Abstract
The aim of this study was to investigate the effects of sevoflurane on skeletal muscle contractility. In the first part, twenty-two American Society of Anesthesiology (ASA I-II) female adult patients undergoing elective hysterectomy surgery inhaled sevoflurane 1.0, 1.5 and 2.0 minimum alveolar concentrations (MAC) in succession. Neuromuscular function was assessed at each dose. In the second part, forty-four ASA I-II female adult patients were randomized into four groups: group 1 (propofol + atracurium, sevoflurane 0 MAC), and groups 2 to 4 (atracurium + sevoflurane 1.0, 1.5 and 2.0 MAC, respectively). In group 1, patients were anesthetized by propofol. Then 0.01 mg/kg atracurium was injected into the tested arm intravenously after the arterial blood flow was blocked using a tourniquet. For the other 3 groups, patients inhaled 1.0 MAC, 1.5 MAC, or 2.0 MAC of sevoflurane. Then 0.01 mg/kg atracurium was injected. Neuromuscular function was recorded for the 4 groups. Neuromuscular function was assessed by acceleromyography measurement of evoked responses to train-of four (TOF) stimuli (2 Hz for 2 s applied every 12 s) at the adductor pollicis using a TOF-GuardTM neuromuscular transmission monitor. Amplitudes of first response (T1) in each TOF sequence and the ratios of fourth TOF response (T4) to the first were similar at 1.0 MAC, 1.5 MAC, and 2.0 MAC sevoflurane. Compared to baseline, there was no significant change in the TOF value after inhaling 1.0 MAC, 1.5 MAC, or 2.0 MAC sevoflurane. Compared to group 1, there was no significant difference in atracurium onset time (time to reach TOF ratio = 0.25) in group 2 ( 5.6 ± 1.8 min vs. 6.5 ± 1.7 min, P>0.05), or degree of adductor pollicis block (subject number with TOF ratio = 0, 5 vs. 2 subjects, p = 0.3). However, inhaling 1.5 or 2.0 MAC sevoflurane decreased atracurium onset time (4.6 ± 1.5 min and 4.0 ± 1.3 min vs. 6.5 ± 1.7 min, P<0.01 and P<0.001, respectively), and enhanced the block degree (9 and 10 vs. 2 subjects, P<0.001) compared with group 1. Sevoflurane has no direct effects on the adductor pollicis contractility, but increased the skeletal muscle sensitivity to atracurium.
Keywords: Sevoflurane, neuromuscular block, inhaled anesthesia, atracurium, propofol
Introduction
Inhaled anesthetics can induce a variety of reversible, clinically important effects including amnesia, hypnosis, immobility (response to noxious stimuli) and muscle relaxation. Potent inhaled anesthetics increase the neuromuscular blockade produced by non-depolarizing drugs in a dose-dependent fashion [1-3] as demonstrated by previous studies showing that effects of neuromuscular blockade on train-of four (TOF) values are amplified by inhaled anesthetics [4-6]. Enhancing the action of non-depolarizing neuromuscular blocking drugs decreases the need for muscle relaxants [7-11]. However, the specific sites of action of inhaled anesthetics such as sevoflurane on neuromuscular blocking are not clear, although some believe the spinal cord maybe one of the sites of action [12-16]. But whether sevoflurane has a direct effect on skeletal muscle contractility is unknown. In this study, we aimed to examine the effects of sevoflurane on skeletal muscle contractility by selectively delivering neuromuscular blocking drugs to the skeletal muscle without affecting in the central nervous system.
Materials and methods
Patients
This study was approved by the Institutional Research Ethics Committee of West China Second University Hospital, Sichuan University, China, and written informed consent was obtained from each patient preoperatively. A total of sixty-six un-premedicated female adult patients, America Society of Anesthesiology (ASA) status I and II scheduled for elective gynecological surgery were enrolled in the study. Body weight was within 20% of the normal value for the height, and the age range was 18-65 years. Exclusion criteria included liver or renal insufficiency, abnormal plasma electrolytes, obesity, peripheral vessel or neuromuscular disease, allergy to atracurium or propofol, and concomitant medication known to interfere with neuromuscular transmission.
Upon arrival in the operating room, standard monitoring including electrocardiograph, pulse oximeter, capnograph and noninvasive blood pressure was applied to the patients. Prior to anesthesia, patients were administered midazolam (<0.05 mg.kg) intravenously followed by oxygen at 6 liters min-1 via a mask for 3 minutes. All the tests were done by one skillful attending anesthesiologist before the surgery.
Part 1: Administration of sevoflurane alone under varying concentrations
Twenty-two patients were enrolled in this part of study. The recirculating system of the anesthesia machine was primed for 30 s with sevoflurane in oxygen 6 liters min-1. The face mask was fitted and the patients were asked to take deep breaths. End-tidal sevoflurane concentration was monitored continuously with an anesthetic gas monitor (Spacelabs Medical, Issaquah, WA, USA). Each patient was examined during three different experimental states. Neuromuscular function was measured at sevoflurane concentrations of 1.0 MAC, 1.5 MAC and 2.0 MAC with O2. The lowest concentration was administered first, and highest was administered last.
Part 2: Administration of sevoflurane or propofol with neuromuscular blocker
Forty-four patients were randomly assigned into four groups with 11 subjects each: group 1: propofol + atracurium (sevoflurane 0 MAC); groups 2 to 4: atracurium + sevoflurane 1.0 MAC, 1.5 MAC and 2.0 MAC, respectively. In group 1, general anesthesia was induced by bolus injection of propofol 2-3 mg·kg-1 and followed by continuous intravenous propofol 8-10 mg·kg-1·h-1 during the anesthesia period as measured in the non-tested arm. After loss of consciousness and stabilization of the concentration, 0.01 mg/kg atracurium (in normal saline diluted to 10 ml) was injected to the tested arm intravenously after the arterial blood flow was blocked by tourniquet (i.e., the same procedure as is used for intravenous regional anesthesia (IVRA)), and then the neuromuscular function was tested.
In groups 2-4, patients inhaled 1.0 MAC, 1.5 MAC, or 2.0 MAC sevoflurane, respectively for 5 min. After loss of consciousness and stabilization of the concentration, the arterial blood flow in the tested arms was blocked using a tourniquet and 0.01 mg/kg atracurium (in normal saline diluted to 10 ml) was injected to the same arm intravenously, and then the neuromuscular function was recorded.
In all the groups, loss of consciousness was defined as loss of the eyelash reflex and lack of response to verbal stimulation. If undesirable respiratory depression occurred, a laryngeal mask airway was applied to maintain the partial pressure of end-tidal carbon dioxide between 35-40 mmHg. Time for tourniquet was less than 30 minutes.
Measurement of neuromuscular blockade
Neuromuscular function was assessed by the acceleromyography measurement of evoked responses to train-of four (TOF) stimuli (2 Hz for 2 s applied every 12 s) at the adductor pollicis using a TOF-GuardTM neuromuscular transmission monitor (Organon Technica, Biometer, Turnhout, Belgium) according to the recommendations of Vibymogensen et al. [17]. We recorded the amplitude of the first response (T1) in each TOF sequence, and calculated the ratio of the amplitude of forth TOF response in each train to that of the first (TOF ratio). A baseline was established during the calibration sequence prior to the administration of either the initial atracurium bolus or the volatile anesthetic agent. Two peripheral nerve stimulators which were used for stimulation of the ulnar nerves via cutaneous electrodes were applied at the wrists. The device was calibrated before administration of atracurium. All procedures were performed by the attending anesthesiologist.
All measurements were performed 15-20 min after obtaining a stable level of each end-tidal sevoflurane concentration in 100% O2. All measurements were recorded in duplicate for each patient.
Statistics
Data was analyzed with SPSS Version 13.0 (SPSS Inc., Chicago, IL). For part 1, values of each neuromuscular variable at different concentrations of sevoflurane were compared by repeated measures analysis of variance (ANOVA). For part 2, demographic data and results obtained for each subject in the experiment were compared by ANOVA. Differences in maximum blockade (number with TOF = 0) between group 1 and groups 2-4 were compared by Fisher’s exact test. All tests were two-sided, with p<0.05 considered significant. Levels of significance are indicated by the number of symbols, e.g., *P = .01 to <.05; **P = .001 to .01; ***P<.001. Data are presented as average ± SD.
Results
All groups did not differ significantly with regard to age, height or weight and blood pressure (Table 1). Figure 1 showed the diagram of the whole study and the purpose of the two parts.
Table 1.
Demographic data for the patients in the study
| Characteristics | Part 1 (n = 22) | Part 2 (n = 44) | |||
|---|---|---|---|---|---|
|
| |||||
| Group 1 (n = 11) | Group 2 (n = 11) | Group 3 (n = 11) | Group 4 (n = 11) | ||
| Age (years) | 45.8 ± 13.2 | 44.2 ± 13.6 | 39.3 ± 14.5 | 46.9 ± 12.7 | 47.9 ± 10.8 |
| Height (cm) | 158.5 ± 9.0 | 152.6 ± 7.8 | 156.3 ± 9.8 | 158.4 ± 8.0 | 160.1 ± 7.6 |
| Weight (kg) | 56.8 ± 7.2 | 54.5 ± 6.7 | 54.6 ± 8.0 | 60.1 ± 7.8 | 58.4 ± 7.0 |
| Blood Pressure (mmHg) | 113.3 ± 9.1 | 114.4 ± 7.8 | 112.9 ± 10.7 | 112.1 ± 8.7 | 111.1 ± 9.0 |
Values are expressed as mean ± SD. No significant among-group differences (P>0.05). Part 1: Sevoflurane group. Group 1: Propofol + atracurium group. Group 2: Sevoflurane 1.0 MAC + atracurium group. Group 3: Sevoflurane 1.5 MAC + atracurium group. Group 4: Sevoflurane 2.0 MAC + atracurium group.
Figure 1.
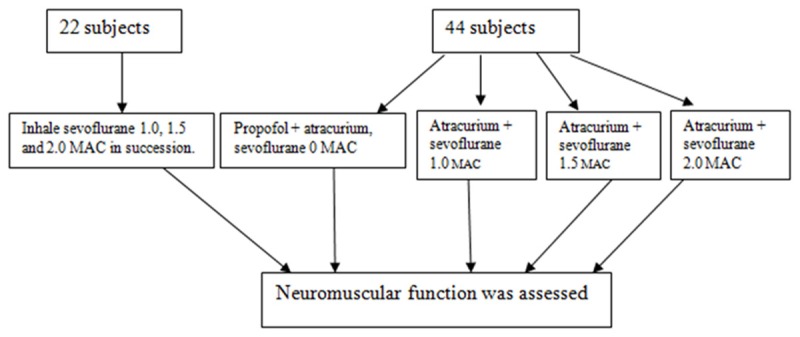
Diagram of the study. First part: 22 subjects were treated in a successive manner was to investigate whether sevoflurane has direct effects on the adductor pollicis contractility. Second part: 44 subjects were decided into 4 groups equally to investigate whether sevoflurane would increase the skeletal muscle sensitivity to atracurium, and which concentration of sevoflurane would the effect the sensitivity.
Sevoflurane alone under varying concentrations
Values for T1 and TOF ratio were similar at 1.0, 1.5, and 2.0 MAC sevoflurane. No significant differences were found between the initial periods of the study and the equilalent experimental data obtained during the final period of neuromuscular function testing. Compared to baseline, there was no significant difference in TOF value after inhalation of 1.0 MAC, 1.5 MAC, or 2.0 MAC sevoflurane (Table 2).
Table 2.
Neuromuscular responses during sevoflurane anesthesia (n = 22)
| Sevoflurane concentration (MAC) | T1 amplitude (% of control) | TOF ratio (%) |
|---|---|---|
| 0 (baseline) | 100 | 100 |
| 1.0 | 103 ± 35 | 100 ± 2 |
| 1.5 | 109 ± 29 | 96 ± 7 |
| 2.0 | 106 ± 27 | 96 ± 8 |
Mean ± SD. No significant among-group differences (P>0.05).
Sevoflurane or propofol with atracuriumin
Compared group 1 and group 2, there was no significant difference in atracurium onset time (time to reach TOF ratio = 0.25; 6.5 ± 1.7 min vs. 5.6 ± 1.8 min, p>0.05) (Figure 2). Though the degree of adductor pollicis block was higher in group 2 at 1.0 MAC servofluroane but it did not reach significance (TOF ratio = 0, 2 vs. 5 subjects, P = 0.36) (Figure 3). Compared group 3 or 4 with group 1, inhaling 1.5 or 2.0 MAC sevoflurane did decrease the atracurium onset time (4.6 ± 1.5 min and 4.0 ± 1.3 min vs. 6.5 ± 1.7 min, P<0.01 and P<0.001, respectively; Figure 2) and significantly enhanced the degree of adductor pollicis block (Figure 3, TOF ratio = 0, 9 and 10 vs. 2 subjects, P<0.001).
Figure 2.
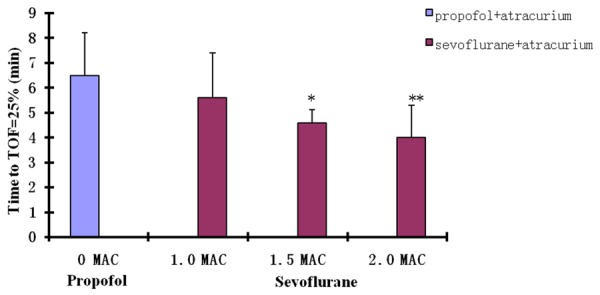
Effects of sevoflurane on atracurium onset time (time to reach TOF ratio = 0.25). Values are expressed as mean ± SD. Compared with group 1 (0 MAC), there was no significant difference in atracurium onset time in group 2 (1.0 MAC) (P>0.05). Compared with group 1, group 3 (1.5 MAC) and group 4 (2.0 MAC) did decrease the atracurium onset time (P<0.01 and P<0.001, respectively).
Figure 3.
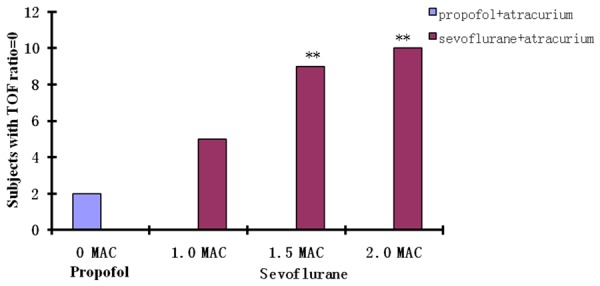
Effects of sevoflurane on atracurium block degree. Numbers of subjects (of 11 per group) with TOF ratio of 0. Compared with group 1 (0 MAC), there was no significant difference significance in group 2 (1.0 MAC) (2 vs. 5 subjects, P =0.36). Compared with group 1 (0 MACA), group 3 (1.5 MAC) or 4 (2.0 MAC) significantly enhanced the degree of adductor pollicis block (9 and 10 vs. 2 subjects, P<0.001).
Discussion
Sevoflurane alone had no significant direct effect on muscle relaxation, however, sevoflurane, but not propofol, increased the sensitivity to muscle relaxant atracurium.
In this study, a procedure as IVRA was obtained by local injection to avoid exposure of spinal cord or supraspinal cord to neuromuscular blockers, and the administered drugs will selectively target skeletal muscle only in the affected region. When a drug is given systematically, it is difficult to determine whether the effect is generated by acting on the muscle, spinal cord, or brain. Yang et al. devised a technique to administer anesthetics only into the spinal cord in experimental animals, and showed that the spinal cord was an important site of anesthetic action [18]. We were interested in determining possible anesthetic effects in skeletal muscle. So we administered the neuromuscular block drugs locally, to affect only the tested skeletal muscles, using IVRA. In 1908 Bier described the use of tourniquets and injected agents to induce localized anesthesia [19,20]. We used this principle to allow preferential delivery of neuromuscular blocking drug to the skeletal muscle by injecting the drug into the upper test arm blood vessel. This method allowed us to study the effects of sevoflurane on muscle relaxation without the interference of the central nervous system clearly demonstrate the direct effects of sevoflurane at the level of the skeletal muscle. This method may contribute to a better understanding of their neuromuscular mechanisms of action.
Our findings using atracurium in are consistent with previous studies showing that sevoflurane did not significantly affect the magnitude and recovery time of another nondepolarizing blocker, rocuronium [21]. In that study, isoflurane and sevoflurane both augmented the intensity of rocuronium-induced NMB to a similar extent
Previous studies [21,22] demonstrated the lack of potentiation of neuromuscular blockade when NMBs were combined with propofol, similar to what we have found in this study. The propofol group showed no increased sensitivity to atracurium. Beaussier et al. showed sevoflurane at 1 MAC decreases accelerometric responses of the adductor pollicis to atracurium [23]. The findings were supported by an animal study in which they showed that 1.0 MAC sevoflurane did not alter responses to peripheral nerve stimulation [24]. Our study confirmed that inhaled anesthetics can provide a dose-related muscle relaxation as reported in the previous studies [1-3] and also showed sevoflurane increased sensitivity to muscle relaxants but no direct muscle relaxation.
Further studies are necessary to determine the mechanisms underlying the enhancement of the sensitivity of skeletal muscles to neuromuscular blockers, and to assess the effects of inhaled anesthetics on neuromuscular blockage in male patients. In addition, it would also be interesting to test using different neuromuscular blockers.
Conclusions
In conclusion, we used a regional anesthesia method to develop a model to preferentially deliver neuromuscular blocking drugs to the skeletal muscle. Using this model, we confirmed that sevoflurane has no direct effects on the adductor pollicis contractility, but can increase the skeletal muscle sensitivity to neuromuscular blocker.
Disclosure of conflict of interest
None.
References
- 1.Eger II E, Eisenkraft J, Weiskopf R. Neuromuscular effects of inhaled anesthetics. In: Eger II E, editor. The Pharmacology of Inhaled Anesthetics. Sponsored by the Danmiller Memorial Educational Foundation, Educational Grant from Baxter Healthcare Corporation; 2003. pp. 133–145. [Google Scholar]
- 2.Kelly RE, Lien CA, Savarese JJ, Belmont MR, Hartman GS, Russo JR, Hollmann C. Depression of neuromuscular function in a patient during desflurane anesthesia. Anesth Analg. 1993;76:868–871. doi: 10.1213/00000539-199304000-00031. [DOI] [PubMed] [Google Scholar]
- 3.Miller RD, Way WL, Dolan WM, Stevens WC, Eger EI. The dependence of pancuronium and d-tubocurarine induced neuromuscular blockades on alveolar concentrations of halothane and forane. Anesthesiology. 1972;37:573–81. doi: 10.1097/00000542-197212000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Fogdall RP, Miller RD. Neuromuscular effects of enflurane, alone and combined with d-Tubocurarine, pancuronium and succinylcholine, in man. Anesthesiology. 1975;42:173–8. doi: 10.1097/00000542-197502000-00010. [DOI] [PubMed] [Google Scholar]
- 5.Cannon JE, Fahey MR, Castagnoli KP, Furuta T, Canfell PC, Sharma M, Miller RD. Continuous infusion of vecuronium: the effect of anesthetic agents. Anesthesiology. 1987;67:503–6. doi: 10.1097/00000542-198710000-00010. [DOI] [PubMed] [Google Scholar]
- 6.Caldwell JE, Laster MJ, Magorian T, Heier T, Yasuda N, Lynam DP, Eger EI, Weiskopf RB. The neuromuscular effects of desflurane, alone and combined with pancuronium or succinylcholine in humans. Anesthesiology. 1991;74:412–8. doi: 10.1097/00000542-199103000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Morita T, Tsukagoshi H, Sugaya T, Yoshhikawa D, Fujita T. The effects of sevoflurane are similar to those of isoflurane on the neuromuscular block produced by vecuronium. Br J Anaesth. 1994;72:465–7. doi: 10.1093/bja/72.4.465. [DOI] [PubMed] [Google Scholar]
- 8.Wulf H, Ledowski T, Linstedt U, Proppe D, Sitzlack D. Neuromuscular blocking effects of rocuronium during desflurane, isoflurane, and sevoflurane anaesthesia. Can J Anaesth. 1998;45:526–32. doi: 10.1007/BF03012702. [DOI] [PubMed] [Google Scholar]
- 9.Kastrup MR, Marsico FF, Ascoli FO, Becker T, Soares JH, Gomez de Segura IA. Neuromuscular blocking properties of atracurium during sevoflurane or propofol anaesthesia in dogs. Vet Anaesth Analg. 2005;32:222–7. doi: 10.1111/j.1467-2995.2005.00240.x. [DOI] [PubMed] [Google Scholar]
- 10.Caldwell JE, Laster MJ, Magorian T, Heier T, Yasuda N, Lynam DP, Eger EI, Weiskopf RB. The neuromuscular effects of desflurane, alone and combined with pancuronium or succinylcholine in humans. Anesthesiology. 1991;74:412–8. doi: 10.1097/00000542-199103000-00004. [DOI] [PubMed] [Google Scholar]
- 11.Miller RD, Eger EI II, Way WL, Stevens WC, Dolan WM. Comparative neuromuscular effects of forane and halothane alone in combination with d-tubocurarine in man. Anesthesiology. 1971;35:38–42. doi: 10.1097/00000542-197107000-00012. [DOI] [PubMed] [Google Scholar]
- 12.Péréon Y, Bernard JM, Nguyen The Tich S, Genet R, Petitfaux F, Guihéneuc P. The effects of desflurane on the nervous system: from spinal cord to muscles. Anesth Analg. 1999;89:490–5. doi: 10.1097/00000539-199908000-00046. [DOI] [PubMed] [Google Scholar]
- 13.Hicks RG, Woodforth IJ, Crawford MR, Stephen JP, Burke DJ. Some effects of isoflurane on I waves of the motor evoked potential. Br J Anaesth. 1992;69:130–6. doi: 10.1093/bja/69.2.130. [DOI] [PubMed] [Google Scholar]
- 14.Rampil IJ, Mason P, Singh H. Anesthetic potency (MAC) is independent of forebrain structures in the rat. Anesthesiology. 1993;78:707–12. doi: 10.1097/00000542-199304000-00014. [DOI] [PubMed] [Google Scholar]
- 15.Antognini JF, Schwartz K. Exaggerated anesthetic requirements in the preferentially anesthetized brain. Anesthesiology. 1993;79:1244–9. doi: 10.1097/00000542-199312000-00015. [DOI] [PubMed] [Google Scholar]
- 16.Yang J, Chai YF, Gong CY, Li GH, Luo N, Luo NF, Liu J. Further proof that the spinal cord, and not the brain, mediates the immobility produced by inhaled anesthetics. Anesthesiology. 2009;110:591–5. doi: 10.1097/ALN.0b013e3181974bfd. [DOI] [PubMed] [Google Scholar]
- 17.Viby-Mogensen J, Engbaek J, Eriksson LI, Gramstad L, Jensen E, Jensen FS, Koscielniak-Nielsen Z, Skovgaard LT, Ostergaard D. Good clinical research practice (GCRP) in pharmacodynamic studies of neuromuscular blocking agents. Acta Anaesthesiol Scand. 1996;40:59–74. doi: 10.1111/j.1399-6576.1996.tb04389.x. [DOI] [PubMed] [Google Scholar]
- 18.Yang J, Li Z, Gong CY, Chai YF, Li T, Li GH, Luo N, Luo NF, Zhu L, Liu J. A model for the preferential delivery of isoflurane to the spinal cord of the goat. Vet J. 2011;187:239–44. doi: 10.1016/j.tvjl.2010.01.004. [DOI] [PubMed] [Google Scholar]
- 19.Holmes CM. The history and development of intravenous regional anaesthesia. Acta Anaesthesiol Scand Suppl. 1969;36:11–8. doi: 10.1111/j.1399-6576.1969.tb00473.x. [DOI] [PubMed] [Google Scholar]
- 20.Brown EM, McGriff JT, Malinowski RW. Intravenous regional anaesthesia (Bier block): review of 20 years’ experience. Can J Anesth. 1989;36:307–10. doi: 10.1007/BF03010770. [DOI] [PubMed] [Google Scholar]
- 21.Wulf H, Ledowski T, Linstedt U, Proppe D, Sitzlack D. Neuromuscular blocking effects of rocuronium during desflurane, isoflurane, and sevoflurane anaesthesia. Can J Anaesth. 1998;45:526–32. doi: 10.1007/BF03012702. [DOI] [PubMed] [Google Scholar]
- 22.McCarthy GJ, Mirakhur RK, Pandit SK. Lack of interaction between propofol and vecuronium. Anesth Analg. 1992;75:536–8. doi: 10.1213/00000539-199210000-00012. [DOI] [PubMed] [Google Scholar]
- 23.Beaussier M, Boughaba A, Schiffer E, Debaene B, Lienhart A, d’Hollander A. Acute desflurane or sevoflurane exposure on a previously stabilized atracurium-induced neuromuscular block. Eur J Anaesthesiol. 2006;23:755–9. doi: 10.1017/S0265021506000706. [DOI] [PubMed] [Google Scholar]
- 24.Kastrup MR, Marsico FF, Ascoli FO, Becker T, Soares JH, Gomez de Segura IA. Neuromuscular blocking properties of atracurium during sevoflurane or propofol anaesthesia in dogs. Vet Anaesth Analg. 2005;32:222–7. doi: 10.1111/j.1467-2995.2005.00240.x. [DOI] [PubMed] [Google Scholar]


