Abstract
Introduction
The study described the effectiveness of a voucher scheme to access sexual and reproductive health and HIV services among young MSM and transgender people aged 15–24 years in Dhaka, Bangladesh, a country with HIV prevalence of less than 0.1%.
Methods
Descriptive and analytical methods were used to assess the net effects of biodemographic factors of the respondents on the voucher scheme. Effectiveness of the scheme was contextualized as target population coverage, and turnaround time of voucher redemption to access services.
Results and discussion
A total of 210 (87.9%) out of the 239 vouchers distributed were redeemed. The mean age of the identified young people was 19.6 years (SD = +2.6 years). The coverage of the scheme against the target population of 200 young MSM and 936 young transgender people was 88% (n = 175) and 4% (n = 35) respectively, with P < 0.001. The median turnaround time for voucher redemption was 7 days. The predictors of voucher turnaround time were age, education, and population group (P < 0.001). HIV testing and counselling was accessed by 160 (76%) respondents, one was positive and linked to antiretroviral treatment and 110 (52%) were diagnosed and treated for sexually transmitted infections.
Conclusion
The voucher scheme was effective in linking young MSM with sexual and reproductive health and HIV services in Dhaka, Bangladesh. The findings are consistent with the low HIV prevalence in the country. The scheme is, however, not optimal for linking young transgender people with services.
Keywords: Bangladesh, peer link associates, respondent driven approach, voucher scheme, youngMSM, young transgender people
INTRODUCTION
Young people aged 15–24 years constitute 16% of the world's population [1], and yet they represent 34% of all new HIV infections among adults [2]. In 2013, there were about four million young people aged 15–24 years living with HIV, 29% of whom are adolescents aged 15–19 years [3]. Key populations for the HIV epidemic have been defined as groups who, because of specific high-risk behaviours, are at increased risk of HIV irrespective of epidemic type or local context [4]. They include men who have sex with men (MSM), people who inject drugs, people in prisons and other closed settings, people who sell sex, and transgender people. Young people who belong to one or more of these key populations, or who engage in activities associated with these populations are made especially vulnerable to HIV by widespread discrimination, stigma and violence, combined with the particular vulnerabilities of youth, power imbalances in relationships, and sometimes, alienation from family and friends [5–7].
In 2012, young people aged 10–24 years in key population for the HIV epidemic (young key populations) were estimated at 50 000 in Bangladesh [8], a significant proportion being adolescents aged 10–18 years (Table 1). The estimate was based on the mapping of young people who inject drugs, young people who sell sex, young MSM, and young transgender people in urban and periurban locations in Bangladesh. According to the national mapping, there were an estimated 333 (6%) young MSM and 1 560 (26%) young transgender people of the total national estimates of young MSM and transgender people in Dhaka, the capital city [8].
Table 1.
Distribution of young key population at risk of HIV infection in Bangladesh [8]
| Young key population at risk of HIV infection | Estimates aged 10–24 years | Estimates aged 10–18 years | ||
| National | Dhaka | National | Dhaka | |
| Young MSM | 5 820 | 333 | 1909 | 122 |
| Young people who inject drugs | 2097 | 648 | 208 | 164 |
| Young people who sell sex | 31 101 | 9 660 | 10 263 | 3168 |
| Young transgender people | 6096 | 1560 | 1207 | 399 |
Bangladesh is one of the countries in Asia and the Pacific with 25% increase in new HIV cases reported over the period of 2001 and 2011 [9]. The HIV epidemic in Bangladesh is low, but concentrated among key population groups [10]. Over the nine rounds of HIV surveillance in the country [10], the HIV prevalence in the general population remained stable at <0.1%, but increased among key populations aged 18–50 years from 0.3% in 2000 to 0.7% in 2011, with a peak at 0.9% in 2006 [10]. In Dhaka, the HIV prevalence among adult MSM and transgender people were estimated at 0.7 [11] and 1.0% [10], respectively. Although age-specific HIV prevalence among young MSM and transgender people aged 15–24 years in Bangladesh are unknown, the reported cases of multiple sexual partnerships, inconsistent condom use, and structural vulnerabilities like sexual violence and limited access to healthcare services among these younger populations increases their risk for HIV infection [8]. The Government of Bangladesh has, however, prioritized data improvement, policy reform, and programme actions for adolescents and young people in key populations in the national HIV programme [12,13].
Intervention description
The study described the effectiveness of the use of vouchers to improve access and uptake of sexual and reproductive health (SRH) and HIV services by young MSM and transgender people aged 15–24 years in Dhaka, Bangladesh. A voucher scheme facilitated by peer link associates was implemented between May 2014 and April 2015 to identify and link 60% of the estimated population of young MSM and transgender people in Dhaka (Table 1) with SRH and HIV services as part of the ‘HIM’ initiative. As such, the voucher scheme was targeted at identifying and linking 200 young MSM and 936 young transgender people aged 15–24 with services in Dhaka, Bangladesh.
The ‘HIM’ initiative involved the establishment of a youth centre – ‘HIM centre’. The centre provides dedicated ‘space’ to young MSM and transgender people to discuss and air their views and feelings. The initiative provides opportunities for young MSM and transgender people to meet in an empathetic environment. The initiative engaged three young people from the young MSM and transgender people community in Dhaka – ‘peer link associates’ as peer educators for the duration of the implementation. The ‘peer link associates’ mobilized their peer through physical networking and social media. At the ‘HIM centre’, young MSM and transgender people are empowered with information, life skills, and offered support on sexuality, health, and human rights issues to practice safer sex and reduce their vulnerability to HIV and AIDS.
The vouchers were distributed through ‘modified respondent driven’ approach informed by respondent-driven sampling (RDS). RDS is one of the network-based recruitment strategies used with hard-to-reach population [14]. Similar to other chain-referral sampling methods, RDS starts with a small number of peers (called seeds) and expands through successive ‘waves’ of peer recruitment [14]. Earlier studies had applied RDS to map sexual networks and assess service uptake among young MSM [15,16]. The three peer link associates (seeds) were engaged by the ‘HIM’ centre as seeds to expand the network in successive waves. The seeds recruited first wave-respondents, first-wave respondents recruited second-wave respondents, and this process continued throughout implementation [14]. The identified peers (respondents) were briefed about the voucher scheme and encouraged to distribute the vouchers to other peers. Both the peer link associates (seeds) and the identified peers (respondents) were allowed reentry throughout the duration of the project once they ran out of vouchers.
The use of vouchers as incentives to encourage uptake of services is documented [17–19]. In this study, the incentives accessible through use of the voucher were free access to HIV and SRH services, internet browsing, life skills education and referral healthcare services in the ‘HIM’ centre. An increase in the identification of new cases of HIV with high rate of linkage to care through a voucher scheme was reported among African-American MSM in Los Angeles [17]. A randomized clinical trial [18] among HIV-positive drug users in Chennai, India reported an association between voucher scheme and higher likelihood (P = 0.002) of visiting antiretroviral treatment (ART) centres. The same randomized clinical trial reported a higher proportion of drug users who received voucher incentives compared to control group initiated on ART (risk ratio = 2.33) and made more frequent visits (P = 0.005) to ART centres. In the multicountry review of family planning and SRH services in Asia and Africa [19], service uptake and client satisfaction were reported to increase following implementation of vouchers. There were, however, mixed findings regarding cost efficiency. Whereas the unit cost per client reduced due in part to increase in service uptake, the average cost of service delivery increased in some of the programmes [19].
METHODS
This is a cross-sectional survey of young MSM and transgender people who responded to the voucher scheme as part of the ‘HIM’ initiative in Dhaka, Bangladesh. Data were extracted from the Microsoft Excel based monitoring system established for the ‘HIM’ initiative. Effectiveness of the voucher scheme was contextualized into proportion of the target population of young MSM and transgender people identified and linked to services, and the turnaround time of voucher redemption to access SRH and HIV services. This study did not include cost analysis.
Bivariate and multivariate analyses were conducted to ascertain the association and net effects of the key independent variables on the dependent variable when the selected biodemographic characteristics were controlled. Bivariate analyses were used for identifying patterns of associations and levels of significance (P < 0.05) of such associations. In addition, we examined the association between turnaround time of voucher redemption and biodemographic variables using a binary logistic regression. The binary logistic regression models for the redemption of voucher within 7 days (against redemption of voucher 8 days or more) and the redemption of voucher within 14 days (against redemption of voucher 15 days or more) were fitted. A P value less than or equal to 0.05 was considered as significant. In the two models, age, location of social network, population group, education attainment, and occupation were estimated as categorical independent variables (Table 2). Logistic regression coefficient (β) and odds ratio were used in the determination of the association between the exposure variables (predictors) and the outcome variables in a logistic regression model [20,21]. Maximum likelihood estimation was applied. The analysis was conducted with STATA/SE 12.0 [22].
Table 2.
Classification of variables in bivariate and multivariate analysis and their respective values
| Variable | Value |
| Outcome variable | |
| Voucher turnaround time (time series 1) | 0 = Redeemed voucher in 8 days or more |
| 1 = Redeemed voucher within 7 days | |
| Voucher turnaround time (time series 2) | 0 = Redeemed voucher in 15 days or more |
| 1 = Redeemed voucher within 14 days | |
| Exposure variable | |
| Location of social network | 1 = Areas within and around tertiary institutions |
| 2 = Open parks and recreation centres | |
| 3 = Metropolitan areas | |
| 4 = Resource centres | |
| Age | 1 = Adolescents aged 15–19 years |
| 0 = Young people aged 20–24 years | |
| Population group | 1 = YoungMSM |
| 2 = Young transgender people (young transgender people) | |
| Highest education attainment | 1 = None/primary education |
| 2 = Secondary education | |
| 3 = Postsecondary education | |
| Occupation | 0 = Nonstudent |
| 1 = Students | |
Ethical considerations
This study was undertaken as part of the implementation of the ‘HIM’ initiative approved by the National AIDS/STD Programme (NASP) of the Ministry of Health and Family Welfare in Bangladesh (Reference # DGHS/AIDS/STD/2012/1518 dated 2 February 2013). Ethical considerations [23,24] relating to the right to full disclosure and informed consent were maintained as the young people were briefed on the voucher scheme. In addition, the vouchers included standard information about available services at the ‘HIM’ centre, and directions to the centre. Participants had the right to refuse to participate in the voucher scheme. Although the vouchers included tracking numbers, the identity of the respondents was not linked to the vouchers and services – preserving the right to anonymity. The right to confidentiality was maintained by not linking collected information to the respondents.
RESULTS AND DISCUSSION
A total of 210 (88%) out of the 239 vouchers distributed were redeemed. The vouchers were distributed over four waves. Among the 210 redeemed vouchers, 105 (50%) vouchers were distributed in the first wave, 86 (41%) in the second wave, 17 (8%) in the third wave, and only 2 (1%) in the fourth wave. The turnaround time of the redeemed vouchers was asymmetrical and right-skewed (coefficient of skewness = 2.049), and more spread out than normal distribution (coefficient of kurtosis = 6.340). The median turnaround time of the redeemed vouchers was 7 days, and ranged from same day return to 180 days (Fig. 1). Among the 210 redeemed vouchers, 100 (47%) were redeemed within 7 days (the median) and a cumulative 141 (67%) vouchers were redeemed within 14 days (twice the median).
FIGURE 1.
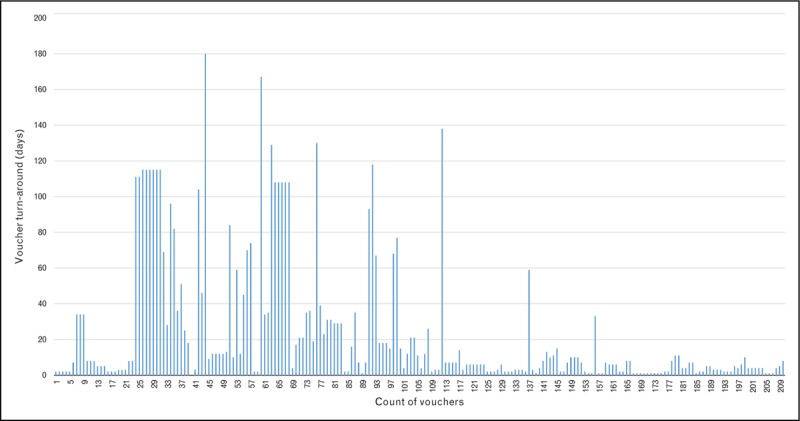
Distribution of turnaround time for voucher redemption to access sexual and reproductive health and HIV services among respondents (N = 210).
Biodemographic characteristics of respondents
The biodemographic characteristics of the respondents who redeemed the vouchers are presented in Table 3. Among the 210 respondents, 121 (58%) were adolescents aged 15–19 years and 89 (42%) were young people aged 20–24 years. The mean age of the respondents was 19.6 years, (SD = + 2.6 years). Earlier mapping of young MSM and transgender people in Dhaka, Bangladesh had, however, reported a much lower proportion of adolescents aged 10–18 years [8]. The respondents were mostly students – 54% (N = 210), and had attained postsecondary education 46% (N = 210). The occupation of 9% (N = 210) of the respondents was ‘badhai’ – traditional entertainment provided by transgender people in marriage and birth ceremonies in Bangladesh [25]. Contrary to expectation, only 35 (17%) of the identified respondents were young transgender people when compared to the higher population estimate of young transgender people relative to young MSM in Dhaka (Table 1).
Table 3.
Biodemographic characteristics of the respondents (N = 210)
| Characteristics | Distribution | Percentage |
| Age | ||
| Adolescents aged 15–19 years | 121 | 57.6 |
| Young people aged 20–24 years | 89 | 42.4 |
| Highest education level | ||
| None/Primary education | 52 | 24.8 |
| Secondary education | 61 | 29.0 |
| Postsecondary education | 97 | 46.2 |
| Population group | ||
| Young MSM | 175 | 83.3 |
| Young transgender people | 35 | 16.7 |
| Occupation | ||
| Students | 113 | 53.8 |
| Job/service | 55 | 26.2 |
| Sex work | 13 | 6.2 |
| Business | 5 | 2.4 |
| ‘Badhai’ (traditional entertainer at marriage/birth ceremonies) | 19 | 9.0 |
| Others | 5 | 2.4 |
| Location of social network | ||
| Areas within and around tertiary institutions | 46 | 21.9 |
| Open parks and recreation centres | 114 | 54.3 |
| Municipal areas | 30 | 14.3 |
| Resource centres | 20 | 9.5 |
The locations of the social networks (Table 3) of the identified respondents in this study were similar to findings from an earlier study in Dhaka, Bangladesh [8]. Other studies have included clubs, sex parties, bathhouses, and anonymous online chat sites in the investigation of venue where MSM meet their sex partners [26–28]. Venue of social networks among hidden population groups like young MSM and transgender people is important because they represent a physical space where the population can be identified, they are potential sites to target interventions, and there may be aspect of the locations themselves that contribute to HIV risk [26,27]. The findings of this study suggest that open park and recreation centres (54%, N = 210), and areas within and around tertiary institutions (22%, N = 210) were the locations to target interventions for young MSM and transgender people in Dhaka, Bangladesh.
Description of voucher scheme among respondents
The coverage of the voucher scheme against the target population of young MSM and young transgender people differs (Table 4). In this study, 88 and 4% of the target population of 200 young MSM and 936 young transgender people respectively, were identified, a difference that was statistically significant (P ≤ 0.001). The low proportion of identified young transgender people might be a reflection of the organization of the social network of transgender people. In Bangladesh, most transgender people belong to a cultural group known as ‘hijra’, and are organized around a ‘guru’ (teacher), to whom several ‘chela’ (disciples) are connected [11,29]. The fact that the target population of young transgender people in this study were mostly ‘chela’, and no specific action was directed at the ‘guru’ (who is influential) might explain the findings. Additional studies are, however, required to explain the utility of voucher schemes in the identification of young transgender people in Dhaka, Bangladesh.
Table 4.
Cross tabulation of the target population and coverage of identified respondents
| Target population group | Coverage (%) | |
| Identified | Not identified | |
| Young MSM (n = 200) | 87.6 | 12.4 |
| Young transgender people (n = 936) | 3.7 | 96.3 |
| χ2 | 768.113 | |
| P value | <0.001 | |
Among the identified respondents, however, the turnaround time to redeem the vouchers for SRH and HIV services in the ‘HIM centre’ varied with the different biodemographic characteristics included in this study (Table 5).
Table 5.
Cross tabulation of voucher turnaround time and selected social characteristics of respondentsa
| Voucher turnaround time | Age (%) | Highest education level (%) | Population group (%) | Occupation (%) | Location of social network (%) | ||||||||
| 15–19 years (n = 89) | 20–24 years (n = 121) | None/Pry. (n = 52) | Sec. (n = 61) | Postsec. (n = 97) | Young MSM (n = 175) | Young transgender people (n = 35) | Nonstudents (n = 97) | Students (n = 113) | Areas within and around tertiary institutions (n = 46) | Open parks and recreation centres (n = 114) | Municipal areas (n = 30) | Resource centres (n = 20) | |
| Within 7 days | 42.2 | 66.3 | 65.4 | 44.3 | 50.5 | 53.1 | 48.6 | 55.7 | 49.6 | 56.5 | 50.8 | 56.7 | 45.0 |
| 8 days or more | 57.9 | 33.7 | 34.6 | 55.7 | 49.5 | 46.9 | 51.4 | 44.3 | 50.4 | 43.5 | 49.1 | 43.3 | 55.0 |
| χ2 | 11.984 | 5.272 | 0.244 | 0.782 | 1.077 | ||||||||
| P value | 0.001 | 0.072 | 0.621 | 0.377 | 0.783 | ||||||||
| Within 14 days | 58.7 | 78.7 | 75.0 | 63.9 | 65.0 | 69.1 | 57.1 | 67.0 | 67.3 | 71.7 | 70.2 | 56.7 | 55.0 |
| 15 days or more | 41.3 | 21.4 | 25.0 | 36.1 | 35.1 | 30.9 | 42.9 | 33.0 | 32.7 | 28.3 | 29.8 | 43.3 | 45.0 |
| χ2 | 9.274 | 1.952 | 1.904 | 0.001 | 3.745 | ||||||||
| P value | 0.002 | 0.377 | 0.168 | 0.970 | 0.290 | ||||||||
aSum did not add up to 100% because of rounding.
The SRH and HIV needs of adolescents and young people differ, and specific measure is required to make services adolescent friendly [30]. In this study, the difference in voucher turnaround time within 7 days (P = 0.001) and 14 days (P = 0.002) among respondents of different age groups, that is, adolescents and young people were statistically significant. At 7 days and 14 days, a higher proportion of young people (aged 20–24 years) redeemed their vouchers when compared to adolescents aged 15–19 years (Table 5). This finding is consistent with other voucher schemes [31,32] where a higher proportion of young people compared to adolescents accessed services.
Higher education attainment is associated with low HIV risk [33] and HIV infection [34]; and subsequent utilization of services. The proportion of respondents in this study who redeemed the vouchers within 7 days and 14 days were higher among those with no or primary level of education, when compared to respondents with higher education levels (Table 5). This finding is contrary to expectation as education attainment, especially among young men in Bangladesh was high [35]. In 2011, only one in four men and about one in three women have never attended school [35]. The voucher turnaround time at 7 days and 14 days among respondents with different levels of education attainments was, however, not statistically significant (Table 5).
About half of the young MSM and transgender people in this study redeemed their vouchers within 7 days. At 14 days, however, a higher proportion of young MSM compared to young transgender people redeemed their vouchers (Table 5). An earlier study among MSM aged 18 years and older indicated the use of vouchers increased uptake of HIV self-testing [17]. Although a higher proportion of respondents in this study were young MSM, the findings, however, indicated that population group did not influence voucher turnaround time (Table 5).
The proportion of students and nonstudents (others involved in business, service industry, and sex work) that redeemed the vouchers within 14 days was at par both (Table 5). A slightly higher proportion of nonstudents, however, redeemed their voucher within 7 days when compared to students that redeemed their vouchers. This finding could be related to the access of non-students to more disposable income when compared to students. The occupation of the respondents, however, did not influence the turnaround time to redeem vouchers (Table 5).
The importance of the location of social networks among hidden populations for population identification, vulnerability to HIV and delivery of interventions was discussed above. Across all the social networks of respondents in this study, a higher proportion redeemed the vouchers within 14 days (Table 5). Voucher redemption within 7 days, however, varied. Unlike respondents in other social locations, a lower proportion of respondents identified in resource centres redeemed their vouchers within 7 days (Table 5). Overall, there is no association between the location of social networks and voucher turnaround time among respondents in this study (Table 5).
Predictors of voucher turnaround time
The independent effects (bivariate analysis) of the biodemographic characteristics of the respondents included in this study on the turnaround time for voucher redemption to access SRH and HIV services varied when analysed, controlling for the effects of other independent variables in the logistic regression (Table 6). In the logistic regression, age, education, and population group were the predictors of the turnaround time to redeem vouchers by respondents in this study. The considerations to redeem vouchers for SRH and HIV services in settings like Dhaka, Bangladesh where there are social exclusion of young MSM and transgender people [25] are likely influenced by HIV risk perception, knowledge of services and the support to access the services. Consistent with the bivariate analysis, adolescent respondents (aged 15–19) were less likely to redeem the vouchers when compared to those aged 20–24 years (reference group) in the logistic regression. Respondents who had attained higher levels of education, however, had a lower likelihood of returning the vouchers when compared with those with no or primary education (reference group). Similar patterns of voucher redemption in respondents with higher education levels were recorded among poor urban female adolescents in Nicaragua [32]. The pattern of the predictive effect of education attainment on the turnaround time for voucher redemption in this study is, however, contrary to expectation in Dhaka, Bangladesh where education attainment is high [35]. The low likelihood of respondents with higher levels of education to redeem vouchers for SRH and HIV services in Dhaka, Bangladesh require further exploration. In line with the low enrolment of young transgender people in this study, respondents who were young transgender people had a lower likelihood to redeem the vouchers when compared to young MSM (reference group).
Table 6.
Predictors of voucher turnaround time among young MSM and transgenders in Dhaka, Bangladesh
| Social Characteristics | Within 7 days | Within 14 days | ||
| Odds ratio exp β (95% CI) | P value | Odds ratio exp β (95% CI) | P value | |
| Age | ||||
| 20–24 years (rc) | ||||
| 15–19 years | 0.37 (0.20–0.67) | 0.001 | 0.33 (0.17–0.64) | 0.001 |
| Highest education level | ||||
| None/primary education (rc) | ||||
| Secondary education | 0.42 (0.17–1.04) | 0.059 | 0.44 (0.16–1.19) | 0.105 |
| Postsecondary education | 0.34 (0.12–0.99) | 0.047 | 0.20 (0.06–0.65) | 0.008 |
| Population group | ||||
| Young MSM (rc) | ||||
| Young transgender people | 0.18 (0.03–0.97) | 0.047 | 0.44 (0.09–2.04) | 0.291 |
| Occupation | ||||
| Nonstudents (rc) | ||||
| Students | 1.16 (0.50–2.71) | 0.732 | 1.85 (0.73–4.66) | 0.196 |
| Location of social network | ||||
| Areas within and around tertiary institutions (rc) | ||||
| Open parks and recreation centres | 0.82 (0.39–1.73) | 0.606 | 0.89 (0.39–2.01) | 0.777 |
| Municipal areas | 2.64 (0.40–17.38) | 0.313 | 0.53 (0.90–3.09) | 0.477 |
| Resource centres | 0.67 (0.22–2.07) | 0.483 | 0.42 (0.13–1.37) | 0.152 |
| Constant | 5.24 (1.83–15.00) | 0.002 | 12.05 (3.57–40.73) | 0.00 |
| Total number of cases | 210 | 210 | ||
| Model χ2 (df = 8) | 21.47 | 21.85 | ||
| Model significance (P value) | 0.006 | 0.0052 | ||
| log likelihood | −134.588 | −122.041 | ||
CI, confidence interval; rc, reference category.
Uptake of HIV and sexual and reproductive health services
Among the 210 respondents who redeemed the vouchers, 186 (89%) accessed the telephone-based help line counselling services and 160 (76%) attended life skills-based HIV prevention education in the ‘HIM’ centre. The help line counselling service provided respondents with information about services available at the ‘HIM’ centre, and addressed concerns and questions raised by the callers. The majority of the 186 callers were young MSM (97%) and aged 20–24 years (72%). The 160 respondents who attended life skills and psychosocial skills education were mostly young MSM (88%) and adolescents aged 15–19 years (77%).
Clinical record at the ‘HIM’ centre indicated that 110 (52%) of the respondents who redeemed the vouchers were treated for sexually transmitted infections (STI) and 160 (76%) accessed HIV testing and counselling services. The majority of the 110 respondents who were treated for STI were young MSM (91%), and adolescents aged 15–19 years (57%). Similarly, the 160 respondents who accessed HIV testing and counselling were mostly young MSM (83%), and adolescents aged 15–19 years (56%). The higher proportion of adolescents (aged 15–19 years) who were treated for STI and took the HIV test indicate the need to focus attention on gay and bisexual adolescent boys in Dhaka, Bangladesh. Consistent with the low HIV prevalence in Bangladesh [10], only one respondent was positive for HIV, and the identified case was linked with the national ART in Bangladesh.
Limitation of the study
Several limitations should be considered when interpreting the results from this study. The cross-sectional nature of the data does not allow for causal relationships to be established [36]. The composition of the social networks in the different location could have changed over the 12 month duration of the study. The ‘modified’ RDS used do not provide the basis for valid generalization of findings to the study population [14]. Despite these limitations, the bivariate and multivariate analysis in this study indicated the effect of the biodemographic characteristics of the respondents on the voucher scheme. In the views of the authors, the study findings are contributions to approaches to improve access of young MSM and transgender people to HIV and SRH services in South Asia.
CONCLUSION
The voucher scheme is effective in linking young MSM with SRH and HIV services in Dhaka, Bangladesh. Among respondents who redeemed the vouchers, age, education, and population group were predictors of the turnaround time to redeem vouchers for SRH and HIV services. In addition, a high proportion of the respondents who sought counselling services in the ‘HIM Centre’ utilized both HIV testing and STI treatment. The findings of this study further support the low HIV prevalence in Bangladesh. The voucher scheme as currently implemented, however, does not work among young transgender people. Defining specific roles for ‘guru’ (teachers) – whom young transgender people are linked and integrating the voucher scheme into social networks led by the ‘guru’ are options to be considered to improve uptake by young transgender people. In the alternative, another approach may be required to effectively link young transgender people with HIV and SRH services in Dhaka, Bangladesh.
Acknowledgements
The ‘HIM’ initiative was developed by Bandhu Social Welfare Society (BSWS) with technical support from UNICEF Bangladesh. The funding for the project was provided by UNICEF Bangladesh as part of the Government of Bangladesh – UNICEF country programme 2012–2016. The National AIDS/STD Programme (NASP) of the Ministry of Health and Family Welfare, Bangladesh provided oversight function to the implementation of the initiative.
T.O.O. was responsible for designing the initiative and preparation of the manuscript. S.A. codesigned the initiative and managed implementation. F.A. supported implementation. M.T. developed the monitoring tool for the initiative and monitored implementation. Z.U. provided technical assistance for implementation. A.R. provided technical oversight for implementation as part of the national HIV programme. K.A.O. was responsible for data analysis. All the authors reviewed the manuscripts.
The views expressed in this paper do not represent the view of the UNICEF, BSWS, NASP nor John Snow Inc., but rather that of the authors of this paper.
Financial support and sponsorship
The study was funded by UNICEF Bangladesh as part of the Government of Bangladesh – UNICEF Country Programme 2012–2016. Bandhu Social Welfare Society was the implementing partner.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Mona Tazreen is a volunteer with United Nations Children's Fund.
Tajudeen O. Oyewale and Ziya Uddin are staff of United Nations Children's Fund.
Kola A. Oyediran is a staff of John Snow Inc.
REFERENCES
- 1.Population division of the department of economic and social affairs of the United Nations secretariat. World population prospects. 2015. http://esa.un.org/unpd/wpp/Publications/Files/Key_Findings_WPP_2015.pdf [Accessed 9 August 2015] [Google Scholar]
- 2.Joint United Nations Programme on HIV/AIDS (UNAIDS). UNAIDS Strategy for 2016–2020. Geneva: UNAIDS; 2015. http://www.unaidsstrategy2021.org/wp-content/uploads/2015/08/UNAIDS-Strategy-2016-2021_Draft-for-review_3-August.pdf [Accessed 9 August 2015] [Google Scholar]
- 3.Joint United Nations Programme on HIV/AIDS (UNAIDS). The gap report. Geneva: UNAIDS; 2014. [PubMed] [Google Scholar]
- 4.World Health Organization (WHO). Consolidated guidelines on HIV prevention, diagnosis, treatment and care for key populations. Geneva: WHO; 2014. [PubMed] [Google Scholar]
- 5.Delany-Moretlw S, Cowan FM, Busza J, et al. Providing comprehensive health services for young key populations: needs, barriers and gaps. J Int AIDS Soc 2015; 18 (Suppl 1):29–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baggaley R, Armstrong A, Dodd Z, et al. Young key populations and HIV: a special emphasis and consideration in the new WHO consolidated guidelines on HIV prevention, diagnosis, treatment and care for key populations. J Int AIDS Soc 2015; 18 (Suppl 1):85–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stults CB, Javdani S, Greenbaum CA, et al. Intimate partner violence and substance use risk among young men who have sex with men: The P18 cohort study. Drug Alcohol Depend 2015; 154:54–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.National AIDS/STD Programme (NASP) Directorate General of Health Services, Ministry of Health and Family Welfare, Bangladesh. Mapping and behavioral study of most at risk adolescents to HIV in specfic urban/semi urban locations in Bangladesh. Dhaka: UNICEF; 2012 [Google Scholar]
- 9.Joint United Nations Programme on HIV/AIDS (UNAIDS). UNAIDS report on the global AIDS epidemic. Geneva: WHO; 2012. [Google Scholar]
- 10.National AIDS/STD Programme (NASP), Directorate General of Health Services, Ministry of Health and Family Welfare, Bangladesh. National HIV serological surveillance, Bangladesh: 9th round technical report. Dhaka: NASP and iccdr,b; 2011 [Google Scholar]
- 11.International Centre for Diarrhoeal Diseases Research, Bangladesh (iccdr,b). Midline survey of HIV, syphilis and risk behaviour among males having sex with males, male sex workers and hijra. Dhaka: iccdr,b; 2013 [Google Scholar]
- 12.National AIDS/STD Programme (NASP), Directorate General of Health Services, Ministry of Health and Family Welfare Bangladesh. 3rd National strategic plan for HIV and AIDS. Dhaka: NASP; 2011 [Google Scholar]
- 13.National AIDS/STD Programme (NASP), Directorate General of Health Services, Ministry of Health and Family Welfare, Bangladesh. National HIV risk reduction strategy for most at risk and especially vulnerable adolescents to HIV & AIDS in Bangladesh (2013–2015). Dhaka: NASP; 2013 [Google Scholar]
- 14.Abdul-Quader AS, Heckathorn DD, Sabin K, Saidel T. Implementation and analysis of respondent driven sampling: Lessons learned from the field. J Urban Health 2006; 83 (Suppl 1):1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mustanski B, Johnson AK, Garofalo R, et al. Perceived likelihood of using HIV preexposure prophylaxis medications among young men who have sex with men. AIDS Behav 2013; 17 (Suppl 6):2173–2179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kuhns LM, Birkett M, Muth SQ, et al. Methods for collection of participant-aided sociograms for the study of social, sexual and substance-using networks among young men who have sex with men. Connect (Tor) 2015; 35 (Suppl 1):1–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Marlin RW, Young SD, Bristow CC, et al. Piloting an HIV self-test kit voucher program to raise serostatus awareness of high-risk African Americans, Los Angeles. BMC Public Health 2014; 14 (Suppl 1226):1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Solomon SS, Srikrishnan AK, Vasudevan CK, et al. Voucher incentives improve linkage to and retention in care among HIV-infected drug users in Chennai, India. Clin Infect Dis 2014; 59 (Suppl 4):589–595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Eva G, Quinn A, Ngo TD. Vouchers for family planning and sexual and reproductive health services: a review of voucher programs involving Marie Stopes International among 11 Asian and African countries. Int J Gynecol Obstet 2015; 3:E15–E20. [DOI] [PubMed] [Google Scholar]
- 20.Kirkwood BR, Sterne JA. Essential medical statistics. 2nd edMalden, MA: Blackwell Publishing Company; 2003. [Google Scholar]
- 21.Burns RB, Burns RA. Logistic regression in business research methods and statistics using SPSS: Extension chapters on advanced techniques. London: SAGE Publications; 2008. [Google Scholar]
- 22.StataCorp, LP. Stata/SE 12.0 for Windows (64-bit). USA: Patent TX77845; 2009 [Google Scholar]
- 23.Mouton J. How to succeed in your Master's and Doctoral studies: a South African guide and resource book. Pretoria: Van Schaik Publishers; 2001. [Google Scholar]
- 24.Patten ML. Understanding research methods: an overview of the essentials. Los Angeles, CA: Pyrczak Publishing; 2002. [Google Scholar]
- 25.Khosla N. HIV/AIDS interventions in Bangladesh: what can application of a social exclusion framework tell us? J Health Popul Nutr 2009; 27 (Suppl 4):587–597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Grov C, Rendina HJ, Parsons JT. Comparing three cohorts of MSM sampled via sex parties, bars/clubs, and Craigslist.org: Implications for researchers and providers. AIDS Educ Prev 2014; 26 (Suppl 4):362–382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Grov C, Crow T. Attitudes about and HIV risk related to the “most common place” MSM meet their sex partners: comparing men from bathhouses, bars/clubs, and Craigslist.org. AIDS Educ Prev 2012; 24 (Suppl 2):102–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Grov C, Bux D, Jr, Parsons JT, Morgenstern J. Recruiting hard-to-reach drug-using men who have sex with men into an intervention study: Lessons learned and implications for applied research. Subst Use Misuse 2009; 44 (Suppl 13):1855–1871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Farid MS, Bontell I, Tahir S, et al. Transgendered people/Hijra. Working paper series on HIV and AIDS in Bangladesh 2015; 6:1–4. [Google Scholar]
- 30.World Health Organization (WHO). Making health services adolescent friendly: Developing national quality standards for adolescent friendly health services, Geneva: WHO, 2012 [Google Scholar]
- 31.Kranzer K, Govindasamy D, van Schaik N, et al. Incentivized recruitment of a population sample to a mobile HIV testing service increases the yield of newly diagnosed cases, including those in need of antiretroviral therapy. HIV Med 2012; 13:132–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Meuwissen LE, Gorter AC, Segura Z, et al. Uncovering and responding to needs for sexual and reproductive healthcare among poor urban female adolescents in Nicaragua. Trop Med Int Health 2006; 11 (Suppl 12):1858–1867. [DOI] [PubMed] [Google Scholar]
- 33.De Neve JW, Fink G, Subramanian SV, et al. Length of secondary schooling and risk of HIV infection in Botswana: evidence from a natural experiment. Lancet Glob Health 2015; 3 (Suppl 8):e470–e477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hargreaves JR, Bonell CP, Boler T, et al. Systematic review exploring time trends in the association between educational attainment and risk of HIV infection in sub-Saharan Africa. AIDS 2008; 22 (Suppl 3):403–414. [DOI] [PubMed] [Google Scholar]
- 35.National Institute of Population Research and Training (NIPORT). Mitra and Associates, and ICF Internatonal. Bangladesh demographic and health survey 2011. Dhaka and Calverton, Maryland: NIPORT, Mitra and Associates, and ICF International; 2013. [Google Scholar]
- 36.Araoye MO. Research methodology with statistics for health and social science. Ilorin Nigeria: Nathadex; 2003. [Google Scholar]


