Abstract
The education sector offers compelling opportunities to address the shortcomings of traditional mental health delivery systems and to prevent and treat youth mental, emotional, and behavioral (MEB) problems. Recognizing that social and emotional wellness is intrinsically related to academic success, schools are moving to adopt multi-tier frameworks based on the public health model that provide a continuum of services to all children, including services to address both academic and MEB problems. In this paper, we review the potential value of multi-tier frameworks in facilitating access to, and increasing the effectiveness of, mental health services in schools and review the empirical support for school-based mental health interventions by tier. We go on to describe a community-academic partnership between the Seattle Public Schools and the University of Washington School Mental Health Assessment, Research, and Training (SMART) Center that exemplifies how multi-tier educational frameworks, research and evidence, and purposeful collaboration can combine to improve development and implementation of a range of school-based strategies focused on MEB needs of students. Finally, we present a set of 10 recommendations that may help guide other research and practice improvement efforts to address MEB problems in youth through effective school mental health programming.
In the United States, roughly one out of every five children experiences a mental health problem severe enough to warrant diagnosis (Costello et al., 2003). These problems interfere with youth functioning across domains, negatively impacting social relationships (Cook et al., 2010) and placing students at increased risk for academic failure (Vander Stoep et al., 2003) and school dropout (Moore et al., 2009). When left unaddressed, mental, emotional, and behavioral (MEB) problems of youth are likely to persist into adulthood and may result in costly long-term outcomes such as incarceration (Moore et al., 2009), unemployment (Nielsen et al., 2011), and reliance on public assistance (Fergusson et al., 2007).
The education sector offers compelling opportunities to address the shortcomings of mental health delivery systems and to prevent and treat youth MEB problems. First, schools are particularly convenient access points, reducing barriers to treatment that plague traditional outpatient settings, such as transportation, health insurance, and parental involvement (Pullmann et al., 2013; Pullmann, VanHooser, Hoffman, & Heflinger, 2010). Schools may be particularly effective in promoting access to care for historically-underserved groups, such as ethnic minority youth (Lyon, Ludwig, Vander Stoep, Gudmundsen, & McCauley, 2013). Second, since free and compulsory education is offered to children aged 5 - 18 in the United States (Cabus & De Witte, 2011), schools are uniquely positioned to deliver a range of interventions from preventive to intensive. Third, school-based mental health interventions, when integrated with academic learning, have shown promise to not only promote MEB well-being but to also improve academic performance (e.g., Durlak, Weissberg, Dymnicki, Taylor, & Schellenger, 2011; Walker, Kerns, Lyon, Bruns, & Cosgrove, 2010). Finally, a positive educational climate that promotes a sense of belonging at school can itself buffer certain students from outside risk factors (Klein, Cornell, & Konold, 2012). For all the above reasons, significant advocacy and federal attention has been directed toward providing students with access to school-based mental health, or SBMH (President's New Freedom Commission, 2003; U.S. Department of Health and Human Services, 1999). In part because of this advocacy, SBMH programs have grown progressively in the U.S. and are now widely available, to the point that the majority (70-80%) of mental health services for youth are provided in schools (Farmer et al., 2003; Rones & Hoagwood, 2000).
In this paper, we highlight the value of the public health model and related multi-tiered frameworks in facilitating access to, and increasing the effectiveness of, mental health services in schools. Next, we briefly review the empirical support for school-based delivery of mental health interventions. We go on to describe a community-academic partnership between the Seattle Public Schools (SPS) and the University of Washington (UW) School Mental Health Assessment, Research, and Training (SMART) Center, as a way of exemplifying how purposeful collaboration between researchers and practitioners can overcome common shortcomings in SBMH and translate educational adaptations of the public health model into specific research-based interventions and strategies. Finally, we present a set of 10 principles that extend from our lessons learned in conducting this work, and that guide our quest to prevent and address MEB problems in youth through effective school mental health programming.
Applying the Public Health Model to Education
Along with the substantial opportunities provided by schools to intervene in MEB disorders of childhood, an array of barriers and challenges must be addressed. For example, schools have traditionally operated under a “Refer-Test-Place” model (Cash & Nealis, 2004), in which only those children who struggle in mainstream educational settings are referred for an assessment of their needs for special education or other individualized services. The model has resulted in the ‘wait-to-fail’ phenomenon in education in which students who struggle socially, emotionally, and academically often fail for prolonged periods of time until their needs can no longer be ignored by educators (Shinn & Walker, 2010). Such traditional approaches often produce a substantial gap in services for students with serious needs and can exacerbate problems that might have been successfully addressed through more proactive attention.
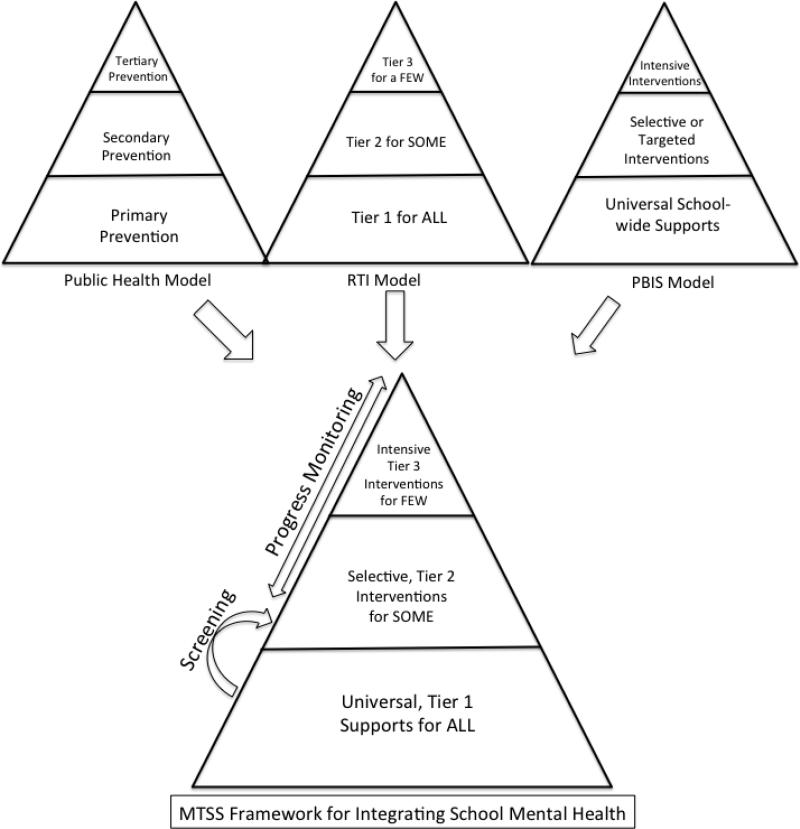
As an alternative, multi-tier frameworks based on the public health model have garnered increased empirical attention and practical adoption in education. From its origins in the 1960s (Leavell & Clark, 1965), the public health model eventually evolved into the educational sector, most notably beginning in 1990s with the introduction of Response to Intervention (RTI) as an alternative model to service delivery that involves (a) delivering a continuum of services to support the academic success of all students and (b) gathering data for earlier identification and progress monitoring of students with learning needs to ensure that they receive more timely and effective intervention (Gresham, 2005). As RTI was gaining popularity, initial momentum for the Positive Behavior Interventions and Supports (PBIS) model was established with the reauthorization of the Individuals with Disabilities Act of 1997 and a federal grant to establish a national center on PBIS for students with significant behavior problems. Continued interest in PBIS morphed into the National Technical Assistance Center on PBIS and the current school-wide, multi-tier framework for preventing, reducing, and managing behavior problems. As shown in Figure 1, the public health model of primary, secondary, and tertiary prevention is conceptually and structurally similar to both the RTI (National Center on Response to Intervention, 2010) and PBIS models (Lewis & Sugai, 1999).
Figure 1.
Integration of multi-level intervention models into a comprehensive Multi-Tier System of Supports (MTSS) for school-based social and emotional programming.
In Table 1, we summarize the commonalities and differences in each of these frameworks and the general progression of them over time, with the public health model undergirding the evolution of both RTI and PBIS in schools as multi-tier frameworks for promoting student outcomes. It is important to note that RTI and PBIS represent the essentially the same public health model-informed framework with sometimes slightly different terminology and different instructional focus (e.g., RTI focusing on academics and PBIS focusing on behavior). Both, however, share the same goal of improving student school experiences and outcomes. As shown, while each model has three tiers, the overall emphasis of each model varies somewhat, as does the focus on each tier. As a result, the core sources of data that inform intervention and assignment of individuals to tiers also varies. In the current paper, we adopt the terminology of “Multi-Tier Systems of Support” (MTSS) as a reflection of this term's current status in the field of education as representing an integrative framework for organizing school-based approaches to preventing and addressing academic problems, as well as MEB problems that impact student academic progress.
Table 1.
Comparison of Leading Multi-Level Models Relevant to School-Based Service Delivery
| Public Health Model | Response to Intervention (RTI) | PBIS Model | |
|---|---|---|---|
| Years | 1965-1970 | 1990-2001a | 1997-2002 |
| Introduced Levels | Primary Prevention Secondary Prevention Tertiary Prevention |
Tier 1 for all students Tier 2 for some students Tier 3 for a few students |
Universal School-wide Supports Selective/Targeted Interventions Intensive Interventions |
| Emphasis of the Model | Prevention, reversal, or management of disorder or illness | Prevent, remediate, or intensively treat academic problems | Prevent and address externalizing behaviors and promote positive school climate |
| Data-Based Decision Making | Collection of prevalence data and examining risk for an illness or disorder | Academic screeners and progress monitoring instruments based on curriculum-based measures | Office discipline referrals for screening purposes and point sheets or direct behavior ratings for progress monitoring. |
| Limitations | System focuses on prevention of specific diseases, illnesses, and disorders, and fails to integrate promotion-based strategies that optimize physical and mental health | Primary focus on academics with limited attention to the integration of MEB supports. | Multi-tier model based on behavior analytic principles that focuses narrowly on preventing and addressing externalizing behaviors. |
Note. PBIS = Positive Behavior Interventions and Supports.
The concept of RTI was introduced by Gresham (1991) and was emphasized in series of reading intervention studies conducted by several different research groups (e.g, Torgesen, Velluntino, Vaughn, and Fuchs). The formal RTI term was not fully introduced until 2001 during a Learning Disabilities Summit hosted by American Institute of Research and later referred to in law in 2004 with the reauthorization of the Individuals with Disabilities Education Act.
Despite the evolution of terminology over time, it is clear that schools have long been seen as a particularly conducive setting for a public health agenda that promotes the wellness of an entire population (Barret, Eber, & Weist, 2013; Cappella, Frazier, Atkins, Schoenwald, & Glisson, 2008). As such, RTI, PBIS, and MTSS are all descendants and share common core principles of the public health model. For one, the models emphasize the provision of appropriate services and supports for all students. Primary, universal, or Tier 1 prevention and promotion efforts are thus a greater focus in multi-tier models than in the “Refer-Test-Place” approach (Cash & Nealis, 2004). Second, systematic surveillance, progress monitoring, and data-based decision making are core strategies at every level of support. Such data collection informs where an individual student is situated within the multi-level system and provides the basis for disability determination for students who have not responded to less intensive supports (Gresham, 2005).
In the MTSS framework, Tier 1 interventions are delivered to all students and can include a research-based core curriculum, culturally and linguistically responsive instructional practices, universal screening to assess current level of performance, social emotional curricula delivered in the classroom, and clear behavioral expectations and supports (National Center on Response to Intervention, 2010; Lewis & Sugai, 1999). Students who are identified as needing additional help beyond available Tier 1 supports receive targeted support at Tier 2. Typical Tier 2 interventions take the form of adult-led individual or small-group instruction, delivered as part of the general education programming (Burns & Coolong-Chaffin, 2006; National Center on Response to Intervention, 2010). Brief, individualized interventions from SBMH providers are also classified as Tier 2 (e.g., Lyon et al., 2014). Those who continue to struggle after receiving secondary-level supports are provided with intensive, individualized, Tier 3 interventions (National Center on Response to Intervention, 2010). Tier 3 supports are often for students with complex needs and, therefore, involve specially trained professionals (e.g., behavior specialists, mental health providers, and social workers).
Effectiveness of School Mental Health Programming Across Multiple Tiers of Support
Excellent reviews of the evidence base for SBMH programming across the three tiers of support have been provided previously (e.g., Farahmand et al., 2011; Fazel, Hoagwood, Stephan, & Ford, 2014; Hoagwood et al., 2007; Rones & Hoagwood, 2000), and we will not attempt a comprehensive review here. There is evidence for positive effects of school-based programs across tiers; however, as described below, few rigorous studies of more intensive and individualized Tier 2 and Tier 3 SBMH interventions exist. We briefly review the evidence here to provide context for the description of the SMART Center's efforts to improve elements of SBMH programming across all tiers of support in Seattle Public Schools, and our recommendations for further research and policy.
Universal Screening and Assessment
Universal school-based screening, another extension of the public health model, has been proposed as one method for early identification of both academic (VanDerHeyden, Witt, & Gilbertson, 2007) and mental health problems (Levitt, Romanelli, & Hoagwood, 2007). Universal screening involves systematic assessment of an entire school population to identify students in need of additional supports. Data can also be aggregated to compare groups or settings within that larger system to determine where significant needs and strengths exist. Conducting ongoing screening allows for monitoring of the prevalence and incidence of specific problem behaviors, enabling schools to prioritize and direct resources towards prevention or intervention efforts that are most needed.
Despite the proposed benefits, less than 2% of schools utilize a systematic screening process to identify risk for MEB problems (Romer & McIntosh, 2005). While limitations to adoption have been documented (e.g., parental and community concerns about screening, lack of flexibility in content, relatively low response rates), little research has been conducted on the impact of screening and assessment efforts on school and MEB outcomes. Although Green et al. (2013) found that a school's level of effort in screening and early identification was related to the level of mental health service use among students, screening efforts may also unintentionally label children if effective interventions are not available or provided, creating stigma that undermines their academic and MEB performance (Sayal, Owen, White, Merrel, Tymms, & Taylor, 2010). Thus, screening efforts must be linked to effective interventions that are matched to students’ identified needs.
Tier 1 Strategies
A number of school-based primary prevention programs have demonstrated empirical support for improving student outcomes, spanning from externalizing behavior such as aggression (Wilson & Lipsey, 2007), internalizing problems such as anxiety (Neil & Christensen, 2009), and substance use (Tobler et al., 2000). A notable exception is Tier 1 interventions for depression, which have demonstrated weaker effect sizes than those targeted at high-risk populations (Calear & Christensen, 2010; Fazel et al., 2014), presumably because of “floor effects” whereby children in the sample with relatively lower depressive symptoms at the outset of the study have less capacity to show improvement. A recent meta-analysis showed that Tier 1 social and emotional learning programs resulted in improved student competencies, including social and emotional skills, attitudes, behavior, as well as an 11 percent increase in academic performance (Durlak et al., 2011).
Tier 2 Strategies
Tier 2 SBMH interventions typically are characterized as “selective approaches” that target students who demonstrate emergent MEB problems or risk factors for developing them. Effective programs have been developed to reduce aggressive behavior (Lochman & Wells, 2002) and substance abuse (Castellanos & Conrod, 2006). Additionally, a number of school-based programs have been shown to be effective for reducing anxiety and depression (Neil & Christensen, 2009; Calear & Christensen, 2010). The research base for Tier 2 programming, however, consists primarily of efficacy studies, and few evaluations exist of Tier 2 programming in real-world education settings.
In addition to interventions that target students with specific risk factors, there has been a longstanding movement to bring mental health practitioners into schools to provide the diverse array of services that might be provided in less accessible settings such as clinics, and thus reduce gaps in access to care (Weist & Evans, 2005). Such SBMH services may be conceived as bridging Tiers 2 and 3, depending on the intensity of intervention provided by the SBMH practitioner. While there is much enthusiasm for SBMH's potential to improve MEB wellness of students and promote broader school goals, the literature consists primarily of program descriptions and uncontrolled outcome studies (Nabors & Reynolds, 2000; Walker, Kerns, Lyon, Bruns, & Cosgrove, 2010). Reviews and meta-analyses of rigorously conducted SBMH research, moreover, typically yield few methodological rigorous studies, and the summary of these analyses often reveal null to small, and even iatrogenic, effects (Farahmand et al., 2011; Hoagwood et al., 2007; Rones & Hoagwood, 2000).
Tier 3 Strategies
At the top of the framework are individually-tailored and intensive interventions. Although the literature is relatively scarce in this tier, there are empirically-supported, school-specific interventions for post-traumatic stress disorder (Stein et al., 2003), depression (Calear & Christensen, 2010), and anxiety (Neil & Christensen, 2009). In addition, there is an extensive literature supporting the common Tier 3 strategy of using functional behavior assessment to inform the development of an individualized behavior intervention plan for students with serious emotional and behavioral disorders that impede their functioning in school and can disrupt the learning of other students. Finally, for youth with the most complex needs, there is an emerging literature demonstrating the potential for positive impacts of structured “Tier 3 wraparound” teams that coordinate care to address a child's needs across different areas of functioning and settings (Eber, Hyde, & Suter, 2011; Malloy, Drake, Abate, & Cormier, 2010).
Challenges and Barriers to School-Based Programming
Despite the benefits cited in the previous sections, several challenges have interfered with the goal of leveraging education-sector mental health programming to effectively address the MEB needs of youth. Consistent with academic interventions and supports, there is a significant gap between “what works” and what actually is implemented in SBMH (Forman et al., 2013). There are several explanations for this limited use of effective SBMH services.
Prioritization of Mental Health by Educators
First, the extent to which MEB problems are a priority for the leadership or staff working in schools is highly variable. Educators who endorse the importance of student emotional and behavioral competencies are more likely to be receptive to related training and administrative adoption decisions, integrate strategies to address MEB into their daily practices (Brackett et al., 2012), and carry out these strategies with integrity (Kincaid et al., 2007). Unfortunately, those who hold attitudes or beliefs that are less conducive to these programs are less likely to adopt or sustain those interventions (Cook, Lyon, Kubergovic, Browning-Wright, & Zhang, in press).
Workforce and Resource Limitations
Workforce development to increase the capacity of schools to support student mental health is sparse and insufficiently interdisciplinary (Suldo et al., 2014). Although universal approaches such as PBIS provide an evidence-based framework for engaging multiple types of school professionals in practices designed to enhance effective discipline and improve student behavior, programs directed at students who are already experiencing mental health symptoms are generally left to dedicated healthcare staff, who are invariably in limited supply. Focusing resources on mental health services is a “hard sell” when basic education remains underfunded (Prodente, Sander, & Weist, 2002). For this reason, school staff often have few mental health training resources available to them (Evans & Weist, 2004).
Contextual Fit of EBP to the School Context
Even when resources are available to support the installation of new mental health programs, the interventions identified may not have been developed or tested in schools (Wong, 2008). As a result, intervention-setting appropriateness – defined as “the perceived fit, relevance, or compatibility of the innovation or evidence-based practice for a given practice setting, provider, or consumer” (Proctor et al., 2011, p. 69) – is often suboptimal. Although there is increasing recognition that appropriateness may be a particularly salient construct when implementing EBP in schools (Lyon, Ludwig, Romano, Koltracht et al., 2014), little research has addressed this issue.
Broader Systemic Issues
Additional contextual barriers to providing timely and effective services in schools include the requirement that, to receive care, students must be actively attending school. School absences, especially among students with the greatest mental health needs, have been referenced by SBMH providers as one barrier to providing needed services (Lyon, Ludwig, Romano et al., 2013). Furthermore, students who drop out are unlikely to be able to continue to receive services. Given these issues, school mental health services need to be flexible and entail outreach to children and families in the community to facilitate access to care. Schools also reflect the larger social context, which can include various institutionalized inequalities and inadvertent staff biases. For instance, substantial racial disproportionality in staff disciplinary responses (e.g., suspensions, expulsions) to student misbehavior has been well documented across a wide range of academic settings (Balfanz, Byrnes, & Fox 2013; Fabelo, et. al., 2011; Losen & Gillespie, 2012; U.S. Department of Education Office for Civil Rights, 2014).
Integrating Behavioral Health into Schools through a Research-Practitioner Partnership
In any systems improvement effort, applications of epistemological orientations (such as a commitment to research-based practices and/or use of data to inform programming and policy) and conceptual frameworks (such as the public health model and/or MTSS framework) inevitably must be married to the local context to increase the likelihood of effective implementation. Thus, applications of MTSS and the public health model will likely look very different from system to system and community to community. Even when adopted with rigor, programmatic elements within these models are free to vary, including screening and assessment measures and approaches; school-wide, universal prevention programs; Tier 2 and Tier 3 interventions; process and outcome measures; and the types of practitioners who do the work.
For over 10 years, scientist-practitioners from the University of Washington School of Medicine and College of Education have collaborated with Seattle Public Schools (SPS) to attempt to bridge the “science to service” gap by (1) building a comprehensive, integrated strategy that reflects frameworks such as MTSS and (2) ensuring that each component within the overarching strategy is guided by relevant research. SPS is the largest school system in Washington State, with 95 schools serving nearly 50,000 students. The district is also highly diverse, as reflected by its racial diversity (43% of students are Caucasian, 22% Asian, 21% African-American, 12% Hispanic, and 2% American Indian), socioeconomic status (41% are on free or reduced price meal programs) and languages spoken, which number over 120.
To integrate UW faculty members’ projects with SPS, the SMART Center (https://education.uw.edu/smart) was founded in 2013 to bring together UW researchers and intervention specialists who are actively engaged in collaborative efforts with SPS schools, as well as schools nationally, to improve access to evidence-informed SBMH programs and mobilize the promise of both the education sector and public health model as vehicles for improving youth mental health. In the remainder of this section, we describe current and proposed projects being implemented through the SPS-SMART collaboration, to illustrate (1) examples of how challenges and barriers in implementing supports and services for students with MEB problems can be addressed across the MTSS continuum, (2) how local context influences the selection and implementation of such strategies, and (3) how academic-public collaboration can shape these efforts.
Universal Screening and Assessment
Starting in 2002, UW faculty partnered with SPS to identify students experiencing or at risk of developing depression and/or conduct problems during the transition periods from elementary to middle school and middle to high school. As a result, UW and SPS collaborated to design protocols to conduct universal emotional health screening among middle school students to identify at-risk youth and facilitate linkages to educational and mental health supports. Research on these local efforts has demonstrated that these programs are feasible, effectively increase student entry into indicated services, and are cost effective (Kuo, Vander Stoep, McCauley, & Kernic, 2009; Vander Stoep et al., 2005). Most recently, we have used system dynamics modeling (Homer & Hirsch, 2006) to estimate the impact of a universal screening program on additional service demand and simulate the effects of implementing “compensatory approaches” (e.g., EBP implementation) designed to address anticipated increases in service need (Lyon, Maras, Pate, Igusa, & Vander Stoep, in press).
Despite these positive outcomes, a number of concerns about school-based screening have surfaced over the last decade, including fears about unnecessary labeling of students as having mental health problems leading to stigma and referral to unwarranted treatment, and potential overuse of psychotropic medications in youth (Conservative Caucus, 2004; Eakman, 2004). There was also apprehension about identifying youth in need of services that were not available. While we documented our ability to successfully connect youth to needed services, our experiences taught us a number of lessons. These include the importance of forming a trusting working partnership with each school and making sure that the entire school staff, as well as parents and youth, are aware of the goals, objectives and limits of the screening program well before it is initiated. This involves engagement with principals and administrative teams, active participation in PTA and “back-to-school” nights to inform parents, and informational sessions with students. Establishing this sense of trust also involves careful but practical attention to confidentiality and its limits, so that students know that their individual responses will not be shared with school personnel or parents and also that a system is in place to follow up on all reports of elevated distress and risk, which could be used with parents to assure student safety. Finally, we learned that screening must be carefully organized and efficient limiting disruption to teaching time and school schedules.
Tier 1
Addressing disproportionality in discipline
Consistent with national statistics, SPS currently struggles with racial disproportionality in its discipline practices, with African-American high school students suspended or expelled more than three times as often as other students. Disproportionality has thus emerged as a high priority for the SPS- SMART partnership. After meetings with SPS personnel, a new partnership called the Minority Engagement and Disproportionality Reduction Collaborative has been proposed, focused on two priorities: First, to build district capacity to use state-of-the-art data analysis techniques to understand where, with whom, and why disproportionality exists; and second, to build on and extend the principles and structures of PBIS (Lewis & Sugai, 1999) to address disproportionality within select schools.
After data review, select schools will be identified to receive professional development training, coaching support, and implementation resources that are part of an empirically-supported process that includes problem identification, problem analysis, development of a plan, implementation of the plan, and evaluation of the plan's effectiveness. School teams will customize an intervention plan that targets the driving forces of discipline disproportionality within their school, selecting from six interventions that align with research on core causes: modifying discipline policy (American Psychological Association Task Force on Zero Tolerance, 2008), increasing staff cultural competence (Banks, 2013; Gillette & Boyle-Baise, 1995), enhancing educator-student relationships (Yeager et al., 2014), improving proactive classroom management (Rathvon, 2008), implementing effective reactive strategies (Reinke, Lewis-Palmer, & Merrell, 2008; Pianta, La Paro, & Hamre, 2008), and screening and referral to selective interventions (Cook, Volpe, & Livanis, 2010).
Tier 2
Development of a brief intervention strategy for school clinicians
In SPS and elsewhere, mental health services available in schools are rarely based on evidence of effectiveness and are often disconnected from the larger school context. Providers carry large caseloads, experience significant time constraints, and must serve youth with a broad array of needs (Lyon, Ludwig, Romano, Leonard, Vander Stoep, & McCauley, 2013; Lyon, Ludwig, Romano, Koltracht, Vander Stoep, & McCauley, 2014). To address these issues, SMART Center faculty have worked with SPS leaders and SBMH providers to develop a brief, evidence-based, flexible mental health intervention that fits the school context while maintaining clear intervention structure. This intervention dually emphasizes MEB and academic outcomes.
The Brief Intervention for School Clinicians (BRISC) is conceptualized as a “Tier 2” strategy within MTSS and intended to emphasize both social-emotional and academic outcomes. BRISC is delivered in approximately four sessions. Clinicians using BRISC quickly assess the student's needs using a structured process and then engage the youth in problem solving around treatment goals. The student's identified goals are addressed quickly, using one or more research-based strategies (e.g., cognitive restructuring, motivation enhancement, communication skills, stress and mood management) that have been incorporated into BRISC based on their match to typical student needs. Systematic progress monitoring is an essential component, and guides clinical decisions about whether students’ needs have been met and/or when students should be referred to more or less intensive or specialized services (Lyon, Bruns et al., 2014).
Funded by a Development and Innovation grant from the Institute for Educational Sciences (DOE R305A120128), early findings of the Brief Intervention for School Clinicians (BRISC) indicate that BRISC promotes students’ motivation to continue counseling, increases proactive coping, and improves overall social-emotional functioning of students. (Bruns, Lyon, & McCauley, 2013; Lyon et al., in submission). Thus, BRISC represents a good example of an effort to address several common barriers to effective SBMH through development of a defined Tier 2 strategy that mobilizes research evidence and promotes better integration with the school context and mission. BRISC's potential for positive effects, however, will not be fully established until evaluation of its effects on student academic outcomes is completed.
Tier 3
Many of SMART Center projects focused on evaluating Tier 3 services within the SPS system have been funded and supported by a series of voter initiatives in Seattle that apply funds collected from a property tax levy to educational support services. The Families and Education Levy was first passed by Seattle voters in 1990 and has since been renewed three times. The most recently passed Levy provides approximately $254 million from 2013-2017 to fund a range of strategies intended to promote school readiness, academic achievement, and reduction of achievement gaps.
Family support program
Under the auspice of the Levy, the SMART Center evaluated and recommended improvements to a school-based Family Support Program (FSP), conceived as spanning Tiers 2 and 3 of the MTSS framework. FSP operated in 28 high-needs, mostly elementary, schools. FSP staff worked directly with families and students on non-academic barriers to success such as transportation, poverty, clothing, medical care, and housing. FSP staff also liaison with teachers, families, child welfare, community service providers, and school administration to identify and serve students with multiple and complex needs such as extreme poverty, homelessness, past trauma, recent immigration, refugee status, mental health needs, and special education.
In 2004, the goals of Levy-supported projects shifted to academic achievement, increasing pressure on the FSP to demonstrate academic impact instead of its previous social-emotional focus, resulting in our evaluation of the program in 2013-2014. While the FSP stressed academic achievement by facilitating family involvement in education, access connecting students to supplementary academic resources, and providing instrumental support to overcome barriers, our evaluation showed that many staff in the FSP felt that their training and experience had not prepared them for a role in directly improving academic functioning. Unsurprisingly, our evaluation found no evidence of a positive impact of the FSP on standardized test scores, disciplinary actions, or attendance. However, trends were found for an impact on outcomes more closely linked to the activities of FSP workers, such as student mobility and schools’ connectedness to community resources (Pullmann, Weathers, Hensley, & Bruns, 2013). Though these results disappointed many in the FSP, they were used to inform refinements to staff training, student triage, and progress monitoring activities to connect them more closely to improvements in student academic functioning. FSP staff now regularly incorporate academic indicators into their monitoring of individual youth plans and progress, and staff trainings are specifically focused on methods to improve academic performance and engage parents in supporting academic success. At a deeper level, the results from this evaluation helped guide the SMART Center's focus on staying connected to the academic mission of schools (see Recommendation #3 below) and to make academic outcomes—traditionally considered distal, mediated indicators of school-based non-academic interventions—more proximally connected to the activities of the intervention (Lyon, Borntrager, Nakamura, Higa-McMillan, 2013; Lyon, Bruns, Ludwig, et al., in preparation).
School health and mental health services
Levy funds also provide the financial support to SBHCs located in each of Seattle's 22 middle and high schools as well as 8 high-need elementary schools. In secondary schools, each SBHC employs either a half-time or full-time health provider, such as a Nurse Practitioner or Physician's Assistant, and mental health clinician. During the 2013-2014 school year, the Seattle SBHC program served 6,540 students, primarily racial minority (69% non-White) and low-SES (59% eligible for free/reduced lunch). Of 33,864 total student visits to SBHCs, 14,365 (42%) were for mental health services. The presence of such SBHCs, which provide mental health service to 13% of all Seattle public high school students, creates an extraordinary opportunity for SMART Center faculty and dedicated SBMH practitioners and their leaders to collaborate on quality improvement activities focused on training and implementation as well as evaluation and research.
SMART Center faculty have worked with the mental health providers working within SBHCs for over 10 years to provide training and consultation on practice models and implementation supports with high potential for effectiveness. Most recently, this training and implementation support has focused on use of flexible, evidence-based emotional and behavioral health treatment (Lyon, Charlesworth-Attie, Vander Stoep, & McCauley, 2011) as well as assessment and progress monitoring (Lyon, Ludwig, Knaster Wasse, Bergstrom, Hendrix, & McCauley, in press). Most recently, our focus on data-based decision making has taken the form of consultation with school-based providers on computerized measurement feedback systems that support mental health intervention (Lyon, Knaster Wasse, Ludwig, Zachry, Bruns, Unützer, & McCauley, in press).
UW evaluated the associations between Seattle's SBHC primary care and mental health services on student academic performance and attendance (Walker et al., 2010). A quasi-experimental statistically controlled analysis comparing SBHC users to non-users found small but significant and positive associations between SBHC physical health service use and increased school attendance, and SBHC mental health service use and GPA. This differential finding is consistent with the argument that the impact of universally-available services such as SBHCs can be best identified through subgroup analyses—for instance, chronic physical conditions that lead to high absenteeism may be addressed through the SBHC physical health service use (Geierstanger et al., 2004). However, an additional study, also quasi-experimental and statistically controlling for service use, did not find any support for a relationship between the risk of dropout and SBHC service use (Kerns et al., 2011). Taken together, these studies illustrate the utility of school-researcher partnerships in examining the impact of school programming on student outcomes, especially given barriers related to the naturalistic, scientifically uncontrolled nature of school settings.
Intensive Tier 3 care coordination model
To address high-need middle school youth experiencing a combination of academic and behavioral health risk factors, members of the SMART Center team collaborated with SPS, an independent foundation, and a community-based mental health service organization to integrate behavioral health services into schools’ existing support systems through the implementation of three levels of behavioral health service: Short-term crisis intervention, assessment and referral to external mental health services, and team-based wraparound care coordination. Students were included in the intensive care coordination condition based on their high risk for disciplinary actions, academic failure, and the presence of behavioral health issues that may have been contributing to these problems. Evaluation of the intensive intervention suggested that the highest-risk youth (e.g., students who had failed at least one academic course in the semester prior to the baseline assessment) were less likely to experience future severe problems, such as subsequent course failures, relative to students recruited from comparable control schools. Analyses also identified disparities in the receipt of specialty mental health sector services for children whose parents were not native English speakers (Cutler, Lyon, Thompson, Vander Stoep, & McCauley, 2012).
Discussion
Federal reports and education-focused funding agencies have encouraged researcher-practitioner partnerships as a strategy for promoting effective use of research and data-informed strategies (IES, 2010). Such collaboration organizes practitioners and researchers to investigate problems confronted in education practice, explore solutions for improving student outcomes, and address the needs of educators, policymakers, students, parents, and community members (Coburn & Turner, 2012). With respect to MEB problems experienced by students – and their impacts on academic success – research and data can be applied in a range of ways to systematically develop, select, test, analyze, and refine interventions and solutions. Moreover, they can also be organized into comprehensive strategies using overarching frameworks such as the public health model and MTSS. As described in this paper, this is the agenda that has emerged from the collaboration between Seattle Public Schools and SMART Center.
At the same time, it is important to recognize that research-practitioner partnerships inevitably will be undertaken within a context that is unique to the local community, whether it is a classroom, school, district, or state. MTSS are not built de novo based on an idealized model and suite of interventions and strategies. Rather, researchers, practitioners, and community members must work to solve unique problems and priorities, leverage indigenous helpers, and take advantage of local opportunities and resources.
Recommendation 1: Attend to Context
Thus, one of the first and most obvious lessons from our collaborative effort to develop an effective continuum of behavioral health services and supports in Seattle schools is that the nature of this work will always be driven by local needs, resources, and priorities. In Seattle, for example, the Families and Education Levy – and Seattle's network of SBHCs – provides an extraordinary resource, and changes the context for implementation of MTSS and overall quality improvement agendas. The availability of SBMH clinicians means that other staff persons serving middle and high schools, such as school nurses, psychologists, and counselors, may serve different roles than in schools with no SBMH clinicians, and may benefit from different kinds of training and support. The FSW program is a unique resource that is poised to help multi-stressed families support their students to succeed in school, but evaluation of the program identified that FSWs could more strategically intervene in ways that use data, are based on research-based practices, and align with the MTSS model. Racial disproportionality in student discipline presents the partnership with another, very specific, “problem of practice” on which research and data now must be focused.
Recommendation 2: Organize Strategies into a Widely Recognized Framework
In complex environments such as school systems, use of clear organizing frameworks can enhance staff understanding and buy-in to change processes and strategies, and facilitate communication about expectations and decision-making (Chorpita & Daleiden, 2010). In our work with school systems such as Seattle's, we have found MTSS – and the accompanying “triangle” depiction of universal, targeted, and intensive supports – as a useful framework and source of common terminology and one that meshes easily with the public health approach (Figure 1). Using such a common framework that extends from federal mandate is extremely useful in helping diverse stakeholders understand how a school system is applying research-based strategies (as shown in Figure 2 for the SPS-SMART collaboration) and make complex decisions, such as (1) choosing critical components of MEB support for students at each tier in the MTSS framework; (2) identifying systems changes needed to support a three-tier MTSS; and (3) developing guidelines and curricula to assist with training school and SBMH personnel on necessary skills to implement services and supports across the three-tier model.
Figure 2.
Summary of selected SMART center projects across the multiple tiers of school supports.
Recommendation 3: Stay Connected to the Academic Mission of Schools
The mental health and academic scientific literature bases have largely emerged independently from one another. Indeed, even the majority of school mental health research has failed to incorporate relevant academic outcomes (Hoagwood & Johnson, 2003). Consequently, the relevance of school mental health practices to academic outcomes is not clearly understood, leaving many educators to question whether resources and time should be devoted to these practices. To better understand the merits of school mental health programs, these practices must be consistently integrated into the academic mission of schools, and clear linkages between school mental health practices and educational outcomes must be provided in order for stakeholders to understand that mental wellness is essential for young people to become truly college, career, and life ready.
Recommendation 4: Mobilize Knowledge from Implementation Science
Because much of our collaborative effort focuses on appropriate use of research evidence, the SMART Center endorses and actively pursues the implementation science research agenda recently articulated by Owens and colleagues (2014) surrounding professional development and coaching. For example, how much coaching is necessary following training to produce sustained practitioner behavior change? To what extent do different dimensions of integrity (e.g., model adherence, practitioner competence) differentially predict student outcomes? Given the academic calendar, what is an appropriate timeline for new practice sustainment in SBMH? Driven by mounting evidence for the importance of aspects of the organizational implementation context in the successful installation of evidence-based programs (e.g., Aarons, Ehrhart, & Farahnak, 2014) and the unique characteristics of the education sector (Owens et al., 2014), SMART Center faculty are exploring the influence of school and district climate, leadership, and school personnel characteristics on implementation success. Moreover, given resource limitations in the education sector, SMART Center researchers necessarily are focused on developing efficient implementation strategies geared toward producing “good enough” outcomes with relatively low cost (Owens et al., 2014).
Recommendation 5: Take Advantage of Opportunities to Integrate Care
In the context of recent federal policy shifts that prioritize mental and physical health parity, information sharing, and integration of services, traditional specialty mental health is likely to be de-emphasized in favor of more accessible and unified alternative service sectors (Hoagwood, 2013). Collaborative care models represent one effective approach to reorganize service systems to decrease healthcare costs, increase service accessibility, and improve intervention quality through the integration of mental health and primary care. A large body of research supports the effectiveness of collaborative care models for adults (e.g., Gilbody et al., 2006; Thota et al., 2012), and an emerging literature has examined the applicability of collaborative care to youth (e.g., Kolko et al., 2014; Richardson et al., in press). Although most of this work has focused on primary care, the education sector may be a more appropriate analog for the accessibility that primary care offers to adults. In addition, given that academic problems are likely to co-occur with both physical and mental health difficulties (McLeod, Uemura, & Rohrman, 2012), collaborative care in schools will need to attend to the additional dimension of educational health (e.g., academic engagement and performance) in order to be effective and contextually relevant. The SMART Center is therefore committed to advancing models that support the development, evaluation, and scale-up service integration models across the fragmented domains of physical, mental, and educational health, and adapting existing collaborative care models where necessary to meet the needs of youth, families, providers, and school systems (Eber, Hyde, & Suter, 2011).
Recommendation 6: Facilitate Communication Across Teams and Providers
New frameworks for coordinating SBMH services, such as the Interconnected Systems Framework (Barrett, Eber, & Weist, 2013), have illuminated the necessity of educational and mental health providers to use their resources wisely and collaboratively. A recent meeting in one school illuminated how, for example, PBIS and SBMH resources were being deployed separately. While a team from the SMART Center and the school's SBMH staff met to discuss progress on a Tier 2 mental health intervention, school staff were meeting with a district administrator and PBIS intervention specialist in a separate room. With foresight and better planning, these teams could have been meeting together and more effectively communicating and coordinating efforts. As proposed by those at the National Technical Assistance Center on PBIS (2014), school and agency providers should complete an inventory of the school's committees, their intended purposes, their staffing arrangements, and resources allocated for the committees in order to facilitate better interaction and communication among providers and productively assign resources to integrated services, reduce redundancy in committee work, and more efficiently use staff time and expertise.
Recommendation 7: Use Indigenous Helpers
Collaboration with and appropriate referral to outside providers is a key characteristic of an effective system of school supports for students with MEB problems (Barrett, Eber, & Weist, 2013). At the same time, numerous professionals naturally exist within schools who can be oriented to delivering mental health services in an MTSS model as a way to improve efficiency and integration into the school context. Clinicians working in SBMH clinics, school social workers, nurses, school psychologists, and school counselors all have professional training to support a range of MEB interventions and address the functioning of all students at all levels of MTSS. SMART Center faculty are working with school psychologists to streamline their assessment practices and free up their capacity to deliver intervention services and consult with other professionals working in schools. SPS administrators have now identified school counselors, social workers, and school nurses as targets of specific training (e.g., on the BRISC model) to efficiently and appropriately implement “stepped care” strategies that involve assessment, student engagement, and strategy selection, including referral to other providers within or outside the school who have expertise relevant to the student's specific MEB need. Additionally, teachers and instructional assistants can be active participants in universal programs that teach and reinforce social behavior. Counselors, teachers on special assignment, and assistant administrators are often primary deliverers of Tier 2 intervention such as Check and Connect (Cheney et al. 2009; Filter et al., 2007). With efficient modeling, coaching, and supervision of staff implementing interventions, professionals already working in schools across a full range of roles can improve the overall capacity of schools to prevent and treat students’ MEB problems (Graczyk, Domitrovich, & Zins, 2003).
Recommendation 8: Build an “Evidence-Based System” of School Supports
As scientist-practitioners, faculty in the SMART Center are committed to leveraging the explosion in published literature on prevention programs, treatment models, and school-based strategies that has accompanied the EBP movement of the past two decades. The complexity of applying science to practice is persistent, however, as are barriers to implementing EBPs. To ensure that our quest to provide a range of empirically supported strategies across all tiers of support is not overwhelming, communicating a set of touchstone principles for building “evidence-based systems” (Chorpita & Daleiden, 2010) can be helpful.
An evidence-based system is one that organizes decision-making around the use of data and evidence, with the goal of improving quality and outcomes (Daleiden & Chorpita, 2005). It is committed to an empirical epistemology that relies on objective and verifiable evidence for making decisions, such as use of data on progress for an individual student, selection of strategies in the MTSS framework based on research, and/or commitment to evaluating novel and unique strategies (as we have done for BRISC, the SBHC initiative, and the FSW program). Second, such a system will be characterized by parsimony and efficiency. Examples include standardized screening and assessment tools, training practitioners on modularized and relevant applications of EBP (as in BRISC), and promoting “dashboard” views of a student's progress for supervision purposes. Finally, an evidence-based system will emphasize transparency and visibility, such as through manualized procedures, common organizing frameworks (such as MTSS), and agreed-upon metrics, such as discipline disproportionality. While referring to such principles will not, in and of itself, improve student outcomes, it can be a useful way to orient collaborators to the SMART Center approach and maintain focus in the face of complex systems change efforts.
Recommendation 9: Account for Diversity and Strive for Social Justice
An ideal social function of education is to serve as Horace Mann's “great equalizer,” but the evidence is mixed, and schools may replicate or even magnify society's gross racial and ethnic disproportionality. Asians and Whites consistently outperform their counterparts in standardized test scores, grades, and graduation rates, and they are far less likely to have a disciplinary action or referral to juvenile justice (Finn & Servoss, 2013; Skiba et al., 2011; Toldson, McGee, & Lemmons, 2013). Racial and ethnic minorities are also less likely than Whites to use SBMH services, with those who do beginning at a later age (Wood et al., 2005). Poverty also plays a major role in school success; our work in Seattle elementary schools revealed a nearly perfect negative relationship (r = −.92) between school-level percentage of children who were qualified for free or reduced meals and percentage of children who passed their standardized tests. These disparities are so great and carry such meaningful ramifications on the development and functioning of society that it is clear to us that even “objective scientists” cannot remain neutral. The SMART Center is therefore committed to understanding and addressing racial, ethnic, and social justice. This includes the analytic disaggregation of our findings by race and poverty, a focus on school programs and supports that are theoretically connected to inequities, and working with schools to consider their policies, practices, and procedures through a lens of cultural sensitivity and social justice.
Recommendation 10: Expand the Knowledge Base
Children spend much of their time in schools. Evidence is strong that school-based interventions can support positive social-emotional outcomes, which are related to academic success as well as healthy transitions to adulthood. However, the magnitude of the opportunity dwarfs the extant research base (Fazel et al., 2014). Thus, the SMART Center's partnerships with local school systems focus on both improving student outcomes at home while also filling gaps in the overall school mental health research base. Through the projects described above, we have the potential to fill a range of critical school-based research gaps, including:
Determining the most efficient, effective, and acceptable screening and assessment strategies to promote prevention and early identification of MEB disorders;
Effective and efficient application of community-based EBPs to the school context;
Strategies for preparing a diverse school-based workforce to prevent and treat MEB problems in youth;
Measuring and addressing crucial school-level organizational factors to target in implementation efforts;
Appropriate use of indigenous helpers (e.g., teachers, nurses, school counselors, FSP workers) to screen, refer, and intervene in MEB problems in youth;
Models for integrating the health, mental health, and education missions of schools;
Cost-effectiveness of specific strategies and combinations of strategies; and
Classroom-, school- and district-level strategies for reducing disproportionality in discipline.
Conclusion
If our ultimate goal is to provide all children and adolescents with access to the most effective and appropriate options for preventing and treating MEB disorders, population-based strategies in the schools may represent the best such opportunity our society has. As described in this paper, there are a range of ways in which academic-school partnerships can leverage the complementary strengths of the public health model and the evidence-based practice movement in children's behavioral health to make the most of this opportunity. However, we agree with the conclusion voiced by Fazel and colleagues (2014) that public and political will are needed to ensure that the evidence base is successfully implemented. To use the phrase applied to the recent federal initiative to ensure that schools are “sanctuaries for teaching and learning,” now is the time for redoubled commitment to research and action on school mental health.
Acknowledgments
This publication was supported in part by funding from grant number R305A120128 awarded by the Institute of Education Sciences and grant K08 MH095939 awarded by the National Institute of Mental Health (NIMH). We thank Seattle Public Schools, Public Health of Seattle-King County, and Seattle's school mental health providers for fostering an effective research-practitioner partnership, and Ricki Mudd for help with manuscript preparation.
Contributor Information
Eric J. Bruns, University of Washington School of Medicine
Mylien T. Duong, University of Washington School of Medicine
Aaron R. Lyon, University of Washington School of Medicine
Michael D. Pullmann, University of Washington School of Medicine
Clayton R. Cook, University of Washington College of Education
Douglas Cheney, University of Washington College of Education.
Elizabeth McCauley, University of Washington School of Medicine.
References
- Aarons GA, Ehrhart MG, Farahnak LR. The Implementation Leadership Scale (ILS): Development of a brief measure of unit level implementation leadership. Implementation Science. 2014;9(1):45–45. doi: 10.1186/1748-5908-9-45. doi: 10.1186/1748-5908-9-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychological Association Zero Tolerance Task Force Are zero tolerance policies effective in the schools? An evidentiary review and recommendations. American Psychologist. 2008;63:852–862. doi: 10.1037/0003-066X.63.9.852. doi: 10.1037/0003-066X.63.9.852. [DOI] [PubMed] [Google Scholar]
- Balfanz R, Byrnes V, Fox J. Sent home and put off-track: The antecedents, disproportionalities, and consequences of being suspended in the ninth grade. The Center for Civil Rights Remedies; 2013. http://civilrightsproject.ucla.edu/resources/projects/center-for-civil-rights-remedies/school-to-prison-folder/state-reports/sent-home-and-put-off-track-the-antecedents-disproportionalities-and-consequences-of-beingsuspended-in-the-ninth-grade. [Google Scholar]
- Banks JA. An introduction to multicultural education. 5th Ed. Pearson; New York, NY: 2013. [Google Scholar]
- Barrett S, Eber L, Weist M. Advancing education effectiveness: Interconnecting school mental health and school-wide positive behavior support. 2013 Retrieved from http://www.pbis.org/common/pbisresources/publications/Final-Monograph.pdf.
- Brackett MA, Reyes MR, Rivers SE, Elbertson NA, Salovey P. Assessing teachers’ beliefs about social and emotional learning. Journal of Psychoeducational Assessment. 2012;30(3):219–236. [Google Scholar]
- Bruns EJ, Lyon AR, McCauley EM. Developing and Testing a Brief, Targeted, Evidence-Informed “Tier 2” MH Intervention for Use in Schools.. Paper presented at the 18th Annual Conference on Advancing School Mental Health; Alexandria, VA.. 2013. [Google Scholar]
- Burns MK, Coolong-Chaffin M. Response to intervention: The role of and effect on school psychology. School Psychology Forum. 2006;1:3–15. [Google Scholar]
- Cabus SJ, De Witte K. Does school time matter?—On the impact of compulsory education age on school dropout. Economics of Education Review. 2011;30(6):1384–1398. doi: 10.1016/j.econedurev.2011.07.003. [Google Scholar]
- Calear AL, Christensen H. Systematic review of school-based prevention and early intervention programs for depression. Journal of Adolescence. 2010;33:429. doi: 10.1016/j.adolescence.2009.07.004. doi: 10.1016/j.adolescence.2009.07.004. [DOI] [PubMed] [Google Scholar]
- Cappella E, Frazier SL, Atkins MS, Schoenwald SK, Glisson C. Enhancing schools' capacity to support children in poverty: An ecological model of school-based mental health services. Administration and Policy in Mental Health and Mental Health Services Research. 2008;35(5):395–409. doi: 10.1007/s10488-008-0182-y. doi: 10.1007/s10488-008-0182-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cash RE, Nealis LK. Mental health in the schools: It's a matter of public policy.. Paper presented at the National Association of School Psychologists Public Policy Institute; Washington, DC.. 2004. [Google Scholar]
- Castellanos N, Conrod P. Brief interventions targeting personality risk factors for adolescent substance misuse reduce depression, panic and risk-taking behaviours. Journal of Mental Health. 2006;15(6):645–658. [Google Scholar]
- Cheney DA, Stage SA, Hawken LS, Lynass L, Mielenz C, Waugh M. A 2-year outcome study of the check, connect, and expect intervention for students at risk for severe behavior problems. Journal of Emotional and Behavioral Disorders. 2009;17(4):226–243. [Google Scholar]
- Chorpita BF, Daleiden EL. Building evidence-based systems in children's mental health. In: Kazdin AE, Weisz JR, editors. Evidence-Based Psychotherapies for Children and Adolescents. Oxford; New York: 2010. pp. 482–499. [Google Scholar]
- Coburn CE, Turner EO. Research on data use: A framework and analysis. Measurement: Interdisciplinary Research and Perspectives. 2012;9(4):173–206. [Google Scholar]
- Conservative Caucus Stop mandatory “psychiatric “mental health” testing. 2004 Retrieved from http://www.conservativeusa.org/mentaltesting.htm.
- Cook C, Lyon AR, Kubergovic D, Browning-Wright D, Zhang A Supportive Beliefs Intervention to facilitate the implementation of evidence-based practices within a multi-tiered system of supports. School Mental Health. in press. [Google Scholar]
- Cook C, Williams KR, Guerra NG, Kim T, Sadek S. Predictors of childhood bullying and victimization: A meta-analytic review. School Psychology Quarterly. 2010;25:65–83. [Google Scholar]
- Cook CR, Volpe R, Livanis A. Universal screening beyond academics: Introduction to the special series. Assessment for Effective Intervention. 2010;35:195–196. [Google Scholar]
- Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Archives of General Psychiatry. 2003;60(8):837–844. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- Cutler J, Lyon AR, Thompson K, Vander Stoep A, McCauley E. Disparities in children’s mental health service use: The impact of language spoken. Emotional and Behavioral Disorders in Youth. 2012;12(64-69) [Google Scholar]
- Daleiden EL, Chorpita BF. From data to wisdom: Quality improvement strategies supporting large-scale implementation of evidence-based services. Child and Adolescent Psychiatric Clinics of North America. 2005;14(2):329–349. doi: 10.1016/j.chc.2004.11.002. doi: 10.1016/j.chc.2004.11.002. [DOI] [PubMed] [Google Scholar]
- Durlak JA, Weissberg RP, Dymnicki AB, Taylor RD, Schellinger KB. The impact of enhancing students' social and emotional learning: A meta-analysis of school-based universal interventions. Child Development. 2011;82:405–432. doi: 10.1111/j.1467-8624.2010.01564.x. doi: 10.1111/j.1467-8624.2010.01564.x. [DOI] [PubMed] [Google Scholar]
- Eakman BK. What? Are you crazy? The screening America. Chronicles Magazine; 2004. [January 17, 2005]. from www.chroniclesmagazine.org. [Google Scholar]
- Eber L, Hyde K, Suter JC. Integrating wraparound into a schoolwide system of positive behavior supports. Journal of Child and Family Studies. 2011;20(6):782–790. [Google Scholar]
- Evans SW, Weist MD. Implementing empirically supported treatments in the schools: What are we asking? Clinical Child and Family Psychology Review. 2004;7:263–267. doi: 10.1007/s10567-004-6090-0. doi: 10.1007/s10567-004-6090-0. [DOI] [PubMed] [Google Scholar]
- Fabelo T, Thompson MD, Plotkin M, Carmichael D, Marchbanks MPI, A., B. E. Breaking schools’ rules: A statewide study of how school discipline relates to students’ success and juvenile justice involvement. Council of State Governments Justice Center; New York, NY: 2011. [Google Scholar]
- Farahmand FK, Grant KE, Polo AJ, Duffy SN, DuBois DL. School-based mental health and behavioral programs for low-income, urban youth: A systematic and meta-analytic review. Clinical Psychology-Science and Practice. 2011;18:372–390. doi: 10.1111/j.1468-2850.2011.01265.x. [Google Scholar]
- Farmer EMZ, Burns BJ, Phillips SD, Angold A, Costello EJ. Pathways into and through mental health services for children and adolescents. Psychiatric Services. 2003;54:60–66. doi: 10.1176/appi.ps.54.1.60. doi: 10.1176/appi.ps.54.1.60. [DOI] [PubMed] [Google Scholar]
- Fazel M, Hoagwood K, Stephan S, Ford T. Mental health interventions in schools in high-income countries. The Lancet Psychiatry. 2014;1(5):377–387. doi: 10.1016/S2215-0366(14)70312-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fergusson DM, Boden JM, Horwood LJ. Recurrence of major depression in adolescence and early adulthood, and later mental health, educational and economic outcomes. The British Journal of Psychiatry. 2007;191(4):335–342. doi: 10.1192/bjp.bp.107.036079. [DOI] [PubMed] [Google Scholar]
- Filter KJ, McKenna MK, Benedict EA, Homer RH, Todd AW, Watson J. Check in/Check out: A post-hoc evaluation of an efficient, secondary-level targeted intervention for reducing problem behaviors in schools. Education & Treatment of Children. 2007;30(1):69–84. [Google Scholar]
- Finn JD, Servoss TJ. Misbehavior, Suspensions, and Security Measures in High School: Racial/Ethnic and Gender Differences.. Paper presented at the National Conference on Race and Gender Disparities in Discipline.2013. [Google Scholar]
- Forman SG, Shapiro ES, Codding RS, Gonzales JE, Reddy LA, Rosenfield SA, et al. Implementation science and school psychology. School Psychology Quarterly. The Official Journal Of The Division Of School Psychology, American Psychological Association. 2013;28:77–100. doi: 10.1037/spq0000019. doi: 10.1037/spq0000019. [DOI] [PubMed] [Google Scholar]
- Geierstanger SP, Amaral G, Mansour M, Walters SR. School-based health centers and academic performance: Research, challenges, and recommendations. Journal of School Health. 2004;74(9):347–352. doi: 10.1111/j.1746-1561.2004.tb06627.x. [DOI] [PubMed] [Google Scholar]
- Gilbody S, Bower P, Fletcher J, Richards D, Sutton AJ. Collaborative care for depression: a cumulative meta-analysis and review of longer-term outcomes. Archives Of Internal Medicine. 2006;166(21):2314–2321. doi: 10.1001/archinte.166.21.2314. [DOI] [PubMed] [Google Scholar]
- Gillette M, Boyle-Baise M. Multicultural education at the graduate level: Assisting teachers in developing multicultural perspectives.. Paper presented at the annual meeting of the American Education Research Association; San Francisco, CA.. Apr, 1995. [Google Scholar]
- Graczyk PA, Domitrovich CE, Zins JE. Facilitating the implementation of evidence-based prevention and mental health promotion efforts in schools. In: Weist MD, Evans SW, Lever NA, editors. Handbook of school mental health: Advancing practice and research. Kluwer Academic/Plenum Publishers; New York, NY, US: 2003. pp. 301–318. [Google Scholar]
- Greif Green J, McLaughlin KA, Alegría M, Costello EJ, Gruber MJ, Hoagwood K, et al. School mental health resources and adolescent mental health service use. Journal of the American Academy of Child & Adolescent Psychiatry. 2013;52:501–510. doi: 10.1016/j.jaac.2013.03.002. doi: 10.1016/j.jaac.2013.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gresham FM. Conceptualizing behavior disorders in terms of resistance to intervention. School Psychology Review. 1991;20:23–36. [Google Scholar]
- Gresham FM. Response to intervention: An alternative means of identifying students as emotionally disturbed. Education & Treatment of Children. 2005;28(4):328–344. [Google Scholar]
- Hoagwood K, Johnson J. School psychology: A public health framework I. From evidence-based practices to evidence-based policies. Journal of School Psychology. 2003;41(1):3–21. [Google Scholar]
- Hoagwood KE. Don't mourn: Organize. Reviving mental health services research for healthcare quality improvement. Clinical Psychology: Science and Practice. 2013;20(1):120–126. [Google Scholar]
- Hoagwood KE, Olin SS, Kerker BD, Kratochwill TR, Crowe M, Saka N. Empirically based school interventions targeted at academic and mental health functioning. Journal of Emotional and Behavioral Disorders. 2007;15(2):66–92. [Google Scholar]
- Homer JB, Hirsch GB. System dynamics modeling for public health: Background and opportunities. American Journal of Public Health. 2006;96(3):452–458. doi: 10.2105/AJPH.2005.062059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute for Education Sciences Researcher-Practitioner Partnerships in Education Research. 2012 Downloaded November 4, 2014 from http://ies.ed.gov/funding/pdf/2013_84305H.pdf.
- Kerns SEU, Pullmann MD, Walker SC, Lyon AR, Cosgrove TJ, Bruns EJ. Adolescent use of school-based health centers and high school dropout. Archives of Pediatrics & Adolescent Medicine. 2011;165(7):617. doi: 10.1001/archpediatrics.2011.10. doi: 10.1001/archpediatrics.2011.10. [DOI] [PubMed] [Google Scholar]
- Kincaid D, Childs K, Blase KA, Wallace F. Identifying barriers and facilitators in implementing schoolwide positive behavior support. Journal of Positive Behavior Interventions. 2007;9(3):174–184. [Google Scholar]
- Klein J, Cornell D, Konold T. Relationships between bullying, school climate, and student risk behaviors. School Psychology Quarterly. 2012;27(3):154–169. doi: 10.1037/a0029350. [DOI] [PubMed] [Google Scholar]
- Kolko DJ, Campo J, Kilbourne AM, Hart J, Sakolsky D, Wisniewski S. Collaborative care outcomes for pediatric behavioral health problems: A cluster randomized trial. Pediatrics. 2014;133(4):e981–e992. doi: 10.1542/peds.2013-2516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuo E, Stoep AV, McCauley E, Kernic MA. Cost-effectiveness of a school-based emotional health screening program. Journal of School Health. 2009;79(6):277–285. doi: 10.1111/j.1746-1561.2009.00410.x. doi:10.1111/j.1746-1561.2009.00410.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leavell HR, Clark EG. Preventive medicine for the doctor in his community. 3rd ed. McGraw-Hill Book Company; New York, NY: 1965. [Google Scholar]
- Levitt JM, Saka N, Romanelli LH, Hoagwood K. Early identification of mental health problems in schools: The status of instrumentation. Journal of School Psychology. 2007;45(2):163–191. [Google Scholar]
- Lewis TJ, Sugai G. Effective behavior support: A systems approach to proactive schoolwide management. Focus on Exceptional Children. 1999;31(6):1–24. [Google Scholar]
- Lochman JE, Wells KC. The Coping Power program at the middle-school transition: Universal and indicated prevention effects. Psychology of Addictive Behaviors. 2002;16(4, Suppl):S40–S54. doi: 10.1037/0893-164x.16.4s.s40. [DOI] [PubMed] [Google Scholar]
- Losen DJ, Gillespie J. Opportunities suspended: The disparate impact of disciplinary exclusion from school. Civil Rights Project / Proyecto Derechos Civiles; Los Angeles, CA: 2012. [Google Scholar]
- Lyon AR, Borntrager C, Nakamura B, Higa-McMillan C. From distal to proximal: routine educational data monitoring in school-based mental health. Advances in School Mental Health Promotion. 2013;6(4):263–279. doi: 10.1080/1754730X.2013.832008. doi: 10.1080/1754730x.2013.832008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyon AR, Bruns EJ, Ludwig K, Vander Stoep A, Pullmann MD, Eaton J, et al. The Brief Intervention for School Clinicians (BRISC): An initial evaluation of feasibility, acceptability, and contextual appropriateness. doi: 10.1007/s12310-015-9153-0. in submission. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyon AR, Bruns EJ, Weathers ES, Canavas N, Ludwig K, Vander Stoep A, et al. Taking evidence-based practices to school: Using expert opinion to develop a brief, evidence-informed school-based mental health intervention. Advances in School Mental Health Promotion. 2014;7(1):42–61. [Google Scholar]
- Lyon AR, Charlesworth-Attie S, Stoep A, McCauley E. Modular psychotherapy for youth with internalizing problems: Implementation with therapists in school-based health centers. School Psychology Review. 2011;40(4):569–581. [Google Scholar]
- Lyon AR, Knaster Wasse J, Ludwig K, Zachry M, Bruns EJ, Unützer J, McCauley E. The Contextualized Technology Adaptation Process (CTAP): Optimizing health information technology to improve mental health systems. doi: 10.1007/s10488-015-0637-x. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyon AR, Ludwig K, Knaster Wasse J, Bergstrom A, Hendrix E, McCauley E. Determinants and functions of standardized assessment use among school mental health clinicians: A mixed methods evaluation. doi: 10.1007/s10488-015-0626-0. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyon AR, Ludwig K, Romano E, Koltracht J, Vander Stoep A, McCauley E. Using modular psychotherapy in school mental health: Provider perspectives on intervention-setting fit. Journal of Clinical Child & Adolescent Psychology. 2014;43(6):890–901. doi: 10.1080/15374416.2013.843460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyon AR, Ludwig K, Romano E, Leonard S, Vander Stoep A, McCauley E. “If it's worth my time, I will make the time”: School-based providers' decision-making about participating in an evidence-based psychotherapy consultation program. Administration and Policy in Mental Health and Mental Health Services Research. 2013;40(6):467–481. doi: 10.1007/s10488-013-0494-4. doi: 10.1007/s10488-013-0494-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyon AR, Maras M, Pate C, Igusa T, Vander Stoep A. Modeling the impact of school-based universal depression screening on additional service capacity needs: A system dynamics approach. doi: 10.1007/s10488-015-0628-y. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malloy JM, Drake J, Abate K, Cormier GM. The RENEW model of futures planning, resource development, and school-to-career experiences for youth with emotional or behavioral disorders. In: Cheney D, editor. Transition of secondary students with emotional or behavioral disorders: Current approaches for positive outcomes. 2nd ed. Research Press; Champaign, IL: 2010. pp. 267–304. [Google Scholar]
- McLeod JD, Uemura R, Rohrman S. Adolescent mental health, behavior problems, and academic achievement. Journal of Health and Social Behavior. 2012;53(4):482–497. doi: 10.1177/0022146512462888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore KA, Redd Z, Burkhauser M, Mbwana K, Collins A. Children in poverty: Trends, consequences, and policy options. Child Trends; Washington, DC: 2009. [Google Scholar]
- Nabors LA, Reynolds MW. Program evaluation activities: Outcomes related to treatment for adolescents receiving school-based mental health services. Children's Services: Social Policy, Research, and Practice. 2000;3:175–189. [Google Scholar]
- National Center on Response to Intervention . Essential components of RTI – A closer look at Response to Intervention. U.S. Department of Education, Office of Special Education Programs, National Center on Response to Intervention; Washington, DC: Mar, 2010. [Google Scholar]
- National Technical Assistance Center on Positive Behavioral Interventions and Supports National Technical Assistance Center on Positive Behavioral Interventions and Supports. 2014 2014. Retrieved from http://www.pbis.org/about_us/default.aspx.
- Neil AL, Christensen H. Efficacy and effectiveness of school-based prevention and early intervention programs for anxiety. Clinical Psychology Review. 2009;29(3):208–215. doi: 10.1016/j.cpr.2009.01.002. [DOI] [PubMed] [Google Scholar]
- Nielsen MBD, Madsen IEH, Bültmann U, Christensen U, Diderichsen F, Rugulies R. Predictors of return to work in employees sick-listed with mental health problems: Findings from a longitudinal study. European Journal of Public Health. 2011;21(6):806–811. doi: 10.1093/eurpub/ckq171. [DOI] [PubMed] [Google Scholar]
- Owens JS, Lyon AR, Brandt NE, Warner CM, Nadeem E, Spiel C, Wagner M. Implementation science in school mental health: Key constructs in a developing research agenda. School Mental Health. 2014;6(2):99–111. doi: 10.1007/s12310-013-9115-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pianta RC, LaParo KM, Hamre BK. Classroom Assessment Scoring System (CLASS) Pre-K Version. Brookes Publishing; Baltimore, MD: 2008. [Google Scholar]
- Proctor E, Silmere H, Raghavan R, Hovmand P, Aarons G, Bunger A, et al. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Administration and Policy in Mental Health. 2011;38:65–76. doi: 10.1007/s10488-010-0319-7. doi: 10.1007/s10488-010-0319-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prodente CA, Sander MA, Weist MD. Furthering support for expanded school mental health programs. Children's Services: Social Policy, Research, & Practice. 2002;5(3):173–188. [Google Scholar]
- Pullmann MD, Ague S, Johnson T, Lane S, Beaver K, Jetton E, Rund E. Defining engagement in adolescent substance abuse treatment. American Journal of Community Psychology. 2013;52:347–358. doi: 10.1007/s10464-013-9600-8. doi: 10.1007/s10464-013-9600-8. [DOI] [PubMed] [Google Scholar]
- Pullmann MD, VanHooser S, Hoffman C, Heflinger CA. Barriers to and supports of family participation in a rural system of care for children with serious emotional problems. Community Mental Health Journal. 2010;46(3):211–220. doi: 10.1007/s10597-009-9208-5. doi: 10.1007/s10597-009-9208-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pullmann MD, Weathers ES, Hensley S, Bruns EJ. Academic outcomes of an elementary school-based family support programme. Advances in School Mental Health Promotion. 2013;6(4):231–246. [Google Scholar]
- Rathvon N. Effective school interventions: Evidence-based strategies for improving student outcomes. Guilford Press; New York, NY: 2008. [Google Scholar]
- Reinke WM, Lewis-Palmer T, Merrell K. The Classroom Check-Up: A classwide teacher consultation model for increasing praise and decreasing disruptive behavior. School Psychology Review. 2008;37(2):315–332. [PMC free article] [PubMed] [Google Scholar]
- Richardson L, Ludman E, McCauley E, Lindenbaum J, Clarke G, Brent D, et al. Collaborative care for adolescents with depression in primary care: A randomized clinical trial. Journal of the American Medical Association. doi: 10.1001/jama.2014.9259. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romer D, McIntosh M. The roles and perspectives of school mental health professionals in promoting adolescent mental health. In: Evans DL, Foa EB, Gur RE, Hendin H, O'Brien CP, Seligman MEP, Walsh T, editors. Treating and preventing adolescent mental health disorders: What we know and what we don't know: A research agenda for improving the mental health of our youth. Oxford University Press; New York, NY: 2005. pp. 597–615. [Google Scholar]
- Rones M, Hoagwood K. School-based mental health services: A research review. Clinical Child and Family Psychology Review. 2000;3(4):223–241. doi: 10.1023/a:1026425104386. [DOI] [PubMed] [Google Scholar]
- Sayal K, Owen V, White K, Merrell C, Tymms P, Taylor E. Impact of early school-based screening and intervention programs for ADHD on children's outcomes and access to services: follow-up of a school-based trial at age 10 years. Archives Of Pediatrics & Adolescent Medicine. 2010;164:462–469. doi: 10.1001/archpediatrics.2010.40. doi: 10.1001/archpediatrics.2010.40. [DOI] [PubMed] [Google Scholar]
- Skiba RJ, Horner RH, Chung C-G, Rausch MK, May SL, Tobin T. Race is not neutral: A national investigation of African American and Latino disproportionality in school discipline. School Psychology Review. 2011;40(1):85–107. [Google Scholar]
- Shinn MR, Walker HM, editors. Interventions academic and behavior problems in a three-tier model, including Response-to-Intervention. National Association of School Psychologists; Bethesda, MD: 2010. [Google Scholar]
- Stein B, Jaycox L, Kataoka S, et al. Mental health intervention for schoolchildren exposed to violence. A randomized controlled trial. Journal of the American Medical Association. 2003;290:603–611. doi: 10.1001/jama.290.5.603. [DOI] [PubMed] [Google Scholar]
- Suldo SM, Gormley MJ, DuPaul GJ, Anderson-Butcher D. The impact of school mental health on student and school-level academic outcomes: Current status of the research and future directions. School Mental Health. 2014;6(2):84–98. [Google Scholar]
- Thota AB, Sipe TA, Byard GJ, Zometa CS, Hahn RA, McKnight-Eily LR, et al. Collaborative care to improve the management of depressive disorders: A community guide systematic review and meta-analysis. American Journal of Preventive Medicine. 2012;42(5):525–538. doi: 10.1016/j.amepre.2012.01.019. [DOI] [PubMed] [Google Scholar]
- Tobler NS, Roona MR, Ochshorn P, Marshall DG, Streke AV, Stackpole KM. School-based adolescent drug prevention programs: 1998 meta-analysis. The Journal of Primary Prevention. 2000;20(4):275–336. [Google Scholar]
- Toldson IA, McGee T, Lemmons BP. Reducing Suspensions by Improving Academic Engagement among School-age Black Males.. Paper presented at the National Conference on Race and Gender Disparities in Discipline.2013. [Google Scholar]
- President's New Freedom Commission on Mental Health . Achieving the promise: Transforming mental health care in America. Department of Health and Human Services; Rockville, MD: 2003. Final report (DHHS Pub. No. SMA-03-3832) [Google Scholar]
- U.S. Department of Health and Human Services . Mental health: A report of the Surgeon General. National Institute of Mental Health; Rockville, MD: 1999. [Google Scholar]
- U.S. Department of Education Office for Civil Rights . Civil rights data collection: Data snapshot (School discipline) U.S. Department of Education; Washington, DC: 2014. [Google Scholar]
- Vander Stoep A, McCauley E, Thompson KA, Herting JR, Kuo ES, Stewart DG, et al. Universal emotional health screening at the middle school transition. Journal of Emotional and Behavioral Disorders. 2005;13(4):213–223. doi: 10.1177/10634266050130040301. doi: 10.1177/10634266050130040301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vander Stoep A, Weiss NS, Kuo ES, Cheney D, Cohen P. What proportion of failure to complete secondary school in the US population is attributable to adolescent psychiatric disorder? Journal of Behavioral Health Services & Research. 2003;30(1):119–124. doi: 10.1007/BF02287817. [DOI] [PubMed] [Google Scholar]
- VanDerHeyden AM, Witt JC, Gilbertson D. A multi-year evaluation of the effects of a Response to Intervention (RTI) model on identification of children for special education. Journal of School Psychology. 2007;45(2):225–256. [Google Scholar]
- Walker SC, Kerns SEU, Lyon AR, Bruns EJ, Cosgrove TJ. Impact of school-based health center use on academic outcomes. Journal of Adolescent Health. 2010;46(3):251–257. doi: 10.1016/j.jadohealth.2009.07.002. [DOI] [PubMed] [Google Scholar]
- Weist MD, Evans SW. Expanded school mental health: Challenges and opportunities in an emerging field. Journal of Youth and Adolescence. 2005;34:3–6. [Google Scholar]
- Wilson SJ, Lipsey MW. School-based interventions for aggressive and disruptive behavior: Update of a meta-analysis. American Journal of Preventive Medicine. 2007;33(2,Suppl):S130–S143. doi: 10.1016/j.amepre.2007.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong M. Interventions to reduce psychological harm from traumatic events among children and adolescents: A commentary on the application of findings to the real world of schools. American Journal of Preventive Medicine. 2008;35(4):398–400. doi: 10.1016/j.amepre.2008.07.002. [DOI] [PubMed] [Google Scholar]
- Wood PA, Yeh M, Pan D, Lambros KM, McCabe KM, Hough RL. Exploring the relationship between race/ethnicity, age of first school-based services utilization, and age of first specialty mental health care for at-risk youth. Mental Health Services Research. 2005;7(3):185–196. doi: 10.1007/s11020-005-5787-0. [DOI] [PubMed] [Google Scholar]
- Yeager DS, Purdie-Vaughns V, Garcia J, Apfel N, Brzustoski P, Master A, et al. Breaking the cycle of mistrust: Wise interventions to provide critical feedback across the racial divide. Journal of Experimental Psychology. 2014;143:804–824. doi: 10.1037/a0033906. doi: 10.1037/a0033906. [DOI] [PubMed] [Google Scholar]