Abstract
Paclitaxel is widely used in the treatment of patients with metastatic breast cancer (MBC). Formulations of paclitaxel contain surfactants and solvents or albumin derived from human blood. The use of co-solvents such as polyoxyethylated castor oil is thought to contribute to toxicity profile and hypersensitivity reactions as well as leaching of plasticizers from polyvinyl chloride bags and infusion sets. Currently, nab-paclitaxel, an albumin-bound paclitaxel in nanometer range continues to be the preferred taxane formulation used in clinic. This study (CTRI/2010/091/001116) investigated the efficacy and tolerability of a polyoxyethylated castor oil- and albumin-free formulation of paclitaxel [paclitaxel injection concentrate for nanodispersion (PICN)] compared with nab-paclitaxel in women with refractory MBC. The current study was a multicenter, open-label, parallel-group, randomized, comparative phase II/III trial evaluating the efficacy and safety of PICN (260 mg/m2 [n = 64] and 295 mg/m2 [n = 58] every 3 weeks) compared with nab-paclitaxel (260 mg/m2 every 3 weeks [n = 58]) in women 18 and 70 years old with confirmed MBC. Overall response rate (ORR) was assessed with imaging every 2 cycles. An independent analysis of radiologic data was performed for evaluable patients. Progression-free survival (PFS) was a secondary efficacy measure. Independent radiologist-assessed ORRs in the evaluable population of women aged ≥70 years were 35, 49, and 43 % in the PICN 260 mg/m2, PICN 295 mg/m2, and nab-paclitaxel 260 mg/m2 arms, respectively. Median PFS in the evaluable population was 23, 35, and 34 weeks in the PICN 260 mg/m2, PICN 295 mg/m2, and nab-paclitaxel 260 mg/m2 arms, respectively. Adverse events occurred in similar proportions of patients across treatment arms. Hypersensitivity reactions were not frequently observed with the clinical use of PICN across the treatment cohorts. In women with metastatic breast cancer, PICN at 260 and 295 mg/m2 every 3 weeks was effective and well tolerated and showed similar tolerability compared with nab-paclitaxel 260 mg/m2 every 3 weeks. Statistically, significant differences were not observed in the PICN and nab-paclitaxel treatment arms for radiologist-assessed ORR or median PFS. The novel paclitaxel formulation, PICN, offers apart from efficacy, potential safety advantage of decreased use of corticosteroid pretreatment and the absence of the risk of transmission of blood product-borne disease.
Keywords: Breast neoplasms, Chemistry, Pharmaceutical, Disease-free survival, Paclitaxel
Implications for practice
The chemotherapeutic agent paclitaxel is widely used in the treatment of women with metastatic breast cancer (MBC). However, currently available formulations contain additives, such as surfactants, solvents that are potentially toxic or lead to hypersensitivity reactions. The current study investigated the efficacy and safety of paclitaxel injection concentrate for nanodispersion (PICN), which is free of these additives, in women with refractory MBC. Based on radiologist-assessed overall response rate and progression-free survival, PICN is as effective and well tolerated as nab-paclitaxel, an albumin-bound paclitaxel in nanometer range which is the current preferred taxane formulation in clinical practice and may have a safety advantage regarding decreased use of pretreatment corticosteroids.
Introduction
Paclitaxel is a widely used chemotherapeutic agent that plays a pivotal role in the treatment of patients with metastatic breast cancer (MBC) [1]. The first approved formulation (Taxol®; Bristol-Myers Squibb, Princeton, NJ) was prepared in nonionic surfactant polyoxyethylated castor oil; (Kolliphor EL®, formerly known as Cremophor® EL, BASF, Ludwigshafen, Germany) and ethanol to enhance drug solubility [2]. The polyoxyethylated castor oil adds to the toxic effects of paclitaxel by producing or contributing to hypersensitivity reactions that commonly occur during infusion, affecting 25–30 % of treated patients [3, 4]. Routine premedication with H1 blockers and H2 blockers, as well as corticosteroids, has become standard practice to minimize the incidence and severity of these sometimes fatal reactions [5]. In addition, plasticizers from polyvinyl chloride bags and infusion sets may leach as a result of the polyoxyethylated castor oil and ethanol solvent, necessitating preparation and administration of conventional paclitaxel in glass bottles or nonpolyvinyl chloride infusion systems and with in-line filtration [6].
With the advancement of nanotechnology applications in healthcare, newer nanoparticle strategies to address the shortcomings of solvent-based taxanes are under clinical evaluation, the first of which to be marketed is nab-paclitaxel (Abraxane®; Celgene Corporation, Summit, NJ). Nab-paclitaxel (an albumin-bound paclitaxel in nanometer range formulation) is approved for the treatment of patients with breast cancer who fail to respond to combination chemotherapy for metastatic disease or experience a relapse within 6 months of adjuvant chemotherapy [7]. Nab-paclitaxel, demonstrated a significant improvement in overall response rate and reduction in toxicities in patients with metastatic breast cancer in a pivotal Phase III clinical trial comparing efficacy of nab-paclitaxel to Taxol in patients with metastatic breast cancer (Study CA012-0) [8]. Routine premedication against hypersensitivity reactions was not required during clinical trials of nab-paclitaxel [9–12] and is not routinely required during its clinical use. Paclitaxel injection concentrate for nanodispersion (PICN; Sun Pharma Advanced Research Co. Ltd., Mumbai, India) is an alternative solvent-free formulation of paclitaxel. PICN is under investigation as a polyoxyethylated castor oil- and albumin-free self-assembly nanoparticle formulation of paclitaxel (100–150 nm) stabilized with a polymer (polyvinylpyrrolidone) and lipid (cholesteryl sulfate and caprylic acid) using Nanotecton® technology (Sun Pharma Advanced Research Co. Ltd.). Unlike, nab-paclitaxel, which utilizes albumin of biological origin, PICN makes use of polymer and lipid mixtures. While nab-paclitaxel continues to be the preferred taxane formulation used in clinic, newer formulations of paclitaxel such as PICN could have potential advantages which need to be evaluated in randomized trials. The current randomized trial aimed to understand the clinical similarities and dissimilarities between PICN and nab-paclitaxel and explore potential advantages offered by PICN due to the differences in the nanotechnology platforms used.
The doses for the current study were derived from the Phase I safety, efficacy, and pharmacokinetic study of Paclitaxel nano-dispersion injection in subjects with metastatic breast cancer. To arrive at a MTD, by adapting the 3 + 3 dose escalation design, the planned dose escalations were performed at 260, 295, and 325 mg/m2. At 260 mg/m2 one subject of the nine subjects enrolled had Cycle 1 DLT of grade 4 neutropenia while at the 295 mg/m2 dose, seven subjects were enrolled and treated, and no Cycle 1 DLTs were observed. These dose escalations resulted in an MTD of 325 mg/m2 for PICN. Since, both 260 and 295 mg/m2 doses were observed to be safe in every 3-week cycle in a limited study population of 16 subjects, they were selected in comparison with nab-paclitaxel for the study [13]. Additionally, the phase I study also demonstrated that PICN administration was free of hypersensitivity reactions despite a lack of premedication. The current comparative phase II/III trial hence was conducted to evaluate the efficacy and safety of 2 dosing regimens of PICN (260 and 295 mg/m2 every 3 weeks) compared with the approved dose of nab-paclitaxel (260 mg/m2 every 3 weeks) in women with MBC. Emphasis was also laid on ensuring that the PICN administration was without premedication to demonstrate negligible hypersensitivity risk associated with clinical use of PICN.
As per the emerging literature on taxanes, the optimal way to administer paclitaxel is in weekly setting and not every 3 weeks as demonstrated by clinical trials conducted using solvent-based taxanes such as Taxol [14]. Solvent-based paclitaxel is being used in a weekly dosing regimen [15]. However, the prescribing information of nab-paclitaxel does not support the weekly use of nab-paclitaxel. The weekly dose for nab-paclitaxel is under evaluation in several clinical trials [16]. Additionally, when evaluated in a randomized phase III trial of weekly paclitaxel (P) compared to weekly nanoparticle albumin-bound nab-paclitaxel (NP) or ixabepilone (Ix) with or without bevacizumab (B) as first-line therapy for locally recurrent or metastatic breast cancer (MBC), weekly nab-paclitaxel was associated with significantly higher Grade 2 + sensory neuropathy and Grade 3 + hematological toxicity (Grade 2 + sensory neuropathy was 48 % for nab-paclitaxel, 44 % for ixabepilone and 37 % for Paclitaxel; Grade 3 + hematologic toxicity was 49 % for nab-paclitaxel, 20 % for ixabepilone, and 12 % for paclitaxel and inferior hazard ratio [17]. Currently, there is lack of clinical literature on randomized clinical trial comparing efficacy and safety of weekly nab-paclitaxel with conventional solvent-based formulations of paclitaxel to support a dose and methodology for use of weekly nab-paclitaxel.
Therefore, the currently approved 3-weekly dosing regimen was selected (in this trial).
The weekly dose for PICN has also been determined in phase 1 trials in the US and India and could potentially be selected for further development and randomized clinical studies [18, 19].
Patients and methods
Patients
Women between age 18 and 70 years with measurable histologically or cytologically confirmed MBC were eligible to participate in this study if they were candidates for single-agent paclitaxel therapy in accordance with current standards of care. Inclusion criteria were as follows: Eastern Cooperative Oncology Group (ECOG) performance status score ≤2; life expectancy ≥12 weeks; prior use of chemotherapy as adjuvant therapy or for metastatic disease; use of chemotherapy (apart from palliative bisphosphonate therapy), major surgery, or radiotherapy >4 weeks before enrollment (6 weeks for mitomycin C or nitrosoureas) and free of any toxicity incurred as a result of such prior therapy; and prior hormonal therapy to be completed ≥2 weeks before enrollment. Organ and immune function had to be adequate, as indicated by the following laboratory test values obtained ≤2 weeks before dosing: absolute neutrophil count (ANC) ≥ 1500/µL, platelet count ≥100,000/µL, hemoglobin level ≥9.0 g/dL, serum creatinine level ≤ 2.0 mg/dL, total bilirubin level ≤1.5 mg/dL (or ≤2.0 mg/dL for liver metastasis), aspartate aminotransferase and alanine aminotransferase levels ≤2.5 times the upper limit of normal (or ≤5 times for liver metastasis), and alkaline phosphatase level ≤5 times the upper limit of normal (unless bone metastases are present in the absence of liver metastases). Women of childbearing potential were required to have a negative urine pregnancy test result and use an acceptable method of birth control as judged by the investigator from ≥2 weeks before study entry and throughout the study; otherwise, they had to be postmenopausal for ≥1 year or surgically sterile.
Exclusion criteria were as follows: relapse within 48 weeks after completion of adjuvant taxane therapy; any other malignancy in the previous 5 years except for nonmelanoma skin cancer, cervical intraepithelial neoplasia, or in situ cervical cancer; only evidence of metastasis as lytic or blastic bone lesions or pleural effusion or ascites; known hypersensitivity to study drugs or their excipients; treatment with any investigational agent within 30 days of study entry; clinically evident active central nervous system metastases, including leptomeningeal involvement, requiring corticosteroid or radiation therapy; pre-existing peripheral neuropathy grade ≥1; any severe concurrent disease that would make the patient inappropriate for study entry in the judgment of the investigator; prior taxane use for MBC; and the presence of pleural or ascitic fluid (if present, fluid was tapped before dosing).
Study design and treatment
This was a multicenter, open-label, parallel-group, randomized, comparative phase II/III study. Patients were screened and recruited at 20 sites in India. The study was conducted in compliance with the Declaration of Helsinki and International Conference on Harmonisation Good Clinical Practice Guidelines. All patients provided written informed consent. The protocol and its subsequent amendments were approved by the Drugs Controller General of India (DCGI) and the institutional review board at each of the participating centers. The trial was registered on Clinical Trials Registry-India (www.ctri.nic.in) on July 9, 2010, and the WHO Clinical Trial Registry on June 8, 2009 (CTRI number: CTRI/2010/091/001116).
An independent company using personnel otherwise unrelated to this study randomly assigned (using a computer-generated randomization code) patients to one of the following 3 treatment arms (1:1:1 ratio): PICN 260 mg/m2, PICN 295 mg/m2, or nab-paclitaxel 260 mg/m2 over the course of 30 min on day 1 of each 3-week cycle. Routine premedication to prevent hypersensitivity reactions with paclitaxel was not required. PICN and nab-paclitaxel concentrates were reconstituted for infusion in 5 % dextrose and 0.9 % saline, respectively. Treatment was continued until disease progression, occurrence of unacceptable toxicity, or withdrawal of patient consent. Patients were also discontinued from the study dependent on investigator discretion, loss to follow-up, noncompliance, death, or complete response.
Dose adjustments for nab-paclitaxel were made in accordance with the authorized package insert. For severe neutropenia (absolute neutrophil count [ANC] < 500/µL for ≥1 week) or severe sensory neuropathy, the dosage of nab-paclitaxel was reduced to 220 mg/m2 for subsequent courses. For recurrence of severe neutropenia or severe sensory neuropathy, there was an additional dose reduction to 180 mg/m2. For grade 3 sensory neuropathy, treatment was held until resolution to grade 1 or 2, followed by a dose reduction for all subsequent courses.
For PICN, a maximum of 2 dose reductions were allowed: (1) 295–260 and 220 mg/m2; and (2) 260–220 and 175 mg/m2. The patient was withdrawn from the study if more than 2 dose reductions were required. No action was to be taken for the first incidence of ANC < 500/µL without fever, but dose reduction was instituted for recurrence or for the first instance of neutropenic fever/sepsis. For subsequent cycles, the dose was maintained if granulocyte colony-stimulating factor was given as secondary prophylaxis or reduced in the absence of growth factor therapy. Dose reduction was required for grade 3/4 thrombocytopenia. Dosing was not resumed until the ANC was ≥1500/µL and the platelet count was ≥100,000/µL. For any nonhematologic toxicity grade ≥2, dose delay was permitted. Dose delay was required for neurotoxicity grade ≥2. For any grade 3/4 nonhematologic toxicity, dose reduction was required. A maximum of 2 dose reductions were permitted. In the event of any other toxicity that was grade ≥2 (excluding alopecia), which in the investigator’s opinion was probably or definitely related to PICN, a dose delay was permitted.
Patient evaluation
Overall response rate (ORR), defined as the percentage of patients who achieved complete or partial response for target and nontarget lesions according to RECIST version 1.1, was determined every 2 cycles after a minimum of 2 cycles of therapy in the intention-to-treat (ITT) population assessed by imaging (computed tomography or magnetic resonance imaging). An independent analysis of radiologic data using RECIST version 1.1 was performed for evaluable patients by a group of radiologists who were blind to treatment and unrelated to the trial. Radiologic data for 136 patients (48, 41, and 47 in the PICN 260-mg/m2, PICN 295-mg/m2, and nab-paclitaxel 260-mg/m2 arms, respectively) underwent independent radiologic assessment. Progression-free survival (PFS) was a secondary efficacy measure.
Safety was assessed by adverse events (AEs) using Common Terminology Criteria for Adverse Events version 4.02. Adverse events were classified with respect to relationship to treatment (unrelated, unlikely, possibly, probably) and intensity, and were derived from changes in vital signs and laboratory parameters, as well as by indirect unbiased questioning, spontaneous patient reports, and observation.
Statistical analysis
This study was designed to allow for direct comparisons of ORR between the 3 treatment arms. The underlying assumptions for the sample size calculation were based on an ITT population with an ORR of 21.51 % for the nab-paclitaxel group and an ORR of 16.5 % for the PICN group at the end of 6 cycles. Forty-five subjects per treatment arm were required to yield at least 80 % power at an α level of 0.05 to conclude that the ORR of PICN was within 14 % of the ORR of nab-paclitaxel (1-sided). Taking into account a dropout rate of approximately 25 %, the projected sample size required was 180 (60 patients per study arm). These assumptions were based on the reconciled target lesion response rate in the randomized Phase III study comparing efficacy of nab-paclitaxel to Taxol in patients with metastatic breast cancer which led to regulatory approval of nab-paclitaxel (Study CA012-0). The reconciled target lesion response rate observed in the Phase III nab-paclitaxel study was 21.5 % [8].
All statistical analyses were performed using SAS version 9.2 software (SAS Institute Inc., Cary, NC). Comparison of baseline demographic and clinical variables was performed using a Chi-square test for categorical variables, Mann–Whitney U test for ordinal variables, and student t test for interval variables. All tests were 2-tailed, and the level of significance was set at .05. Compliance was measured as the percentage of scheduled doses administered and was compared between groups using student t test. ORRs were compared using the Chi-square test. Progression-free survival was measured using Kaplan–Meier analysis and compared using the log-rank test.
Results
Patient characteristics
From July 2010 to April 2013, 233 patients were screened; 180 were randomized to treatment and comprised the intent to treat (ITT)/safety population (Fig. 1). There were no statistically significant differences across the treatment arms with respect to baseline demographic and clinical characteristics (Table 1). Patient disposition and reasons for treatment discontinuations are detailed in the CONSORT diagram (Fig. 1). The proportion of patients who discontinued treatment for specific reasons was similar across the treatment arms, including the proportion who discontinued because of disease progression (n = 13 [27 %] in the PICN 260-mg/m2 arm; n = 18 [31 %] in the PICN 295-mg/m2 arm; n = 20 [34 %] in the nab-paclitaxel 260-mg/m2 arm).
Fig. 1.
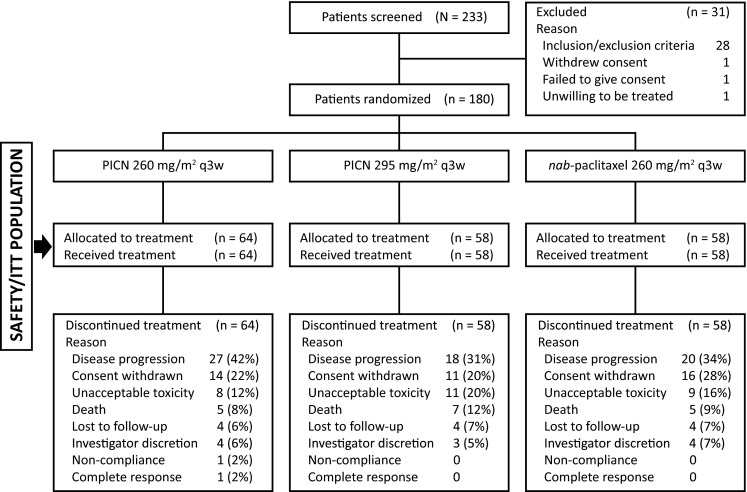
CONSORT diagram of the participants. ITT intent to treat, PICN paclitaxel injection concentrate for nanodispersion; q3w every 3 weeks
Table 1.
Patient baseline demographic and clinical characteristics
| Characteristica | PICN 260 mg/m2 (n = 64) | PICN 295 mg/m2 (n = 58) | nab-paclitaxel 260 mg/m2 (n = 58) | |||
|---|---|---|---|---|---|---|
| No. of patients (%) | No. of patients (%) | No. of patients (%) | ||||
| Age (years) | ||||||
| Median | 50 | 49 | 51 | |||
| Range | 32–68 | 27–70 | 35–69 | |||
| Race | ||||||
| Asian | 64 | 100 | 58 | 100 | 58 | 100 |
| Weight (kg) | ||||||
| Median | 54 | 55 | 56 | |||
| Range | 33–84 | 33–110 | 34–90 | |||
| Height (cm) | ||||||
| Median | 151 | 152 | 153 | |||
| Range | 138–164 | 140–161 | 136–182 | |||
| Menopausal status | ||||||
| Postmenopausal | 50 | 78 | 44 | 76 | 45 | 78 |
| Premenopausal | 14 | 22 | 14 | 24 | 13 | 22 |
| ECOG PSa | ||||||
| 0 | 28 | 44 | 26 | 45 | 31 | 53 |
| 1 | 34 | 53 | 31 | 53 | 25 | 43 |
| 2 | 2 | 3 | 1 | 2 | 2 | 3 |
| Prior breast cancer therapy | ||||||
| Chemotherapy | 63 | 98 | 46 | 79 | 55 | 95 |
| Radiotherapy | 18 | 28 | 19 | 33 | 11 | 19 |
| Surgery | 51 | 80 | 46 | 79 | 42 | 72 |
| No. of prior chemotherapy regimens | ||||||
| 0 | 5 | 8 | 14 | 24 | 8 | 14 |
| 1 | 43 | 67 | 27 | 47 | 35 | 60 |
| 2 | 7 | 11 | 10 | 17 | 8 | 14 |
| ≥3 | 9 | 14 | 7 | 12 | 7 | 12 |
| No. of lesionsb | ||||||
| Median | 5 | 5 | 4.5 | |||
| Range | 2–9 | 2–12 | 2–13 | |||
| Dominant metastatic site | ||||||
| Liver | 19 | 30 | 16 | 28 | 21 | 36 |
| Lung | 19 | 30 | 14 | 24 | 18 | 31 |
| Bone | 9 | 14 | 7 | 12 | 12 | 21 |
| CNS | 0 | 0 | 0 | 0 | 1 | 2 |
| Other | 39 | 61 | 38 | 66 | 34 | 59 |
ECOG Eastern Cooperative Oncology Group, CNS central nervous system, PICN paclitaxel injection concentrate for nanodispersion, PS performance status
aDescriptive statistics performed to provide evidence that the groups were balanced with no statistically significant between groups (p > 0.1)
bPercentages may not total 100 because of rounding
cIncludes target and nontarget lesions
The mean (±standard deviation [SD]) cumulative doses administered during the study were 2026 ± 1391 mg/m2 in the PICN 260-mg/m2 arm, 2260 ± 1823 mg/m2 in the PICN 295-mg/m2 arm, and 2290 ± 1293 mg/m2 in the nab-paclitaxel 260-mg/m2 arm. Mean dose intensities were 155 ± 88 mg/m2, 186 ± 126 mg/m2, and 137 ± 61 mg/m2, respectively. The mean number of cycles administered per patient was 5.2 ± 3.5 in the PICN 260-mg/m2 arm, 5.07 ± 3.7 in the PICN 295-mg/m2 arm, and 5.9 ± 3.5 in the nab-paclitaxel 260-mg/m2 arm. Treatment was administered at the specified dosage without dose reduction in 92 % (n = 59), 86 % (n = 50), and 88 % (n = 51) of patients in the PICN 260-mg/m2, PICN 295-mg/m2, and nab-paclitaxel 260-mg/m2 arms, respectively.
Efficacy
The independent radiologist-assessed ORRs in the evaluable population were 35, 49, and 43 % in the PICN 260-mg/m2, PICN 295-mg/m2, and nab-paclitaxel 260-mg/m2 arms, respectively, which revealed no significant difference when comparing the PICN 260-mg/m2 arm (p = 0.7613) or the PICN 295-mg/m2 arm (p = 0.6233) with the nab-paclitaxel 260-mg/m2 arm (Table 2).
Table 2.
Independent radiologist-assessed response rates (evaluable population)
| PICN 260 mg/m2 (n = 48) | PICN 295 mg/m2 (n = 41) | nab-paclitaxel 260 mg/m2 (n = 47) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| No. of patients | (%) | 95 % CI (%) | No. of patients | (%) | 95 % CI (%) | No. of patients | (%)a | 95 % CI (%) | |
| ORR (CR + PR) | 17 | 35b | 22.2–50.5 | 20 | 49c | 32.9–64.9 | 20 | 43 | 36.6–63.4 |
| SD | 18 | 38 | 14 | 34 | 15 | 32 | |||
| PD | 13 | 27 | 7 | 17 | 12 | 26 | |||
CI confidence interval, CR complete response, ORR overall response rate, PICN paclitaxel injection concentrate for nanodispersion, PD progressive disease, PR partial response, SD stable disease
aPercentages do not total 100 because of rounding
b p = 0.7613 versus nab-paclitaxel
c p = 0.6233 versus nab-paclitaxel
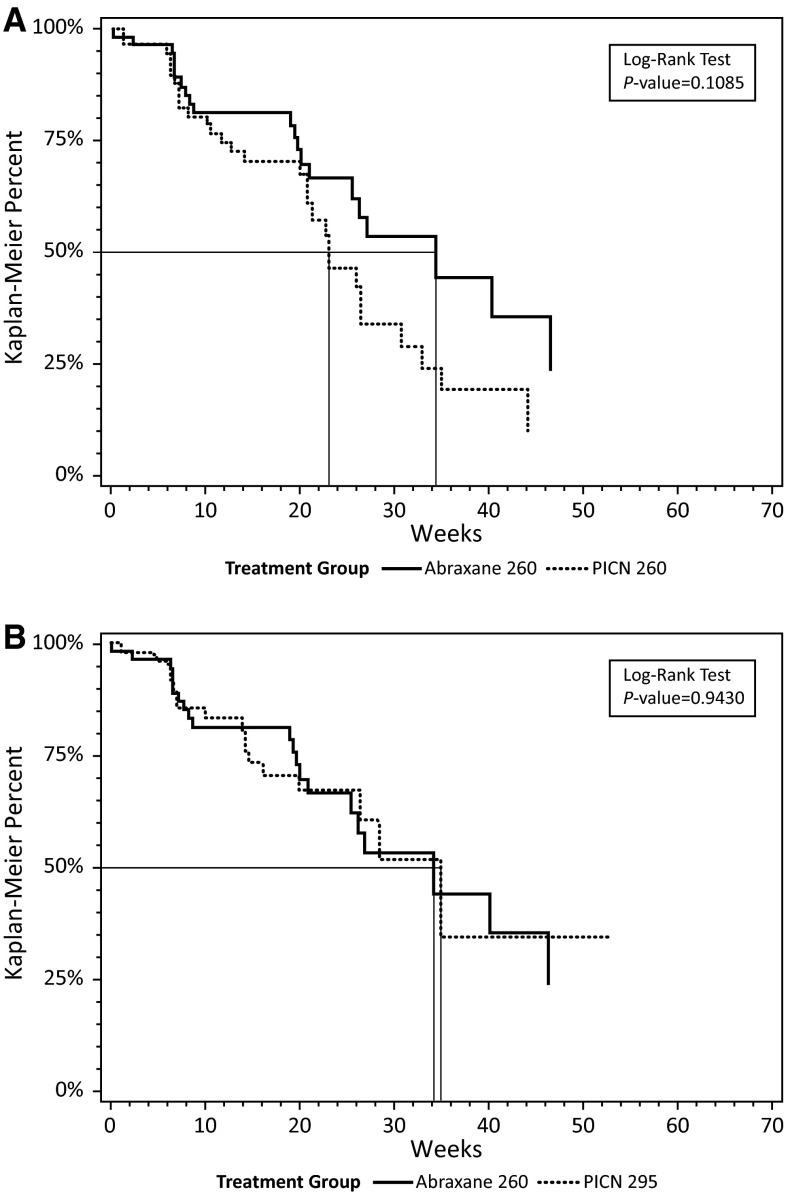
Median PFS was 23 weeks [95 % confidence interval (CI) 21–21 weeks], 35 weeks (95 % CI 27 to not reached weeks), and 34 weeks (95 % CI 25 to not reached weeks) in the PICN 260-mg/m2, PICN 295-mg/m2, and nab-paclitaxel 260-mg/m2 arms, respectively (Fig. 2). There was no significant difference in PFS between the PICN 260-mg/m2 (p = 0.1085) or PICN 295-mg/m2 (p = 0.9430) arms compared with the nab-paclitaxel 260-mg/m2 arm.
Fig. 2.
Kaplan–Meier plots of progression-free survival comparing a PICN 260 mg/m2 and nab-paclitaxel 260 mg/m2 and b PICN 295 mg/m2 and nab-paclitaxel 260 mg/m2. PICN paclitaxel injection concentrate for nanodispersion
Safety
The most common AEs of any grade and grade 3/4 per patient irrespective of treatment relationship across all cycles are summarized in Table 3. Adverse events of any grade were generally reported in similar proportions of patients across the treatment arms. Grade 3/4 AEs were reported in a lower proportion of patients in the PICN 260-mg/m2 arm compared with those in the PICN 295-mg/m2 and nab-paclitaxel 260-mg/m2 arms, with a similar prevalence in the latter 2 arms: neutropenia (12 vs. 24 vs. 21 %); peripheral neuropathy (8 vs. 21 vs. 17 %); and leukopenia (9 vs. 14 vs. 16 %), respectively.
Table 3.
Most common adverse events over all cycles
| PICN 260 mg/m2 (n = 64) | PICN 295 mg/m2 (n = 58) | nab-paclitaxel 260 mg/m2 (n = 58) | ||||
|---|---|---|---|---|---|---|
| No. of patients | (%) | No. of patients | (%) | No. of patients | (%) | |
| Any grade AE occurring in ≥20 % of patients in any arm, by preferred terma | ||||||
| Pain | 36 | 56 | 34 | 59 | 39 | 67 |
| Peripheral neuropathy | 37 | 58 | 37 | 64 | 35 | 60 |
| Alopecia | 24 | 37 | 21 | 36 | 30 | 52 |
| Mucosal inflammation | 26 | 41 | 25 | 43 | 23 | 40 |
| Asthenia | 24 | 37 | 24 | 42 | 21 | 36 |
| Nausea | 14 | 22 | 16 | 28 | 21 | 36 |
| Pyrexia | 19 | 30 | 20 | 34 | 20 | 34 |
| Neutropenia | 21 | 33 | 24 | 41 | 19 | 33 |
| Leukopenia | 19 | 30 | 18 | 31 | 16 | 28 |
| Cough | 14 | 22 | 15 | 26 | 13 | 22 |
| Infection | 13 | 20 | 11 | 19 | 15 | 26 |
| Vomiting | 16 | 25 | 8 | 14 | 9 | 16 |
| Diarrhea | 16 | 25 | 9 | 16 | 8 | 14 |
| Anemia | 9 | 14 | 14 | 24 | 9 | 16 |
| Anorexia | 10 | 16 | 13 | 22 | 13 | 22 |
| Pruritus | 13 | 20 | 12 | 21 | 9 | 16 |
| Grade 3/4 AE occurring in ≥5 % of patients in any arm, by preferred terma | ||||||
| Neutropenia | 8 | 12 | 14 | 24 | 12 | 21 |
| Peripheral neuropathy | 5 | 8 | 12 | 21 | 10 | 17 |
| Leukopenia | 6 | 9 | 8 | 14 | 9 | 16 |
| Anemia | 1 | 2 | 5 | 9 | 2 | 3 |
| Febrile neutropenia | 1 | 2 | 4 | 7 | 2 | 3 |
| Pain | 2 | 3 | 3 | 5 | 4 | 7 |
| Asthenia | 3 | 5 | 3 | 5 | 4 | 7 |
| Infection | 2 | 3 | 3 | 5 | 3 | 5 |
AE adverse event, PICN paclitaxel injection concentrate for nanodispersion
aCoded by MedDRA version 14.0
There were 46, 53, and 28 serious AEs irrespective of treatment relationship reported for all cycles in the PICN 260-mg/m2, PICN 295-mg/m2, and nab-paclitaxel 260-mg/m2 arms, respectively. The most frequently (≥5 % in any arm) reported serious AEs were diarrhea (13 vs. 2 vs. 7 %); infection (9 vs. 6 vs. 11 %); mucosal inflammation (9 vs. 8 vs. 7 %); neutropenia (7 vs. 9 vs. 7 %); pyrexia (9 vs. 2 vs. 4 %); thrombocytopenia (0 vs. 9 vs. 4 %); death (8 vs. 12 vs. 9 %); febrile neutropenia (2 vs. 6 vs. 7 %); cardiac arrest (2 vs. 4 vs. 7 %); nausea (2 vs. 2 vs. 7 %); and leukopenia (2 vs. 6 vs. 4 %).
Unacceptable toxicity resulting in treatment discontinuation occurred in 8 (12 %), 11 (20 %), and 9 (16 %) patients in the PICN 260-mg/m2, PICN 295-mg/m2, and nab-paclitaxel 260-mg/m2 arms, respectively, and death occurred in 5 (8 %), 7 (12 %), and 5 (9 %) patients, respectively.
Discussion
Careful consideration was given to selecting the comparative dosages in this phase II/III trial. The PICN 295-mg/m2 dosage was the maximum tolerated dose in a previously performed phase I study in women with MBC. Since the PICN 295-mg/m2 dosage was obtained from the phase I study with a limited sample size, additionally 260 mg/m2 was selected as the comparator against the approved and indicated dosage of nab-paclitaxel 260 mg/m2 for MBC because it was the next lower dosage step [13].
There were no statistically significant differences between the treatment arms with respect to independent radiologist-assessed ORR in the evaluable population (Table 2). The median PFS was somewhat lower in the PICN 260-mg/m2 arm, after 23 weeks, in comparison to that which was reported for nab-paclitaxel 260 mg/m2 at 34 weeks. It should be noted, however, that this difference was statistically insignificant, and therefore may not be interpreted to have a clinical impact. The median PFS in the PICN 295-mg/m2 arm at 35 weeks was remarkably similar to the PFS observed in the nab-paclitaxel 260-mg/m2 arm at 34 weeks. There was no statistically significant difference between treatment arms. The proportion of patients who discontinued treatment because of disease progression was similar across the study arms, the PICN 260-mg/m2 arm (n = 13 [27 %]), the nab-paclitaxel 260-mg/m2 arm (n = 20 [34 %]), and the PICN 295-mg/m2 arm (n = 18 [31 %]).
The safety profiles when comparing PICN 295 mg/m2 with nab-paclitaxel 260 mg/m2 were similar, whereas the PICN 260-mg/m2 dosage appeared to be somewhat better tolerated than the nab-paclitaxel 260-mg/m2 and PICN 295-mg/m2 dosages. For example, the incidence of each of the most frequent grade 3/4 AEs (neutropenia, peripheral neuropathy, and leukopenia) was lowest in the PICN 260-mg/m2 arm, and similar between PICN 295 mg/m2 and nab-paclitaxel 260 mg/m2 (Table 3). Historically, chemotherapy-induced neutropenia is the most common toxicity associated with the administration of anticancer agents [20, 21]. In fact, the risk of developing neutropenia is >20 % for those patients with MBC exposed to dose-dense anthracycline/taxane- and docetaxel-based regimens [22]. Head-to-head studies of patients with MBC randomized to polyoxyethylated castor oil-paclitaxel (175 mg/m2 every 3 weeks), docetaxel (100 mg/m2 every 3 weeks), and nab-paclitaxel (260 mg/m2 to 300 mg/m2 every 3 weeks) have been performed. They demonstrated rates of grade 3/4 neutropenia ranging from 46 to 54.5 % for polyoxyethylated castor oil-paclitaxel (N = 444), 92 to 93.3 % for docetaxel (N = 296), and 31–43 % for nab-paclitaxel (N = 302) [23]. These rates of grade 3/4 neutropenia are in sharp contrast to those observed in the present study, where rates were reported to be 33 % for patients in the PICN 260-mg/m2 arm, and 41 and 33 % for those patients in the PICN 295-mg/m2 and nab-paclitaxel 260-mg/m2 arms, respectively. The safety results in the current study were also reflected in the rates of discontinuation for unacceptable toxicity in the respective arms.
In addition, the initial hypothesis, of a decreased incidence of hypersensitivity reactions due to the presence of polyoxyethylated castor oil and albumin in the comparator, was substantiated by the highly limited number of hypersensitivity reactions reported with PICN (3.13 % for PICN 260 mg/m2, 0.0 % for PICN 295 mg/m2, and 1.72 % for nab-paclitaxel). Incidence of hypersensitivity reactions reported for polyoxyethylated castor oil-containing paclitaxel formulations is between 25 and 30 % [3]. Reported grade 3/4 neuropathies were also limited with both dosages of PICN, and comparable to those reported with the comparator, nab-paclitaxel. The clinical observations of this study also indicate that despite chemical dissimilarities and differences between the nanotechnology platforms used for the studied taxane formulations, PICN has similar efficacy and safety to nab-paclitaxel as demonstrated in this trial in patients with metastatic breast cancer. Similar to nab-paclitaxel, PICN administration did not require corticosteroid pretreatment and was well tolerated.
In conclusion, PICN 295 mg/m2 and PICN 260 mg/m2 every 3 weeks was as effective and showed similar tolerability compared with nab-paclitaxel 260 mg/m2 every 3 weeks in the treatment of women with MBC. The current study showed that additive-free PICN, when used in women with refractory MBC, is as effective and well tolerated as additive-containing formulations of paclitaxel (i.e., nab-paclitaxel), and may have potential advantage of decreased use of pretreatment corticosteroids.
Acknowledgments
Editorial assistance was provided by James A. Shiffer, RPh, Write On Time Medical Communications, LLC, and was supported by Sun Pharma Advanced Research Co. Ltd.
Funding
This study was funded by Sun Pharma Advanced Research Co. Ltd.
Compliance with ethical standards
Disclosures
Drs. Ajay Khopade, Shravanti Bhowmik, and Geetanjali Chimote are employed by Sun Pharma Advanced Research Co. Ltd and associated with this study. Dr. Khopade owns stock in Sun Pharma Advanced Research Co. Ltd. Authors Minish M. Jain, Shekhar G. Patil, Anand B. Pathak, Chetan D. Deshmukh, Niraj Bhatt, K. Govind Babu, Chiramana Haritha, Shailesh A. Bondarde, Raghunadharao Digumarti, Jyoti Bajpai, Ravi Kumar, Smita U. Gupte, Ashish V. Bakshi, Gouri Sankar Bhattacharyya, Poonam Patil, Sundaram Subramanian, Ashok K. Vaid, Chirag J. Desai, and Poonamalle P. Bapsy received research funding from Sun Pharma Advanced Research Co. Ltd. Poonamalle P. Bapsy is employed by Sun Pharma Advanced Research Co. Ltd.
References
- 1.Gradishar WJ. Taxanes for the treatment of metastatic breast cancer. Breast Cancer (Auckl) 2012;6:159–171. doi: 10.4137/BCBCR.S8205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Taxol® (paclitaxel) Injection [prescribing information]. Princeton, NJ: Bristol-Myers Squibb Co.; 2011
- 3.Rowinsky EK, Donehower RC. Paclitaxel (taxol) N Engl J Med. 1995;332:1004–1014. doi: 10.1056/NEJM199504133321507. [DOI] [PubMed] [Google Scholar]
- 4.Weiss RB, Donehower RC, Wiernik PH, et al. Hypersensitivity reactions from Taxol. J Clin Oncol. 1990;8:1263–1268. doi: 10.1200/JCO.1990.8.7.1263. [DOI] [PubMed] [Google Scholar]
- 5.Kloover JS, den Bakker MA, Gelderblom H, van Meerbeeck JP. Fatal outcome of a hypersensitivity reaction to paclitaxel: a critical review of premedication regimens. Br J Cancer. 2004;90:304–305. doi: 10.1038/sj.bjc.6601303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Waugh WN, Trissel LA, Stella VJ. Stability, compatibility, and plasticizer extraction of taxol (NSC-125973) injection diluted in infusion solutions and stored in various containers. Am J Hosp Pharm. 1991;48:1520–1524. [PubMed] [Google Scholar]
- 7.Abraxane® for Injectable Suspension (paclitaxel protein-bound particles for injectable suspension) (albumin bound) [prescribing information]. Summit, NJ: Abraxis BioScience, LLC; Oct 2013
- 8.NDA-21660, Abraxane, Medical Review (S), Centre for Drug Evaluation and Research; 2005
- 9.Ibrahim NK, Desai N, Legha S, et al. Phase I and pharmacokinetic study of ABI-007, a Cremophor-free, protein-stabilized, nanoparticle formulation of paclitaxel. Clin Cancer Res. 2002;8:1038–1044. [PubMed] [Google Scholar]
- 10.Gradishar WJ, Krasnojon D, Cheporov S, et al. Significantly longer progression-free survival with nab-paclitaxel compared with docetaxel as first-line therapy for metastatic breast cancer. J Clin Oncol. 2009;27:3611–3619. doi: 10.1200/JCO.2008.18.5397. [DOI] [PubMed] [Google Scholar]
- 11.Ibrahim NK, Samuels B, Page R, et al. Multicenter phase II trial of ABI-007, an albumin-bound paclitaxel, in women with metastatic breast cancer. J Clin Oncol. 2005;23:6019–6026. doi: 10.1200/JCO.2005.11.013. [DOI] [PubMed] [Google Scholar]
- 12.Gradishar WJ, Tjulandin S, Davidson N, et al. Phase III trial of nanoparticle albumin-bound paclitaxel compared with polyethylated castor oil-based paclitaxel in women with breast cancer. J Clin Oncol. 2005;23:7794–7803. doi: 10.1200/JCO.2005.04.937. [DOI] [PubMed] [Google Scholar]
- 13.Jain MM, Deshmukh CD, Bhatt NN, et al. (2011) Phase I, PK, dose-finding, active controlled study of paclitaxel injection concentrate for nanodispersion (PICN) in subjects with metastatic breast cancer. J Clin Oncol, 29: (suppl; abstr e11585)
- 14.Lombardi D, Crivellari D, et al. Long term, Weekly one hour infusion of paclitaxel in patients with metastatic breast cancer: a Phase II monoinstitutional study. Tumori. 2004;19:285–288. doi: 10.1177/030089160409000304. [DOI] [PubMed] [Google Scholar]
- 15.Eniu A, Palmieri FM, et al. Weekly administration of docetaxel and paclitaxel in metastatic or advanced breast cancer. Oncologist. 2005;10:665–685. doi: 10.1634/theoncologist.10-9-665. [DOI] [PubMed] [Google Scholar]
- 16.Blum JL, Savin MA, et al. Phase II study of weekly albumin-bound paclitaxel for patients with metastatic breast cancer heavily pretreated with taxanes. Clin Breast Cancer. 2007;7:850–856. doi: 10.3816/CBC.2007.n.049. [DOI] [PubMed] [Google Scholar]
- 17.Rugo HS, Barry WT, et al. (2012) CALGB 40502/NCCTG N063H: randomized phase III trial of weekly paclitaxel (P) compared to weekly nanoparticle albumin bound nab-paclitaxel (NP) or ixabepilone (Ix) with or without bevacizsumab (B) as first-line therapy for locally recurrent or metastatic breast cancer (MBC). J Clin Oncol, 30 (suppl; abstr CRA1002) [DOI] [PMC free article] [PubMed]
- 18.Jain MM, Patil S, et al. (2014) The efficacy and safety of paclitaxel injection concentrate for nano-dispersion (PICN) at two different doses versus paclitaxel albumin-stabilized nanoparticle formulation in subjects with metastatic breast cancer (MBC). J Clin Oncol, 32: (suppl; abstr 1069)
- 19.Ma WW, Diamond JR (2014) A phase I and pharmacokinetic study of a weekly dosing schedule of paclitaxel injection concentrate for nano-dispersion (PICN) in patients with advanced solid tumors. J Clin Oncol, 32:(suppl; abstr 2566)
- 20.Crawford J, Wolff DA, Culakova E, et al. First cycle risk of severe and febrile neutropenia in cancer patients receiving systemic chemotherapy: results from a prospective nationwide study. Blood. 2004;104:607a–608a. doi: 10.1182/blood-2004-03-0880. [DOI] [PubMed] [Google Scholar]
- 21.Culakova E, Thota R, Poniewierski MS, et al. Patterns of chemotherapy-associated toxicity and supportive care in US oncology practice: a nationwide prospective cohort study. Cancer Med. 2014;3:434–444. doi: 10.1002/cam4.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.National Comprehensive Cancer Network. NCCN guidelines. Myeloid growth factors. www.nccn.org/professionals/physician_gls/pdf/myeloid_growth.pdf. Accessed 6 Oct 2015
- 23.Gradishar WJ. Taxanes for the treatment of metastatic breast cancer. Breast Cancer (Auckl) 2012;6:159–171. doi: 10.4137/BCBCR.S8205. [DOI] [PMC free article] [PubMed] [Google Scholar]