Abstract
The efficiency of suturing training and testing (SUTT) model by laparoscopy was evaluated, measuring the suturingskill acquisition of trainee gynecologists at the beginning and at the end of a teaching course. During a workshop organized by the European Academy of Gynecological Surgery (EAGS), 25 participants with three different experience levels in laparoscopy (minor, intermediate and major) performed the 4 exercises of the SUTT model (Ex 1: both hands stitching and continuous suturing, Ex 2: right hand stitching and intracorporeal knotting, Ex 3: left hand stitching and intracorporeal knotting, Ex 4: dominant hand stitching, tissue approximation and intracorporeal knotting). The time needed to perform the exercises is recorded for each trainee and group and statistical analysis used to note the differences. Overall, all trainees achieved significant improvement in suturing time (p < 0.005) as measured before and after completion of the training. Similar significantly improved suturing time differences (p < 0.005) were noted among the groups of trainees with different laparoscopic experience. In conclusion a short well-guided training course, using the SUTT model, improves significantly surgeon’s laparoscopic suturing ability, independently of the level of experience in laparoscopic surgery.
Key words: Endoscopy, laparoscopic suturing, psychomotor skills, surgery, teaching, training suturing model.
Keywords: Endoscopy, laparoscopic suturing, psychomotor skills, surgery teaching, training suturing model
Introduction
Minimally invasive surgery (MIS) enables accurate diagnosis, treatment and fast recovery mainly due to better viewing ability, magnification and small skin incisions. In the early 1990s, comprehensive and structured training in MIS was not available, hence the apprentice-tutor model was followed, but was however associated with long operating hours andhigh complication rate (Deziel et al., 1993). Moreover, it has been evidenced that unconditional board implementation of laparoscopic surgery might be related to increased morbidity and mortality (Van der Wal, 2007). The demand by “Health Systems” to audit provided health services, especially reporting on post-operative complications, morbidity and mortality, led to the development of structured and validated tests for psychomotor and surgical skills acquisition prior to patient surgery. The limitations of the classic apprentice-tutor model are obvious and the vast majority of surgeons agree today that training should be initiated outside the operating theatre such as use of simulators, dry lab facilities and animal models (Campo et al., 2005; Kirlum et al., 2005; Van Velthoven and Hoffman, 2006; Heinrich et al., 2006). The European Academy of Gynecological Surgery (EAGS) provides gynecologists scientifically validated training programs and certification in gynecological endoscopic surgery. Training and testing the basic and complex laparoscopic psychomotor skills (LPS) provides the fundamental needs for surgery and improves patient’s safety which is especially important for a surgeon’s initial steps (Molinas et al., 2008; Campo et al., 2010; Molinas and Campo, 2010). The European Society for Gynecological Endoscopy (ESGE), realizing the need of improving surgeons’ knowledge and skills,adopted the new certification program “Gynecological Endoscopic Surgical Education and Assessment” (GESEA) program which is based on 5 domains of surgical professional competence: a) Electronic Learning and Self-assessment, b) Specific Endoscopic Skills, c) Assessment, d) Surgical Practice Curriculum and e) Continuing Medical Education.
In 2012, the EAGS enquiring surgeons’ performance and patients’ safety focused on minimal acceptable level of LPS and knowledge to offer patients’ optimal laparoscopic surgery. Among other LPS acquisition, laparoscopic suturing was considered the most difficult exercise during a laparoscopic operation. Fundamental knowledge as well as tips and tricks in laparoscopic suturing can enormously help to learn a fast, yet correct and safe suturing technique. Frequent exercise in dry lab but also routine practice of laparoscopic suturing secure efficiency and reduce operative complications (Campo et al., 2012a). The EAGS provides education and training by certified instructors and has organized and performed more than 100 workshops in endoscopic surgery until now in Europe and abroad. The SUTT model is a well guided 3 day training in laparoscopic suturing designed by the EAGS and used for training and testing laparoscopic suturing performance. The objective of this study was to evaluate the benefits of the SUTT model in laparoscopic suturing skill acquisition and improvement, and to check if the acquired suturing skills after training are dependent on the experience and the degree of exposure of the trainee in laparoscopic surgery.
Materials and Methods
Trainees
Twenty-five trainees attending a three day endoscopic course organized by the EAGS and the faculty of medicine in Porto were included in the study. The course was held at the endoscopic training center of “Hospitalcuf” in Porto-Portugal on May 23rd, 24th and 25th, 2013. The group included post graduates and certified gynecologists with different levels of experience in laparoscopy. All participants filled out the identification form of the EAGS in order to determine their level of exposure to laparoscopic training and their surgical experience. The EAGS identification form defines the current academic level, the exposure to typical psychomotor skills (video games and musical instruments), the exposure to hands-on lab laparoscopic training and the experience in the operation room. The surgical experience is based on the classification of the ESGE (Campo et al., 2010; Molinas and Campo, 2010). This classification establishes four levels of procedures: first level (basic), second level (intermediate), third level (advanced) and fourth level (special procedures). For each level, the numbers of procedures performed were recorded and then scored in the following categories: no procedures (score 0), 1-30 procedures (score 1), 31-50 procedures (score 2) and more than 50 procedures (score 3). The scores obtained in each level were added, giving a final score ranging from 0 to 12. This score, resulting from many possible combinations, represents the amount of laparoscopic procedures to which an individual was exposed. At the time of data analysis, three levels of exposure were identified: the group of minimal exposure comprised those with no or very little exposure to laparoscopy (final score 0 or 1). The group of intermediate exposure comprised those with limited exposure to laparoscopy (final score 2 or 3). The group of major exposure comprised those with important exposure to laparoscopy (final score ≥ 4). The study was exempt from institutional review board approval, since no harm could be done to living organisms.
Design
In this study, each trainee performed the SUTT at the beginning of the course prior to any hands on session. The test was explained during a lecture and all exercises were described and demonstrated in a video. During the test every trainee was supervised by a mentor. At the end of the course, the same test was repeated by all trainees following the same instruction rules. In the mean time they attended the course conferences and they performed a mean of 12 hours of hands-on training in different psychomotor skills including camera navigation, eye-hand coordination, and bimanual coordination and suturing.
Exercises
The suturing test (SUTT) is a tool developed by the Academy to train and test different stitching and suturing skills. It consists of a 6 cm round white soft pad with black and red dots (Fig. 1). Red dots sign the starting point for each exercise. The absence of red dot means that one can choose the starting stitching point. All exercises were performed in Szabo trainer box (Karl Storz, Tutlingen, Germany), connected to an all-in-one (monitor, light source and video-camera) laparoscopic tower (Telepack, Karl Storz). A 10 mm, 0 degree optic was introduced through a midline port and the needle holders through lower and lateral ports to the right for the left curve (right needle holder) and to the left for the right curve (left needle holder). The participant stood to the left of the trainer box. The camera was fixed at a distance that allowed visualization of the entire operating field. The needle holders were held with the relevant hands and when an intracorporeal knot was required, it was made as follows: A double counter-clockwise knot, followed by a single clockwise knot and, finally, by a single counter-clockwise knot.
Fig. 1. The SUTT model of the European Academy.
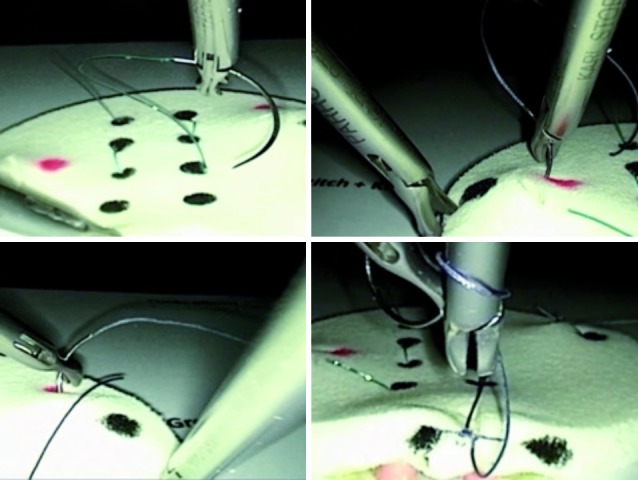
The test includes 4 suturing exercises (Ex). Ex 1 evaluates both hands stitching skills by performing a Greek continuous suturing line starting with the left hand, using a 10 cm 2-0 monocryl thread (A). Ex 2 is a right hand stitch and an intracorporeal knot, using a 15cm 2-0 monocryl thread (B). Ex 3 is a left hand stitch and an intracorporeal knot, using a 15 cm 2-0 vicryl thread (C). In Ex 4, the trainee is free in the choice of the dominant or non-dominant hand to make a stitch and an intracorporeal knot, using a 10cm 2-0 vicryl thread. Two black dots are then placed at the posterior aspect of the model (D). Each exercise starts when the mentor gives the sign and ends when the trainee considers that he finished the task or when the time has expired. The maximal allowed time is 15 minutes for Ex 1 and 10 minutes for each of the other exercises. Each mentor notes the time in minutes and seconds for every exercise using a stopwatch. In each exercise, participants should perform a correct task meaning that the thread should pass through the do without any tissue tearing, and a good tissue approximation with a correct knot are required.
Outcome measurements
Five parameters were measured in the SUTT test: the time needed for each trainee to complete each exercise, the number of mistakes (thread passing out of the dot), the number of traumas (tear made to the tissue), the correct tying of the knot (Ex 2, 3 and 4), and good tissue approximation (Ex 4). While the time of the exercise was noted by the mentor on the spot, other parameters were reviewed later by another mentor in order to avoid any subjective evaluation. The Academy had developed an online scoring platform to register participants’ data and test results in a central database. For each participant, the previous exposure to gynecological laparoscopy was registered and documented according to the previously published scoring system (Campo et al., 2010; Molinas and Campo, 2010). The central database provides an online calculation of the results and an appreciation of the skills of the participants with a colour code system similar to thetraffic colour code, comparing to the previously registered experts benchmark. Three levels of performance can be delivered in each of the four exercises: insufficient performance (red), fair performance (yellow), or excellent performance (green). Statistical analysis was performed in order to compare the five tested parameters for each of the4 exercises at the beginning and at the end of thetraining, for every trainee and for the whole group depending on their level of exposure.
The study was exempt from institutional ethical board approval, since no harm could be done to living organisms.
Results
The level of exposure to laparoscopic surgery of all trainees was divided into three subgroups. Eight participants (32%) had minimal exposure, 7 (28%) had intermediate exposure, and 10 (40%) had major exposure. All 25 trainees performed the suturing test before the training and 24 trainees repeated it after the training. One trainee from the subgroup of intermediate exposure was missed.
Table I shows the comparison of different parameters before the training (B = before) and after the training (A = after). For the group of 24 trainees, mean time to perform the exercise, mean number of mistakes and mean number of trauma were calculated. It also shows the number of trainees who performed a correct knot tying and a good tissue approximation. The mean time to perform each exercise significantly decreased after the training session (p < 0.05). The number of mistakes is also reduced for all exercises. In Ex 1 and Ex 4, this reduction is statistically significant (p < 0.05). We noticed less traumas as well with a significant decrease in Ex 1 and Ex 4 (p < 0.05). The quality of the intracorporeal knot was assessed in Ex 2, Ex 3, and Ex 4. In each of the three exercises, participants were able to improve the quality of knot tying. For example, in Ex 4, 4 participants made a correct knot. After the training, 17 participants performed a correct knot. The same result is noticed in the tissue approximation. Only 2 participants made a satisfactory tissue approximation in Ex 4. This number increased to 16 after the training.
Table I. omparison between the 5 parameters before training (B) and after the training (A) among the 4 exercises (Ex 1: both hands stitching and continuous suturing, Ex 2: right hand stitching and intracorporeal knotting, Ex 3: left hand stitching and intracorporeal knotting, Ex 4: dominant hand stitching, tissue approximation and intracorporeal knotting).
| Time (sec) | Mistakes | Traumas | Good knot tying | Good tissue approximation | ||||||
| B | A | B | A | B | A | B | A | B | A | |
| Ex 1 | 789.75 | 649.42 | 4.833 | 2.167 | 2.375 | 0.833 | ||||
| p value | 0.011 | 0.008 | 0.029 | |||||||
| Ex 2 | 538.67 | 391.54 | 1.167 | 0.333 | 0.583 | 0.291 | 7 | 18 | ||
| p value | 0.015 | 0.518 | 0.426 | 0.0014 | ||||||
| Ex 3 | 539.33 | 435.2 | 1.292 | 0.5 | 0.583 | 0.291 | 5 | 17 | ||
| p value | 0.0001 | 0.286 | 0.087 | 0.0005 | ||||||
| Ex 4 | 564.33 | 476.04 | 1.417 | 0.625 | 0.75 | 0.416 | 4 | 17 | 2 | 16 |
| p value | 0.0001 | 0.009 | 0.165 | 0.000 | 0.000 | |||||
Based on the time and the number of mistakes ineach exercise, and in order to simplify and standardize the grading, the European Academy provides the trainee a well defined report of three levels of performance in each exercise (insufficient, fair and excellent).
There is a clear improvement in the performance of trainees in each exercise. For instance, in Ex 3, 19 (76%) of the trainees had insufficient performance, 3 (12%) had a fair score, and 3 (12%) had an excellent performance. After the training, the trainees were distributed as follows: 8 (33.3%) with insufficient performance, 12 (50%) with fair score and 4 (16.7%) with excellent performance (p value 0.017). The distribution of the different performance scores among each exercise is represented in Table II.
Table II. Comparison of the performance scores for each exercise before and after the training.(Ex 1: both hands stitching and continuous suturing, Ex 2: right hand stitching and intracorporeal knotting, Ex 3: left hand stitching and intracorporeal knotting, Ex 4: dominant hand stitching, tissue approximation and intracorporeal knotting).
| Exercises | Performance scores | Before training | After training | P value | ||
|---|---|---|---|---|---|---|
| Trainees | % | Trainees | % | |||
| Ex 1 | Insufficient (red) | 19 | 76 | 8 | 33 | 0.02 |
| Fair (yellow) | 3 | 12 | 12 | 50 | ||
| Excellent (green) | 3 | 12 | 4 | 17 | ||
| Ex 2 | Insufficient (red) | 20 | 80 | 6 | 25 | 0.002 |
| Fair (yellow) | 4 | 16 | 10 | 42 | ||
| Excellent (green) | 1 | 4 | 8 | 33 | ||
| Ex 3 | Insufficient (red) | 16 | 64 | 5 | 21 | 0.017 |
| Fair (yellow) | 4 | 16 | 5 | 21 | ||
| Excellent (green) | 5 | 20 | 14 | 58 | ||
| Ex 4 | Insufficient (red) | 22 | 88 | 12 | 50 | 0.049 |
| Fair (yellow) | 3 | 12 | 8 | 33 | ||
| Excellent (green) | 0 | 0 | 5 | 17 | ||
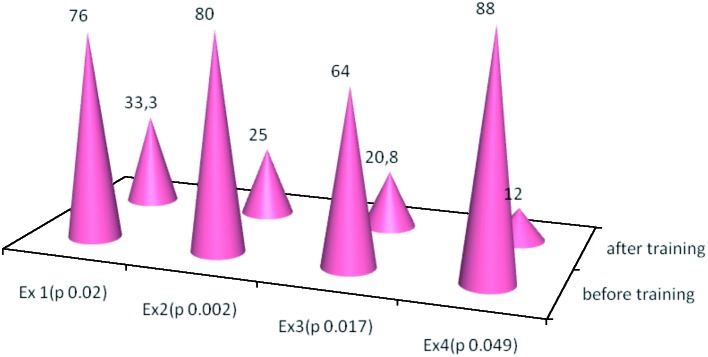
The percentages of trainees with insufficient performance significantly decreased in each exercise before and after the training. This decrease went from 19 (76%) to 8 (33.3%) (p value 0.02) in Ex 1, from 20 (80%) to 6 (25%) (p value 0.002) in Ex 2, from 16 (64%) to 5 (20.8%) (p value 0.017) in Ex 3 and from 22 (88%) to 12 (50%) p value (0.049) in Ex 4 (Fig. 2).
Fig. 2. Percentages of trainees with insufficient performances.
Concerning the 8 trainees with minimal exposure to laparoscopic surgery, each one performed 4 exercises and overall 32 exercises. The overall score was insufficient and this was noticed in 30 trials among. This number decreased significantly to 17 after the training (p = 0.005). Similar results are demonstrated in the 7 trainees with intermediate exposure and in the 10 trainees with major exposure where we noticed a significant decrease in the insufficient performance scores from 20 to 7 (p = 0.008), and from 27 to 7 (p = 0.00001) respectively. The difference in performances among each subgroup is summarized in Table III.
Table III. Performances before and after training among the different subgroups.
| Exposure | Performance scores | Before training | % | After training | % | P value |
|---|---|---|---|---|---|---|
| Minimal | Insufficient | 30 | 93.75 | 17 | 53.12 | 0.005 |
| Fair | 1 | 3.12 | 9 | 28.12 | ||
| Excellent | 1 | 3.12 | 6 | 18.75 | ||
| Intermediate | Insufficient | 20 | 71.42 | 7 | 29.16 | 0.008 |
| Fair | 4 | 14.28 | 11 | 45.83 | ||
| Excellent | 4 | 14.28 | 6 | 25 | ||
| Major | Insufficient | 27 | 67.75 | 7 | 17.5 | 0.00001 |
| Fair | 9 | 22.5 | 15 | 37.5 | ||
| Excellent | 4 | 10 | 18 | 45 |
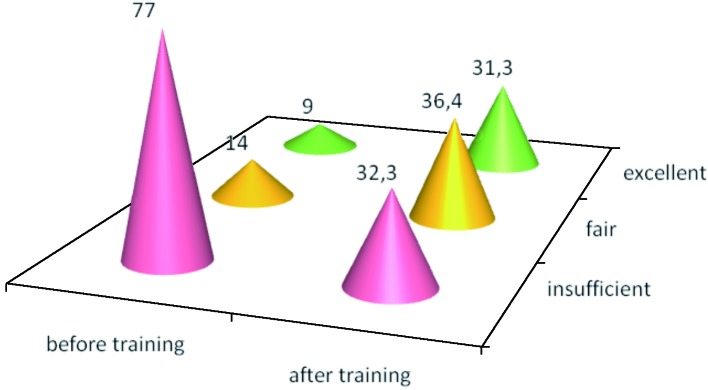
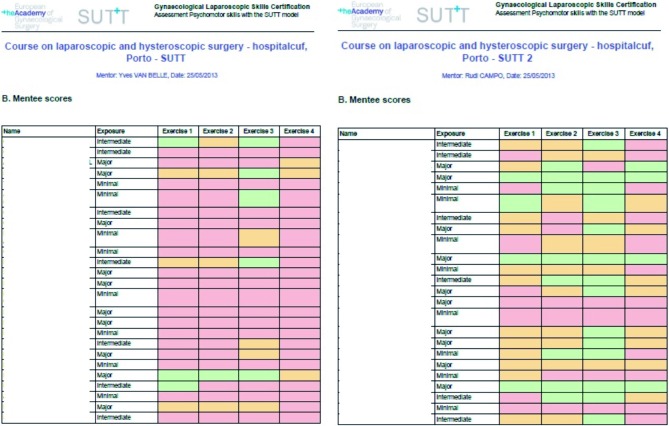
Taking into account all the 3 subgroups, 77 (77%) of the exercises were scored insufficient (red) and decreased to 31 (32.2%) after the training, as shown in figure 3. This improvement is clearly noticed in the increased number of improved performances scored as fair (yellow) or excellent (brown). figure 4 represents the official score sheet of the trainees as delivered by the Academy for the institutions performing the tests.
Fig. 3. Rate (%) of different performance scores before and after the training.
Fig. 4. Official SUTTscoring sheet for the trainees before and after the training.
Discussion
Acquiring laparoscopic suturing is a challenging task and probably the most difficult skill to master in the MIS (Misra et al., 2007; Gurusamy et al., 2008). The major concerns about teaching how to suture are the time needed for acquisition of this task and the absence of a universal tool to assess it. Studies reveal that laparoscopic suturing skills can be acquired with extensive training outside the operation room (Moorthy et al., 2004; Rosenthal et al., 2010).
In this cohort study it has been shown that each surgeon independently of his experience in laparoscopic surgery can significantly improve his laparoscopic suturing abilities using the SUTT model. These validated suturing exercises objectively demonstrate the improvement of each trainee in ambidexterity handling, suturing accuracy and knotting. The above results also show the reduction of the number of mistakes and the time needed to accomplish each exercise (Table I).
The time needed to load the needle, accurately pass through the tissues, and then approximate the edges and knotting has been used as an objective parameter for the assessment of laparoscopic suturing skills (Vossen et al., 1997; Risucci et al., 2001; Chung et al., 2005). The method used to assess the acquisition of laparoscopic suturing skill varies among studies and has not been uniform. Assessment of a single intracorporeal knotting to 100 consecutive knots has been used in order to evaluate suturing performance (Pearson et al., 2002). Nevertheless, there is a lack for a universal system to evaluate this complex LPS.
The SUTT model adopted by the Academy and the ESGE is a simple and effective tool made of 4 laparoscopic suturing exercises. The online scoring platform enables to collect all the data from each exercise; then the Academy provides to the trainee a defined scoring system of 3 levels of performance: insufficient (red), fair (yellow) and excellent (green). New computerized systems register the motion tracking and analysis of the instruments in order to evaluate the accuracy of suturing (Mason et al., 2013). This technique is lacking in our model and would be of major value once added and compared like other parameters.
Despite the reported extensive time to acquire laparoscopic suturing skills, we are convinced that this time could be significantly reduced in the presence of well-trained instructors with didactic abilities. In fact, during the training session, instructors were giving direct feedback to the trainees to correct their mistakes, and suggesting tips and tricks on every step of the suturing in order to improve their performance. In result, during a 3 days course, all the participants improved their level of performance. This improvement is highlighted in two aspects. First, the total number of trainees with insufficient score has been significantly reduced in all exercises (Table II). This reflects that the improvement is at different levels of LPS because each exercise simulates different real OR situation: right hand suturing, left hand suturing, continuous suturing, and tissue approximation.
The major advantage of the Academy scoring system is based on the fact that each trainee is informed specifically about which exercise failed and ways to improve his skills. A fair score on Ex 2 but insufficient score in Ex 3 means that more training for the left hand suturing should be done.
Second, the improvement of suturing ability after training has been noticed independently of the level of exposure in laparoscopic surgery (Table III). Even though a bias does exist in the group of intermediate exposure because one of the trainees didn’t perform the after-training SUTT, the overall performance score of the three groups is clearly improved (Fig. 3). Many studies have shown a variable impact of experience on acquisition of laparoscopic suturing skills. Rissuci et al. (2001) and Kroeze et al. (2009) demonstrated a positive relationship between laparoscopic suturing skill and experience. In the group of major exposure to laparoscopy, it is interesting to notice the lowest rate of insufficient scores, yet too high for their presumed level of exposure. It could be that even though being exposed to a larger number of procedures, the presence of new devices sparing the classical suturing like the staplers, the new brands of auto locking threads and the glues, experienced surgeons may lose their suturing skills. On the other hand, it is important to note that this is the group that has the highest reduction of this ratio from 67.75% to 17.5% after the training. Our study suggests that even experienced surgeons could benefit from training courses of complex LPS.
Many authors showed the effectiveness of short training courses. Aggarwal et al. (2006) proved that regardless of the baseline laparoscopic experience, endoscopic suturing can be learned during short skills courses. Merleu et al. (2013) stressed on the quality of training to acquire suturing skills, and they demonstrate the utility of a 5-day suturing course using a three-step model “gladiator rule” in teaching laparoscopic suturing. Based on the net improvement on all levels of exposure and in different types of suturing skills, we consider that in the SUTT model of training, novices and experienced surgeons can respectively acquire and improve their laparoscopic suturing skills. The findings of this study could have had a stronger value if the SUTT models were performed on larger scale and with a greater number of trainees.
Training in laparoscopic gynecological surgery significantly improves surgeon performance as correlated with operation accuracy, timing and patients’ reduced risk of complications.
The traditional apprentice tutor model has its value and position among other teaching modalities and should be applied during clinical training. The evidence based beneficial outcome after EAGS LPS training and testing creates an ethical as well as an objective issue about training prior to life surgery initiation on patients (Campo et al., 2012a). Laparoscopic suturing is the most fundamental act during an operation; hence, more attention and encouragement on learning the principles, training and exercising should be made on this issue.
In the lack of a universal system for laparoscopic skills assessment, the European Academy proposed and validated the laparoscopic skills testing and training (LASTT) model and performed two studies evaluating its feasibility and the construct validity of three different exercises (camera navigation, camera navigation and forceps handling, and forceps handling and bi-manual coordination), specifically selected to test and train laparoscopic basic psychomotor skills (Molinas and Campo, 2010). This study proposed a new validated tool to assess more complex laparoscopic psychomotor skills: suturing. The SUTT scoring is user friendly and easy to understand. While other studies only compare suturing skills between novices and experts, the Academy model provides a clear level of performance showing that every insufficient score can be improved independently of the surgeon exposure to laparoscopy. Moreover, it provides the ESGE with a validated material in the assessment of specific endoscopic skills, to accomplish the five domains of the new GESEA program.
All gynecologists interested in performing endoscopic surgery should be trained in laparoscopic suturing prior to performing on patients even under supervision. Accomplishment of SUTT and especially achieving excellent scores may help with an excellent start in their surgery career in case of young surgeons while experienced surgeons can maintain their excellent operative results. In both cases higher confidence in laparoscopic surgery is acquired, and possible future complications and lawsuits are decreased. Above all, patients’ safety and surgery outcome presenting the major targets of each minor and major endoscopic surgery can be secured to a great degree. The Academy (EAGS) organizes and supervises training courses and seminars always taking care to provide an objective and effective way of education that substantially can improve patient’s health care (Campo et al., 2012b).
Conclusion
The EAGS SUTT model of training provides an effective didactic method for learning but also testing the abilities of each surgeon in laparoscopic suturing technique. Independently of the level and time of exposure in laparoscopic surgery, the SUTT training course can teach and train surgeons to acquire and substantially improve their laparoscopic suturing skills.
Acknowledgments
We would like to thank Dr Samer Maalouf for the precious assistance in all the statistical data analysis of this paper.
References
- Aggarwal L, Hance J, Undre S, et al. Training junior operative residents in laparoscopic suturing skills is feasible and efficacious. Surgery. 2006;6:729–734. doi: 10.1016/j.surg.2005.12.010. [DOI] [PubMed] [Google Scholar]
- Campo R, Molinas CR, De Wilde RL, et al. Are you good enough for your patients? The European certification model in laparoscopic surgery. Facts Views Vis Obgyn. 2012;(Monograph):21–27. [PMC free article] [PubMed] [Google Scholar]
- Campo R, Reising C, Van Belle Y, et al. valid model fortesting and training laparoscopic psychomotor skills. Gynecol Surg. 2010;7:133–141. [Google Scholar]
- Campo R, Wattiez A, De Wilde RL, et al. Training in laparoscopic surgery: From the lab to the OR. Zdar Var. . 2012;51:285–298. [Google Scholar]
- Campo R, Wattiez A, Wallwiener D, et al. raining and education in endoscopic surgery: is there a future for endoscopy in OB&GYN training? Gynecol Surg. 2005;2:57–65. [Google Scholar]
- Chung SY, Landsittel D, Chon CH, et al. Laparoscopic skills training using a webcam trainer. J Urol. 2005;173:180–183. doi: 10.1097/01.ju.0000145885.28315.a4. [DOI] [PubMed] [Google Scholar]
- Deziel DJ, Millikkan KW, Economou SG, et al. Complications of laparoscopic cholecystectomy: A national survey of 4,292 hospitals and an analysis of 77,604 cases. Am J Surg. 1993;165:9–14. doi: 10.1016/s0002-9610(05)80397-6. [DOI] [PubMed] [Google Scholar]
- Gurusamy k, Aggarwal L, Palanivelu L, et al. Systematic review of randomized controlled trials on the effectiveness of virtual reality training for laparoscopic surgery. Br J Surg. 2008;95:1088–1097. doi: 10.1002/bjs.6344. [DOI] [PubMed] [Google Scholar]
- Heinrich M, Tillo N, Kirlum HJ, et al. Comparison of different training models for laparoscopic surgery in neonates and small infants. Surg Endosc. 2006;20:641–644. doi: 10.1007/s00464-004-2040-7. [DOI] [PubMed] [Google Scholar]
- Kirlum HJ, Heinrich M, Tillo N, et al. Advanced paediatric laparoscopic surgery: repetitive training in rabbit model provides superior skills for live operations. Eur J Pediatr Surg. 2005;15:149–152. doi: 10.1055/s-2005-837600. [DOI] [PubMed] [Google Scholar]
- Kroeze GCS, Mayer EK, Chopra S, et al. Assessment of laparoscopic suturing skills of urology residents: a pan-European study. Eur Urol. 2009;56:865–873. doi: 10.1016/j.eururo.2008.09.045. [DOI] [PubMed] [Google Scholar]
- Mason JD, Ansell J, Warren N, et al. Is motion analysis a valid tool for assessing laparoscopic skill? Surg Endosc. 2013;27:1468–1477. doi: 10.1007/s00464-012-2631-7. [DOI] [PubMed] [Google Scholar]
- Mereu L, Carri G, Albis Florez ED, et al. Three-step model course to teach intracorporeal laparoscopic suturing. doi: 10.1089/lap.2012.0131. J Laparoendosc Adv Surg Tech A. 2013;23:26–32. doi: 10.1089/lap.2012.0131. [DOI] [PubMed] [Google Scholar]
- Misra MC, Bansal VK, Bhowate P, et al. Training in laparoscopic surgery. JIMSA. 2007;20:15–19. [Google Scholar]
- Molinas CR, Campo R. Defining a structured training program for acquiring basic and advanced laparoscopic psychomotor skills in a simulator. Gynecol Surg. 2010;7:427–435. [Google Scholar]
- Molinas CR, De Win G, Ritter O, et al. Feasibility and construct validity of a novel laparoscopic and training model. Gynecol Surg. 2008;5:281–290. [Google Scholar]
- Moorthy K, Munz Y, Dosis A, et al. Bimodal assessment of laparoscopic suturing skills. Surg Endo. 2004;18:1608–1612. doi: 10.1007/s00464-003-9312-5. [DOI] [PubMed] [Google Scholar]
- Pearson AM, Gallagher AG, Rosser JC, et al. Evaluation of structured and quantitative training methods for teaching intracorporeal knot tying. Surg Endosc. 2002;6:130–137. doi: 10.1007/s00464-001-8113-y. [DOI] [PubMed] [Google Scholar]
- Risucci D, Geiss A, Gellman L, et al. Surgeon-specific factors in the acquisition of laparoscopic surgical skills. Am J Surg. 2001;181:289–293. doi: 10.1016/s0002-9610(01)00574-8. [DOI] [PubMed] [Google Scholar]
- Rosenthal ME, Ritter EM, Goova MT. Proficiency-based Fundamentals of laparoscopic surgery skills training results in durable performance improvement and a uniform certification pass rate. Surg Endosc. 2010;24:2453–2457. doi: 10.1007/s00464-010-0985-2. [DOI] [PubMed] [Google Scholar]
- Van der Wal G. Den Haag, the Netherlands: 2007. Risico’s minimaal invasieve chirurgie onderschat. [Google Scholar]
- Van Velthoven RF, Hoffman P. Methods for laparoscopic training using animal models. Curr Urol Rep. 2006;7:114–119. doi: 10.1007/s11934-006-0069-y. [DOI] [PubMed] [Google Scholar]
- Vossen C, Ballaer PV, Shaw RW, et al. Effect of training on endoscopic intracorporeal knot tyring. Hum Reprod. 1997;12:2658–2663. doi: 10.1093/humrep/12.12.2658. [DOI] [PubMed] [Google Scholar]