has to be improved. The tool is effective for assessing the treatment status of HIV-positive pregnant woman, retention in care and early infant diagnosis of the baby. The tool has identified programmatic bottlenecks component wise such as the need to focus on earlier detection of HIV-positive women during pregnancy, decreasing the time delay between detection and ART registration, and improving the early infant diagnosis.
Keywords: prevention of parent-to-child transmission line list, prevention of parent-to-child transmission tool, prevention of parent-to-child transmission tracking
INTRODUCTION
The state of Maharashtra, with a population of 112 million is one of the six high prevalent states for HIV in India [1]. As of 2014, Maharashtra State AIDS Control Society (MSACS) had 578 stand-alone Integrated Counselling and Testing Centres (SA-ICTC), and 60 antiretroviral treatment (ART) centres in 33 districts of Maharashtra, excluding two districts of Mumbai [2]. In addition there are more than 3000 facility ICTCs (F-ICTCs) located in all 1811 Primary Health centres (PHCs) and remaining as public–private partnership ICTCs [2]. Whereas, the SA-ICTCs offer three HIV tests to confirm HIV status of individuals, the F-ICTCs offer only a screening test for HIV and individuals found reactive in the screening test are then referred to SA-ICTC for confirmation.
Under the national programme, pregnant women are tested for HIV in the public as well as private sector. Pregnant women registered at these facilities are tested for HIV under Opt-out testing strategy and if screened positive by one test are then linked to SA-ICTC for confirmation of HIV status by three tests before initiation of ART.
The estimated annual number of pregnancy for the state of Maharashtra is 2.1 million [3]. MSACS has up scaled HIV testing facilities to the scale that all government health facilities are conducting HIV testing for pregnant women and are reporting to the Department of AIDS Control, New Delhi. The up scaling of testing facilities has facilitated in reaching more than 80% of the estimated pregnant women, in 33 districts of Maharashtra from 42% in 2009–2010 [4]. In 2009–2010, the number of pregnant women tested for HIV were only 899 329 but because of rapid upscale of testing centres the number of pregnant women tested for HIV were 1 927 842 for 2014–2015 [4].
The HIV prevalence in pregnant women has decreased from 0.3% in 2009–2010 to 0.07% in 2014–2015. This is evident from more than 50% decline in the number of HIV-positive pregnant women from 3054 in 2009–2010 to 1385 in 2014–2015 [4].
The ICTCs reported the aggregate numbers of the pregnant women tested and detected with HIV infection to the National programme on a monthly basis in a predefined template. Apart from the aggregated monthly reports there was no other tool to monitor and keep tab of the HIV-positive pregnant women. The aggregated report for the period April 2013–March 2014 is given in Table 1.
Table 1.
Annual prevention of parent-to-child transmission report for Maharashtra for the period April 2013–March 2014. (Source: data from SIMS software, NACO)
| Parameter | Numbers |
| Number of expected pregnancies | 1 419 898 |
| Number of new antenatal registrations | 1 122 219 |
| Number of pregnant women referred by ANM after HIV screening test | 389 514 |
| Number of pregnant women receiving pretest counselling/information | 1 180 822 |
| Number of pregnant women tested for HIV | 1 134 950 |
| Pregnant women diagnosed with HIV infection in the first trimester | 1330 |
| Pregnant women diagnosed with HIV infection in the second trimester | 1097 |
| Pregnant women diagnosed with HIV infection in the third trimester | 828 |
| Number of pregnant women who underwent MTP | 858 |
| Number of pregnant women for whom CD4 count was done and reported | 1576 |
| Number of pregnant women for whom CD4 count was less than 350 | 596 |
| Number of women who were referred for treatment and registered at ART | 1397 |
| Number of spouses of HIV-infected pregnant women tested for HIV | 2050 |
| Number of spouses of HIV-infected pregnant women detected with HIV infection | 1001 |
| Number of mother baby pairs received NVP | 2424 |
| Number of vaginal deliveries among HIV-infected pregnant women | 2084 |
| Number of caesarean section deliveries among HIV-infected pregnant women | 1078 |
| Number of pregnant women delivering in the same hospital | 2945 |
| Number of pregnant women delivering in other government hospital | 470 |
| Number of pregnant women delivering in private hospital | 95 |
| Number of HIV-infected pregnant women delivering at home | 65 |
| Number of stillbirths in HIV-infected pregnant women | 115 |
| Number of infant deaths in HIV-infected pregnant women | 50 |
ANM, auxiliary nurse midwife.
The above data can be disaggregated month wise, institute wise, district wise, and by the numbers reported during antenatal period or direct in labour. Apart from this, there is no disaggregation and further drill-down analysis is not possible. One cannot generate details regarding the profile of the pregnant women who were detected at later stages of pregnancy, those who have not reached ART centre, with low CD4+ counts, delayed for ART registration, initiation and not retained for treatment, and those missed follow-up for early infant diagnosis (EID).
Prior to January 2014, HIV-positive pregnant women linked to ART centre were initiated on ART drugs only when the CD4 count was less than 350 cells/cu mm. Also those pregnant women who had CD4 count higher than 350 were given single-dose nevirapine (NVP) before delivery and for the baby, single dose of NVP was given within 72 h of delivery.
In the month of January 2014, NACO, Government of India, launched the WHO Option B plus regimen to be implemented across the country [3]. In the WHO-prescribed Option B plus, every HIV-positive pregnant woman or breastfeeding woman shall be initiated on lifelong ART irrespective of CD4 count and WHO clinical staging. The ART shall be initiated as soon as the pregnant woman is detected with HIV infection. For the babies born to HIV-positive mothers, syrup NVP is provided for duration of 6 or 12 weeks depending on the duration of ART of the mother during pregnancy [3]. If ART duration of mother during pregnancy is more than 24 weeks, then 6 weeks of NVP is provided and if duration is less than 24 weeks, in breastfeeding mothers, 12 weeks of NVP is provided.
MSACS launched this regimen in the month of February 2014, after ensuring that all field staffs were sufficiently trained and all the logistics were in place. MSACS wanted to document and study the profile of the HIV-infected pregnant women such as their demographic characteristics, time of detection during the pregnancy, baseline CD4 count, delay in initiating ART, retention in ART, HIV infection of the spouse, outcome of the pregnancy, and EID of the baby. To monitor the renewed prevention of parent-to-child transmission (PPTCT) services, MSACS designed and developed a Microsoft excel-based tool. The MSACS aimed to collect such information and identify programmatic gaps so that necessary program improvements can be made.
The study focusses on the utility of the tracking tool in terms of providing such information for understanding the challenges and the gaps in implementing the Option B Plus regimen in Maharashtra and how it could be used for better programme planning for decision-making.
METHODS
The excel-based offline tracking tool has 91 columns which includes all the indicators of PPTCT services from detection of HIV infection in the pregnant mother until the HIV confirmatory testing of the baby at 18 months of age. The tool serves as a line list of all HIV-positive mothers tracking the various services rendered to them and maintaining the longitudinal cohort details, including their babies until the babies completed 18 months.
Every SA-ICTC shall have their own excel sheet with details of all pregnant women registered with their centre. The counsellor at the SA-ICTC shall maintain and update the records of every pregnant women or breastfeeding women as and when the services are provided in their respective centre.
The tool captures the demographic and address details of the pregnant women, details of spouse, HIV testing, order of pregnancy, ART status, including clinical staging and baseline CD4 count, pregnancy outcome, breastfeeding details, and EID details of the baby. For certain key service provision dates were captured wherever possible.
Whenever HIV infection is identified in a pregnant woman or postnatal woman, the details elicited at the ICTC are captured in the register and then later entered in the tool. The tool also includes known HIV-positive women who are currently pregnant. The tool is then shared with the ART centre for the ART counsellor or data manager to enter the ART details of that particular pregnant woman. In this manner the complete service provision details of the pregnant women are updated. The updates shall be on a regular basis. Hence the line list captured each HIV-positive pregnant woman along with her baby as separate longitudinal cohort.
This line list was shared between the 578 testing sites and 70 care and support units in the state. The line list was then compiled and analyzed at the state headquarters. The secondary data from the tracking tool is analyzed for the period April–September 2014 to check for the utility of the data outcomes that the tool provides.
RESULTS
A total of 1118 HIV-positive pregnant women were registered and tracked using the tool between April and September 2014. 760 (68%) pregnant women were newly detected and 358 (32%) pregnant women had already been detected with HIV infection before the current pregnancy. 646 (85%) of the newly detected cases were in WHO Clinical stage I at the time of registration. 669 (60%) of HIV-infected pregnant women were less than 25 years of age and 464 (41%) were primigravida.
General characteristics of the HIV-positive antenatal/postnatal women
Table 2 shows the distribution of registration of pregnant women across the 6-months period. Figure 1 shows the distribution of pregnant women registrations across the different districts of Maharashtra, excluding Mumbai.
Table 2.
Month-wise frequency of registration of antenatal/postnatal women
| Month (2014) | Number of antenatal/postnatal registered |
| April | 212 |
| May | 173 |
| June | 193 |
| July | 196 |
| August | 174 |
| September | 170 |
| Total (n) | 1118 |
FIGURE 1.
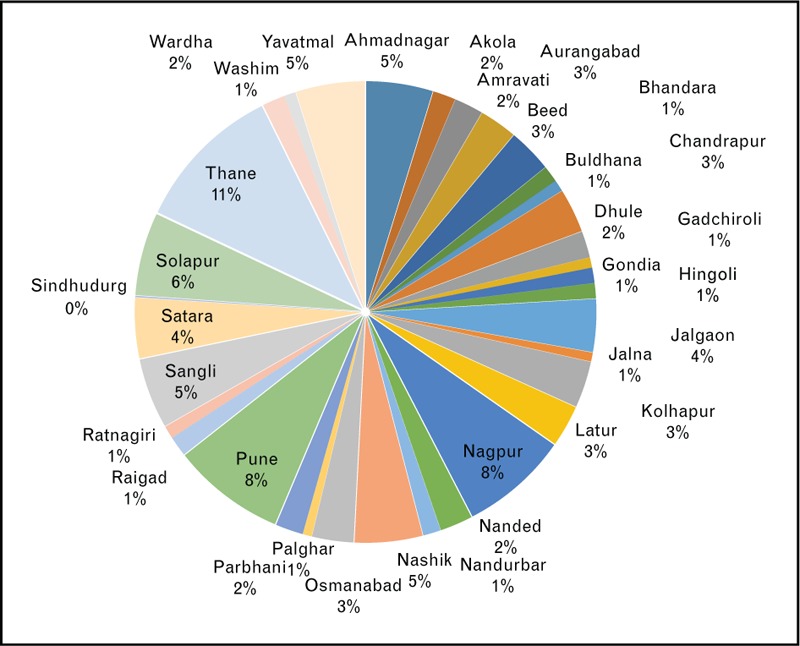
Pie chart showing distribution of HIV-positive antenatal/postnatal women registered.
It is observed from Fig. 1 that 57% of the HIV-positive antenatal cases are registered in the nine districts out of total 34 districts of Maharashtra.
Table 3 shows that 90% of the registered clients are antenatal women, which shows high uptake of HIV testing service during the antenatal period. Nevertheless, there are 7% of direct in labour clients, which needs to be addressed.
Table 3.
Type of clients
| Type of client | Numbers |
| ANC | 1004 |
| Direct in labour | 75 |
| Postdelivery mother | 39 |
| Total (n) | 1118 |
Table 4 shows the age group-wise frequency of the clients. 74% of the clients are in the age group of 20–29. The median gestational age in weeks at the time of registration was 24 weeks. The median gestational age remained unchanged across all age groups (except age group ≥ 40).
Table 4.
Age group-wise classification of antenatal/postnatal mothers
| Age group | Numbers |
| < 20 years | 61 |
| 20–24 | 458 |
| 25–29 | 370 |
| 30–34 | 176 |
| 35–39 | 44 |
| ≥ 40 | 3 |
| Total (n) | 1112 |
As per Table 5, 42% of the pregnant women are primigravida.15% of the primigravida and 43% of clients registered for second order and third order pregnancies are already known positives and have been registered at ART prior to the current pregnancy.
Table 5.
Frequency table by order of pregnancy
| Order of pregnancy | Numbers |
| 1 | 464 |
| 2 | 430 |
| 3 | 150 |
| 4 | 49 |
| 5 | 15 |
| 6 | 3 |
| 7 | 2 |
| Total (n) | 1113 |
Table 6 shows that 45% of the pregnant women were registered only in the third trimester. Of all the pregnant women registered in third trimester, 38% are primigravida and 40% are of second order pregnancy. Among pregnant women registered in third trimester, 16% of primigravida and 40% of second gravida are known positives and have been already registered at ART.
Table 6.
Frequency table showing HIV detection by trimester
| Trimester of HIV detection | Numbers |
| 1st | 219 |
| 2nd | 329 |
| 3rd | 446 |
| Total (n) | 994 |
Table 7 and Table 8 respectively show that 80% of the registered mothers are literate and 80% of the registered women are reported as housewives or homemakers.
Table 7.
Frequency table showing education qualification of the clients
| Education qualification | Numbers |
| Non literate | 227 |
| Primary education | 393 |
| Secondary education | 381 |
| College and above | 111 |
| Total (n) | 1112 |
Table 8.
Occupation-wise frequency table
| Occupation | Numbers |
| Agricultural labourer | 123 |
| Nonagricultural labourer | 52 |
| Domestic worker | 3 |
| Housewife | 888 |
| Skilled worker | 3 |
| Semiskilled worker | 2 |
| Petty business/self-employed | 6 |
| Government/private service | 16 |
| Local transport workers | 1 |
| Hotel staff | 2 |
| Agricultural cultivator/landholder | 5 |
| Unemployed | 2 |
| Others | 7 |
| Total (n) | 1110 |
Table 9 shows that around 55% of antenatal/postnatal women are referred from within government health facilities to the SA-ICTCs and the remaining 45% are referred from nongovernmental facilities.
Table 9.
Frequency table for referral in
| Referred in from | Frequency |
| TI-NGO | 9 |
| NonTI NGO | 80 |
| Maternity homes | 97 |
| RNTCP | 15 |
| Blood bank | 1 |
| Government health facilities | 461 |
| ART centres | 70 |
| STI clinics | 1 |
| PLHIV networks | 3 |
| Private health facilities | 45 |
| Link workers | 4 |
| FICTC government | 20 |
| PPP-ICTC | 19 |
| PHC/subcenter | 27 |
| Other/self-referred | 222 |
| Total (n) | 1074 |
ART, antiretroviral treatment; FICTC, Facility Integrated Counseling and Testing Centre; ICTC, Integrated Counselling and Testing Centres; PHC, Primary Health Center; PLHIV, people living with HIV; PPP, public–private partnership; RNTCP, Revised National Tuberculosis Control Program; STI, sexual transmitted infection; TI-NGO, Targeted Intervention Non-Government Organisation.
Registration at antiretroviral treatment
Out of the total pregnant women detected, 1095 (98%) were registered at ART centre. However, there was a 12-day delay (n = 844) in registering the women at ART after HIV detection. Out of the women registered 644 (61%) women underwent CD4 testing the same day and 712 (70%) of all women on ART were initiated on ART the very next day of registration at the ART centre. A total of 1007 (92%) women were initiated on lifelong ART.
The baseline CD4 count at the time of registration at the ART centre for the current pregnancy was 415 (n = 1019). The median baseline CD4 count was 415. For 214 newly detected antenatal pregnant women who were detected and delivered during this period, ART was given for an average period of 8 weeks during pregnancy.
Outcome of pregnancy
Out of the 1073 recorded outcome events, 47% (500) of the pregnant women had live births, 43% (465) were yet to deliver, 7% had medical termination of pregnancy (MTP) (76), and 2% had still births (23).
Of the 500 live births, 84% (422) were conducted in government health facilities. 84% of the live births were conducted as normal vaginal deliveries. 93% (466) of the babies born were started with either 6 or 12 weeks of syrup NVP.
During this period there were three maternal deaths, in which two pregnant women delivered live births and one stillbirth.
Infant feeding and early diagnosis
Out of 500 live births, 231 (46%) infants were recorded as to have completed 6 weeks of age. Among these 231 infants, 191 infants were given exclusive breastfeeding, 37 were given exclusive replacement feeding, and three were being given mixed feeding.
Only 31 infants were registered at the ICTC centre, out of which 29 infants were tested for HIV.
Total 24 infants were tested using dried blood spot sample and five using whole blood sample for DNA PCR. 16 infants were found nonreactive and six infants were found reactive in the HIV testing; results were awaited for seven infants.
Although it has been recorded that 231 infants had completed 6 weeks of age only 29 were tested for EID. Only one infant had completed 6 months of age and had been subjected to second HIV testing at 6 months for HIV antibody; the result was nonreactive. Three infants reportedly died even before completing 6 weeks of age.
Spouse testing
A total of 399 (36%) spouses of the pregnant women were tested and 280 (70%) were found HIV positive and subsequently 257 (92%) were registered at ART centre. In total, 30% spouse discordancy has been noted among those tested.
CONCLUSION
The information generated from the tool provides valuable insight into the PPTCT program for the reported period. It highlights key programmatic areas of concern and provides sufficient information for action. With respect to tracking and follow-up, the services rendered to the mother and her child has been captured at every stage of the process.
The number of newly detected antenatal cases and known cases can be used for the purpose of trend analysis over a period of time, to check whether newly detected cases are decreasing or increasing year after year. Since 60% of the pregnant women are less than 25 years of age, counselling services have to be strengthened and focused more on lifelong ART, safe sexual practice, and family planning measures (considering that 59% are multigravida).
It is seen that an average of 186 cases are detected every month (range minimum 170–maximum 212) and hence, the ART centres can plan for the drug logistics accordingly and also that the ART centres can expect to register roughly 126 newly detected pregnant women every month, since 68% of all HIV-positive pregnant women are newly detected.
Improving testing coverage among all antenatal women in nine districts namely Thane, Pune, Nagpur, Solapur, Yavatmal, Ahmednagar, Sangli, Nashik, and Satara shall yield higher number of positive pregnant women in quick time, since 57% of positive pregnant women are reported in these nine districts only. Likewise, the registrations for treatment shall also be concentrated in the ART centres in these nine districts.
Total 114 of registered pregnant women have presented directly in labour or during the post natal period in the 6-month period, which highlights that they have been missed HIV detection throughout the pregnancy period. The HIV testing coverage has to be increased so that all pregnant women are screened for HIV in early part of pregnancy. Detecting HIV infection in early part of pregnancy is essential since the pregnant mother and baby shall benefit with the ART (minimum 24 weeks of ART during pregnancy is indicated for decreasing viral load sufficiently).
We observe that 45% of the pregnant women are registered only in the third trimester and that too 40% in this group are of second order pregnancy, out of which 40% are already known positive cases and have already been registered at the ART centres. Even though the pregnant women are registered at the ART centre and receiving ART regularly, they are encouraged to get registered at the ICTC for the current pregnancy. The responsibility of registration, treatment, and follow-up of HIV-infected pregnant women until delivery and EID of the baby is vested with the ICTC counsellor. The ART centres should ensure that women under their care who become pregnant should immediately get registered at an ICTC centre which is convenient for the women to visit.
It is observed that 20% of the registered pregnant women are nonliterate, hence the program should ensure that audio visual messages regarding HIV screening and its benefits apart from routine display charts/posters are repeatedly telecasted at the antenatal clinics and ICTC centres.
It is positive to note that 98% of the pregnant women are registered at the ART centre, however, it is also noted that there is a 12-day delay in reaching the ART centre. As it is beneficial for both the mother and baby that she receives ART of 24 weeks during pregnancy and given that 22% of the pregnant women only are detected in the first trimester, nearly two weeks delay in reaching ART centre will deprive majority of the pregnant women the benefit of early initiation of ART.
Again it is noted that the average period of ART given to the newly detected antenatal women is only 8 weeks. Hence more emphasis has to be given on early detection and early initiation of ART.
Total 9% of the women who had either undergone MTP or had stillbirths it has to be ensured that they still continue on ART. As against 231 infants eligible for dried blood spot testing at 6 weeks only 29 have been tested. The program has sufficient details of the mothers whose babies have not undergone EID testing, that they can track the mother and baby and provide necessary services to them. Regular follow-up of the babies and their HIV status confirmation at 18 months shall provide excellent information and insights into the effects of treatment upon HIV transmission.
Only 399 spouses of the registered pregnant women were tested, which resulted detection of 280 (70%) spouses with HIV infection. Increasing the HIV testing of spouses of all the registered pregnant women shall increase the detection of HIV infection in the general population.
As discussed above, the outputs from the tracking tool provides specific information to the program managers to identify programmatic gaps such as delays in HIV testing, detection and linkage to ART registration, and subsequent initiation of lifelong ART; this information shall enable them to manage the program in a more effective manner.
In this tool, the analysis can also be done for a particular institution or a district or for a specific time period. Timely identification of the gaps and planning necessary interventions can help the program reach its ultimate goal of PPTCT of HIV infection.
The PPTCT tracking tool has demonstrated its utility in terms of providing valuable program information for action and it definitely provides much more information when compared with the aggregated monthly reports.
FUTURE RECOMMENDATIONS
The current tool has some operational challenges; has to be managed manually, in terms of sharing the file between ICTC and ART for data capture and analysis, which is an effort consuming process. The current tool usage and process is person dependant for the timely update and completeness of the data.
Such tools can be developed and provided as web-based software, so that the data entry, sharing and analysis can be effortless and time saving.
Acknowledgements
R.S.G., A.H., T.M., K.Y., conceived and designed the individual tracking tool. A.H., T.M. and K.Y. collected and analyzed data. P.K.A.B., T.M., and K.Y. contributed to analysis. P.K.A.B. wrote first draft of the analysis. A.H., T.M., K.Y., N.S., S.B., and D.C.S.R. gave significant intellectual contribution to the article.
We thank all the ICTC, DAPCU, ART, and SACS staff of Maharashtra State AIDS Control Society for their sincerity and hard work in facilitating this study. A special acknowledgement to all the ICTC Counsellors who facilitated this study.
∗The authors alone are responsible for the views expressed in this article and they do not necessarily represent the decisions, policy or views of the WHO.
Financial support and sponsorship
None.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.“Technical Report India HIV Estimates-2012,” NACO, 2012. [Google Scholar]
- 2.“Annual Report 2013–14 NACO,” Department of AIDS Control, Ministry of Health and Family Welfare, Government of India, New Delhi, 2014. [Google Scholar]
- 3.“National Strategic Plan Multi Drug ARV for prevention of parent to child transmission of HIV (PPTCT) under National AIDS control program in India,” Department of AIDS Control, Ministry of Health and Family welfare, Government of India, New Delhi, 2013. [Google Scholar]
- 4.“Mahasacs,” [Online]. Available: http://mahasacs.org/index.php?option=com_content%26view=article%26id=88%26Itemid=181%26lang=en [Accessed 7 August 2015]


