Abstract
Objectives
Emergency department (ED) discharge requires conveying critical information in a time-limited and distracting setting. Limited health literacy may put patients at risk of incomplete comprehension, but the relationship between discharge communication needs and health literacy has not been well defined. The goal of this study was to characterize the variation in needs and preferences regarding the ED discharge process by health literacy, and identify novel ideas for process improvement from parents and patients.
Methods
This was an in-depth qualitative interview study in two EDs using asthma as a model system for health communication. Adult patients and parents of pediatric patients with an asthma exacerbation and planned discharge were enrolled using purposive sampling to balance across literacy groups at each site. Interviews were audiotaped, transcribed, coded independently by two team members, and analyzed using a modified grounded theory approach. Interviews were conducted until thematic saturation was reached in both literacy groups at each site.
Results
In-depth interviews were completed with 51 participants: 20 adult patients and 31 pediatric parents. The majority of participants identified barriers related to ED providers, such as use of medical terminology; and systems of care, such as absence of protected time for discharge communication. Patients with limited health literacy, but not those with adequate literacy, identified conflicting information between health care sources as a barrier to successful ED discharge.
Conclusions
Participants across literacy groups and settings identified multiple actionable areas for improvement in the ED discharge process. These included the use of simplified/lay language, increased visual learning and demonstration, and the desire for complete information. Individuals with limited literacy may particularly benefit from increased attention to consistency.
INTRODUCTION
The emergency department (ED) discharge process requires the communication of complex information to patients in a time-limited and distracting setting.1,2 Previous studies have shown that patients often leave the ED without complete understanding of their ED care and home management plans.3 Although studies have suggested an important role for standardized verbal content4 and dosing demonstration5 in improving discharge instructions, the optimal timing, content, and methodology for discharge teaching remain to be described.2 In particular, guidelines for ED discharge have been based on the medical literature,2 physician and health system sources,6 but have not incorporated parent or patient perspectives. Patients and parents, as participants in discharge communication and with ultimate responsibility for implementing instructions at home, may have novel ideas for improvement to the process and add a unique perspective to our understanding of the discharge process.
Health literacy, the ability to acquire and use health information to make decisions,7 involves both the individual’s skill set and the complexity of the information and decision at hand.7 Limited health literacy is highly prevalent in the ED8,9 and associated with worse health outcomes10 including increased ED visits,11,12 particularly for low acuity complaints,13 and dosing errors.14 Limited health literacy is also associated with increased parental perception of asthma disease burden.15 ED discharge communication may be particularly challenging for patients with limited health literacy.16 The absence of parental input into the creation of discharge processes and materials is likely to be particularly detrimental to parents with limited health literacy, as provider-derived materials are often written at too adequate a level of health literacy and parents with limited health literacy may ask fewer questions about their medical care and have less access to additional sources of information.17
Asthma provides an excellent model system for studying ED discharge communication. Asthma is common, with 1.1 million ED visits annually, and expensive, costing $18 billion every year in medical expenses.18 Asthma is common in both adult and pediatric populations, accounting for an estimated 600,000 pediatric visits.19 Minority children, those living in urban areas, and those with lower socio-economic status are most at risk, with African American children having the highest rates of ED visits and death from asthma.19 The ED discharge process requires communication of information regarding chronic care and acute exacerbations.
Asthma patients with limited health literacy have poorer quality of life, decreased functional status and increased ED visits when compared with their adequate literacy counterparts.20,21 In particular, discharge teaching for patients presenting to the ED with asthma exacerbations is often a missed opportunity to ask questions and have the provider summarize key information.22 While educational interventions to improve asthma care have been shown to be efficacious in some settings,23 efforts to improve asthma teaching in the ED have not had significant effects on follow-up24,25 or subsequent ED visits,24,26 although they may change beliefs about asthma24 and increase spacer use.27 This suggests that novel approaches to intervention are needed. Parents and families are an untapped resource to understand what processes and information would be most helpful at ED discharge and may have perspectives that differ in important ways from their providers.
The goal of this study was to characterize patient and parent perceptions of needs and preferences regarding the ED discharge process by health literacy, compare perspectives between the adult and pediatric populations, and identify novel ideas for process improvement from parents and patients.
METHODS
Study Design
Semi-structured, open-ended, interviews were conducted in person during ED visits using purposive sampling to balance across adult and pediatric populations and literacy groups. Unlike quantitative research, designed to achieve the power necessary to test a specific hypothesis, qualitative research is used to assess the scope of ideas related to a concept. As such, the goal is to identify the range of opinions and identify new ideas and concepts, rather than to measure how many individuals have each opinion. Qualitative research continues until thematic saturation is reached; the point at which no new themes are emerging. The sampling strategy is purposive, designed to make sure the full range of themes is elicited within each pre-specified group. Interviews are continued until thematic saturation is reached in each pre-specified group, which is the point at which interviews are no longer revealing new information about the primary topic of interest; in this case, needs and preferences around the ED discharge process.28 This study was approved by the Institutional Review Board at the University of Pennsylvania and Children’s Hospital of Philadelphia.
Study Setting and Population
Study participants were recruited until thematic saturation was reached in adequate and limited literacy groups in each of the populations (adult patient and parents of pediatric patients). Transcripts were coded and analyzed throughout the study process (see Analysis below) to allow for the identification of thematic saturation in each group. Thematic saturation was identified by team consensus.
The study was conducted in two EDs: adult patients were recruited from an urban tertiary care ED with an annual volume of 72,000 patients and parents of pediatric patients were recruited from a neighboring tertiary care pediatric ED with an annual volume of over 90,000 patients. At both sites patients are discharged primarily by registered nurse (RN) providers giving unscripted instructions, which can be highly variable in length, content and detail. Each site has a slightly different pre-written set of asthma instructions that are provided in written form to patients as part of their electronically generated discharge instructions.
Adult patients were eligible for inclusion if they were 18 years or older and were undergoing treatment for asthma with plan for discharge home. Due to the need to participate in an in-depth interview with a research assistant, patients were required to be fluent in English. Patients were excluded from the study if they were undergoing active resuscitation, had expected need for hospital admission, had major medical co-morbidities or their provider determined they were inappropriate for the study. Because of the overlap between chronic obstructive pulmonary disease (COPD) and asthma, patients with dual diagnoses were considered eligible for inclusion.
Parents of pediatric patients were eligible if they had a child aged 11 or under being treated for asthma in the ED with planned discharge home. The age limit was designed to select a population where the teaching is focused primarily on the parent, rather than on an adolescent or young adult. Similar to the adult patient criteria, parents were eligible for inclusion if they spoke English. Parents of children with complex healthcare needs were excluded from the sample, as they have very different experiences of learning in the healthcare system; also excluded were parents the provider felt it would be inappropriate to approach. Major medical co-morbidities or complex health care needs included artificial airways, active congestive heart failure exacerbation, cystic fibrosis and active cancer treatment.
Study Protocol
Participants were identified while they or their child were in the ED receiving care for asthma during periods when a trained research assistant was present. Participants underwent a verbal consent process to minimize literacy barriers to participation. Interviews occurred after the medical team determined the patient would be discharged but usually before the actual discharge process to avoid interfering with ED workflow and room turnover. Nominal gift cards were offered as incentives for participation. A brief demographic survey with information on race, education, and insurance status was completed. Adult patients were then administered the Newest Vital Sign, a well-validated tool to assess health literacy.29 This tool consists of a nutrition label with six accompanying questions and takes approximately three minutes to complete. Parents of pediatric patients completed the Parental Health Literacy Activities Test (PHLAT),30 which covers domains of literacy and numeracy particularly relevant for the care of young children. Score on the literacy assessment was used to define adequate and inadequate (limited) health literacy, based on comparisons to previously published mean values.30,31
Interview domains
Patient interviews were conducted by a two research assistants trained in in-depth interviewing by experts in qualitative methodology (MSK, CM, KR). The interview guide was developed based on a literature review of articles examining discharge communication and underwent an iterative process of revision during the early stages of recruitment. Interviewees were asked questions about styles of learning, education from their primary care provider and about ED discharge teaching, in general and not limited to asthma-related visits. Interview domains and sample questions are shown in Table 1. Initial interviews were directly observed by trained staff, and investigators met regularly to assess the quality of interviews.
Table 1.
Interview guide domains and sample questions
| Domains | Sample questions |
|---|---|
| Prior learning experience |
|
| ED learning experience |
|
| Desired content of instruction |
|
| Preferred method of learning |
|
| Barriers to understanding and implementation of discharge instructions |
|
Data Analysis
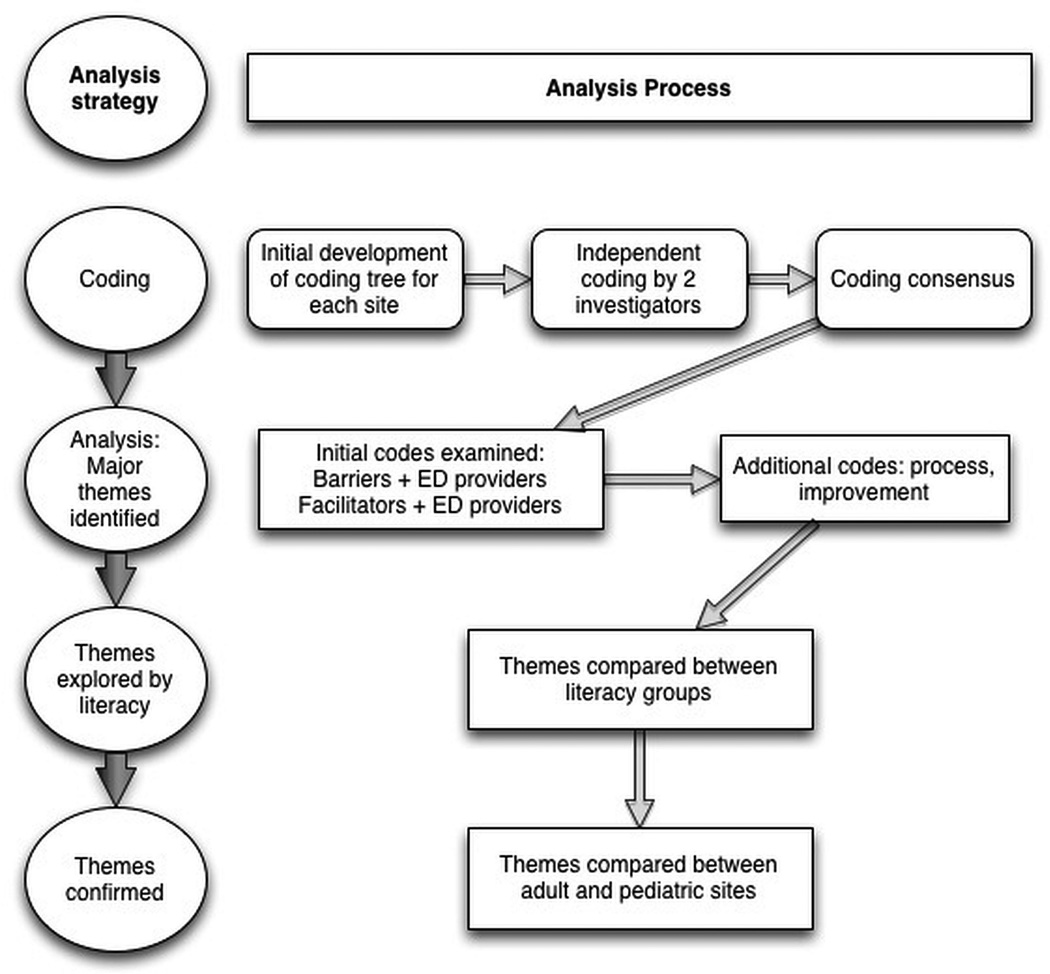
All interviews were recorded and professionally transcribed. A coding tree was developed based on the interview guide, and was refined with input of the entire team. Transcripts were coded by two independent investigators who met regularly to assess agreement. All differences were resolved by consensus. Themes were identified by reviewing relevant sections of transcripts, and were discussed by the entire study team. Coding and theme development were ongoing throughout the study process, with changes made to the coding tree and interview guide as themes emerged. Analyses used a modified grounded theory framework (Figure 1) and thematic saturation was identified by team consensus.
Figure 1.
RESULTS
In-depth interviews were completed with 51 participants. Of the 31 pediatric parents interviewed, 15 (48%) were limited literacy, 26 (85%) were black or African-American, and 25 (81%) had public insurance. Of the 20 adult patients interviewed, 12 (60%) patients had limited literacy, 17 (85%) were African American, and 16 (80%) had public/no insurance. These demographics are similar to those of the population with asthma served at each center. Of the pediatric parents interviewed, 12 (39%) completed high school, GRE or less; 14 (45%) completed some college and five (16%) completed college or a higher degree. Of the adult patients interviewed, six (30%) had a high school degree, GRE or less; ten (50%) had some college and four (20%) finished college or a higher degree.
The majority of participants identified barriers to discharge success related to ED providers and systems of care. A minority identified important patient-level barriers (Table 2 and Data Supplement 1).
Table 2.
Summary of key themes and supporting quotes
| Theme | Literacy group |
Adult patients | Pediatric Parents |
|---|---|---|---|
| Importance of avoiding medical jargon Need for simplified/lay language and materials |
Both | [You] can say a lot of these crazy words, but everybody doesn’t really know what you’re saying… [I’m] more comfortable when doctors break it down. (limited literacy) | They’ll give you a printout at the end of the day when you leave about what happened with the visit. But I know a lot of times I’ll go home and Google because I really didn’t understand like what that meant…what it really mean in layman’s terms…for me it would be more helpful if it was already written in those terms, in just like general speaking terms. (Limited literacy) |
| Need for verbal teaching and demonstration | Both | But if you show them step-by-step, just like you with a child, if you show a child a step-by-step on how to do something, then they’ll get it, instead of them, instead of you just telling them what to do. You have to show them what to do. And they have visualizing and they’ll remember it. (limited literacy) | Actually show me, so that way I know exactly everything instead of me, you know, guessing or assuming … I had to give him 5.2 MLs, and the – what is it called – the medicine tube thing, it only had 5 MLs on there, so like I didn't know like where the two point was at, like 5.2. So if someone would have showed me like this is where 5.2 is, I would know. (adequate literacy) |
| Desire for increased information | Both | Don't put [important information] too far back [in the discharge paperwork], because then if you're just scanning through it you don't really care about the rest of the paper. (adequate literacy) | I want them to pretty much be more detailed about stuff, letting me know what's going on, just don’t go out there and talk, it’s my child. Let me know what's going on, too. (limited literacy) |
| Request for more, and protected, time with provider | Both | So if he take his time…I’m better able to get it. So, I would say people need patience. If somebody patient with me and explain it, and I’m listening to them, I pick it up. (adequate literacy) | I mean, have one person that can come in instead of being a doctor that’s trying to do 1,000 things at one time. Just the one person that could come in and just all about information and you could sit down and talk with them, and if you have any questions, you can ask some questions and they can answer your questions (limited literacy) |
| Concern about conflicting information | Limited literacy, primarily | I go home with the instructions they give me. I follow them. They don’t work. I call my primary and have me go in to their office, then they’ll say, well, they shouldn’t have gave you this if you’re already on this, and the next thing you know, I’m at another hospital. (Limited literacy) | I actually think the box instructions is pretty much always different from what the doctor say do…a lot of times when he’s discharged, I’ll follow up with his doctor and it’s different instructions of when to come back and it kind of get – a lot of times it gets like this tug of war between emergency and his regular primary care, when to go to either place, so I don’t really know (limited literacy) |
| Concern about provider judgment | Both | A lot of people don’t come back to the ER because they sometimes feel like they're being judged, because we come to the hospital when we do. (Limited literacy) | I seem like I'm listening and I'm like yeah, okay. And I don't want to – because they're doing so well trying to explain it to me and being real nice. And I feel like – oh, I feel like I'm gonna tell them I don't understand and they're gonna feel like they're wasting their time or anything. So I just nod like, you know, you get what I'm saying, I'm like yeah, yeah. (limited literacy) |
Provider Factors
Adult patients
In both literacy groups, a majority of adult patients identified barriers to discharge success related to ED providers. Patients discussed struggling with medical jargon and their desire for the use of simplified/lay language, a need for increased visual learning and demonstration, and the desire for complete information.
One patient with adequate literacy recalled an interaction in which she did not understand the language her physician used, later prompting her to look-up words in the dictionary: “I don’t know these big medical terms. They just throw you information with no explanation.” The majority of patients in both literacy groups voiced a desire for visual and verbal adjuncts to discharge teaching. Another patient with adequate literacy described a particularly helpful interaction in which a provider demonstrated nebulizer use. “She broke it down… start from the plug, how to plug it in, how to drip the medicine in… how to hook the tube up to the machine.”
A majority of patients in both literacy groups also expressed the desire for increased written information. A patient with adequate literacy also commented on the value of discharge paperwork, but suggested that material be presented in a more concise fashion using “a bullet-point list of what you need to do.” Patients discussed the importance of complete and candid information during their ED care, including detailed information regarding medications, with a limited literacy patient suggesting that physicians should “tell you why the medicine works and what the medicine does to help you… it would show you how important it is.”
Several themes were reported by fewer participants including the need to feel heard by providers and provider engagement of family. For example, many patients expressed concerns about feeling heard by their providers, with one patient with adequate literacy stating that “doctors will think they know better than you and not really take into consideration what you’re trying to tell them.” To improve the discharge process, some patients suggested that providers engage families during discharge teaching. Interestingly, a limited literacy patient suggested that providers engage family members to help bridge literacy gaps, suggesting that patients should “bring somebody with them that will understand… someone that knows your situation that can read, or that can explain to you.”
Parents of Pediatric Patients
Among the pediatric parents, the most prevalent theme was also a desire for lay language and simplified terms. Parents in both literacy groups frequently reported feeling uncomfortable with medical terminology, and how that led to leaving the ED without full comprehension. Parents in both literacy groups raised concerns about the labeling of dosing instruments not matching the amount they were instructed to give, and the calculations required to make sure they are giving an appropriate dose of liquid medication. One parent with limited literacy said: “Droppers sometimes don’t say how much they need to give them, so it need to be exactly say this amount of milliliters, it needs to be that on the dropper. Not teaspoons…. I was never good in measuring. It’s like the percents and fractions, I wasn’t good at math at all. So that's like difficult for me.”
Across all literacy groups, parents emphasized the importance of written information. Parents with limited literacy requested simplified sheets containing only the most important points: “I think legally you have to put all this stuff down, but like if you give us just our own separate page just for us as parents, like especially me. I'm working. I'm tired, and then I'm trying to go back to school, but it's just like I don't need a whole lot of pressure, like oh, I have to read this or I'm a bad parent because I don't know what I'm talking about.”
However, written materials alone were seen by parents as insufficient, and parents in both literacy groups discussed the importance of having verbal instructions to reiterate and emphasize the information provided in the verbal instructions. Parents particularly emphasized the importance of demonstration of medication administration and dosing (Table 2).
The idea of creating a dosing schedule to help parents remember when to give different medications or complete elements of the treatment plan was mentioned repeatedly by parents with adequate literacy. Although one parent with limited literacy did mention that an “itinerary” listing tasks to complete after the ED visit would be helpful, no other limited literacy parents discussed the creation of a dosing schedule.
In both literacy groups, parents reported a desire for more information from ED providers. Parents wanted to be active participants in their child’s care, and to be updated with results or changes in exam findings.
System Factors
Adult patients
A majority of patients in both literacy groups also identified factors at the system level impacting the discharge process. Major themes included the need for protected time for communication in the ED and desire for reminders after discharge. Patients with limited health literacy also identified conflicting information between healthcare sources as a barrier to successful ED discharge, which was not mentioned by the patients with adequate literacy.
In regard to protected time for communication, one patient with adequate literacy recalled an interaction with an emergency medicine provider who was waiting for the arrival of a trauma patient. The patient described the hurriedness of the interaction: “the doctor’s asking me questions real, real quick, real, real quick, and before I got to respond, he was out the door.” Many patients in both literacy groups also expressed the desire for increased reminders after ED discharge including telephone calls and letters from their physicians. Several patients also discussed the role of cellular phone reminders and email reminders from providers in supporting discharge plans.
Patients with limited health literacy were more likely to discuss struggling with conflicting information. Likewise, limited literacy patients were much more likely to discuss switching between hospitals.
Parents of Pediatric Patients
Similar to the adult patients, information inconsistency was mentioned frequently by parents with limited literacy but not by those with adequate literacy. Parents described inconsistencies between medication package instructions and physician information and between different health care providers. One limited literacy parent discussed being confused by information from different providers: “I think sometimes it can be the doctors or nurses, respiratory… and it’s just like one person can say this, then the next moment, somebody else is saying this, and sometimes make you a little confused”
Parents also emphasized the importance of protected time and space for discharge communication. As one limited literacy parent said, “If we could have just like a room right before we leave, like a nice little room where it's quiet and he's treated and everything, and we could just actually sit down and just talk with our physician and our nurse, like what can we do to like make sure this doesn't happen again, and there's no distraction.”
A few parents from both literacy groups reported a desire to follow-up in the ED, and a wish for a follow up call from the ED provider to find out how their child is doing. Others suggested the use of existing down time in the ED (such as the waiting room) for enhanced teaching opportunities.
Patient Factors
Adult patients
Some patients also expressed patient level factors influencing the ED discharge process, including the feeling of provider judgment (Table 2) and the complex role of family dynamics on care. A small proportion of patients also identified finances as a barrier to care.
Patients in both literacy groups discussed the complex role family dynamics play in their asthma care. One patient with adequate literacy recalled her family’s skepticism of her asthma exacerbation, stating “my family, they not very supportive… Like the other day somebody was saying, oh, you didn’t look sick. You just lazy or making excuses.” Alternatively, one patient with limited literacy described the role of family and the broader community in understanding asthma, stating “every other person you run into has asthma. So I just talk to them and we bounce ideas off each other.” Many patients with children also discussed prioritizing their children’s health needs above their own.
Finally, some patients identified finances as a barrier to care with one limited literacy patient stating, “Insurance play[s] a big part of it. If they don’t have insurance, some people don’t go to the doctors at all because they don’t have insurance. Sometimes the patient might not have the money to go back to the doctors. So they’ll just wait.”
Parents of Pediatric Patients
Some pediatric parents also identified concerns about being judged by providers, as one parent with limited literacy said: “Some people, they just don't want to ask questions because they don't want to feel like they're being like a bother or a pest.” Less frequently identified themes included the need for child care and assistance with distraction in the ED.
DISCUSSION
The majority of patients in both literacy groups discussed factors at the provider and system level that impact care, providing novel and actionable opportunities for improvement. Similar themes were identified across the adult and pediatric population, suggesting that the same process improvements may work for both populations. Participants in all literacy groups requested simplified language, verbal learning and demonstration. Attention to consistency of information was particularly important for participants with limited health literacy.
Provider factors
Patients and parents, in all literacy groups, expressed strong preference for the use of simplified language, visual learning and demonstration. Simplification of written materials2,32, use of verbal and written instructions4,33,34 and dosing demonstration5,35 have been shown to be associated with increased comprehension and dosing accuracy in prior research. A previous study of patient recommendations regarding ED discharge instructions identified eight themes for improvement: define complex words, present motivational information, provide practical information and examples, clarify uncertainty and manage expectations, use visual aids, address inappropriate practices, provide a logical flow of information and identify key points.17 Although that study did not examine how patient perspectives varied based on literacy, and only focused on changes to the written materials, the themes of simplification of language, clarifying uncertainty, using visual aids and identifying key points were echoed in our interviews with parents
Participants requested more detailed information about the ED care and home management plan. These data suggest that such information should be provided through verbal instruction in lay language, with simplified written instructions for home reference and demonstration of medication administration. Restructuring written ED discharge instructions using patient-generated suggestions of bulleted lists and highlighting the most important information is a low cost intervention with significant potential benefit.
Systems factors
Newly identified from the current study is the importance of consistency in language and terminology across providers, particularly for parents with limited health literacy. We suspect that limited health literacy makes it more difficult to reconcile differing language choices between providers, leading to the perception of conflicting information, and these patients may be less able to access written materials to help resolve those differences.
Participants expressed the need for protected time for communication. Environmental modifications, such as quiet spaces for discharge teaching, may safeguard the patient-physician interaction and facilitate better understanding during the discharge process. Implementation of reminders after discharge, such as cellular phone text messages or automated telephone calls, may also help patients implement discharge instructions.
Participants in all groups discussed wanting follow-up after their ED visit. While email or phone contact from emergency physicians after the visit does appear to improve patient satisfaction,36 due to the staffing constraints of most EDs, it is unlikely that patients will regularly receive a call from their ED treatment team. Previous studies of ED follow-up rely on a practitioner separate from the initial treating team to follow-up results,37 enhance education,38 or reinforce linkage to primary care.39 While systems of follow-up calls are often implemented to reduce 72-hour return visits, one study found that follow-up calls by medical students were associated with an increase in the 72-hour return visit rate.40 More research is needed to investigate the optimal form contact with patients and families to improve implementation of instructions and post-ED outcomes.
Patient factors
Some participants in both settings identified provider feeling of judgment as a deterrent to seeking medical care. Our data suggest that parents are often unwilling or uncomfortable admitting to the team that they do not understand. More research is needed on how best to create an environment where parents feel comfortable admitting when they do not understand so that patients and families can leave the ED with meaningful comprehension of their care plan.
Several parents discussed the challenge of trying to learn complex new information while also supervising one or more children, and suggested that assistance with a brief period of child-care could greatly improve their retention of the material.
Adult patients, but not pediatric parents, discussed the complex role of family on healthcare. Similar to prior studies showing that social networks influence the way asthma patients understand their disease and care for themselves, patients in this study identified interaction with family as a key factor is seeking care for themselves. While modifying baseline family dynamics is not feasible, understanding this dynamic may provide a better understanding of our patients. Engaging family and community networks in facilitating understanding and implementing discharge instructions may also be useful.
LIMITATIONS
As with all qualitative studies, these results should be interpreted as hypothesis generating rather than hypothesis testing. While we interviewed to thematic saturation in both the adequate and limited literacy groups in both adult and pediatric settings, it is possible that additional interviews with many more participants– or participants in other settings - would have yielded new perspectives and suggestions. Indeed, we did not design the study to stratify on other potential predictors of preferences, such as age, race or insurance status. We chose to enroll parents of children <11years old to focus on the discharge needs and preferences of parents with young children; further work is needed to investigate the preferences of the pediatric patient, particularly the adolescent, and the role of the child’s literacy.21 We chose to use asthma as a model system for studying health communication, as discussed in the introduction. Although the participants discussed experiences with learning in the healthcare system and the ED beyond just their asthma care, this patient population does potentially limit the generalizability of our findings. In addition, our participants were primarily African American and state insured, and further research will be needed to explore if these themes and improvements are relevant to other patients. However, given the significant disease burden of asthma, particularly on African-American and low socio-economic status patients, we would argue that even if these findings only apply to this group, the resultant ideas for intervention have the potential to be significant improvements to care. Finally, additional work is needed to characterize the specific needs of parents and patients with limited English fluency.
CONCLUSIONS
To our knowledge, this is the first study to compare parent and patient perspectives on ED discharge needs and address potential improvements by health literacy. Participants across literacy groups and settings identified multiple actionable areas for improvement in the ED discharge process at the provider and system levels. These included the use of simplified/lay language, a need for increased visual learning and demonstration, and the desire for complete information. Limited literacy patients and parents may particularly benefit from increased attention to consistency across different sources of provided information. Increasing comfort with asking questions and admitting confusion will be important to improve discharge communication. Our data suggest that these improvements would be beneficial across the adult and pediatric ED populations. These data provide hypotheses for testing in future studies to investigate the effects of these interventions on patient and parent understanding, implementation of instructions and satisfaction.
Supplementary Material
Acknowledgments
Dr. Samuels-Kalow is supported by NIH K12 HL10900904. The project was funded by the Region II Academic Pediatric Association Young Investigator Award and the Armstrong Award (Masters of Science Program in Health Policy Research, University of Pennsylvania).
Footnotes
Presentations: The Pediatric Academic Societies (San Diego, 2015), and the Society for Academic Emergency Medicine (San Diego, 2015) meetings.
Disclosures: The authors have no financial disclosures or conflicts of interest.
References
- 1.Vashi A, Rhodes KV. "Sign Right Here and You're Good to Go": a content analysis of audiotaped emergency department discharge instructions. Ann Emerg Med. 2011;57:315–322. doi: 10.1016/j.annemergmed.2010.08.024. [DOI] [PubMed] [Google Scholar]
- 2.Samuels-Kalow ME, Stack AM, Porter SC. Effective discharge communication in the emergency department. Ann Emerg Med. 2012;60:152–159. doi: 10.1016/j.annemergmed.2011.10.023. [DOI] [PubMed] [Google Scholar]
- 3.Engel KG, Heisler M, Smith DM, Robinson CH, Forman JH, Ubel PA. Patient comprehension of emergency department care and instructions: are patients aware of when they do not understand? Ann Emerg Med. 2009;53:454–461. doi: 10.1016/j.annemergmed.2008.05.016. [DOI] [PubMed] [Google Scholar]
- 4.Isaacman DJ, Purvis K, Gyuro J, Anderson Y, Smith D. Standardized instructions: do they improve communication of discharge information from the emergency department? Pediatrics. 1992;89:1204–1208. [PubMed] [Google Scholar]
- 5.McMahon SR, Rimsza ME, Bay RC. Parents can dose liquid medication accurately. Pediatrics. 1997;100:330–333. doi: 10.1542/peds.100.3.330. [DOI] [PubMed] [Google Scholar]
- 6.Limpahan LP, Baier RR, Gravenstein S, Liebmann O, Gardner RL. Closing the loop: best practices for cross-setting communication at ED discharge. Am J Emerg Med. 2013;31:1297–1301. doi: 10.1016/j.ajem.2013.04.017. [DOI] [PubMed] [Google Scholar]
- 7.Paasche-Orlow MK, Wolf MS. The causal pathways linking health literacy to health outcomes. Am J Health Behav. 2007;31(Suppl 1):S19–S26. doi: 10.5555/ajhb.2007.31.supp.S19. [DOI] [PubMed] [Google Scholar]
- 8.Ginde AA, Weiner SG, Pallin DJ, Camargo CA., Jr Multicenter study of limited health literacy in emergency department patients. Acad Emerg Med. 2008;15:577–580. doi: 10.1111/j.1553-2712.2008.00116.x. [DOI] [PubMed] [Google Scholar]
- 9.Herndon JB, Chaney M, Carden D. Health literacy and emergency department outcomes: a systematic review. Ann Emerg Med. 2011;57:334–345. doi: 10.1016/j.annemergmed.2010.08.035. [DOI] [PubMed] [Google Scholar]
- 10.DeWalt DA, Hink A. Health literacy and child health outcomes: a systematic review of the literature. Pediatrics. 2009;124(Suppl 3):S265–S274. doi: 10.1542/peds.2009-1162B. [DOI] [PubMed] [Google Scholar]
- 11.DeWalt DA, Dilling MH, Rosenthal MS, Pignone MP. Low parental literacy is associated with worse asthma care measures in children. Ambul Pediatr. 2007;7:25–31. doi: 10.1016/j.ambp.2006.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Morrison AK, Myrvik MP, Brousseau DC, Hoffmann RG, Stanley RM. The relationship between parent health literacy and pediatric emergency department utilization: a systematic review. Acad Pediatr. 2013;13:421–429. doi: 10.1016/j.acap.2013.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Morrison AK, Schapira MM, Gorelick MH, Hoffmann RG, Brousseau DC. Low caregiver health literacy is associated with higher pediatric emergency department use and nonurgent visits. Acad Pediatr. 2014;14:309–314. doi: 10.1016/j.acap.2014.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yin HS, Mendelsohn AL, Wolf MS, et al. Parents' medication administration errors: role of dosing instruments and health literacy. Arch Pediatr Adolesc Med. 2010;164:181–186. doi: 10.1001/archpediatrics.2009.269. [DOI] [PubMed] [Google Scholar]
- 15.Shone LP, Conn KM, Sanders L, Halterman JS. The role of parent health literacy among urban children with persistent asthma. Patient Educ Couns. 2009;75:368–375. doi: 10.1016/j.pec.2009.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Williams DM, Counselman FL, Caggiano CD. Emergency department discharge instructions and patient literacy: a problem of disparity. Am J Emerg Med. 1996;14:19–22. doi: 10.1016/S0735-6757(96)90006-6. [DOI] [PubMed] [Google Scholar]
- 17.Buckley BA, McCarthy DM, Forth VE, et al. Patient input into the development and enhancement of ED discharge instructions: a focus group study. J Emerg Nurs. 2012;61:394–403. doi: 10.1016/j.jen.2011.12.018. [DOI] [PubMed] [Google Scholar]
- 18.Pai S, Boutin-Foster C, Mancuso CA, Loganathan R, Basir R, Kanna B. "Looking out for each other": a qualitative study on the role of social network interactions in asthma management among adult Latino patients presenting to an emergency department. J Asthma. 2014;51:714–719. doi: 10.3109/02770903.2014.903967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nelson KA, Zorc JJ. Asthma update. Pediatr Clin N Am. 2013;60:1035–1048. doi: 10.1016/j.pcl.2013.06.003. [DOI] [PubMed] [Google Scholar]
- 20.Mancuso CA, Rincon M. Impact of health literacy on longitudinal asthma outcomes. J Gen Intern Med. 2006;21:813–817. doi: 10.1111/j.1525-1497.2006.00528.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Robinson LD, Jr, Calmes DP, Bazargan M. The impact of literacy enhancement on asthma-related outcomes among underserved children. J Natl Med Assoc. 2008;100:892–896. doi: 10.1016/s0027-9684(15)31401-2. [DOI] [PubMed] [Google Scholar]
- 22.Crain EF, Mortimer KM, Bauman LJ, et al. Pediatric asthma care in the emergency department: measuring the quality of history-taking and discharge planning. J Asthma. 1999;36:129–138. doi: 10.3109/02770909909065156. [DOI] [PubMed] [Google Scholar]
- 23.Boyd M, Lasserson TJ, McKean MC, Gibson PG, Ducharme FM, Haby M. Interventions for educating children who are at risk of asthma-related emergency department attendance. Cochrane Database Syst Rev. 2009:CD001290. doi: 10.1002/14651858.CD001290.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zorc JJ, Chew A, Allen JL, Shaw K. Beliefs and barriers to follow-up after an emergency department asthma visit: a randomized trial. Pediatrics. 2009;124:1135–1142. doi: 10.1542/peds.2008-3352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Smith SR, Jaffe DM, Highstein G, Fisher EB, Trinkaus KM, Strunk RC. Asthma coaching in the pediatric emergency department. Acad Emerg Med. 2006;13:835–839. doi: 10.1197/j.aem.2006.03.565. [DOI] [PubMed] [Google Scholar]
- 26.Smith SR, Jaffe DM, Fisher EB, Jr, Trinkaus KM, Highstein G, Strunk RC. Improving follow-up for children with asthma after an acute emergency department visit. J Pediatr. 2004;145:772–777. doi: 10.1016/j.jpeds.2004.08.029. [DOI] [PubMed] [Google Scholar]
- 27.Cheng NG, Browne GJ, Lam LT, Yeoh R, Oomens M. Spacer compliance after discharge following a mild to moderate asthma attack. Arch Dis Child. 2002;87:302–305. doi: 10.1136/adc.87.4.302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rhodes KV, Bisgaier J, Lawson CC, Soglin D, Krug S, Van Haitsma M. "Patients Who Can't Get an Appointment Go to the ER": access to specialty care for publicly insured children. Ann Emerg Med. 2012;61:394–403. doi: 10.1016/j.annemergmed.2012.10.030. [DOI] [PubMed] [Google Scholar]
- 29.Weiss BD, Mays MZ, Martz W, et al. Quick assessment of literacy in primary care: the newest vital sign. Ann Fam Med. 2005;3:514–522. doi: 10.1370/afm.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kumar D, Sanders L, Perrin EM, et al. Parental understanding of infant health information: health literacy, numeracy, and the Parental Health Literacy Activities Test (PHLAT) Acad Pediatr. 2010;10:309–316. doi: 10.1016/j.acap.2010.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yin HS, Sanders LM, Rothman RL, et al. Assessment of health literacy and numeracy among Spanish-Speaking parents of young children: validation of the Spanish Parental Health Literacy Activities Test (PHLAT Spanish) Acad Pediatr. 2012;12:68–74. doi: 10.1016/j.acap.2011.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jolly BT, Scott JL, Sanford SM. Simplification of emergency department discharge instructions improves patient comprehension. Ann Emerg Med. 1995;26:443–446. doi: 10.1016/s0196-0644(95)70112-5. [DOI] [PubMed] [Google Scholar]
- 33.Johnson A, Sandford J, Tyndall J. Written and verbal information versus verbal information only for patients being discharged from acute hospital settings to home. Cochrane Database Syst Rev. 2003:CD003716. doi: 10.1002/14651858.CD003716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Paasche-Orlow MK, Riekert KA, Bilderback A, et al. Tailored education may reduce health literacy disparities in asthma self-management. Am J Respir Crit Care Med. 2005;172:980–986. doi: 10.1164/rccm.200409-1291OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hussain-Rizvi A, Kunkov S, Crain EF. Does parental involvement in pediatric emergency department asthma treatment affect home management? J Asthma. 2009;46:792–795. [PubMed] [Google Scholar]
- 36.Patel PB, Vinson DR. Physician e-mail and telephone contact after emergency department visit improves patient satisfaction: a crossover trial. Ann Emerg Med. 2013;61:631–637. doi: 10.1016/j.annemergmed.2012.12.005. [DOI] [PubMed] [Google Scholar]
- 37.O'Neill K, Silvestri A, McDaniel-Yakscoe N. A pediatric emergency department follow-up system: completing the cycle of care. Pediatr Emerg Care. 2001;17:392–395. doi: 10.1097/00006565-200110000-00018. [DOI] [PubMed] [Google Scholar]
- 38.Khan MS, O'Meara M, Stevermuer TL, Henry RL. Randomized controlled trial of asthma education after discharge from an emergency department. J Paediatr Child Health. 2004;40:674–677. doi: 10.1111/j.1440-1754.2004.00490.x. [DOI] [PubMed] [Google Scholar]
- 39.Racine AD, Alderman EM, Avner JR. Effect of telephone calls from primary care practices on follow-up visits after pediatric emergency department visits: evidence from the Pediatric Emergency Department Links to Primary Care (PEDLPC) randomized controlled trial. Arch Pediatr Adolesc Med. 2009;163:505–511. doi: 10.1001/archpediatrics.2009.45. [DOI] [PubMed] [Google Scholar]
- 40.Goldman RD, Wei JJ, Cheyne J, et al. Impact of follow-up calls from the pediatric emergency department on return visits within 72 hours: a randomized controlled trial. Pediatr Emerg Care. 2014;30:613–616. doi: 10.1097/PEC.0000000000000207. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.