Abstract
Background
The Anastomotic Coupling Device has demonstrated safety and efficacy; however, the coupler has never been compared directly to handsewn venous anastomoses exclusively in breast reconstruction. We hypothesized that rates of venous thrombosis would be lower using the coupler versus handsewn anastomoses in free flap breast reconstruction.
Methods
We performed a retrospective review utilizing clinic records, hospital records, and operative reports for 857 consecutive breast free flaps at a single institution from 1997-2012. Data was collected on reconstruction type, recipient vessels, timing, laterality, preoperative radiation, chemotherapy, venous thrombosis, and flap outcome. We compared rates of venous thrombosis between handsewn and coupled anastomoses for breast free flaps. Chi square test was used to calculate statistical significance.
Results
A total of 857 consecutive free flaps were performed for breast reconstruction in 647 patients over 16 years. The venous anastomosis was handsewn in 303 flaps, and the anastomotic coupler was used in 554 flaps. The rate of venous thrombosis requiring anastomotic revision in the handsewn group was 0.04% (12/303), compared to 0.01% in the coupled group (8/554; p=0.02).
Conclusion
The anastomotic coupler was more effective in preventing venous thrombosis than handsewn anastomoses in our series. While our study demonstrates improved patency rates using the venous coupler in breast reconstruction, we were unable to definitively separate this finding from potential confounding variables due to the low rates of thrombosis in both groups. Our data is consistent with current literature, which suggests that the coupler is a safe and effective alternative to hand sutured anastomoses.
Keywords: venous thrombosis, anastomotic coupling device, breast reconstruction
Introduction
The Anastomotic Coupling Device (ACD) has gained widespread popularity in venous anastomoses for microvascular free tissue transfer. Since the first metal coupling device was introduced in 1962 [1], several adaptations of materials and design have improved the efficacy and ease-of-use of anastomotic coupling devices. The currently favored device at Memorial Sloan-Kettering Cancer Center is the GEM Microvascular Anastomotic Coupler System (Synovis Micro Companies Alliance, Birmingham AL), a high-density polyethylene ring with interlocking stainless steel pins (Figure 1a). The system includes a vessel measurement gauge for coupler size selection, an anastomotic instrument to apply the coupler, and a coupler forceps to ensure accurate placement of vessel edges on the steel pins (Figure 1b).
Figure 1.
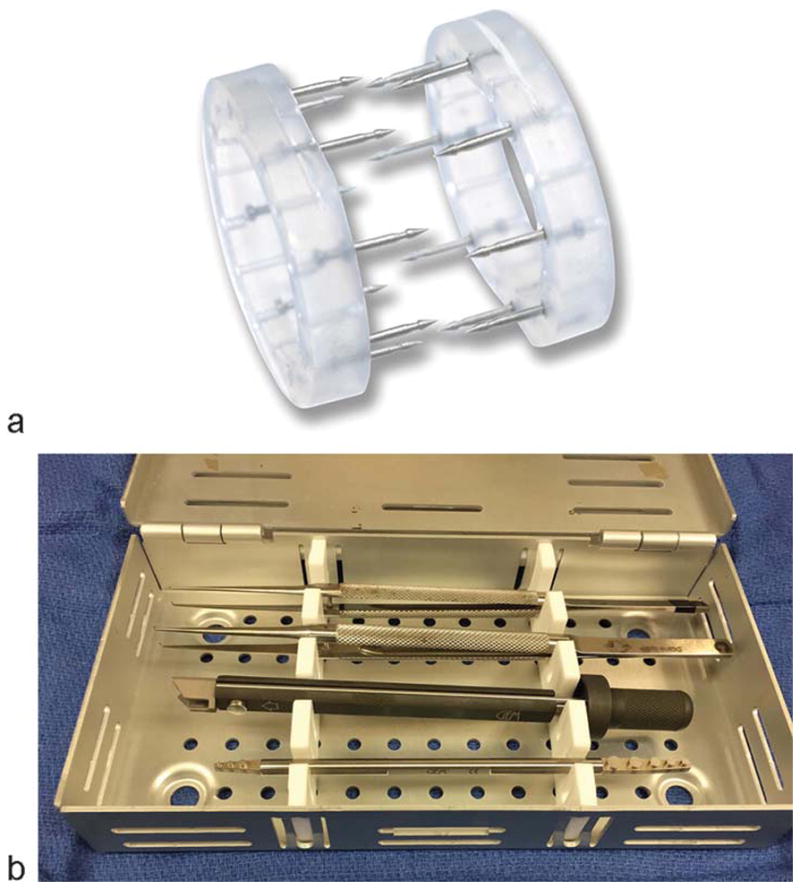
(a) GEM Microvascular Anastomotic Coupler (Synovis Micro Companies Alliance, Birmingham AL). (b) Coupler instrument tray including coupler forceps (2), anastomotic instrument, and vessel measuring gauge.
The safety and efficacy of the ACD has been evaluated by several large series in recent years. The device has been shown to reduce operative time while maintaining a high level of vessel patency [2]. A recent meta-analysis including more than 3500 free flaps showed flap survival and revision-free application in more than 99% of cases [3]. Jandali et al reviewed 1000 consecutive breast free flaps using the ACD for venous anastomosis, and found a thrombosis rate of 0.6% [2]. Rozen et al compared coupled vs. handsewn anastomoses in 1000 reconstructive free tissue transfers to the breast, head and neck, and extremities, and found a coupler thrombosis rate of 2.9%, which was not significantly different than the handsewn group [4]. A similar comparison by Yap et al showed no difference in thrombosis rates of coupled vs. handsewn venous anastomoses in more than 700 free flaps [5]. The device has been evaluated extensively in head and neck reconstruction with similar positive findings [6-8].
The predominance of literature suggests excellent outcomes with use of the ACD for venous anastomoses. Possible reasons for high patency rates include rigidity of the anastomosis and improved intimal contact. The literature is unclear regarding utility of the ACD when a vessel size and thickness mismatch is present. While some reports suggest that ACDs protect against thrombosis in vessel mismatch by creating a rigid lumen, other studies have suggested that size and thickness mismatch can lead to crimping of the intima, subsequently increasing potential risk of thrombosis [9 10].
While the body of literature affirming the safety of ACDs is growing, to our knowledge, there has not been a large series directly comparing coupled vs. handsewn anastomoses exclusively in breast reconstruction. This comparison is particularly important to plastic surgeons given that microsurgical breast reconstruction is one of the most common uses of free tissue transfers among plastic surgeons nationally. While other applications of microsurgery, such as head and neck reconstruction, have extended to the scope of practice of other specialties, microsurgical breast reconstruction remains nearly exclusively the domain of plastic surgeons.
Our institution transitioned to the routine use of the coupler for venous anastomosis in breast reconstruction around 2007. We hypothesized that rates of venous thrombosis requiring revision would be lower using the coupler versus handsewn anastomoses.
Methods
We performed a retrospective review utilizing clinic records, hospital records, and operative reports for 857 consecutive breast free flaps at Memorial Sloan-Kettering Cancer Center from 1997-2012. Surgeries were performed at a single institution by 6 surgeons with the assistance of microsurgical fellows. All surgeons performed both handsewn and coupled venous anastomoses. After approval by the institutional review board, data was collected on type of reconstruction (Transverse Rectus Abdominis Myocutaneous flap vs. Muscle-Sparing Transverse Rectus Abdominis Myocutaneous flap vs. Deep Inferior Epigastric Perforator vs. Superior Gluteal Artery Perforator), recipient vessels (internal mammary vs. thoracodorsal), timing (immediate vs. delayed), laterality (unilateral vs. bilateral), preoperative radiation, and preoperative chemotherapy. The technique of venous anastomosis (venous coupler vs. handsewn), and the size of coupler (2.0 mm – 3.5 mm) were evaluated. Outcomes of interest were venous thrombosis requiring reoperation with revision of anastomosis, and flap salvage.
Venous thrombosis was defined as clinically significant venous congestion requiring return to the operating room and revision of anastomosis. Cases in which the venous circulation was compromised secondary to arterial occlusion were excluded. Cases in which venous congestion was suspected preoperatively, but no thrombosis was identified intra-operatively and no revision of anastomosis was performed, were also excluded. We compared rates of true venous thrombosis requiring reoperation among patients with coupled anastomoses vs. handsewn anastomoses. Chi square test was used to calculate statistical significance (p<0.05).
Results
A total of 857 consecutive free flaps were performed for breast reconstruction in 647 patients over 16 years. The venous anastomosis was handsewn using 8.0 or 9.0 nylon suture in 303 flaps, and the anastomotic coupler was used in 554 flaps. Most free flaps performed were muscle-sparing transverse rectus abdominis myocutaneous (MS-TRAM, 50.4%) or deep inferior epigastric perforator (DIEP, 41.3%) flaps. The handsewn group was more likely to utilize the thoracodorsal system for recipient vessels (51.2%), while the coupled group was more likely to utilize the internal mammary system (92.4%). The coupled group was more likely than the handsewn group to be reconstructed in a delayed fashion (36.3% vs. 20%), to be bilateral (56.7% vs. 37%), and to receive chemotherapy and radiation (34.7% vs. 25.1%; 37.2% vs. 26.7%) (Table 1).
Table 1. Study sample demographics of handsewn vs. coupled venous anastomoses. Study Sample Demographics (N=857 flaps).
| Variables | HANDSEWN | COUPLED | p-value | ||
|---|---|---|---|---|---|
| (n=303) | (n=554) | ||||
| Type of Reconstruction | |||||
| MS-TRAM | 160 | (52.8%) | 272 | (49.1%) | 0.30 |
| DIEP | 92 | (30.4%) | 262 | (47.3%) | <0.001 |
| Free TRAM | 41 | (13.5%) | 10 | (0.02%) | <0.001 |
| SIEA | 4 | (0.01%) | 4 | (0.01%) | 0.38 |
| SGAP | 6 | (0.02%) | 1 | (0.001%) | 0.005 |
| TUG | 0 | (0%) | 5 | (0.01%) | 0.10 |
| Recipient Vessel | |||||
| IMA/IMV | 147 | (48.5%) | 512 | (92.4%) | <0.001 |
| TDA/TDV | 155 | (51.2%) | 41 | (7.4%) | <0.001 |
| Other | 1 | (0.3%) | 1 | (0.2%) | 0.66 |
| Timing of Reconstruction | |||||
| Immediate | 242 | (80%) | 353 | (63.7%) | <0.001 |
| Delayed | 61 | (20%) | 201 | (36.3%) | |
| Laterality | |||||
| Unilateral | 191 | (63%) | 240 | (43.3%) | <0.001 |
| Bilateral | 112 | (37%) | 314 | (56.7%) | |
| Preoperative Radiation | 81 | (26.7%) | 206 | (37.2%) | 0.002 |
| Preoperative Chemotherapy | 76 | (25.1%) | 192 | (34.7%) | 0.002 |
|
| |||||
| Venous thrombosis requiring revision | 12 | (0.04%) | 8 | (0.01%) | 0.02 |
The rate of venous thrombosis requiring anastomotic revision in the handsewn group was 0.04% (12/303), compared to 0.01% in the coupled group (8/554; p=0.02). The venous thrombosis events were distributed across flap types in both the handsewn and coupled groups (Table 2). Most thrombotic events occurred in MS-TRAM or DIEP flaps; however, this is likely due to the low numbers of alternative flaps evaluated in this study. Immediate reconstruction in both groups was more likely to result in venous thrombosis vs. delayed reconstruction. Similar numbers of thrombotic events occurred in radiated patients in both groups. Descriptive analysis of the individual thrombotic events in the handsewn vs. coupled group did not reveal any differences between them; however, analysis for statistical significance was not possible due to the low numbers of thrombotic events in each group.
Table 2. Descriptive variables of venous thrombosis events in handsewn vs. coupled anastomoses.
| Variables | HANDSEWN | COUPLED |
|---|---|---|
| (n=12) | (n=8) | |
| Type of Reconstruction | ||
| MS-TRAM | 5 | 3 |
| DIEP | 3 | 5 |
| Free TRAM | 2 | - |
| SIEA | - | - |
| SGAP | 2 | - |
| TUG | - | - |
| Recipient Vessels | ||
| IMA/IMV | 10 | 8 |
| TDA/TDV | 2 | - |
| Other | ||
| Timing of Reconstruction | ||
| Immediate | 10 | 6 |
| Delayed | 2 | 2 |
| Laterality | ||
| Unilateral | 4 | 4 |
| Bilateral | 8 | 4 |
| Preoperative Radiation | 5 | 5 |
| Preoperative Chemotherapy | 3 | 4 |
| Flap Salvage | 10 | 4 |
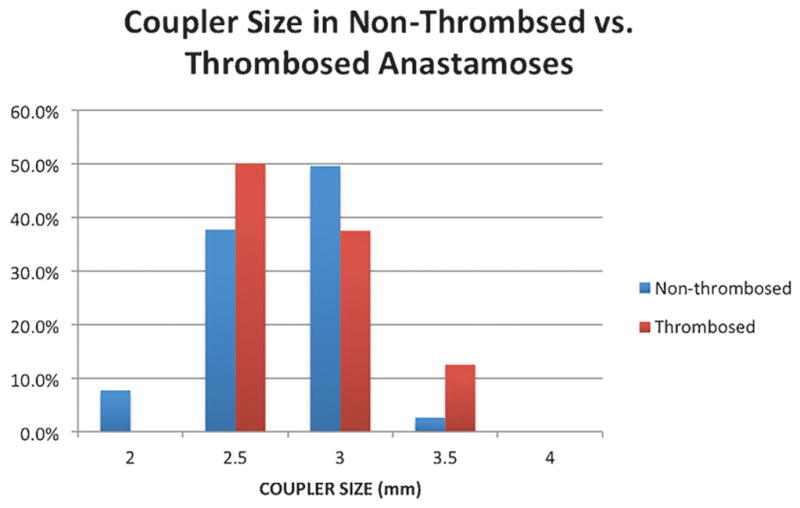
The size of the venous coupler utilized for anastomosis did not appear to have an effect on rate of venous thrombosis (Figure 2). More than 85% of anastomoses in both the non-thrombosed and thrombosed group were performed with 2.5 mm or 3.0 mm couplers. The distribution of coupler size was roughly equivalent in both groups.
Figure 2. Diameter of venous coupler used in successful venous anastomoses vs. anastomoses that experienced thrombosis.
Discussion
The venous anastomosis remains one of the most challenging and critical aspects of microsurgery. Venous thrombosis continues to be the leading cause of free flap failure; therefore, technical advancements that potentially reduce risk of venous thrombosis are particularly valuable to microsurgeons [11 12]. The goal of any microsurgical device is to maintain vessel patency while simultaneously improving technical ease and reducing operative time. The anastomotic coupler meets these requirements and has therefore gained widespread popularity [3 13-16].
In our series of breast free flaps, use of the anastomotic coupler resulted in fewer venous thrombosis events than handsewn anastomoses. Previous studies have shown similar rates of thrombosis between coupled and handsewn anastomoses, though no study to our knowledge has focused exclusively on breast reconstruction to compare the two techniques[2 4 5 17-19]. While our study demonstrates improved patency rates using the venous coupler in breast reconstruction, we were unable to definitively separate this finding from potential confounding variables due to the low rates of thrombosis in both groups. Our data is consistent with current literature, which suggests that the coupler is a safe and effective alternative to hand sutured anastomoses.
The success of the venous coupler in achieving vessel patency may be related to a number of factors that have been discussed in the literature. The learning curve for device utilization is fairly rapid owing to the technical ease of application. Our thrombotic events in the coupled group were evenly distributed over the time period of the study, suggesting that thrombotic events did not decrease with user experience. There may be greater intimal contact versus traditional suture techniques, as the device forces eversion of vessel edges prior to anastomotic connection. This ensures continuous contact along the entire vessel, which may be more difficult to achieve with hand-placed sutures distributed at self-selected intervals. The rigidity of the rings may prevent turbulent flow at the anastomosis that could contribute to venous thrombosis, and may further protect against vasospasm at the anastomotic site. Finally, by creating an anastomosis with a rigid circumference determined by the diameter of the ring, vessel size mismatches can be effectively addressed without relying largely on technical skill [9].
Our study is chiefly limited by the small number of thrombotic events in both groups. This limited our ability to perform detailed statistical analysis, including multiple logistic regression, to eliminate confounding variables that may have affected our conclusion.
Conclusions
This is the largest series to date directly comparing rates of venous thrombosis in coupled vs. handsewn anastomoses exclusively in breast reconstruction. Our study adds to the growing body of literature supporting widespread use of the coupler as a safe, effective, reliable, and reproducible means of vessel anastomosis.
Abbreviations
- ACD
Anastomotic Coupling Device
- TRAM
Transverse Rectus Abdominis Myocutaneous flap
- MS-TRAM
Muscle-Sparing Transverse Rectus Abdominis Myocutaneous flap
- DIEP
Deep Inferior Epigastric Perforator flap
References
- 1.Nakayama K, Tamiya T, Yamamoto K, et al. A simple new apparatus for small vessel anastomosisi (free autograft of the sigmoid included) Surgery. 1962;52:918–31. [PubMed] [Google Scholar]
- 2.Jandali S, Wu LC, Vega SJ, et al. 1000 consecutive venous anastomoses using the microvascular anastomotic coupler in breast reconstruction. Plastic and reconstructive surgery. 2010;125(3):792–8. doi: 10.1097/PRS.0b013e3181cb636d. [published Online First: Epub Date]|. [DOI] [PubMed] [Google Scholar]
- 3.Grewal AS, Erovic B, Strumas N, et al. The utility of the microvascular anastomotic coupler in free tissue transfer. The Canadian journal of plastic surgery = Journal canadien de chirurgie plastique. 2012;20(2):98–102. doi: 10.1177/229255031202000213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rozen WM, Whitaker IS, Acosta R. Venous coupler for free-flap anastomosis: outcomes of 1,000 cases. Anticancer research. 2010;30(4):1293–4. [PubMed] [Google Scholar]
- 5.Yap LH, Constantinides J, Butler CE. Venous thrombosis in coupled versus sutured microvascular anastomoses. Annals of plastic surgery. 2006;57(6):666–9. doi: 10.1097/01.sap.0000229958.57126.21. [published Online First: Epub Date]|. [DOI] [PubMed] [Google Scholar]
- 6.DeLacure MD, Wong RS, Markowitz BL, et al. Clinical experience with a microvascular anastomotic device in head and neck reconstruction. American journal of surgery. 1995;170(5):521–3. doi: 10.1016/s0002-9610(99)80344-4. [DOI] [PubMed] [Google Scholar]
- 7.Zhang T, Lubek J, Salama A, et al. Venous anastomoses using microvascular coupler in free flap head and neck reconstruction. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons. 2012;70(4):992–6. doi: 10.1016/j.joms.2011.02.111. [published Online First: Epub Date]|. [DOI] [PubMed] [Google Scholar]
- 8.Barker EV, Enepekides DJ. The utility of microvascular anastomotic devices in head and neck reconstruction. Current opinion in otolaryngology & head and neck surgery. 2008;16(4):331–4. doi: 10.1097/MOO.0b013e32830139a7. [published Online First: Epub Date]|. [DOI] [PubMed] [Google Scholar]
- 9.Sullivan SK, Dellacroce F, Allen R. Management of significant venous discrepancy with microvascular venous coupler. Journal of reconstructive microsurgery. 2003;19(6):377–80. doi: 10.1055/s-2003-42632. [published Online First: Epub Date]|. [DOI] [PubMed] [Google Scholar]
- 10.Bank J, Teng E, Song DH. Microvascular coupler-induced intimal crimping causing venous thrombosis. Journal of reconstructive microsurgery. 2015;31(2):157–8. doi: 10.1055/s-0034-1390302. [published Online First: Epub Date]|. [DOI] [PubMed] [Google Scholar]
- 11.Fearon JA, Cuadros CL, May JW., Jr Flap failure after microvascular free-tissue transfer: the fate of a second attempt. Plastic and reconstructive surgery. 1990;86(4):746–51. doi: 10.1097/00006534-199010000-00024. [DOI] [PubMed] [Google Scholar]
- 12.Tsai TM, Bennett DL, Pederson WC, et al. Complications and vascular salvage of free-tissue transfers to the extremities. Plastic and reconstructive surgery. 1988;82(6):1022–6. doi: 10.1097/00006534-198812000-00013. [DOI] [PubMed] [Google Scholar]
- 13.Sasson HN, Stofman GM, Berman P. Clinical use of the 3M 2. 5 mm mechanical microcoupling device in free tissue transfer Microsurgery. 1994;15(6):421–3. doi: 10.1002/micr.1920150610. [DOI] [PubMed] [Google Scholar]
- 14.Schubert HM, Schoeller T, Wechselberger G. 1000 consecutive venous anastomoses using the microvascular anastomotic coupler in breast reconstruction. Plastic and reconstructive surgery. 2010;126(5):1789. doi: 10.1097/PRS.0b013e3181ef916f. author reply 89. [published Online First: Epub Date]|. [DOI] [PubMed] [Google Scholar]
- 15.de Bruijn HP, Marck KW. Coupling the venous anastomosis: safe and simple. Microsurgery. 1996;17(7):414–6. doi: 10.1002/(sici)1098-2752(1996)17:7<414(x02237)aid-micr12>3.0.co;2-2. [published Online First: Epub Date]|. [DOI] [PubMed] [Google Scholar]
- 16.Berggren A, Ostrup LT, Ragnarsson R. Clinical experience with the Unilink/3M Precise microvascular anastomotic device. Scandinavian journal of plastic and reconstructive surgery and hand surgery / Nordisk plastikkirurgisk forening [and] Nordisk klubb for handkirurgi. 1993;27(1):35–9. doi: 10.3109/02844319309080289. [DOI] [PubMed] [Google Scholar]
- 17.Ahn CY, Shaw WW, Berns S, et al. Clinical experience with the 3M microvascular coupling anastomotic device in 100 free-tissue transfers. Plastic and reconstructive surgery. 1994;93(7):1481–4. doi: 10.1097/00006534-199406000-00022. [DOI] [PubMed] [Google Scholar]
- 18.Nishimoto S, Hikasa H, Ichino N, et al. Venous anastomoses with a microvascular anastomotic device in head and neck reconstruction. Journal of reconstructive microsurgery. 2000;16(7):553–6. doi: 10.1055/s-2000-8394. [DOI] [PubMed] [Google Scholar]
- 19.Camara O, Herrmann J, Egbe A, et al. Venous coupler for free-flap anastomosis. Anticancer research. 2009;29(7):2827–30. [PubMed] [Google Scholar]


