Abstract
Partner notification is a widely accepted method whose intent is to limit onwards HIV transmission. With acceleration in the use of new technologies such as text-messaging, e-mail and social network sites, there has been growing interest in utilizing these techniques for “next-generation” HIV partner services (PS). We conducted a systematic review to assess the utilization and effectiveness of these technologies in HIV PS. Our literature search resulted in 1,343 citations, and 8 met our inclusion criteria. We found efforts focused in 3 domains: 1) patient-led anonymous referral online (n=3); 2) provider-led efforts to augment traditional partner notification techniques at public health departments (n=4); 3) a hybrid approach utilizing a website for e-notification available to those with confirmed STI through an STI clinic (n=1). For the provider-led efforts a modest increase in HIV case-finding was noted despite a generally lower rate of successful notification in comparison to traditional PS. The public websites had a high total number of e-notifications sent, but less than 10% of cards were sent for HIV. Furthermore, low awareness of these services was found in surveys amongat-risk target populations. When given a choice, the majority of clients chose to send an e-notification via text versus e-mail. Although successful notification may be lower overall, use of next-generation services provides an avenue to contact those that would previously have been untraceable. Additional research is needed to determine to what extent technology enhanced partner services improves identification of newly infected persons as well as initiating new prevention for HIV negative clients within high-risk networks.
Introduction
Partner notification (PN) and counseling – also known as partner services – has been in widespread use for the control of sexually transmitted infections (STIs) since the early 20th century, when it was formally initiated in response to gonorrhea and syphilis(1). Traditionally, PN for STIs has involved disease intervention specialists (DIS) identifying and contacting at-risk partners of newly infected patients using contact information such as house phone or address(2,3). Partners are then informed of their STI risk, provided testing and if they test positive, engaged in care.
With the expansion of new technologies such as text-messaging, internet hook-up and social networking sites, there has been a growing interest in harnessing these modalities for use in STI partner services. In the US, 74.4% of households report access to the internet(4), >90% of people report owning a cellphone and 64% a smartphone(5). In terms of STI risk, the internet has emerged as an important venue for seeking dating and sexual partners(6–8), particularly in high-risk populations such as MSM, where finding a partner online has been associated with condomless sex(9).
Use of next-generation techniques (internet and text notifications) for partner services is now recommended by the CDC as an adjunct to traditional programs(10). In Public Health Departments there appears to be widespread use with a recent US survey demonstrating that 74% of federally-funded STD programs had internet partner services (iPS) protocols in place(11). However, little is known about the effectiveness of these programs. Previous reviews of HIV partner services have included little data on next-generation techniques. A recent Cochrane review included only randomized or quasi-randomized controlled trials which do not capture a large proportion of the published experience surrounding next-generation partner services(12–14). In this systematic review we seek to assess what efforts using next-generation techniques for HIV partner services have been implemented and evaluate their effectiveness.
Methods
This systematic review was conducted according the PRISMA guidelines (Table S1)(15). We searched PubMed, PsychInfo, Scopus and the Cochrane Library for relevant articles employing a strategy combining the terms “Partner Notification/Partner Services/Contact Tracing,” “STI/HIV/AIDS” and “SMS/Texting/Internet/Social Media/Online” (full search strategy in Appendix A.) The search was last run on April 23, 2015. Our inclusion criteria were studies that: 1) Involve partner services for HIV, 2) Report primary data (no reviews or attitude surveys), and 3) Utilize next-generation techniques, defined as usage of text or internet-based strategies. US and international studies in English were included.
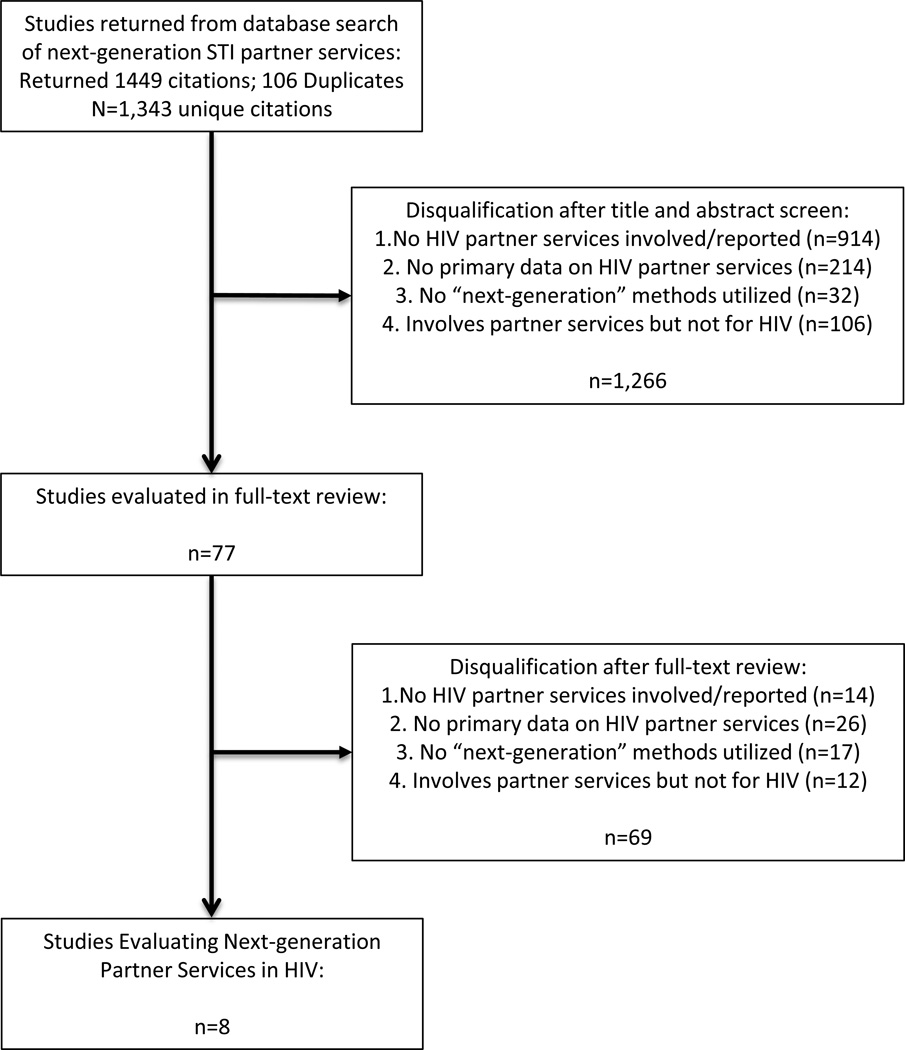
Eligible articles were compiled into a Microsoft Excel Database (version 14.4.8, Microsoft, Redmond, WA). An initial review of the titles and abstracts was undertaken by the first author, who marked articles as “eligible,” “ineligible,” or “uncertain” (Figure 1). For quality control, 10% of the initial articles were also screened by the senior author with high inter-rater agreement (κ= 0.92). Disagreements were re-reviewed with a final decision made by consensus of all authors. Articles marked as “eligible” or “uncertain” underwent a full-text review by the first author to assess for inclusion in the review.
Figure 1.
Study quality was assessed using the checklist from Downs and Black(16). The score is calculated across the following domains: reporting, external validity, bias, confounding and power. We simplified the power item on the checklist to a binary outcome of reported power calculation or not and the reporting of confounders as “yes” or “no”. Many of the studies included in this review are program evaluations and we found that a small portion of the Downs and Black questions were not relevant. Irrelevant questions were marked as N/A and final scores were given as a fraction of items scored as “yes/1,” over total number of eligible questions. Scoring was done by authors CHH and KB with disagreements reviewed by all three authors to establish a consensus. (For scoring please see supplementary Table S2).
Results
Of the 1,343 unique citations returned in the literature search, 8 articles were included in this review (Figure 1)(17–24). Two broad types of interventions were reported: 1) Public Health Department-based efforts at implementing next-generation partner services (n=4), all based in the US (17,19,22,24) and 2) Evaluations of websites used for partner notification (n=4), two based in the US, one from the Netherlands and one from Australia (Table 1)(18,20,21,23).
Table 1.
Studies of Next-generation Methods for HIV Partner Services
| Author and Year of Publication |
Study Design | Intervention | Location and Study Period |
Study Population | Sample Size | Results | Quality Assessment |
|---|---|---|---|---|---|---|---|
| Vest et al., 2007 | Case-control Study |
Compares PN outcomes between index patients reporting traditional contact info (controls) and those reporting pseudoanonymous (e-mail only) partners (cases) |
Austin, TX Health Department; 2004–2006 |
HIV and/or syphilis index patients with pseudoanonymous partners were 98.0% MSM vs. 80.6% MSM in traditional group. |
53 cases with e-mail only contacts; 265 unmatched controls. Overall 46 case index patients (86.8%) were HIV+ with/without other STI. 33 (62.3%) HIV+ only. |
Traditional PN had higher rate of successful notification (69.7 vs. 49.7%). Similar rate of new infections in tested partners (26.8% cases vs. 29.9% controls). Partners notified per index was (1.40 controls vs. 0.5 with e-mail. |
16/26 |
| Levine et al., 2008 | Evaluation of website usage statistics; brief surveys assessing awareness of inSPOT |
inSPOT website for that allows users to send e-cards to partners at risk of STI |
14 US States; 2 Canadian Cities, Romania; 2004–2007 |
Users of inSPOT | Since 2004 >30,000 people have sent >49,500 cards |
2006–2007, 2,203 (9.3%) of cards sent for HIV. Click- through rates 20.4–48.2% depending on site; no disease- specific results. Awareness of inSPOT ranged from 13% in online survey of general population to 26% among HIV providers in San Francisco. |
5/22 |
| Mendez et al., 2012 | Brief summary of public health department usage of SMS in partner services |
Used SMS to contact "cases," no data on contacting partners. SMS sent immediately after unsuccessful attempt to contact via phone call |
Portland, OR; Jan– September 2011 |
STI Cases in Portland; Gonorrhea/Syphilis and HIV |
149 Clients received SMS (not broken down by STI) |
56% of clients contacted called back after SMS was sent; >50% response rate for HIV, early syphilis and gonorrhea. No further delineation of results. 1 case responded that they did not want to be contacted via SMS |
5/23 |
| Plant et al., 2012 | Retrospective STI clinic database review + analysis of two cross-sectional surveys using time-location sampling. |
inSPOTLA is a website for sending e-card notification to partners at risk of STI. Ad campaign undertaken in 2007 with surveys aiming to assess if there was an increase in inSPOT awareness. |
Los Angeles, CA; 2007– 2009 clinic data; baseline surveys done at 20 venues at baseline (2007) and 21 at follow- up (2009) |
Largely MSM (>85% of clinic patients); time- location sample yielded 86% exclusively MSM with 13.6% who slept with both men and women. Racially diverse with 52.7% white, 24.4% Hispanic, and 13.9% black. |
STI Clinic: 29,857 patients Survey: 300/707 participated (13.6% HIV+) |
1287/29,857 (4.3%) clinic patients visited after partner notification, with 2 (0.2%) reporting inSPOTLA referral. In surveys: low overall awareness of inSPOTLA (15.8% baseline, 14.4% baseline follow-up.) 1.3% of follow-up participants had used inSPOTLA. HIV(+) follow-up participants had higher percentage of inSPOTLA awareness compared to HIV(− ) (25.6 vs. 12.3%.) |
13/17 |
| Bourne et al., 2012 | Evaluation of website usage statistics + cross-sectional survey assessing website awareness |
"WhyTest.com" is a website for homosexual men in Australia. E- partner notification feature added in 2005. Can notify partners with either SMS or e- mail. |
Australia national website usage statistics (2007–2010); survey-data from Sydney (2007) |
MSM in Australia; survey-data obtained over 1 week of heavily attended major gay community festival (Mardi Gras) |
Survey included 2342 men. |
From 2007–2010 7,923 e- notifications were sent; 96% by SMS with only 4% by e- mail. Usage increased month- to-month over evaluation period. High awareness of "WhyTest," website (50%) amongst survey participants. |
13/18 |
| Hightow-Wiedman et al., 2014 | Retrospective comparison of partner notification outcomes before and after intervention |
UNC collaborated with NC Department of Public Health in 2011 to centralize and formalize iPS and txtPS. |
North Carolina; Traditional, 2010 vs. intervention 2011–2012 |
HIV and Syphilis index cases. Internet and text referrals were largely MSM, 93.8 and 92.9 and African-american 59.1 and 71.4%. |
2011–2012: 362 clients gave 455 internet referrals, compared with 133 referrals in 2010. Text messaging used for 29 contacts who did not respond to traditional or iPS. |
Of 455 e-contacts, 39% were contacted for HIV, 39% syphilis and 21.6% dual. After the collaboration 65% of internet- contacts were notified vs. 26% in 2010. iPN identified 7 new HIV-cases. txtPS used for 29 otherwise untraceable partners and yielded a 48% response rate and 1 new HIV case. |
7/20 |
| Gotz et al., 2014 | Cross-sectional pilot study with multivariate logistic regression analysis of determinants for internet- based notification use. |
"SuggestATest (SAT)," e- notification tool for index notification of partners (SMS or e-mail). Only confirmed STI cases; provider gives index case PIN for website. Site can be used for patient or provider-referral. |
Amsterdam and Rotterdam, Netherlands; 2012 |
SAT piloted at large public STI clinics in Amsterdam and Rotterdam; 58% male and 36% MSM. |
1717 index patients with 988 SAT codes with follow-up data |
46% of patients intended to use SAT, but only 17% logged in, 14% of the total group sent a message. 20% of HIV notification done with SAT (10% in Amsterdam and 44% in Rotterdam.) Majority preferred anonymous (88%) notification by SMS (84%). Of 294 SAT notices sent, 58% of partners logged in and 20% subsequently went to STI clinics for testing. Of the patients tested as result of SAT, 28% tested positive for STI, and 1 of 4 tested positive for HIV. |
17/24 |
| Udeagu et al., 2014 | Retrospective evaluation of traditional PS, iPS and txtPS |
NYC Field Services begin using internet and text partner services (iPS and txtPS) for those clients in whom traditional contact info was missing or utilized unsuccessfully. |
NYC: traditional and iPS, 2011; txtPS, 2012 |
NYC HIV Index- cases mostly male (66–85%), MSM (62–94%) and non- white (82–90%) in iPS and txtPS |
1828 index cases named 3319 eligible partners; 2604 with traditional info, 275 internet- contact only; 368 partners in txtPS group |
Internet and text partners more likely to be MSM (OR 8.3 and 2.9) and iPS contacts more likely to be younger than 30 (− <0.0001). Contact rates were 69% traditional, 41% iPS, and 77% txtPS, although actual notification of HIV-risk with contacted partners was higher with iPS and txtPS. 65, 82 and 82% of traditional, iPS and txtPS were previously HIV(−). 69, 34 and 45% were tested, yielding 13, 10 and 5% testing positive for new HIV diagnosis. |
13/22 |
PN=partner notification, SMS=short-messaging system (i.e. text messaging), NC=North Carolina, iPS=internet partner services, txtPS=text partner services
Study Design and Quality
Of the eight articles, none were randomized trials. One of the health department-based interventions was designed as a case-control study, with cases defined as partners with e-mail only contact information and unmatched controls with traditional contact info(17). Two of the reports were comprehensive evaluations of partner services utilizing internet or text(22,24), and one was a brief letter describing implementing a short-messaging system (SMS, i.e. texting) PN program(19). Two of the four website evaluations reported on website usage statistics paired with surveys of awareness of the service(18,21). A third website evaluation asked STI clinic patients whether or not they had received website partner notification and paired these data with surveys assessing awareness of the service(20). The last type of study was a cross-sectional pilot program of a secure website used for partner notification in those with confirmed STI diagnosis(23).
According to our modified DB scaled-scoring, the study quality scores ranged from to 4/21 (19%) to 18/26 (69%). No studies scored in the top 75–100% of quality score, n=6 were in the 50–75% range, 1 study in the 25–50% range and 1 in 0–25% range.
Outcomes for Public Health Department Studies
The interventions at the Health Departments largely involved incorporating next-generation methods into existing partner notification programs. In the three studies reporting detailed demographic information, the populations in which next-generation techniques were employed were largely MSM (78–90%)(17,22,24). The next-generation groups were majority non-white in the studies from North Carolina (NC) and NYC (76.9 and 82–86.0%)(22,24) and 26.4% non-white in the case-control study from Austin, Texas(17).
Three of the four health departments used internet partner services (iPS) and these techniques were only used if traditional contact information was not available(17,22,24). In two of three studies, attempts at using “closed e-mail systems” such as social networking and/or hook-up sites were used in addition to standard “open systems” such as g-mail or yahoo, and where reported the “closed systems” were used in 73% of cases(22,24). Text partner services (txtPS) were utilized in three out of four studies and were used only after unsuccessful traditional and/or iPS notification(19,22,24), with the exception of the Portland, OR program where a text message was sent immediately after an unsuccessful phone call(19). The study from NC presented an evaluation of next-generation services after a public-academic partnership formalizing and centralizing next-generation efforts(22).
Given the differences in evaluation design, the only consistently available outcomes were number of notifications/contacts and number of successful notifications (Table 2). Successful partner notification rates for iPS ranged from 33.5–63.5% and where there was a comparison to traditional partner services, rates of successful contact were lower for iPS (49.7 vs. 69.7, p<.001 and 41 vs. 69%)(17,24). However, in the study by Udeagu et. al., despite lower contact rates in iPS, actual notification of HIV risk was higher among those contacted with iPS versus traditionalPS (82 vs. 65%, p<0.0001)(24). This study also compared txtPS to traditionalPS and found that the txtPS had a higher contact rate (77 vs. 69%, p<0.0001) and higher actual notification rate (82 vs. 65%)(24). After the centralization and formalization of iPS with the public-academic partnership in North Carolina, the number of iPS notifications increased from 131 to 455(22).
Table 2.
Next-generation Partner Notification Outcomesa
| Author and Year of Publication |
# Index Cases (% with HIV) |
# Contacts Elicited (# of contacts/index) |
# Notifiedb (% of elicited) |
#Tested (% of notified) |
New HIV Diagnosis (% of tested) |
|---|---|---|---|---|---|
| Vest et al., 2007 | 53c (62.3) | 534 (10.1) | 88 (49.7) | 71 (80.7) | Not Reportedd |
| Mendez et al., | Not reported | 149 (n/a) | |||
| Hightow-Wiedman et al., 2014 | Not reported | Internet: 362 (N/A) Text: 29 (N/A) |
Internet: 230 (63.5) Text: 14 (48) |
Unknown | Internet: 7 (n/a) Text: 1 (n/a) |
| Gotz et al., 2014 | 138 (% HIV not reported) |
505 (3.7) notifications sente |
294 (58) | Unknown | Unknown |
| Udeagu et al., 2014 | Internet: 73 (100) Text: 176 (100) |
Internet: 275 (3.8) Text: 368 (2.1) |
Internet: 92 (33.5) Text: 233 (63.3) |
Internet: 31 (34) Text: 105 (45) |
Internet: 3 (10) Text: 5 (5) |
Only studies reporting outcome data (public health or clinic-based studies) are reported here
Only including cases that were confirmed to have been notified, not just attempts
Case-control study with cases having pseudoanonymous e-mail and controls with traditional contact info. Only cases reported here; 62.3% with HIV only, but 86.8% had HIV or HIV plus other STI
19/71 (26.8%) of evaluated patients were "infected;" results not broken down by STI
Not broken down by # of contacts for both clinic sites, only total number of notifications sent
Not all of the studies reported new cases of HIV, and some reported only new STI cases without further delineation. The study by Udeagu et al. contained the most robust data, reporting HIV testing in 34 and 45% of the notified iPS and txtPS groups, with 10% (iPS) and 5% (txPS) of tests resulting in new HIV diagnosis(24). In the paper from Hightow-Wiedman et al., the number of notified partners receiving HIV testing is not reported, but of 230 and 14 notifications in the iPS and txtPS groups they report 7 (3% of notified) and 1 (7% of notified) new HIV cases. Also of note, they were able to utilize a NC viral load (VL) surveillance database to assess whether previously positive patients were likely to be engaged in care and found that 18 of 19 partners with known HIV appeared to be unengaged in care. In the 12-months following partner notification, 7 clients with no VL recorded in the previous 24 months, had a recorded VL in the database, signaling reengagement with HIV care(22). Although the data are not broken down by STI type, Vest et. al. report that of the 88 patients notified, 80.7% received testing, and 26.8% had STI.
Outcomes for Partner Notification Websites
Of the partner notification websites, two reports involved the usage of inSPOT (http://www.inspot.org/), a publically-accessible partner notification website currently operating in the US and Canada that allows individuals to anonymously send e-cards notifying partners that they are at risk of STI. One of the included reports focuses on overall inSPOT usage in 2006 and 2007(18), and the other focuses on inSPOTLA (which now directs to the inspot.org website) in 2007–2009(20). For inSPOT as a whole, 23,584 e-cards were sent in 2006–2007, including 2,203 (9.3%) for HIV. Click-through rates were heterogeneous depending on location with average rates of of 26.8–28.5%. In the brief surveys they found a low overall awareness of the website among gay/MSM men in San Francisco (SF) (19%), HIV providers in SF (26%), and an online general population sample (13%)(18). The lower level of service awareness was consistent with the findings from inSPOTLA that reported a 15.8 and 14.4% rate of awareness in the pre and post surveys surrounding an advertising campaign(20). However, there were higher levels of awareness among HIV+ participants and those that had recently met sexual partners over the internet (25.6 and 31.8%). The inSPOTLA report also included data from a large urban STI clinic and found that from 2007–2009 only 2 of 1,287 (0.2%) patients coming to the clinic as result of partner notification had received an inSPOTLA notification. As a whole, although low numbers of those surveyed had ever sent or received an e-card (2–4%), a much higher percentage reported that they would send one (65–73%)(18).
The study from Australia evaluated a partner notification feature on an Australian gay men’s health website, “Why Test” (previously services at www.whytest.org, now found at http://www.thedramadownunder.info/introduction).(21) Through the service, anonymous notifications are sent by user via choice of e-mail or SMS. From 2007–2010 7,923 notifications were sent with 96% of messages being sent via SMS. No breakdown by STI was provided. In an awareness survey conducted at a major Gay community event in Sydney, 1287/2342 (54.6%) of men recalled the WhyTest website image, but knowledge of the STI partner notification feature was not directly assessed.
The study from the Netherlands by Götz et. al. used an internet-based partner notification system, “SuggestATest (SAT)” (website no longer available), for those with a confirmed STI to notify partners and used elements of both patient referral (patient notifies partners) and provider referral (provider notifies partners)(23). The system was piloted at two large urban STI clinics in Rotterdam and Amsterdam where those with confirmed STIs were given an access code to log in and send notifications. Patients could then choose to send notifications via e-mail or SMS and anonymously or non-anonymously. Of 988 patients given login-codes, n=457 (46%) intended to use the system, but only 170 (17%) logged in and 138 (14% of all) sent a notification. 88% of notifications were anonymous, with 84% sent via SMS. Depending on the clinic site, the use of SAT for HIV varied from 10% (2/21) in Amsterdam and 44% in Rotterdam (4/9), where nurses performed provider notification for all HIV cases. The authors found that of the 294 partners receiving SAT notifications, 58% logged into the SAT system and 20% reported to STI clinics for testing. The authors also looked at patients reporting to the clinics and found that 5 and 17% had been notified of STI risk via SAT in Amsterdam and Rotterdam respectively. Of the 99 patients presenting to the clinic for HIV testing, 4 had been notified via SAT and 1 patient tested positive.
Discussion
Overall we found reports on 3 general techniques of utilizing next-generation HIV partner services: 1) incorporation of these services into existing efforts at public health departments; 2) decentralized publically-accessible websites for patient-led partner notification; 3) a hybrid approach using a clinic based web-service accessible to those with confirmed STI.
Despite lower than traditional notification rates in the public-health department-based efforts, it is notable that next-generation techniques were utilized exclusively for partners with no traditional contact information, a previously unreachable group. This may in part explain the lower rates of successful contact, as this may be a particularly “hard-to-reach” population. Given the estimated 20–30% of HIV-positive individuals that are unaware of their infection(25), finding a high prevalence previously unreachable groups is a priority. However, from these data it is not clear that most at risk populations are being reached. Where assessed, new HIV diagnoses ranged from 3–10% of those notified/tested(22,24). While higher than the US population incidence of HIV(26), these rates are lower than the 20% aggregate rate of new HIV case finding reported in a 2007 systematic review of traditional HIV PN(12). More work needs to be done to assess whether the incidence of new HIV in the population that technology informed services reach is high enough to warrant directing resources to these efforts versus investing more in traditional services or other social network based testing (ie clustering). However, as shown by Hightow-Wiedman et al., these services also have the potential to re-engage previously positive HIV patients in care. Along those lines the effectiveness of these services may be best measured using total HIV infection case finding rather than just new cases. Re-linkage and re-engagement of previously positive patients can potentially impact onwards transmission and improve outcomes for patients. Taken together, the modest new case-finding ability among a previously unreachable population and increase in total case finding does support including these services as an adjunct to traditional techniques.
Among the public website evaluations there was a relatively low awareness and directly traceable utilization of the site services. Overall, little data was presented on HIV specifically, limiting our ability to draw firm conclusions about the effectiveness of these services for HIV partner notification. Overall these sites may be more effective for partner notification in treatable STIs, for which public health efforts at partner notification may be much less robust than for HIV, although previous trials have been disappointing(27). Future work should consider how branding of such sites with a recognized name of a health department, academic center or prominent community-based organization, might affect uptake of services.
The pilot program presented by Götz et. al., involves a unique blending of website notifications with a centralized clinic-based approach. This may limit potential for abuse by enabling only those with confirmed STI to use these services. This system also allows for both provider referral and patient referral. This is an important innovation to web-notification services, given that provider notification is thought to be more effective than patient referral alone(12,14,28,29). A main barrier to effective implementation of partner services is the rejection or suboptimal use of those services by patients(30,31). This may be related to a number of factors, including distrust of health departments and HIV-related stigma(31). Hybrid programs such as these enable provider notification while also allowing greater patient input and choice in how and by what means partners are notified. This may help to effectively address the aforementioned barriers and increase the acceptability of partner services among patients. In terms of patient choice it is also important to note that in these studies the vast majority of patients chose to send SMS versus internet notifications. While previous work has shown high acceptability for iPS in certain groups, SMS may be more preferable(3,32). Future research should determine the factors associated with desire to send SMS over e-mail and if the findings of preference for SMS are confirmed, programs should take this into account.
In addition to expanding the platforms for partner services delivery (ie. text, email, sex-seeking applications), innovations to partner services programs should also focus on improvements to the approach and method of notification by service providers. Given the importance of developing trusting relationships between service providers and patients(31), programs should dedicate more attention to non-invasive approaches that could strengthen this relationship. For example, research on attitudes and opinions about partner notification indicates that some participants would prefer to accept partner notification assistance from a medical provider or social worker rather than a health department employee(33). Other studies demonstrate differences between MSM patients and their providers regarding perceptions about determinants of sexual risk behavior, indicating that increased training and education might help to improve trust(31). Other recommendations for innovations to service provision include enhanced point-of-care counseling(13), as well as broadening referral for testing from sexual partners to social network members and peers(33).
This review has a few limitations. First, no search of the gray literature was undertaken and we may have inadvertently missed other relevant reports. Secondly, the conclusions of this review are limited by the nature of the studies included. Only 2 studies had comparison arms and most were cross-sectional evaluations. Many studies lacked hard partner notification outcomes. This may be in part a limitation of the contacting partners electronically, given that conclusive evidence of having reached the partner may not be available. Additionally, if a partner decides to seek care outside of the public health network, that outcome may not be captured in these databases. Furthermore these studies are limited by mostly being conducted in the US and amongst MSM, limiting generalizability. Lastly, the Downs and Black tool may not be ideally suited to these types of evaluation studies and may under or over-quantify study quality.
In summary, next-generation techniques appear to be a useful adjunct to traditional partner services. Utilization of patient-initiated web notification is low for HIV in particular and methods that include an option for provider-led e-notification and for sending notifications via SMS may be more effective.
Supplementary Material
Acknowledgments
Funding: This work was funded in part by NIH grant R34 MH104058.
Footnotes
Conflict of Interest: The authors have no conflicts of interest to report at this time.
References
- 1.Cowan FM, French R, Johnson AM. The role and effectiveness of partner notification in STD control: a review. Genitourin Med. 1996 Aug;72(4):247–252. doi: 10.1136/sti.72.4.247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fenton KA, Peterman TA. HIV partner notification: taking a new look. Aids. 1997;11(13):1535–1546. doi: 10.1097/00002030-199713000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Mimiaga MJ, Tetu AM, Gortmaker S, Koenen KC, Fair AD, Novak DS, et al. HIV and STD Status Among MSM and Attitudes About Internet Partner Notification for STD Exposure. Sex Transm Dis. 2008 Feb;35(2):111–116. doi: 10.1097/OLQ.0b013e3181573d84. [DOI] [PubMed] [Google Scholar]
- 4.File T, Ryan C. United States Census Bureau; 2014. [cited 2015 Apr 14]. Computer and Internet Use in the United States: 2013 [Internet] Available from: https://www.census.gov/content/dam/Census/library/publications/2014/acs/acs-28.pdf. [Google Scholar]
- 5.Street 1615 L., NW, Washington S 700, Inquiries D 20036 202 419 4300 | M 202 419 4349 | F 202 419 4372 | M. Mobile Technology Fact Sheet [Internet] [cited 2015 Apr 14];Pew Research Center’s Internet & American Life Project. Available from: http://www.pewinternet.org/fact-sheets/mobile-technology-fact-sheet/ [Google Scholar]
- 6.McFarlane M, Bull SS, Rietmeijer CA. The Internet as a newly emerging risk environment for sexually transmitted diseases. JAMA. 2000 Jul 26;284(4):443–446. doi: 10.1001/jama.284.4.443. [DOI] [PubMed] [Google Scholar]
- 7.Bull SS, McFarlane M, Rietmeijer C. HIV and sexually transmitted infection risk behaviors among men seeking sex with men on-line. Am J Public Health. 2001 Jun;91(6):988–989. doi: 10.2105/ajph.91.6.988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Buhi ER, Klinkenberger N, McFarlane M, Kachur R, Daley EM, Baldwin J, et al. Evaluating the Internet as a Sexually Transmitted Disease Risk Environment for Teens: Findings From the Communication, Health, and Teens Study. Sex Transm Dis. 2013 Jul;40(7):528–533. doi: 10.1097/OLQ.0b013e31829413f7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liau A, Millett G, Marks G. Meta-analytic Examination of Online Sex-Seeking and Sexual Risk Behavior Among Men Who Have Sex With Men. Sex Transm Dis. 2006 Sep;33(9):576–584. doi: 10.1097/01.olq.0000204710.35332.c5. [DOI] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention (CDC) Recommendations for partner services programs for HIV infection, syphilis, gonorrhea, and chlamydial infection. MMWR Recomm Rep Morb Mortal Wkly Rep Recomm Rep Cent Dis Control. 2008 Nov 7;57(RR-9):1–83. quiz CE1–4. [PubMed] [Google Scholar]
- 11.Moody V, Hogben M, Kroeger K, Johnson J. Internet-Based Partner Services in US Sexually Transmitted Disease Prevention Programs: 2009–2013. J Public Health Manag Pract. 2015 Jan 1; doi: 10.1097/PHH.0000000000000201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hogben M, McNally T, McPheeters M, Hutchinson AB. The Effectiveness of HIV Partner Counseling and Referral Services in Increasing Identification of HIV-Positive Individuals: A Systematic Review. Am J Prev Med. 2007 Aug;33(2, Supplement):S89–S100. doi: 10.1016/j.amepre.2007.04.015. [DOI] [PubMed] [Google Scholar]
- 13.Hogben M, Niccolai LM. Innovations in sexually transmitted disease partner services. Curr Infect Dis Rep. 2009;11(2):148–154. doi: 10.1007/s11908-009-0022-6. [DOI] [PubMed] [Google Scholar]
- 14.Ferreira A, Young T, Mathews C, Zunza M, Low N. Strategies for partner notification for sexually transmitted infections, including HIV. [cited 2015 Apr 14];Cochrane Database Syst Rev [Internet] 2013 (10) doi: 10.1002/14651858.CD002843.pub2. Available from: http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD002843.pub2/full. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009 Jul 21;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52(6):377–384. doi: 10.1136/jech.52.6.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vest JR, Valadez AM, Hanner A, Lee JH, Harris PB. Using e-mail to notify pseudonymous e-mail sexual partners. Sex Transm Dis. 2007;34(11):840–845. doi: 10.1097/OLQ.0b013e318073bd5d. [DOI] [PubMed] [Google Scholar]
- 18.Levine D, Woodruff AJ, Mocello AR, Lebrija J, Klausner JD. inSPOT: The First Online STD Partner Notification System Using Electronic Postcards. PLoS Med. 2008 Oct 21;5(10):e213. doi: 10.1371/journal.pmed.0050213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mendez J, Maher J. Evidence Supporting the Use of Text Messaging for Partner Services. [Letter] Sex Transm Dis. 2012 Mar;39(3):238–239. doi: 10.1097/OLQ.0b013e3182471b31. [DOI] [PubMed] [Google Scholar]
- 20.Plant A, Rotblatt H, Montoya JA, Rudy ET, Kerndt PR. Evaluation of inSPOTLA.org: An Internet Partner Notification Service. Sex Transm Dis. 2012 May;39(5):341–345. doi: 10.1097/OLQ.0b013e31824e5150. [DOI] [PubMed] [Google Scholar]
- 21.Bourne C, Zablotska I, Williamson A, Calmette Y, Guy R. Promotion and uptake of a new online partner notification and retesting reminder service for gay men. Sex Health. 2012 Sep;9(4):360–367. doi: 10.1071/SH11132. [DOI] [PubMed] [Google Scholar]
- 22.Hightow-Weidman L, Beagle S, Pike E, Kuruc J, Leone P, Mobley V, et al. “No One’s at Home and They Won’t Pick up the Phone”: Using the Internet and Text Messaging to Enhance Partner Services in North Carolina. Sex Transm Dis. 2014 Feb;41(2):143–148. doi: 10.1097/OLQ.0000000000000087. [DOI] [PubMed] [Google Scholar]
- 23.Götz HM, Rooijen MS van, Vriens P, Coul EO de, Hamers M, Heijman T, et al. Initial evaluation of use of an online partner notification tool for STI, called “suggest a test”: a cross sectional pilot study. Sex Transm Infect. 2014 May 1;90(3):195–200. doi: 10.1136/sextrans-2013-051254. [DOI] [PubMed] [Google Scholar]
- 24.Udeagu C-CN, Bocour A, Shah S, Ramos Y, Gutierrez R, Shepard CW. Bringing HIV partner services into the age of social media and mobile connectivity. Sex Transm Dis. 2014;41(10):631–636. doi: 10.1097/OLQ.0000000000000181. [DOI] [PubMed] [Google Scholar]
- 25.Burns DN, DeGruttola V, Pilcher CD, Kretzschmar M, Gordon CM, Flanagan EH, et al. Toward an Endgame: Finding and Engaging People Unaware of Their HIV-1 Infection in Treatment and Prevention. AIDS Res Hum Retroviruses. 2014 Mar 1;30(3):217–224. doi: 10.1089/aid.2013.0274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hall H, Song R, Rhodes P, et al. EStimation of hiv incidence in the united states. JAMA. 2008 Aug 6;300(5):520–529. doi: 10.1001/jama.300.5.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rietmeijer CA, Westergaard B, Mickiewicz TAB, Richardson DM, Ling S, Sapp T, et al. Evaluation of an Online Partner Notification Program. Sex Transm Dis. 2011 May;38(5):359–364. doi: 10.1097/OLQ.0b013e31820ef796. [DOI] [PubMed] [Google Scholar]
- 28.Landis SE, Schoenbach VJ, Weber DJ, Mittal M, Krishan B, Lewis K, et al. Results of a Randomized Trial of Partner Notification in Cases of HIV Infection in North Carolina. N Engl J Med. 1992 Jan 9;326(2):101–106. doi: 10.1056/NEJM199201093260205. [DOI] [PubMed] [Google Scholar]
- 29.Mathews C, Coetzee N, Zwarenstein M, Lombard C, Guttmacher S, Oxman A, et al. A systematic review of strategies for partner notification for sexually transmitted diseases, including HIV/AIDS. Int J STD AIDS. 2002 May 1;13(5):285–300. doi: 10.1258/0956462021925081. [DOI] [PubMed] [Google Scholar]
- 30.Golden MR. Editorial: HIV partner notification: a neglected prevention intervention. Sex Transm Dis. 2002 Aug;29(8):472–475. doi: 10.1097/00007435-200208000-00007. [DOI] [PubMed] [Google Scholar]
- 31.Edelman EJ, Cole CA, Richardson W, Boshnack N, Jenkins H, Rosenthal MS. Opportunities for improving partner notification for HIV: results from a community-based participatory research study. AIDS Behav. 2014 Oct;18(10):1888–1897. doi: 10.1007/s10461-013-0692-9. [DOI] [PubMed] [Google Scholar]
- 32.Apoola A, Radcliffe KW, Das S, Robshaw V, Gilleran G, Kumari BS, et al. Patient preferences for partner notification. Sex Transm Infect. 2006 Aug;82(4):327–329. doi: 10.1136/sti.2005.018119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Golden MR, Hopkins SG, Morris M, Holmes KK, Handsfield HH. Support among persons infected with HIV for routine health department contact for HIV partner notification. J Acquir Immune Defic Syndr 1999. 2003 Feb 1;32(2):196–202. doi: 10.1097/00126334-200302010-00012. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.