Abstract
The purpose of this study was to gauge patient perceptions of the RSNA Image Share Project (ISP), a pilot program that provides patients access to their imaging studies online via secure Personal Health Record (PHR) accounts. Two separate Institutional Review Board exempted surveys were distributed to patients depending on whether they decided to enroll or opt out of enrollment in the ISP. For patients that enrolled, a survey gauged baseline computer usage, perceptions of online access to images through the ISP, effect of patient access to images on patient-physician relationships, and interest in alternative use of images. The other survey documented the age and reasons for declining participation for those that opted out of enrolling in the ISP. Out of 564 patients, 470 enrolled in the ISP (83 % participation rate) and 456 of these 470 individuals completed the survey for a survey participation rate of 97 %. Patients who enrolled overwhelmingly perceived access to online images as beneficial and felt it bolstered their patient-physician relationship. Out of 564 patients, 94 declined enrollment in the ISP and all 94 individuals completed the survey for a survey participation rate of 100 %. Patients who declined to participate in the ISP cited unreliable access to Internet and existing availability of non-web-based intra-network images to their physicians. Patients who participated in the ISP found having a measure of control over their images to be beneficial and felt that patient-physician relationships could be negatively affected by challenges related to image accessibility.
Keywords: RSNA Image Share, Patient-physician relationship, Image-enabled personal health records, Image accessibility
Introduction
Access to one’s own diagnostic medical images has traditionally posed significant challenges. Patients often demand copies of their imaging studies for a number of reasons, which include the following: receiving healthcare at multiple institutions with closed-platform imaging networks, interacting with specialists who require access to their images, and seeking second opinions from various radiologists. Currently, patients receive a compact disc (CD) at the conclusion of their imaging study at an institution. This CD is, most often, the only method for patients to access and distribute their images to other institutions or healthcare providers.
However, these CDs pose significant limitations and may be a source of frustration for the patient [1–5]. For example, CDs may be incompatible with another institution’s Picture Archiving and Communications System (PACS). Also, CDs may display images of low quality, leading to repeat imaging at other institutions [6–11]. With the ever increasing complexity of healthcare and patient’s desire for more autonomy over their own imaging, the need for an alternative solution to image sharing has become critical, and reliance on optical media such as CDs may no longer be a feasible option.
As a possible remedy for these concerns, the Radiological Society of North America (RSNA), with support from the National Institute for Biomedical Imaging and Bioengineering (NIBIB), piloted a program that enables secure access and exchange of medical images by patients through secure online vendor-provided image-enabled Personal Health Record (PHR) accounts. The RSNA Image Share Project (ISP) gives control to patients over the access and distribution of their images and associated radiology reports [12]. The security and privacy issues revolving around this project have been discussed previously [13]. In short, a unique 128-bit encrypted single-use identifier called the RSNA ID is created for every patient that participates in the ISP. This RSNA ID consists of an exam/token ID, patient’s birthdate, and a random single-use computer-generated password. Armed with their RSNA ID, patients are able to use online PHR accounts to gain secure web-based access and download their images and reports.
The RSNA ISP spearheads an accelerating trend towards patient-centric imaging. However, this vanguard project for online sharing of images and reports with patients raises several questions. Would patients voluntarily enroll in such a project, and if so, would online security and privacy concerns prevent patients from using the service? How would patient access to images affect the patient-physician relationship? Also, what would patients do with their images after accessing them online?
To date, seven pilot institutions have enrolled in the RSNA ISP and a total of 13,458 patients have enrolled in the project. The patient recruitment experiences at each site reveal a positive outlook for the role of image-sharing in healthcare. But, there was considerable motivation to understand the patients’ decision to enroll or opt out of the ISP. Our study analyzes whether concerns about online security and privacy prevent patients from adopting ISP. Additionally, we attempt to characterize the impact on the patient-physician relationship upon the patient’s adoption of ISP.
Materials and Methods
From a period between June 18, 2013 and August 9, 2013, patients voluntarily enrolled in the RSNA ISP while awaiting their imaging studies at one of the seven pilot sites. Two different IRB-exempted surveys were administered depending on whether a patient wanted to enroll or opt out of participating in the ISP.
For patients enrolled in the ISP, the survey gauged eight different factors (Table 1). For frequency of computer and Internet usage, patients chose from four options: daily, weekly, monthly, or never. To assess patient perceptions towards direct access to medical records and exam images, participants responded to the statements “I like having direct access to my exam images” and “I like having direct access to my medical records” with one of five options: strongly agree, agree, neutral, disagree, and strongly disagree. .
Table 1.
Factors assessed in the survey for patients enrolled in the RSNA Image Sharing Project
| Patient age | Patient perceptions regarding ISP system security |
| Frequency of computer usage | Effects of image accessibility on the patient-physician relationship |
| Frequency of internet usage | Possible alternative uses of images for reasons other than patient care |
| Patient perception towards direct access to medical images | Patient perception towards direct access to their medical records |
To gauge patients’ attitudes towards ISP system security, participants responded to the statement “Since the RSNA Image Share Project relies on security features used by banks, I am comfortable accessing my exam images online” with one of five options: strongly agree, agree, neutral, disagree, or strongly disagree. The effect of image accessibility towards the patient-physician relationship was assessed by asking patients to respond to two statements: “I would find it acceptable if my doctor delayed my appointment because they had difficulty getting access to my medical imaging study” and “I would find it acceptable to repeat my imaging study because my doctor was unable to access it”. Patients chose one of five options to the previous two statements: strongly agree, agree, neutral, disagree, and strongly disagree. Finally, to evaluate alternative usage of imaging for reasons other than patient care, patients were asked to answer affirmatively or negatively to the following questions:
“Would you download the images to your personal computer or device?”
“Would you email your images to family members or friends?”
“Would you post one or more of the images to social media (Facebook, Twitter, or other)?”
“Would you give your password and access information to family members so that they could access your data on the Image Sharing System?”
“Would you ask your physician any NEW questions that you may have after viewing images?”
The survey given to patients who opted out of participating in the ISP asked for their age and reasons for declining participation in the ISP.
Results
During the study period, at the central outpatient-imaging center of one of the academic image sharing sites, a total of 470 patients enrolled in the ISP (83 % participation rate) and 456 of these 470 individuals completed the survey for a survey participation rate of 97 %. The age range of patients who completed the survey was 18–86 years of age, mean age of 52 years, with 64 % female and 36 % male. Ninety-four patients opted out of participating in the ISP and all 94 individuals completed the survey for a survey participation rate of 100 %. The age range of patients who completed the survey was between 19 and 83 years of age; mean age of 55 years, 58 % female and 42 % male.
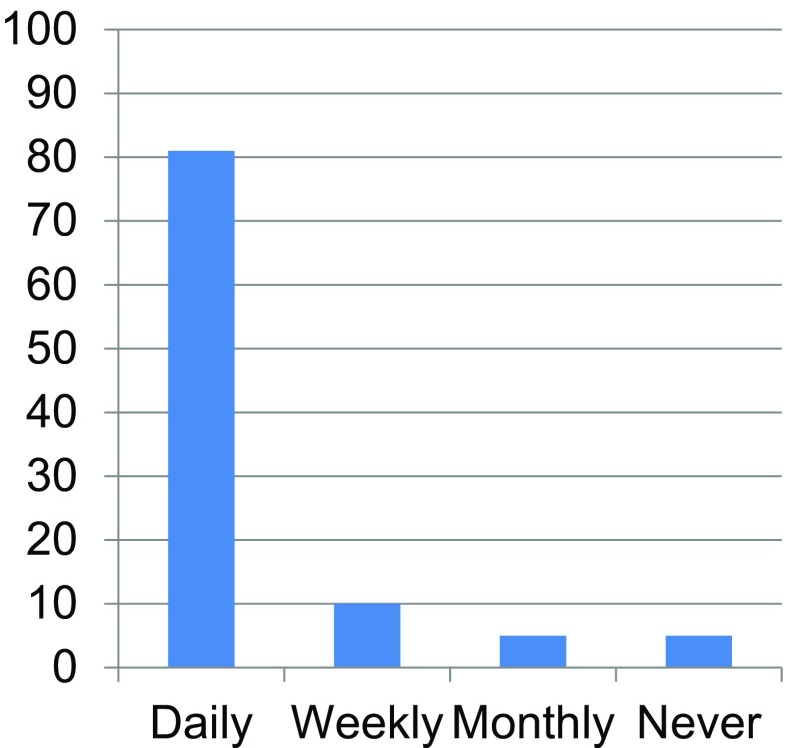
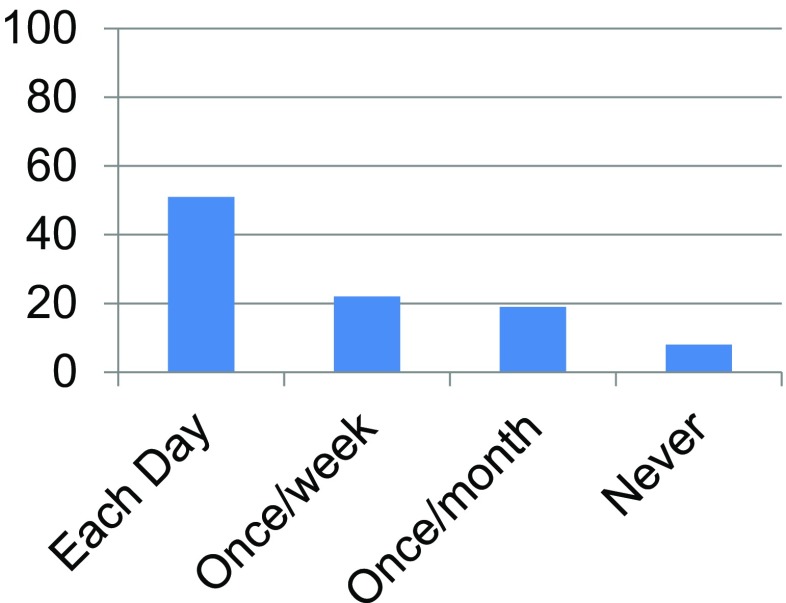
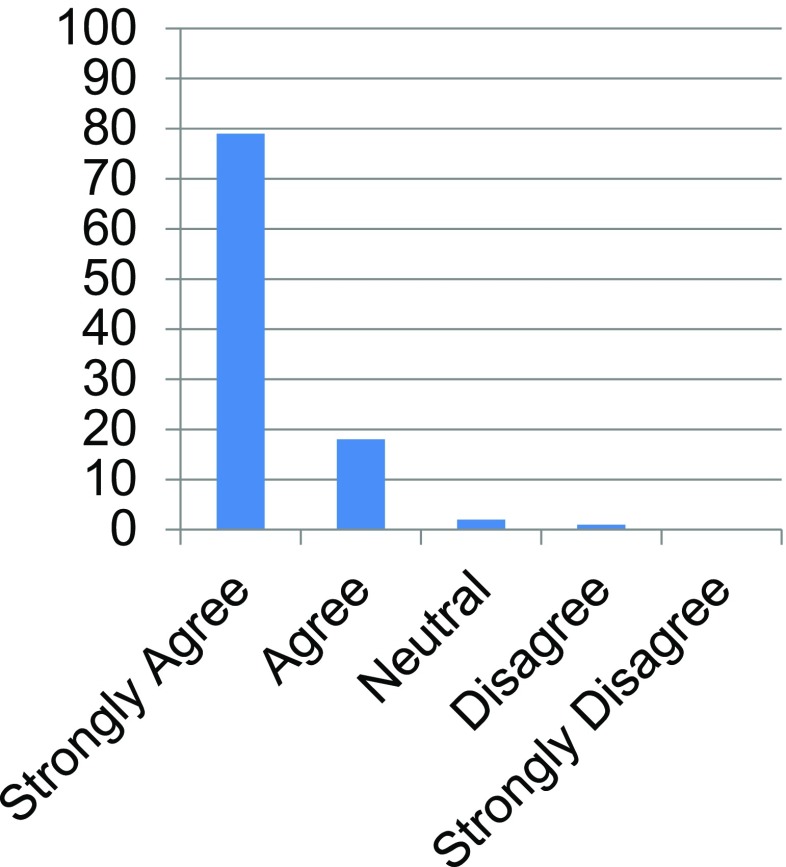
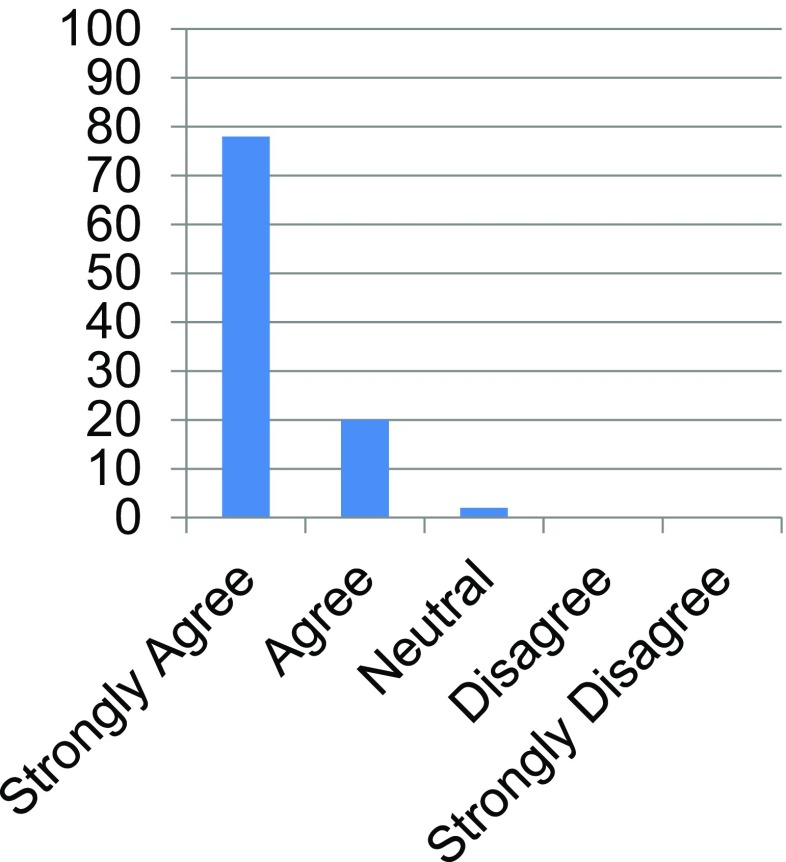
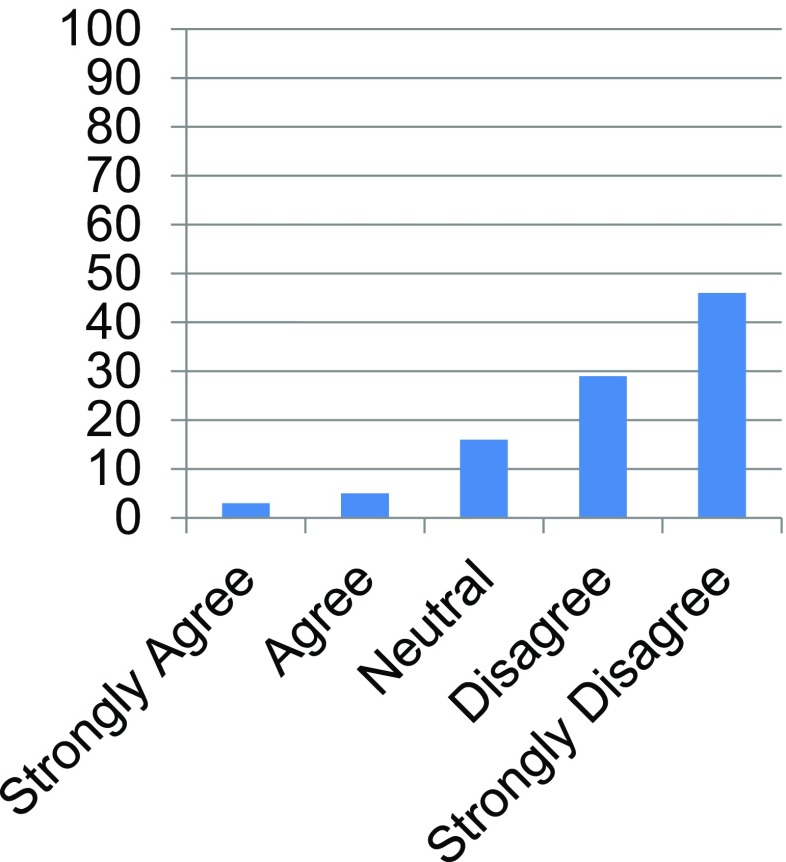
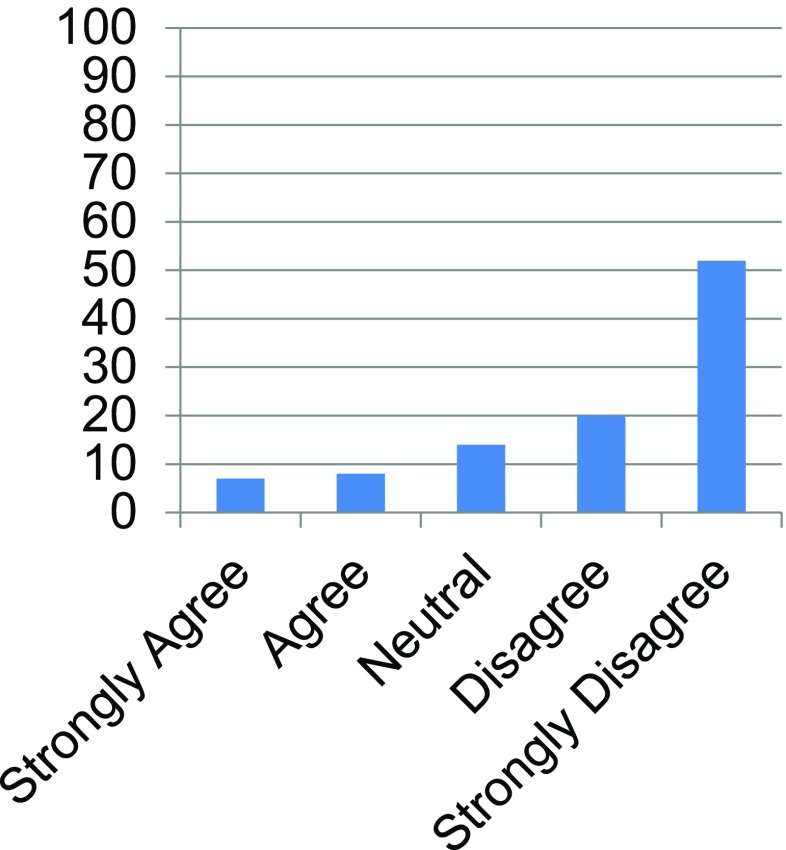
The majority of patients enrolled in the ISP used a computer on a daily basis (>80 %, Fig. 1), and over 50 % of patients utilized the Internet on a daily basis for either online purchases or social media (Fig. 2). The majority of patients (>95 %) expressed a strong desire to have direct access to their exam images and medical records (Figs. 3 and 4). Furthermore, at least 70 % of patients found it unacceptable for a physician to delay an appointment based on difficulty accessing images (Fig. 5) or repeat imaging if unable to access images (Fig. 6). Interestingly, at least 15 % of patients remained neutral.
Fig. 1.
Bar graph demonstrating frequency of computer usage. Vertical axis represents percentage of patients enrolled in the RSNA Image Share Project who responded to the survey
Fig. 2.
Bar graph illustrating frequency of Internet usage. Vertical axis represents percentage of patients enrolled in the RSNA Image Share Project who responded to the survey
Fig. 3.
Patient responses to the statement “I like having direct access to my exam images.” Vertical axis represents percentage of patients enrolled in the RSNA Image Share Project who responded to the survey
Fig. 4.
Patient responses to the statement “I like having direct access to my medical records.” Vertical axis represents percentage of patients enrolled in the RSNA Image Share Project who responded to the survey
Fig. 5.
Patient responses to the statement “I would find it acceptable if my doctor delayed my appointment because they had difficulty getting access to my medical imaging study.” Vertical axis represents percentage of patients enrolled in the RSNA Image Share Project who responded to the survey
Fig. 6.
Patient responses to the statement “I would find it acceptable to repeat my imaging study because my doctor was unable to access it.” Vertical axis represents percentage of patients enrolled in the RSNA Image Share Project who responded to the survey
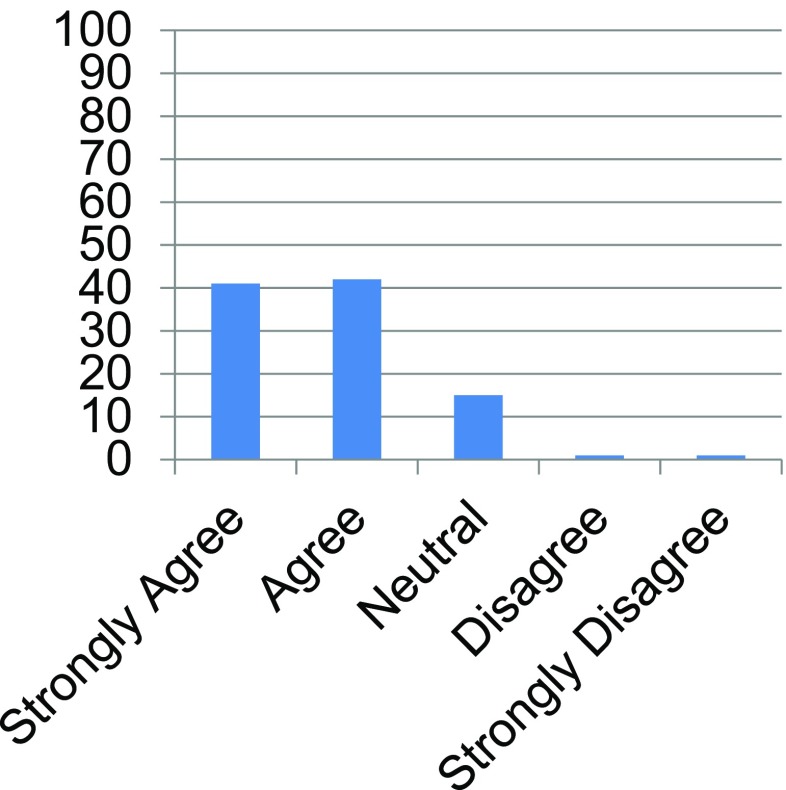
About 85 % of patients either agreed or strongly agreed to feeling comfortable with accessing images using ISP due to its robust security features (Fig. 7). Finally, with regards to alternative usage of images, about 80 % would download images to a personal computer or device, interestingly 32 % would email images to family and friends, 9 % would post images to social media, and 25 % would give password and access information to family members. Also, of note, 97 % of patients would anticipate asking additional questions to their physicians after accessing their images.
Fig. 7.
Patient responses to the statement “Since the RSNA Image Sharing Project relies on security features used by banks, I am comfortable accessing my exam images online.” Vertical axis represents percentage of patients enrolled in the RSNA Image Share Project who responded to the survey
Patients who opted out of the ISP cited three reasons: unreliable Internet access (38 %), existing availability of images to their physicians who already have access to the facility PACS (35 %), as well as the desire to defer enrollment to a later date (27 %).
Discussion
Based on our results, patients express a strong desire to access their own medical images. Patients strongly feel that ease of access to images plays a considerable role in the patient-physician relationship. In fact, our study shows that the majority of patients felt it was unacceptable if physicians delayed appointments due to difficulty accessing the necessary radiologic images. [14]. In addition to improving image accessibility, the ISP has the potential to bolster communication and rapport about medical imaging studies between physicians and patients. As noted before, 97 % of patients indicated that they anticipated that they would ask new questions to their physicians after viewing their images through ISP.
Interestingly, for the subset of patients who opted out of the ISP, the reasons for not enrolling in the project did not involve security issues or technical reasons related to the ISP. In fact, almost one third of the patients wished to defer enrollment to a later date. Another approximately one third (35 %) of patients who opted out of the ISP cited existing availability of images to their physicians via the enterprise PACS. We hypothesize that many of these patient’s physicians were faculty at the institution where the imaging study took place and thus, the physicians had immediate access to their patient’s images via the institution’s closed-network PACS and the patients did not desire to see the images/reports themselves.
An unexpected result from our study was the relatively high percentage of patients that decided to email images to family members and friends (32 %) and give password and access information to family and friends (25 %) which seemed ironic given the tremendous amount of effort that was spent safeguarding images from potential access by family, friends, colleagues, and others. Additionally, 9 % of ISP-enrolled patients were comfortable sharing their images on social media platforms. It should be noted that patients enrolled in ISP had access to images independent of whether their ordering physician was in-network or not. Moreover, while we may have underestimated patients’ eagerness to share their medical data, we understand that many patients do and are entitled to discuss their healthcare with family and friends for advice and various opinions. Also, it is important to note that a patient sharing his/her own images to family/friends does not violate the requirements of the Health Information Portability and Accountability Act (HIPAA) [15]. Nonetheless, current practices in healthcare do not adequately account for patient ownership of medical data. The introduction of patient-centric systems, such as ISP, necessitates the need to explore the dissemination of medical information outside the controlled confines of the institutional healthcare infrastructure.
While our single-institution study adequately gauged the perceptions of patients toward the ISP, it is associated with important limitations. Firstly, we surveyed patients from only one of the seven pilot institutions. Thus, trends in our data may not be generalizable across all institutions participating in the ISP and may not reflect results at other types of institutions that may be considering digital sharing of medical images using a system such as the RSNA’s ISP. Consequently, there may have been selection bias in our study. Since we primarily recruited from our academic site’s outpatient imaging center, the patients undergoing imaging at this facility could have been more likely to be computer-literate, as shown in Fig. 1 where over 80 % of patients participating in the ISP used a computer at least daily. This selection bias may also be reflected in that our outpatient center was located downtown in a major city in the USA. Finally, selection bias was manifested in the almost 2:1 ratio of females to males who participated in the ISP (64 % females, 36 % males). We hypothesize that the large number of females in our study was a direct result of the large volume of women’s imaging and mammography in our outpatient practice.
Additionally, there was no granular exploration of the types of imaging studies that were shared. Knowing what particular imaging studies patients downloaded and shared with their physicians, family, and friends could help optimize future practices in image sharing. For instance, a female patient getting a mammogram may not have been as comfortable downloading her images and sharing them with friends when compared to an MRI of the knee after a fall on the ice.
Also, the survey did not assess patient’s preference for ISP over alternative forms of image-sharing solutions. For instance, patients could be granted access to their images on the hospital’s Health Information Exchange (HIE). Unlike ISP where the patients control access to their images, HIE restricts image-sharing to only those healthcare systems that participate in the hospital’s HIE. The patient’s preference for image-sharing solutions that provide enterprise-centric vs. patient-centric control of images should be explored in future studies.
Another limitation revolved around the fact that we did not survey referring physicians with regards to their perceptions of the ISP. To fully understand the dynamics of the patient-physician relationship, physicians should be surveyed regarding their perceptions of the ISP.
Conclusion
Overall, patients find having a measure of control over their images to be beneficial.
The patient-physician relationship can be negatively affected by challenges related to image accessibility.
The relatively high rate of image sharing with family/friends and on social media remains an unexpected and yet to be explored result from this study.
Additional research will be needed involving physicians as well as patients to better grasp patient and physician perceptions and impact on patient care associated with digital access to images and reports by patients.
Compliance with Ethical Standards
Conflict of Interest
None
Footnotes
Grant: 2013 RSNA Research Medical Student Grant
Contributor Information
Atheeth Hiremath, Email: Atheeth.Hiremath@som.umaryland.edu.
Omer Awan, Phone: 410 913 7787, Email: Omer.awan786@gmail.com.
David Mendelson, Email: David.mendelson@mountsinai.org.
Eliot L. Siegel, Email: unceleliot@gmail.com
References
- 1.Morin RL. Outside images on CD: a management nightmare. J Am Coll Radiol. 2005;2:958. doi: 10.1016/j.jacr.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 2.Flanagan PT, Relyea-Chew A, Gross JA, Gunn ML. Using the Internet for image transfer in a regional trauma network: effect on CT repeat rate, cost, and radiation exposure. J Am Coll Radiol. 2012;9:648–656. doi: 10.1016/j.jacr.2012.04.014. [DOI] [PubMed] [Google Scholar]
- 3.Sung JC, Sodickson A, Ledbetter S. Outside CT imaging among emergency radiology transfer patients. J Am Coll Radiol. 2009;6:626–632. doi: 10.1016/j.jacr.2009.04.010. [DOI] [PubMed] [Google Scholar]
- 4.Sodickson A, Opraseuth J, Ledbetter S. Outside imaging in emergency department transfer patients: CD import reduces rates of subsequent imaging utilization. Radiology. 2011;260:408–413. doi: 10.1148/radiol.11101956. [DOI] [PubMed] [Google Scholar]
- 5.Macura KJ, Carrino JA, Kahn CE., Jr Reviewing images from portable media: an ongoing challenge. J Am Coll Radiol. 2009;6:61–64. doi: 10.1016/j.jacr.2008.08.013. [DOI] [PubMed] [Google Scholar]
- 6.Emick DM, Carey TS, Charles AG, Shapiro ML. Repeat imaging in trauma transfers: a retrospective analysis of computed tomography scans repeated upon arrival to a level I trauma center. J Trauma Acute Care Surg. 2012;72:1255–1262. doi: 10.1097/TA.0b013e3182452b6f. [DOI] [PubMed] [Google Scholar]
- 7.Harrington DT, Connolly M, Biffl WL, Majercik SD, Cioffi WG. Transfer times to definitive care facilities are too long-a consequence of an immature trauma system. Ann Surg. 2005;241:961–966. doi: 10.1097/01.sla.0000164178.62726.f1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Young AJ, Meyers KS, Wolfe L, Duane TM. Repeat computed tomography for trauma patients undergoing transfer to a level I trauma center. Am Surg. 2012;78:675–678. [PubMed] [Google Scholar]
- 9.Lee CY, Bernard AC, Fryman L, Coughenour J, Costich J, Boulanger B, Chang P, Kearney PA. Imaging may delay transfer of rural trauma victims: a survey of referring physicians. J Trauma. 2008;65:1359–1363. doi: 10.1097/TA.0b013e31818c10fc. [DOI] [PubMed] [Google Scholar]
- 10.Haley T, Ghaemmaghami V, Loftus T, Gerkin RD, Sterrett R, Ferrara JJ. Trauma: the impact of repeat imaging. Am J Surg. 2009;198:858–862. doi: 10.1016/j.amjsurg.2009.05.030. [DOI] [PubMed] [Google Scholar]
- 11.Matin A, Bates DW, Sussman A, Ros P, Hanson R, Khorasani R. Inpatient radiology utilization: trends over the past decade. AJR Am J Roentgenol. 2006;186:7–11. doi: 10.2214/AJR.04.0633. [DOI] [PubMed] [Google Scholar]
- 12.RSNA Image Share. Radiological Society of North America. Available at http://www.rsna.org/Image_Share.aspx. Accessed 10 November 2014.
- 13.RSNA Image Share: Letting patients take control of their medical images. Radiological Society of North America. Available at http://rsnaimageshare.org/downloads/3.0/RSNAImageShareNetworkExecutiveOverview3.0.pdf. Accessed 10 November 2014.
- 14.Delbanco T, Walker J. A must-read. Patients should have easier access to their doctors’ medical notes. Mod Healthc. 2011;41:22. [PubMed] [Google Scholar]
- 15.Kavoussi SC, Huang JJ, Tsai JC, Kempton JE. HIPAA for physicians in the information age. Conn Med. 2014;78:425–427. [PubMed] [Google Scholar]