Abstract
In 2012, the Reggio Emilia Breast Cancer Screening Program introduced digital mammography in all its facilities at the same time. The aim of this work is to analyze the impact of digital mammography introduction on the recall rate, detection rate, and positive predictive value. The program actively invites women aged 45–74 years. We included women screened in 2011, all of whom underwent film-screen mammography, and all women screened in 2012, all of whom underwent digital mammography. Double reading was used for all mammograms, with arbitration in the event of disagreement. A total of 42,240 women underwent screen-film mammography and 45,196 underwent digital mammography. The recall rate increased from 3.3 to 4.4 % in the first year of digital mammography (relative recall adjusted by age and round 1.46, 95 % CI = 1.37–1.56); the positivity rate for each individual reading, before arbitration, rose from 3 to 5.7 %. The digital mammography recall rate decreased during 2012: after 12 months, it was similar to the recall rate with screen-film mammography. The detection rate was similar: 5.9/1000 and 5.2/1000 with screen-film and digital mammography, respectively (adjusted relative detection rate 0.95, 95 % CI = 0.79–1.13). The relative detection rate for ductal carcinoma in situ remained the same. The introduction of digital mammography to our organized screening program had a negative impact on specificity, thereby increasing the recall rate. The effect was limited to the first 12 months after introduction and was attenuated by the double reading with arbitration. We did not observe any relevant effects on the detection rate.
Keywords: Breast cancer, Cancer screening, Mammography, Specificity, Digital mammography
Introduction
An organized breast cancer screening program reduces breast cancer mortality [1–3]. Since the 1990s, digital mammography has been tested in screening programs, providing evidence that its accuracy is similar to that of screen-film mammography [4, 5]. Nevertheless, many European screening programs have implemented digital mammography for logistical purposes rather than because of its increased accuracy. The change was inevitable for this reason and also came about due to the shortage of screen-film mammography supplies, the difficulties inherent to film machine maintenance, the need for cumbersome film archives, and, more recently, the lower costs of digital mammography [6].
Nevertheless, shifting from screen-film mammography to digital mammography has a significant organizational impact [7–13] and requires radiologists to undergo retraining or a period of adaptation [7, 8, 14]. In fact, several studies have shown a notable increase in recall rates after the introduction of digital mammography in organized screening [7, 8, 11, 13, 15–22], while the effect on sensitivity has been controversial, with some studies observing a slight increase in the detection rate [7, 11, 15, 20–24] and others observing no change [14, 18, 25, 26]. Even a small decrease in specificity, e.g., an increase in the recall rate, can have a large impact on the screening program workload and can also increase the harms caused by false positives during screening. It is thus important to be aware of the possible effects of switching to digital mammography so that these effects can then be kept in check.
In Reggio Emilia, the screening program-wide transition to digital mammography took place in 2012.
This paper aims to describe the impact of the introduction of digital mammography in the Reggio Emilia Breast Cancer Screening Program on specificity, recall rate, detection rate, and predictive positive value (PPV).
Materials and Methods
Setting
The province of Reggio Emilia, located in northern Italy, has a population of around 550,000. The population-based breast cancer screening program has been active since 1999 and invites all women aged 50–69 years to be screened every 2 years. In 2010, the target population was expanded to include women aged 45–49 years on an annual basis and women aged 70–74 years on a 2-year basis. The total target population was around 60,000 women in 2011. Double reading is used for all mammograms, with arbitration in the event of disagreement; the second reading is not necessarily blind to the first. Mammogram readings for the six provincial mammography centers are all performed by a single coordinating center employing ten radiologists. All radiologists carry out both first and second readings. Kodak was used for all screen-film mammograms.
Data Source
The data source is the screening information system, which collects individual data on each invitation, mammography results (individual readings and final recommendation), second-level examinations, and final histological findings.
We evaluated the aggregated data for 2011–2012, which included information on the age of the women invited to attend, the screening round, and screening results, on whether the examinations were digital or screen-film, the results of each individual reading, together with the details of the first and second radiologists, the final first-level recommendation, and the final histological results (negative, ductal carcinoma in situ (DCIS), invasive cancer).
We included all women screened from 1 January 2011 to 31 December 2012 in the Reggio Emilia screening program. Women who attended spontaneously with symptoms were excluded.
Description of the Introduction of the Digital Mammography
In Reggio Emilia, the transition to digital mammography was implemented on 1 January 2012 installing 11 GE Senographe Essential direct digital systems. The readers had been trained in digital mammography in clinical practice for at least 4–6 months before the switch and only had limited experience in digital mammograms for prevention performed in women outside the screening target age.
Statistical Analyses
The study reports the recall rate, detection rate (all cancers and DCIS only), positive predictive value, and estimated specificity with relative 95 % CI. All rates were adjusted by direct standardization using the age (5-year bracket) and screening round (first vs. subsequent) distribution of the screened population in 2011 and in 2012.
In order to calculate the specificity (true negative/(true negative + false positive)), we estimated the true negative by subtracting the expected number of interval cases in the first year from the total number of negative women; interval cases were estimated on the basis of regional estimates [27], e.g., 10 % of screen-detected cases.
We present the monthly recall rate and PPV level trends for the 2-year period. We tested the significance of the linear trend using chi-squared test.
To show the variability among readers, we built logistical models to test the effect of each individual reader, with adjustments for reading type and first/second reading using two different dependent variables: positivity (mammograms classified as positive by the reader) and false negatives (mammograms classified as negative by the reader then identified as positive in the final recommendation in which cancer was found). To test whether the variability among readers was higher than would be expected by chance, we built a multilevel model, with adjustments for mammogram type and first/second reading, in which the reader was the cluster level. The results of the cluster level component are reported: the probability that alpha coefficient is equal to zero is the probability that the cluster level effect is due to random fluctuations. Analyses were performed using the STATA statistical package version 13.
Ethics
This study was conducted in accordance with the routine quality assurance procedures established by the Local Health Authority for its screening programs. The Reggio Emilia Cancer Registry, which routinely collects the screening history of each case of breast cancer, has been approved by the Provincial Ethic Committee.
Results
During 2011–2012, 87,436 screening mammograms were performed, all of which are included in this study. Of these, 42,240 were screen-film mammograms performed in 2011 (9722 first screening and 32,518 subsequent screening) and 45,196 were digital mammograms performed in 2012 (6311 first screen and 38,885 subsequent screening) (Table 1). There were 485 screen-detected cancers (250 with screen-film mammography and 235 with digital mammography), of which 83 were DCIS (42 with screen-film mammography and 41 with digital mammography) (Table 1). The mean age was 56 years (56.2 years for the screen-film mammography group and 55.7 years for the digital mammography group) (Table 1).
Table 1.
Overall results and results by screening round and age
| Screened women | Invasive cancers | DCIS | Recall rate (%) | PPV (%) | Detection rate per 1000 | Specificity (%) | ||
|---|---|---|---|---|---|---|---|---|
| Overall | Film-screen mammography | 42,240 | 208 | 42 | 3.3 | 18.0 | 5.9 | 97.3 |
| Digital mammography | 45,196 | 194 | 41 | 4.4 | 11.8 | 5.2 | 96.1 | |
| Film-screen mammography | First screen | 9722 | 34 | 10 | 5.5 | 8.3 | 4.5 | 95.0 |
| Subsequent screen | 32,518 | 174 | 32 | 2.6 | 24.0 | 6.3 | 98.0 | |
| Digital mammography | First screen | 6311 | 28 | 7 | 9.2 | 6.0 | 5.5 | 91.3 |
| Subsequent screen | 38,885 | 166 | 34 | 3.6 | 14.3 | 5.1 | 96.9 | |
| Film-screen mammography | 45–49 years | 14,354 | 30 | 7 | 4.3 | 6.0 | 2.6 | 95.9 |
| 50–54 years | 7208 | 27 | 8 | 3.0 | 16.1 | 4.9 | 97.5 | |
| 55–59 years | 5405 | 26 | 6 | 2.3 | 26.2 | 5.9 | 98.3 | |
| 60–64 years | 5602 | 30 | 6 | 3.0 | 27.2 | 8.2 | 97.8 | |
| 65–69 years | 5732 | 35 | 8 | 2.3 | 32.1 | 7.5 | 98.4 | |
| 70–74 years | 3939 | 50 | 7 | 3.2 | 44.9 | 14.5 | 98.2 | |
| Digital mammography | 45–49 years | 16,144 | 24 | 14 | 5.9 | 5.1 | 3.0 | 94.4 |
| 50–54 years | 7387 | 32 | 3 | 4.2 | 11.3 | 4.7 | 96.3 | |
| 55–59 years | 5997 | 28 | 5 | 3.5 | 15.6 | 5.5 | 97.0 | |
| 60–64 years | 6650 | 34 | 4 | 3.1 | 18.7 | 5.7 | 97.5 | |
| 65–69 years | 6039 | 40 | 8 | 3.4 | 23.6 | 7.9 | 97.4 | |
| 70–74 years | 2979 | 26 | 7 | 3.7 | 29.7 | 11.1 | 97.3 |
All invasive cancers and DCIS are included
Comparison of Film and Digital Mammography Recall Rates, Specificity, PPV, and Detection Rates
A total of 1388 women (3.3 %) in the screen-film mammography group and 1986 women (4.4 %) in the digital mammography group were recalled (Table 1).
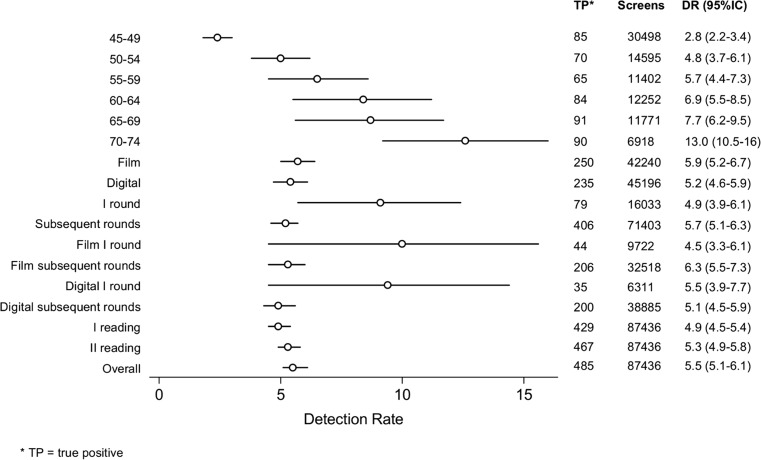
The detection rate was higher in older women for both screen-film and digital mammography (Table 1). The unadjusted detection rate was higher in subsequent rounds, but age-adjusted rates were much higher in the first screening round than in subsequent rounds.
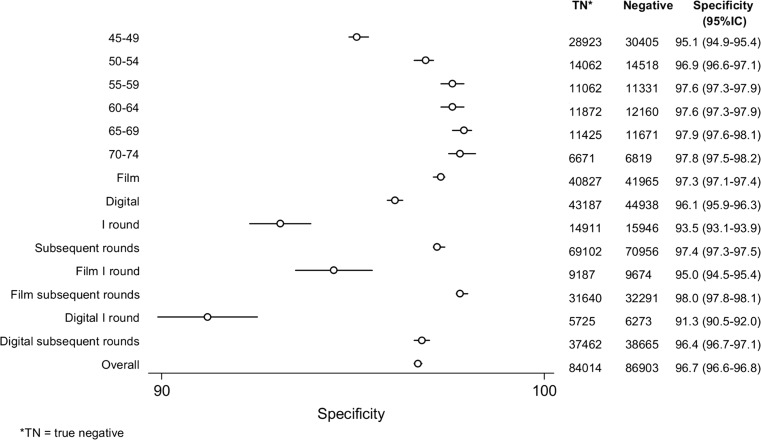
Taking into account age and round (first vs. subsequent), the recall rate was lower for film-screen mammography than for digital mammography (RR = 1.46, 95 % CI = 1.37–1.56) (Table 1). Specificity increased with age until reaching a plateau for women over 55 years of age (Fig. 1). The age and screening round-adjusted detection rate was slightly lower for digital mammography (5.4/1000) than for screen-film mammography (5.7/1000), with the difference possibly being due to a random fluctuation (RR = 0.95, 95 % CI = 0.79–1.13) (Fig. 2). As a result, the positive predictive value was lower for digital mammography than for screen-film mammography (RR = 0.70, 95 % CI = 0.59–0.84). We did not observe any difference in the detection rate for DCIS: the relative digital vs. film-screen mammography detection rate was 0.91 (95 % CI = 0.59–1.40). In order to avoid biases due to the expansion of the target population in 2010, we also calculated the age, passage-adjusted relative recall rate, and detection rate for the 45–69-year-old subgroup (RR = 1.50, 95 % CI = 1.19–1.89; RR = 1.00, 95 % CI 0.81–1.22).
Fig. 1.
Specificity per 100 screens adjusted by age (95 % confidence interval)
Fig. 2.
Cancers and DCIS detection rate per 1000 screens adjusted by age and screening round (95 % confidence interval)
The comparison between screen-film and digital mammography was also made within groups. The recall rate was higher in digital mammography than in screen-film mammography for all age groups, both during the first and subsequent screening rounds. The biggest difference was observed for the first screening, with a recall rate for digital mammography of 9.2 % compared to 5.5 % for screen-film mammography. Differences in detection rate between screen-film and digital mammography were small and similar among all age groups and screening rounds (Table 1).
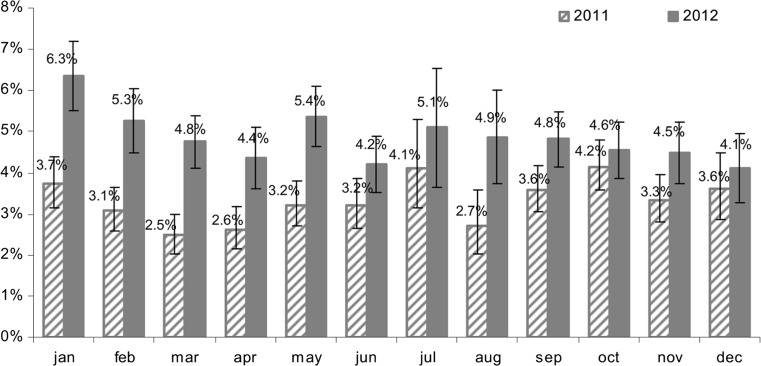
Learning Curve
The recall rate changed slightly during the study periods: the age and round-adjusted recall rate were almost stable during 2011 (screen-film mammography) (p = 0.15), while in 2012 (digital mammography) (Fig. 3), the recall rate decreased from January to December (p = 0.02). In December 2012, the digital mammography recall rate reached that of screen-film mammography observed in December 2011. The positive predictive value recorded an opposite trend during the two periods, decreasing in 2011 (p = 0.02) and increasing in 2012 (p = 0.26).
Fig. 3.
Recall rate per 100 screens by month and mode of screening: film-screen (2011) and digital (2012)
Variability Between Readers
Each mammogram was read by two radiologists and by a third referee if the two initial diagnoses disagreed. We analyzed the results of each individual reading and the effect of the introduction of digital mammography on the variability between readers (Table 2). The positivity rate for each individual reading was higher in digital mammography (RR = 0.48, 95 % CI = 0.43–0.54) (Table 3). The adjusted increase in the individual radiologist positivity rate was higher than the increase in the recall rate because double reading and arbitration reduced the impact of the individual radiologist positivity rate on the recall rate. The positivity rate varied between the most and the least conservative radiologists by about 35 %. The individual radiologist component of the variance, estimated using a multilevel model, was small but significant (alpha = 0.009; likelihood ratio of alpha = 0:chi2(df01) = 59.8, p < 0.0005). The recall rate variance among readers was higher with digital than with screen-film mammography (screen-film mammography: alpha 0.011, 95 % CI = 0.003–0.036; digital mammography: alpha 0.026, 95 % CI = 0.01–0.06), but the difference may be due to chance.
Table 2.
Film-screen and digital mammography recall rate and detection rate by readers
| Readers | Film-screen mammography | Digital mammography | Film-screen mammography recall rate (%) | Digital mammography recall rate (%) | Film-screen mammography detection rate per 1000 | Digital mammography detection rate per 1000 |
|---|---|---|---|---|---|---|
| Reader a | 12,371 | 13,752 | 2.9 | 4.8 | 4.4 | 4.5 |
| Reader b | 7060 | 6166 | 3.0 | 5.7 | 5.4 | 3.7 |
| Reader c | 7965 | 9500 | 2.7 | 6.5 | 4.9 | 4.9 |
| Reader d | 8497 | 7779 | 2.3 | 5.6 | 4.9 | 5.0 |
| Reader e | 5320 | 4519 | 2.6 | 5.3 | 4.5 | 3.8 |
| Reader f | 7117 | 6485 | 2.8 | 6.0 | 6.7 | 4.0 |
| Reader g | 15,175 | 16,075 | 3.4 | 3.6 | 7.4 | 4.9 |
| Reader h | 3692 | 7612 | 3.4 | 6.5 | 5.4 | 5.9 |
| Reader i | 6832 | 6640 | 3.4 | 5.0 | 4.0 | 4.7 |
| Reader j | 10,451 | 11,864 | 3.1 | 6.2 | 5.7 | 5.3 |
| Overall | 84,480 | 90,392 | 3.0 | 5.4 | 5.5 | 4.8 |
All invasive cancers and DCIS are included
Table 3.
Probability of positive results and risk of false-negative results by order of reading, screening round, type of mammography, and reader. Multivariate analysis with Poisson model
| False positive | False negative | |||||
|---|---|---|---|---|---|---|
| RR | p value | 95 % CI | RR | p value | 95 % CI | |
| First reader | Ref. | Ref. | ||||
| Second reader | 1.01 | 0.629 | 0.97–1.06 | 0.33 | 0.000 | 0.19–0.56 |
| Film-screen mammography | Ref. | Ref. | ||||
| Digital mammography | 1.78 | 0.000 | 1.69–1.87 | 1.22 | 0.403 | 0.77–1.93 |
| Reader a | Ref. | Ref. | ||||
| Reader b | 1.12 | 0.030 | 1.01–1.24 | 0.53 | 0.269 | 0.17–1.63 |
| Reader c | 1.20 | 0.000 | 1.10–1.32 | 0.64 | 0.338 | 0.26–1.59 |
| Reader d | 1.02 | 0.766 | 0.92–1.12 | 1.16 | 0.713 | 0.53–2.50 |
| Reader e | 1.01 | 0.917 | 0.89–1.13 | 0.98 | 0.966 | 0.35–2.72 |
| Reader f | 1.12 | 0.026 | 1.01–1.24 | 1.16 | 0.714 | 0.52–2.63 |
| Reader g | 0.90 | 0.018 | 0.83–0.98 | 0.35 | 0.024 | 0.14–0.87 |
| Reader h | 1.28 | 0.000 | 1.16–1.42 | 0.48 | 0.244 | 0.14–1.66 |
| Reader i | 1.07 | 0.179 | 0.97–1.19 | 0.65 | 0.455 | 0.22–1.99 |
| Reader j | 1.21 | 0.000 | 1.11–1.32 | 0.53 | 0.151 | 0.22–1.26 |
The risk of a false-negative result for each individual reading was slightly, but not significantly, higher in digital mammography (RR = 1.2, 95 % CI = 0.77–1.93) (Table 3). The second reader had a much lower risk of false negative, but this is a consequence having access to the first reading result. The risk of a false negative varied between the most and the least sensitive radiologists by a factor of about two, but this variance was not significant overall (alpha = 0.07; likelihood-ratio test of alpha = 0:chibar2(01) = 1.17, p > 0.139) nor when stratified by mammogram type (screen-film mammography: likelihood-ratio test alpha = 0:chibar2(01) = 1.00, p = 0.159; digital mammography: likelihood-ratio test alpha = 0:chibar2(01) = 0.03, p = 0.427).
Discussion
In the Reggio Emilia Breast Cancer Screening Program, the introduction of digital mammography had a non-negligible effect on the recall rate. The effect was more pronounced during the first few months, but was no longer detectable after 1 year. The higher recall rate did not have any significant impact on the detection rate.
In our setting, the switch from screen-film to digital mammography took place in all the organized screening program facilities at the same time. The readers had been trained in digital mammography, although not specifically within the screening setting and with the target age group, and consequently had limited experience of preventive mammograms. As expected, when making the switch from clinical mammograms to preventive mammograms, it takes longer to improve specificity than sensitivity [7].
However, this rapid transformation gave us the opportunity to measure the differences between the two screening methods in a natural experiment.
Our results are similar to those of previous studies on several points: many papers found lower specificity or higher recall rates for digital vs. screen-film mammography [7, 8, 11, 13, 15–22], while only few observed similar or lower recall rates with digital mammography when it was first introduced [9, 12, 23–25, 28]. Furthermore, our observations relating to detection rates are not surprising. In fact, although most literature and a systematic review noted higher detection rates than for screen-film mammography [7, 11, 15, 20–24], many other authors found no increase in detection rates or sensitivity [14, 18, 25, 26]. Nevertheless, our data on 45–69-year-old women shows exactly the same detection rate in the two periods. This age-related subgroup was unaffected by the expansion of the target population that took place in April 2010. In fact, the 70–74-year age groups had only recently been included within the target age group; consequently, the actual interval was between 2 and 5 years for all these women in 2011 and for a smaller fraction in 2012.
The increased detection rate cannot be considered an increase in sensitivity per se nor necessarily an advantage in terms of breast cancer screening. Some authors have found that the increase was almost entirely due to DCIS [14], while another study found that digital mammography screen-detected cancers comprised a higher proportion of high-risk cancers in terms of genetic characteristics [29]. Only one study observed a reduction in interval cancers [20], while two others found no effect on interval cancers [14, 30], suggesting that not all detection rate increases will boost screening efficacy, although they may lead to a rise in overdiagnosis. Our study is not powerful enough to observe differences in DCIS detection. However, we did not observe any increases.
In terms of induced ascertainments, the excess was only noteworthy for the first 6 months after introduction of digital mammography when the second-level workload was almost doubled. After the summer, however, the number of ascertainments was almost identical to that of the previous year during the same period. Some studies analyzed trends and learning curves and found that the effect was more pronounced in, or limited to, the initial period. Other studies observed both a short-term increase in the recall rate, mainly in the first year, which then almost disappeared [8] or even fell in the long term [14]. The short-term peak of positivity should be taken into account when introducing digital mammography into a screening program: in general, even a small change in the specificity of the screening algorithm may have a major impact on program organization, while the impact of sensitivity changes only have a minor impact on organization, but a bigger impact on screening efficacy. In our study, there was a bigger increase in the recall rate among women attending their first screening round than among those attending subsequent rounds. It is possible that the availability of previous screen-film mammograms, which were consulted before making a recall decision, may have partially reduced the impact of digital mammography on the recall rate.
Finally, it is worth noting that the effect was not identical for all radiologists: the recall rate variability among radiologists rose slightly. The use of double reading in our program, accompanied by arbitration in the event of disagreements, must have reduced the impact of the introduction of digital mammography on the recall rate. In order to control the loss of specificity during the initial period of digital mammography implementation, it may therefore be a good strategy to have the most experienced digital mammography radiologists arbitrating as the third reader.
Strengths and Limitations
One of the strengths of our study was that the data used was collected as part of a routine screening program rather than from a research setting. What we observed is probably what would happen in many other routine screening programs introducing digital mammography. On the other hand, our comparison does not come from a randomized design and it is therefore impossible to rule out changes in the incidence and prevalence of breast cancer during the study period. We did not have enough follow-up time to analyze interval cancers after digital mammography or the detection rate of advanced cancer during subsequent rounds: these are the only two indicators that can measure screening sensitivity. We therefore plan to carry out all these analyses over the next few years. Furthermore, although a large number of women were included in the study, the number of cancers was small. Thus, even considerable differences in the sensitivity of the two screening techniques could not be detected as statistically significant and it was difficult to study the learning curve for sensitivity.
Conclusions
The introduction of digital mammography in our organized screening programs led to an increased recall rate. The effect was limited to the first few months after the introduction and was attenuated by the double reading with arbitration. We did not observe any effect on detection rate.
Acknowledgments
Authors’ Contribution
Study concepts were contributed by PGR, PP, and CC. Study design was done by PGR and CC. Data acquisition was performed by PM, CC, PP, and SR. Quality control of data and algorithms was ensured by PM. Data analysis and interpretation were done by PGR, PM, and CC. Statistical analysis was performed by PM and CC. Manuscript preparation was done by PGR. Manuscript editing and review were done by all authors.
Compliance with Ethical Standards
This study was conducted in accordance with the routine quality assurance procedures established by the Local Health Authority for its screening programs. The Reggio Emilia Cancer Registry, which routinely collects the screening history of each case of breast cancer, has been approved by the Provincial Ethic Committee.
Footnotes
Key Points
• The introduction of digital mammography in screening produced an initial increase in the recall rate.
• After 12 months, the recall rate returned to the levels achieved with screen-film mammography.
• We did not observe any effects on the detection rate.
• We did not observe any increase in ductal carcinoma in situ (DCIS) detection.
Contributor Information
Cinzia Campari, Email: cinzia.campari@ausl.re.it.
Paolo Giorgi Rossi, Email: paolo.giorgirossi@ausl.re.it.
Carlo Alberto Mori, Email: carloalberto.mori@asmn.re.it.
Sara Ravaioli, Email: sara.ravaioli@asmn.re.it.
Andrea Nitrosi, Email: andrea.nitrosi@asmn.re.it.
Rita Vacondio, Email: rita.vacondio@asmn.re.it.
Pamela Mancuso, Phone: +390522335499, Email: pamela.mancuso@ausl.re.it.
Antonella Cattani, Email: antonella.cattani@ausl.re.it.
Pierpaolo Pattacini, Email: pierpaolo.pattacini@asmn.re.it.
References
- 1.Segnan N, Patnick J, von Karsa L Eds. European guidelines for quality assurance in colorectal cancer screening and diagnosis. 1st edition. Edited by Luxembourg: European Communities, 2010:1–339
- 2.Independent UK Panel on Breast Cancer Screening The benefits and harms of breast cancer screening: an independent review. Lancet. 2012;380(9855):1778–1786. doi: 10.1016/S0140-6736(12)61611-0. [DOI] [PubMed] [Google Scholar]
- 3.Paci E, Broeders M, Hofvind S, the EUROSCREEN Working Group et al. European Breast Cancer Service Screening Outcomes: A First Balance Sheet of the Benefits and Harms. Cancer Epidemiol Biomarkers Prev. 2014;23(7):1159–1163. doi: 10.1158/1055-9965.EPI-13-0320. [DOI] [PubMed] [Google Scholar]
- 4.Vinnicombe S, Pinto Pereira SM, McCormack VA, et al. Full-field digital versus screen-film mammography: comparison within the UK breast screening program and systematic review of published data. Radiology. 2009;251(2):347–358. doi: 10.1148/radiol.2512081235. [DOI] [PubMed] [Google Scholar]
- 5.Skaane P. Studies comparing screen-film mammography and full-field digital mammography in breast cancer screening: updated review. Acta Radiol. 2009;50(1):3–14. doi: 10.1080/02841850802563269. [DOI] [PubMed] [Google Scholar]
- 6.Comas M, Arrospide A, Mar J, et al. Budget impact analysis of switching to digital mammography in a population-based breast cancer screening program: a discrete event simulation model. PLoS One. 2014;9(5):e97459. doi: 10.1371/journal.pone.0097459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bluekens AM, Karssemeijer N, Beijerinck D, et al. Consequences of digital mammography in population-based breast cancer screening: initial changes and long-term impact on referral rates. Eur Radiol. 2010;20(9):2067–2073. doi: 10.1007/s00330-010-1786-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.van Luijt PA, Fracheboud J, Heijnsdijk EA, National Evaluation Team for Breast Cancer Screening in Netherlands Study Group (NETB) et al. Nation-wide data on screening performance during the transition to digital mammography: observations in 6 million screens. Eur J Cancer. 2013;49(16):3517–3525. doi: 10.1016/j.ejca.2013.06.020. [DOI] [PubMed] [Google Scholar]
- 9.Vigeland E, Klaasen H, Klingen TA, et al. Full-field digital mammography compared to screen film mammography in the prevalent round of a population-based screening programme: the Vestfold County Study. Eur Radiol. 2008;18(1):183–191. doi: 10.1007/s00330-007-0730-y. [DOI] [PubMed] [Google Scholar]
- 10.Karssemeijer N, Bluekens AM, Beijerinck D, et al. Breast cancer screening results 5 years after introduction of digital mammography in a population-based screening program. Radiology. 2009;253(2):353–358. doi: 10.1148/radiol.2532090225. [DOI] [PubMed] [Google Scholar]
- 11.Bjurstam N, Hofvind S, Pedersen K, et al: Full-field digital mammography screening in the population based screening program in North-Norway: preliminary results. Radiology /241(P):/392,2006.
- 12.Perry NM, Pinto Pereira SM, McCormack VA, et al: Comparison of full-field digital mammography with conventional screen-film mammography within a population-based breast screening program. Radiology /245(P):/382,2007.
- 13.Nederend J, Duijm LE, Louwman MW, et al. Impact of transition from analog screening mammography to digital screening mammography on screening outcome in The Netherlands: a population-based study. Ann Oncol. 2012;23(12):3098–3103. doi: 10.1093/annonc/mds146. [DOI] [PubMed] [Google Scholar]
- 14.Hofvind S, Skaane P, Elmore JG, et al. Mammographic performance in a population-based screening program: before, during, and after the transition from screen-film to full-field digital mammography. Radiology. 2014;272(1):52–62. doi: 10.1148/radiol.14131502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bluekens AM, Holland R, Karssemeijer N, et al. Comparison of digital screening mammography and screen-film mammography in the early detection of clinically relevant cancers: a multicenter study. Radiology. 2012;265(3):707–714. doi: 10.1148/radiol.12111461. [DOI] [PubMed] [Google Scholar]
- 16.Nederend J, Duijm LE, Louwman MW, et al. Impact of the transition from screen-film to digital screening mammography on interval cancer characteristics and treatment - a population based study from the Netherlands. Eur J Cancer. 2014;50:31–39. doi: 10.1016/j.ejca.2013.09.018. [DOI] [PubMed] [Google Scholar]
- 17.Skaane P, Young K, Skjennald A. Population-based mammography screening: comparison of screen-film mammography and full-field digital mammography using soft-copy reading: the Oslo I study. Radiology. 2003;229:877–884. doi: 10.1148/radiol.2293021171. [DOI] [PubMed] [Google Scholar]
- 18.Skaane P, Skjennald A, Young K, et al. Follow-up and final results of the Oslo I study comparing screen-film mammography and full-field digital mammography with soft-copy reading. Acta Radiol. 2005;46:679–689. doi: 10.1080/02841850500223547. [DOI] [PubMed] [Google Scholar]
- 19.Skaane P, Skjennald A. Screen-film mammography versus full-field digital mammography with soft-copy reading: randomized trial in a population-based screening program - the Oslo II study. Radiology. 2004;232:197–204. doi: 10.1148/radiol.2321031624. [DOI] [PubMed] [Google Scholar]
- 20.Skaane P, Hofvind S, Skjennald A. Randomized trial of screen-film versus full-field digital mammography with soft-copy reading in population-based screening program: follow-up and final results of Oslo II study. Radiology. 2007;244:708–717. doi: 10.1148/radiol.2443061478. [DOI] [PubMed] [Google Scholar]
- 21.Del Turco MR, Mantellini P, Ciatto S, et al. Full-field digital versus screen-film mammography: comparative accuracy in concurrent screening cohorts. AJR Am J Roentgenol. 2007;189(4):860–866. doi: 10.2214/AJR.07.2303. [DOI] [PubMed] [Google Scholar]
- 22.Karssemeijer N, Beijerinck D, Visser R, et al: Effect of introduction of digital mammography with CAD in a population based screening program. Eur Radiol /Suppl 1:/151_2,2008.
- 23.Heddson B, Roennow K, Olsson M, et al. Digital versus screen-film mammography: a retrospective comparison in a population-based screening program. Eur J Radiol /64:/419-25,2007. [DOI] [PubMed]
- 24.Pisano ED, Gatsonis C, Hendrick E, et al. Diagnostic performance of digital versus film mammography for breast-cancer screening. N Engl J Med. 2005;353:1773–1783. doi: 10.1056/NEJMoa052911. [DOI] [PubMed] [Google Scholar]
- 25.Lewin JM, D’Orsi CJ, Hendrick RE, et al. Clinical comparison of full-field digital mammography and screen-film mammography for detection of breast cancer. Am J Roentgenol. 2002;179:671–677. doi: 10.2214/ajr.179.3.1790671. [DOI] [PubMed] [Google Scholar]
- 26.Kerlikowske K, Hubbard RA, Miglioretti DL, et al. Comparative effectiveness of digital versus film-screen mammography in community practice in the United States: a cohort study. Ann Intern Med. 2011;155(8):493–502. doi: 10.7326/0003-4819-155-8-201110180-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bucchi L, Ravaioli A, Foca F, Emilia-Romagna Breast Screening Programme et al. Incidence of interval breast cancers after 650,000 negative mammographies in 13 Italian health districts. J Med Screen. 2008;15(1):30–35. doi: 10.1258/jms.2008.007016. [DOI] [PubMed] [Google Scholar]
- 28.Sala M, Comas M, Macià F, et al. Implementation of digital mammography in a population-based breast cancer screening program: effect of screening round on recall rate and cancer detection. Radiology. 2009;252(1):31–39. doi: 10.1148/radiol.2521080696. [DOI] [PubMed] [Google Scholar]
- 29.Drukker CA, Schmidt MK, Rutgers EJ, et al. Mammographic screening detects low-risk tumor biology breast cancers. Breast Cancer Res Treat. 2014;144(1):103–111. doi: 10.1007/s10549-013-2830-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hoff SR, Abrahamsen AL, Samset JH, et al. Breast cancer: missed interval and screening-detected cancer at full-field digital mammography and screen-film mammography results from a retrospective review. Radiology. 2012;264(2):378–386. doi: 10.1148/radiol.12112074. [DOI] [PubMed] [Google Scholar]