Abstract
tert-butylhydroquinone (tBHQ), an Nrf2 signaling pathway inducer that is widely used as a food additive in the U.S., prevents oxidative stress-induced cytotoxicity in neurons. This study assesses the effects of tBHQ on ischemic stroke outcomes in mice. We measured infarct size, neurological deficits, and brain volume after tBHQ treatments in murine permanent middle cerebral artery occlusion (pMCAO) model in vivo. Further, we evaluated the regulation of tBHQ on mitochondrial function in cerebrovascular endothelial cells in vitro, which is critical to the blood–brain barrier (BBB) permeability. Our results demonstrated that tBHQ increased post-stroke mortality and worsened stroke outcomes. Mitochondrial function was suppressed by tBHQ treatment of cerebrovascular endothelial cells, and this suppression was potentiated by co-treatment with lipopolysaccharide (LPS), the bacterial mimic. These data indicate that tBHQ-exacerbated stroke damage might due to the compromised BBB permeability in permanent stroke.
Keywords: Nrf2, Tert-butylhydroquinone, stroke
Introduction
As reported by the World Health Organization, over 15 million people a year suffer from stroke worldwide [1]. In the United States, stroke is the fifth leading cause of mortality and the leading cause of long-term disability [2]. Ischemic stroke accounts for approximately 80–85% of all cases, which is caused by the disruption of cerebral blood flow and lack of oxygen and glucose to the affected area due to a clot. Currently, the only Food and Drug Administration approved treatment for ischemic stroke is tissue plasminogen activator (tPA), which is a thrombolytic therapy to break up the clot. Properly titrated use of tPA improves clinical outcomes. However, less than 5% of patients receive tPA [3]. Overall, the current therapeutic strategy for ischemic stroke is not optimal.
Brain injury following cerebral ischemia develops from a complex series of pathophysiological events that evolve in time and space [4]. Energy failure leads to intracellular ionic imbalance, excessive production of oxygen radicals and impairment of mitochondrial function in neurons [5, 6]. A considerable body of evidences suggest that excessive production of reactive oxygen species (ROS) is a fundamental contributor to brain damage in ischemic stroke [7]. Even though ROS are short-living compounds, they can initiate complex chain reactions. ROS directly react with a multitude of biological target molecules, such as proteins, lipids and DNA, to produce a wide range of intracellular damage [8]. All of oxidative modified intracellular molecules exert a fundamental impairment of biological function. Not only might ROS induce accidental damage to molecules, but also actively modulate critical subcellular organelle functions, such as endoplasmic reticulum stress and mitochondrial dysfunction [9]. Many therapeutic strategies have targeted antioxidants to promote neuroprotection during ischemia [10]. However, to date, no antioxidative approaches have been approved in the United States. We should note that most of drug candidates tested in the clinical trials of stroke are free radical scavengers that directly react with ROS. This strategy can rapidly eliminate ROS, but it fails to improve endogenous antioxidative status. Overall, the current antioxidative strategy for ischemic stroke therapy is not optimal.
The nuclear factor E2-related factor 2 (Nrf2)-antioxidant response element (ARE) signaling pathway controls a battery of antioxidative gene expression. Activation of Nrf2-ARE signaling pathway improves intracellular antioxidant capacity and is critical for the detoxification and elimination of oxygen-derived free radicals. Under normal condition, Nrf2 binding with Kelch-like ECH-associated protein 1 (Keap1), a sensor of intracellular redox status, is inactivated [11]. Upon the stimulation of oxidative stress, Nrf2 dissociates with Keap1, translocates into the nucleus and further activates the transcription of ARE-driven genes [12]. ARE-driven genes are involved in a battery of antioxidant and phase II enzymes production [13]. One well-characterized Nrf2 inducer is tert-butylhydroquinone (tBHQ). In addition, tBHQ is an antioxidant, used as a food additive for unsaturated vegetable oils as well as many other edible animal fats. The maximal content of a food containing the additive is 0.02% of the oil or fat content [14]. As an antioxidant, tBHQ can boost intracellular antioxidative capacity immediately after administration, which directly reacts with ROS and prevents oxidative damage. Activation of Nrf2-ARE signaling pathway results in an increase in a wide range of intracellular antioxidant and antioxidative enzyme levels. This can fundamentally reestablish intracellular redox hemostasis. The dual antioxidative activities make tBHQ as a valuable candidate for the treatment of oxidative stress-induced neurodegeneration. Our previous study has shown that tBHQ exerts protection against oxidative stress-induced cytotoxicity in neurons though preserving mitochondrial function [15]. A published study reported that pretreatment with tBHQ reduced cortical damage and improved functional recovery up to 1 month after ischemia-reperfusion in rats [16].
We investigated the effect of tBHQ on a murine permanent middle cerebral artery occlusion (pMCAO) model, a severe ischemic damage. Surprisingly, tBHQ induced a significant increase of mortality and failed to protect stroke outcomes compared to control. Further, we demonstrated that tBHQ significantly increased brain volume in murine pMCAO model. Finally, we found that tBHQ inhibited mitochondrial function of cerebrovascular endothelial cells, which is critical to the blood–brain barrier (BBB) permeability [17]. BBB disruption can lead to edema and further aggravate the ischemic damage [18]. These data suggest that tBHQ exposure leads to mitochondrial suppression-mediated BBB disruption, which exacerbates acute stroke outcomes.
Materials and Methods
Animals and experimental treatment
All procedures were conducted according to the criteria approved by the Institutional Animal Care and Use Committees at the West Virginia University (WVU). C57/BL6J male mice (3–4 months old, 25–30 g; Jackson Laboratories) were used for all studies. tBHQ (Sigma, Saint Louis, MO) solution was prepared at 0.116, 0.668 and 6.68 mg/ml in vehicle (1% DMSO in saline). Intraperitoneal injection of tBHQ (0.582, 3.34 or 33.4 mg/kg) was performed every 12 h, starting at 24h before pMCAO. An equal volume of saline was administered to control mice. To assign pretreatments of mice, we numbered the animals and applied a simple randomization by using excel-generated random numbers. The experimenters were blinded to the pretreatments and data analysis.
Permanent middle carotid artery occlusion
All surgical anesthesia was induced with 4–5% isoflurane until the animal showed no response to a toe pinch and was maintained with 1–2% isoflurane via face-mask in O2-enriched air. We performed focal cerebral ischemia for 24 hr by occlusion of the right middle cerebral artery with a 6.0 monofilament suture (Doccol, Sharon, MA). We used laser Doppler flowmetry (Moor Instruments, United Kingdom) to detect regional cerebral blood flow and confirmed a successful occlusion (>70% decrease in flow). Rectal temperature was maintained at 37±0.5°C with a warm blanket (Stoelting Co, IL USA) during surgery.
Neurological Deficits
Neurological deficit was determined daily before and after tMCAO according to a 0- to 5-point scale neurological score system as published [17]. 0 = no neurological dysfunction; 1 = failure to extend left forelimb fully when lifted by tail; 2 = circling to the contralateral side; 3 = falling to the left; 4 = no spontaneous walk or in a comatose state; 5 = death. The experimenters were blinded to group allocations.
Exclusion Criteria for the Successful Animal Experiments
The following criteria for successful pMCAO were observed for all animals. (1) Regional cerebral blood flow decreased <70% during occlusion as detected by laser Doppler flowmetry. (2) Surgery time was never over 30 minutes. (3) Neurological deficits were observed 3 hours after MCAO (neurological score 0). (4) Infarction in the MCA territory (striatum) on 2,3,5-triphenyltetrazolium chloride (TTC) staining was seen. (5) There was no subarachnoid hemorrhage on postmortem examination. (6) There was no substantial ambient temperature change (22–24 °C) in the animal facility. Animals that died before the planned time of assessments were postmortem examined for subarachnoid hemorrhage, and the mortality was recorded.
Analysis of Infarct Size and Brain Volume
Mice were euthanized with isofluorane. We removed the brains and cut 2-mm coronal sections with a mouse brain matrix. We stained the sections with 2% TTC (Sigma, Saint Louis, MO) in phosphate buffer solution at 37°C for 30 minutes then fixed the tissue in 10% formalin phosphate buffer for digital photograph. We analyzed the digitized images of each brain section using a computerized image analysis software (ImageJ, National Institutes of Health) in a blinded manner. The infarction volume was expressed as a percentage of contralateral cortex, striatum, and total hemisphere. Brain volume for ipsilateral hemisphere (right) and contralateral hemisphere (left) was calculated.
Cell Culture
The bEnd.3 cell line (CRL-2299 from ATCC, Manassas, VA) was originally derived from mouse brain cortex endothelial cells and confirmed by the observed major phenotypic features of the BBB [17]. Passages 25 to 30 were used in the study. The bEnd.3 cells were routinely grown in high glucose Dulbecco modified Eagle medium (ATCC) supplemented with 10% FCS and 1% penicillin/streptomycin (Hyclone, South Logan, UT) at 37°C in 5% CO2 humid atmosphere.
Oxygen Consumption
Oxygen consumption rate was measured at 37°C using an XF96e extracellular analyzer (Seahorse Bioscience, North Billerica, MA) according to the manufacturer’s instructions. Briefly, the bEnd.3 cells were seeded into Seahorse Bioscience XF96e cell culture plates (16,000 cells/well) in 80-μL medium and allowed to adhere and grow overnight. After respective exposures, the media was exchanged 1 hr prior to the assay with XF assay medium (Seahorse Bioscience, North Billerica, MA). Oligomycin (1 μM), carbonilcyanide p-triflouromethoxyphenylhydrazone (FCCP, 0.5 μM) and antimycin (1 μM) and rotenone (1 μM) (Sigma) were diluted into XFe96 media and loaded into the accompanying cartridge. Injections of the components into the wells occurred at the time points specified. Oxygen consumption rate (OCR) was monitored using a Seahorse Bioscience XFe96 Extracellular Flux Analyzer. To calculate basal respiration, the measurement prior to oligomycin addition was subtracted from OCR measurement after rotenone and antimycin injection. ATP production was measured using the third OCR measurement prior to addition of oligomycin subtracted from OCR after oligomycin injection. Maximal respiration was calculated using the maximal OCR after FCCP injection subtracted from OCR after rotenone and antimycin injection. To calculate spare capacity, the maximal OCR after FCCP injection was subtracted from the measurement prior to addition of oligomycin.
Statistical analysis
The data were shown as means ± SD. Statistical analyses were performed using one-way ANOVA with Tukey’s post hoc tests for multiple comparisons or Chi-Square test for mortality rates. GraphPad PRISM 5.0 was used for statistical analyses.
Results
Pre-ischemic exposure to tBHQ failed to protect mice from pMCAO and significantly increased the mortality
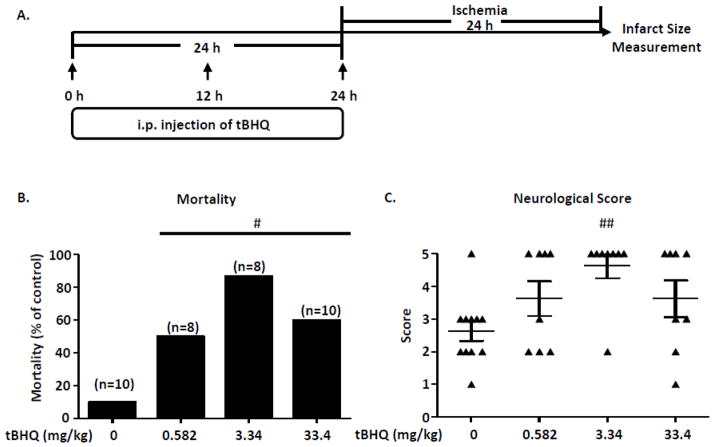
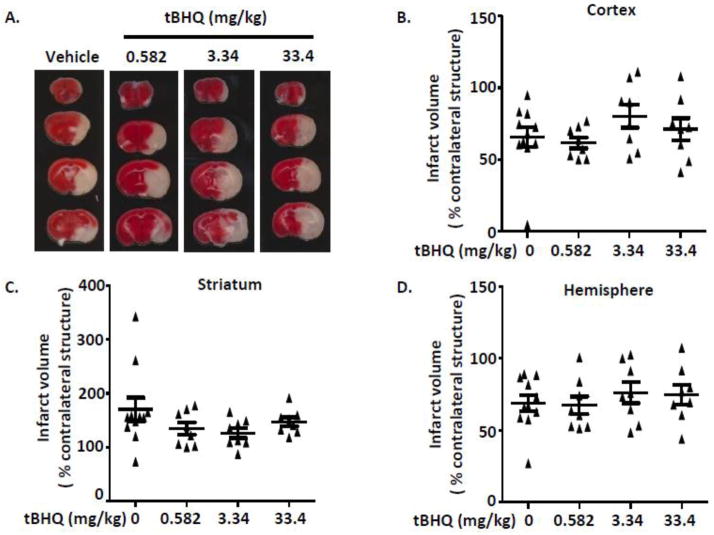
As shown in Figure 1A, we performed three i.p. injections of tBHQ with a 12 hr interval starting at 24 hr before pMCAO. Following a 24 hr of pMCAO, neurological score and brain infarct size were evaluated. Three dosages of tBHQ (0.582, 3.34 and 33.4 mg/kg) were included in this study. Based on the dosage published in an animal study [16], ten mice were injected with tBHQ at dose of 33.4 mg/kg. Two mice died before pMCAO surgery and four mice died during ischemic stroke (Figure 1B). According to our previous study in vitro, this dosage induced cytotoxicity in neurons [15]. Therefore, we reduced dosage to 3.34 mg/kg, a protective concentration against oxidative toxicity in the neuronal cell line [15]. However, the mortality remained high. Further, we lowered the dose to 0.582 mg/kg, which has been shown to be protective in primary cortical neurons [15]. However, the mortality of tBHQ treatment group was still higher than control group (Figure 1B). For the neurological assessment, all tBHQ treatment group demonstrated a severer damage of motor function compared to vehicle group (Figure 1C). Overall, these data indicate that pre-ischemic treatment with tBHQ significantly increases the mortality of pMCAO in mice and worsens neurological score. After a 24hr of occlusion, we measured brain infarction by TTC staining. Representative stained coronal sections used to analyze brain infarction of mice. As shown in Figure 2, there was no significant difference of the infarct sizes in tBHQ treatment groups compared to vehicle.
Figure 1. Pre-ischemic treatment with tBHQ increases mortality and does not improve neurological score in the murine pMCAO model.
(A). Schematic diagram summarizing the injection and stroke timeline. The short arrows represent time points of tBHQ injection. (B). Mortality after 24 hr pMCAO. Vehicle, n=11, tBHQ 0.582 mg/kg, n=8, tBHQ 3.34 mg/kg, n=8, tBHQ 33.4 mg/kg, n=10. (C). Neurological score after pMCAO. Data are expressed as mean ± SD. Vehicle, n=11, tBHQ 0.582 mg/kg, n=8, tBHQ 3.34 mg/kg, n=8, tBHQ 33.4 mg/kg, n=8. One-way ANOVA followed by post hoc Tukey test and Chi-Square test were used for multiple group comparison. #P < 0.05, ##P < 0.01 compared to vehicle.
Figure 2. Pre-ischemic treatment of tBHQ has no effect on infarct size compared to vehicle group.
(A). Infarct volumes were measured at 24 hr after ischemia induction. Representative triphenyltetrazolium chloride–stained coronal sections used to analyze infarction of mice treated with vehicle vs. tBHQ. Mice treated with tBHQ had a similar infarct volume when compared to vehicle group in cortex (B), striatum (C), and total hemisphere (D). Vehicle, n=11, tBHQ 0.582 mg/kg, n=8, tBHQ 3.34 mg/kg, n=8, tBHQ 33.4 mg/kg, n=8. Mean ± SD; One-way ANOVA followed by post hoc Tukey test was used for multiple group comparison.
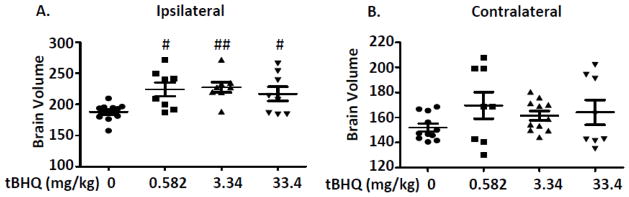
tBHQ increased brain volume in murine pMCAO model
Disruption of the BBB contributes to the formation of edema and impairs survival from stroke [17, 19]. To investigate if tBHQ induces BBB damage, we calculated brain volume after tBHQ exposure in murine pMCAO model. tBHQ exposure induced a significant increase in the ipsilateral brain volume (Figure 3A), and there was no significant change in the contralateral brain volume (Figure 3B). The data indicate that the increased brain volume in the ipsilateral hemisphere might be caused by the BBB disruption, which leads to the exudation of plasma proteins, fluid, and white blood cells into the brain tissue.
Figure 3. Pre-ischemic treatment of tBHQ increases brain volume compared to vehicle group.
Ipsilateral (A) and contralateral (B) brain volumes were measured at 24 hr after ischemia induction. Representative coronal sections were used to analyze brain volume of mice treated with vehicle vs tBHQ. Vehicle, n=11, tBHQ 0.582 mg/kg, n=8, tBHQ 3.34 mg/kg, n=8, tBHQ 33.4 mg/kg, n=8. Mean ± SD; One-way ANOVA followed by post hoc Tukey test was used for multiple group comparison. #P < 0.05, ##P < 0.01 compared to vehicle.
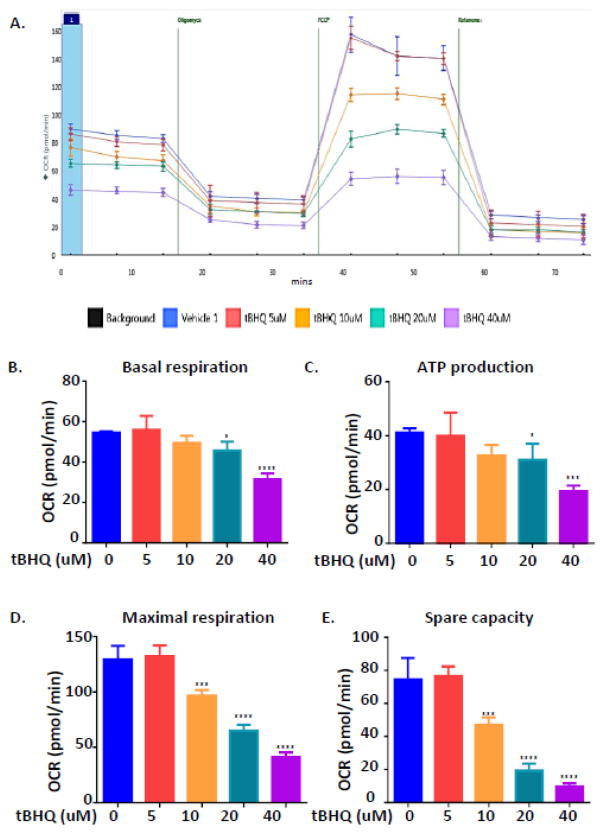
tBHQ suppressed mitochondrial respiration of brain cortex endothelial cells
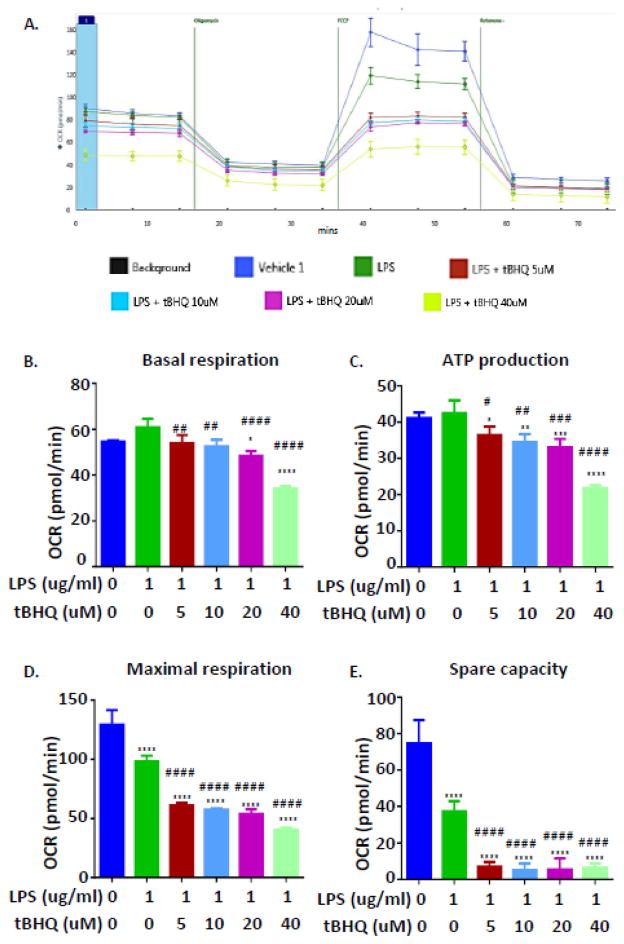
Even though tBHQ has been reported to be protective against oxidative stress-induced cell death in neurons, our data demonstrated that tBHQ induce a toxicity in murine pMCAO model. Other than neuronal cell death, cerebrovascular system also participates in ischemic brain injury during stroke. Our published study reported that inhibition of mitochondrial function disrupted the BBB and further worsened stroke outcomes [17]. Next, we evaluated the effect of tBHQ on mitochondrial function in a brain cortex endothelial cell line, bEnd.3 cells. After a 24 hr exposure to tBHQ (5–40 uM), a bioenergetic assay was used to examine cellular energetic oxygen consumption rate (Figure 4A). As shown in Figure 4B and C, basal oxygen consumption rate and ATP production were reduced at high concentration of tBHQ treatment groups (20 and 40 uM). Beginning at the concentration of 10 uM, tBHQ induced a dose-dependent suppression on maximal respiration and spare capacity (Figure 4D and E). We noted that an exposure of 40 uM tBHQ almost fully abolished mitochondrial spare capacity and reduced maximal respiration to 30% of control.
Figure 4. tBHQ suppresses mitochondrial respiration in the bEnd.3 cell line.
After 24-hr treatment with various concentration of tBHQ, OCR was recorded by a Seahorse XFe96 flux analyzer (n=8). (A) OCR recording at baseline and subsequent treatment of 1μM oligomycin, 0.5 μM FCCP, and a 1 μM rotenone and antimycin mixture. Basal respiration (B), ATP production (C), maximum respiration (D) and spare capacity (E) were calculated. All experiments were repeated three times and the results indicate the mean ± SEM. *P < 0.05, ***P < 0.001, ****P < 0.00001 compared to control. (One-way ANOVA, Tukey’s test).
tBHQ exacerbated LPS-induced mitochondrial dysfunction
Lipopolysaccharide (LPS), a bacterial infection mimic, leads to the mitochondrial dysfunction-induced BBB disruption and further worsens stroke outcomes [17]. To mimic our in vivo study, we evaluated mitochondrial respiration after co-treatment of tBHQ and LPS challenge for 24 hr (Figure 4A). LPS (1 ug/ml) alone resulted in a decrease in maximal respiration and spare capacity without a significant change of basal respiration and ATP production (Figure 5B, C, D and E). Surprisingly, co-treatment with tBHQ induced a significant inhibition of mitochondrial function, including basal respiration and ATP production. At a concentration of 5 uM, tBHQ treatment alone did not inhibit mitochondrial respiration (Figure 4); while, a substantial mitochondrial inhibition was observed in the presence of LPS. Overall, we conclude that tBHQ reduces mitochondrial respiration in cerebrovascular endothelial cells, and this inhibition is potentiated by LPS challenge.
Figure 5. tBHQ exacerbates LPS-induced mitochondrial inhibition in the bEnd.3 cell line.
(A) Bioenergetics functional assay exposed to LPS and various concentration of tBHQ compared with vehicle control for 24 hr. Basal respiration (B), ATP production (C), maximal respiration (D), and spare capacity (E) were calculated from the assay and presented. Mean ± SD; n=4 per group; One-way ANOVA followed by post hoc Tukey test was used for data analysis. *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.00001 compared to control. #P < 0.05, ##P < 0.01, ###P < 0.001, ####P < 0.00001 compared to LPS treatment.
Discussion
The present study demonstrates that pre-ischemic exposure to tBHQ significantly increases the mortality from pMCAO in mice. tBHQ profoundly compromises mitochondrial respiration of brain cortex endothelial cells in vitro and leads to increased brain volume in murine pMCAO model. The present study is the first to report an adverse effect of tBHQ-enhanced mortality from permanent stroke.
The increase in oxygen-derived free radicals generation has been observed during cerebral ischemia. In focal cerebral ischemia, the production of ROS mainly occurs in the special ischemic brain regions where the local oxygen tension is partially preserved by residual collateral flow, such as in the ischemic penumbra [20]. Free radicals plays a key role in the pathophysiologic cascade leading to ischemic tissue damage [21, 22]. One published study reported that administration of tBHQ before stroke improves sensorimotor and histological outcomes in transient ischemic mouse model [16], while, our study demonstrated a significant toxicity of tBHQ in pMCAO model. It is important to note that the formation of oxygen-free radicals in the acute phase of pMCAO is different with that occurring in tMCAO. A burst-like pattern of ROS accumulation is generated after reperfusion, while a steady accumulation of ROS is induced during permanent occlusion [23]. Our previous data showed that tBHQ induces a rapid activation of Nrf2-ARE signaling pathway. However, activation of Nrf2-ARE signaling pathway is diminished with prolonged exposure of tBHQ [15]. A persistent accumulation of ROS during permanent occlusion may exceed the effective time window of tBHQ. This provides a potential explanation why tBHQ exerts a quite different effect in pMCAO versus tMCAO model. Since the patterns of ROS generation are diversiform depending on ischemic conditions, a universal intervention of antioxidants may be too simplistic. Therefore, the complexity of pathophysiological events that involved in ischemic brain injury need to be considered for antioxidative strategy design.
Free radicals are typically generated during ATP production in mitochondria. As the primary site of ROS generation, the steady state concentration of ROS in the mitochondria is much higher than other subcellular component. This makes mitochondria a vulnerable target of oxidative damage. ROS can induce the modification of subunits in the mitochondrial electron transport chain, which results in an increased propensity to generate free radicals. Further, it overwhelms the mitochondria’s ability to protect itself from endogenous oxidative stress and triggers mitochondrial-mediated cell apoptosis. Therefore, oxidative stress-induced mitochondrial dysfunction is one of the major pathogenic mechanisms of neurodegeneration [24]. Our previous study elucidated that tBHQ improves mitochondrial antioxidative capacity by up-regulating the expression of SOD2 and HO-1, which further prevents oxidative stress-induced mitochondrial dysfunction and cell death [15]. These promising neuroprotective activities led us to investigate the effect of tBHQ on ischemic stroke. Other than neuronal cells, mitochondrial dysfunction is also known to induce a detrimental effect on the cerebrovascular system. Our recent work have demonstrated that a compromised mitochondrial function in cerebrovascular endothelial cells robustly disrupts BBB both in vitro and in vivo, and further exacerbates stroke outcomes [17]. Even though a slight decrease in mitochondrial respiration is induced by tBHQ in neuronal cells, tBHQ still exerts a profound protection against oxidative stress-induced neuronal cell death [15]. We speculate that preventing the accumulation of ROS by tBHQ is enough to rescue neurons from glutamate-induced oxidative damage in neurons. On the other hand, tBHQ suppresses mitochondrial respiration in endothelial cells and might lead to the disruption of BBB. tBHQ significantly suppresses mitochondrial function of brain endothelial cells (Figure 4). Our previous study showed that LPS disrupted BBB and exacerbated stroke outcomes due to the compromised mitochondrial function of cerebrovascular endothelial cells [17]. In the presence of LPS, tBHQ induces a more potent inhibition of mitochondrial function (Figure 5). This indicates that tBHQ-induced mitochondrial suppression can be potentiated in the present of other mitochondrial toxins. Therefore, the detrimental effect on cerebrovascular effect might cover the beneficial effect of tBHQ on neurons but result in the toxicity of tBHQ in permanent stroke.
There are several limitations of this study. First, the assessment of the effects of tBHQ on endothelial cells was conducted in vitro, using an endothelial cell line. Our only evidence that tBHQ may affect endothelial structural function in vivo, is the demand increase in ipsilateral brain volume to stroke. We do not have direct evidence for a tBHQ effect on brain endothelial cells in vivo. Further studies need to be carried out to investigate if tBHQ also induces adverse effects on other cell types in the central nervous system.
BBB is a highly specialized vascular interface that maintains homeostasis in brain by separating the blood compartment from the central nervous system. Disruption of BBB not only disrupts the normal central nervous system entry route of critical nutrients, but also allows entry of unwanted toxins into brain [25]. BBB disruption leads to influx of toxic substances, inflammation and vasogenic edema after stroke. Brain edema aggravates the ischemic process by its volumetric effect, through a compression of microcirculation, an increase of intracranial pressure, and a dislocation of parts of the brain [26]. The disruption of BBB is detectable in animals after 4.5–6 hr of pMCAO, while the hemispheric lesion volume increases progressively during permanent cerebral ischemia [27]. This indicates that the increase in BBB permeability occurs in a relatively early phase of ischemic stroke and contributes to the further brain damage. Although tBHQ is known to increase the expression of many antioxidative enzymes, a rapidly impairment of BBB function induced by tBHQ during ischemia might override its antioxidative activity.
tBHQ is a United States Food and Drug Administration-approved food additive which is commonly used to preserve unsaturated vegetables and animal fats. As such, it is consumed daily by most Americans and is considered safe for consumption [14, 28]. The maximal content of a food containing the additive would be equivalent on average to 0.4 mg/kg (body weight) for an adult [25]. The half-life of elimination of tBHQ in human is about 20–24 hours [26]. This indicates higher concentration of tBHQ might accumulated after repeatedly consumption of food containing tBHQ. Since tBHQ can be consumed daily, it might exert a harmful effect on cerebrovascular system and exacerbate BBB disruption when stroke occurs. Although it is unknown if tBHQ affects other organs as well as diverse cell types, our study raises a safety concern for tBHQ as a food additive or a potential therapeutic treatment for stroke.
Highlights.
tBHQ is widely used as a food additive in the U.S.
tBHQ increases mortality and worsens stroke outcomes in murine experimental stroke.
Mitochondrial function is suppressed by tBHQ in cerebrovascular endothelial cells.
tBHQ-induced mitochondrial suppression is potentiated by co-treatment with LPS.
Acknowledgments
Sources of Funding
This work was supported by National Institutes of Health [P01 AG022550, P01 AG027956 and P20 GM109098], National Institutes of Health/National Institute of General Medical Sciences Award Number [U54GM104942].
List of Abbreviations
- ARE
antioxidant response element
- BBB
blood–brain barrier
- FCCP
carbonilcyanide p-triflouromethoxyphenylhydrazone
- Keap1
kelch-like ECH-associated protein 1
- Nrf2
nuclear factor E2-related factor 2
- OCR
oxygen consumption rate
- pMCAO
permanent middle cerebral artery occlusion
- ROS
reactive oxygen species
- tBHQ
tert-butylhydroquinone
- tMCAO
transient middle cerebral artery occlusion
- TTC
2,3,5-triphenyltetrazolium chloride
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Weir NU, Dennis MS. Meeting the challenge of stroke. Scott Med J. 1997;42:145–147. doi: 10.1177/003693309704200510. [DOI] [PubMed] [Google Scholar]
- 2.Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Makuc DM, Marcus GM, Marelli A, Matchar DB, Moy CS, Mozaffarian D, Mussolino ME, Nichol G, Paynter NP, Soliman EZ, Sorlie PD, Sotoodehnia N, Turan TN, Virani SS, Wong ND, Woo D, Turner MB. American Heart Association Statistics Committee and Stroke Statistics Subcommittee, Executive summary: heart disease and stroke statistics--2012 update: a report from the American Heart Association. Circulation. 2012;125:188–197. doi: 10.1161/CIR.0b013e3182456d46. [DOI] [PubMed] [Google Scholar]
- 3.Miller DJ, Simpson JR, Silver B. Safety of thrombolysis in acute ischemic stroke: a review of complications, risk factors, and newer technologies. Neurohospitalist. 2011;1:138–147. doi: 10.1177/1941875211408731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.White BC, Sullivan JM, DeGracia DJ, O’Neil BJ, Neumar RW, Grossman LI, Rafols JA, Krause GS. Brain ischemia and reperfusion: molecular mechanisms of neuronal injury. J Neurol Sci. 2000;179:1–33. doi: 10.1016/s0022-510x(00)00386-5. [DOI] [PubMed] [Google Scholar]
- 5.Dirnagl U, Iadecola C, Moskowitz MA. Pathobiology of ischaemic stroke: an integrated view. Trends Neurosci. 1999;22:391–397. doi: 10.1016/s0166-2236(99)01401-0. [DOI] [PubMed] [Google Scholar]
- 6.Lee JM, Zipfel GJ, Choi DW. The changing landscape of ischaemic brain injury mechanisms. Nature. 1999;399:A7–14. doi: 10.1038/399a007. [DOI] [PubMed] [Google Scholar]
- 7.Manzanero S, Santro T, Arumugam TV. Neuronal oxidative stress in acute ischemic stroke: Sources and contribution to cell injury. Neurochem Int. 2013;62:712–718. doi: 10.1016/j.neuint.2012.11.009. [DOI] [PubMed] [Google Scholar]
- 8.Imlay JA. Pathways of oxidative damage. Annu Rev Microbiol. 2003;57:395–418. doi: 10.1146/annurev.micro.57.030502.090938. [DOI] [PubMed] [Google Scholar]
- 9.Jacobson MD. Reactive oxygen species and programmed cell death. Trends Biochem Sci. 1996;21:83–86. [PubMed] [Google Scholar]
- 10.Gilgun-Sherki Y, Rosenbaum Z, Melamed E, Offen D. Antioxidant therapy in acute central nervous system injury: current state. Pharmacol Rev. 2002;54:271–284. doi: 10.1124/pr.54.2.271. [DOI] [PubMed] [Google Scholar]
- 11.Itoh K, Wakabayashi N, Katoh Y, Ishii T, Igarashi K, Engel JD, Yamamoto M. Keap1 represses nuclear activation of antioxidant responsive elements by Nrf2 through binding to the amino-terminal Neh2 domain. Genes Dev. 1999;13:76–86. doi: 10.1101/gad.13.1.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Apopa PL, He X, Ma Q. Phosphorylation of Nrf2 in the transcription activation domain by casein kinase 2 (CK2) is critical for the nuclear translocation and transcription activation function of Nrf2 in IMR-32 neuroblastoma cells. J Biochem Mol Toxicol. 2008;22:63–76. doi: 10.1002/jbt.20212. [DOI] [PubMed] [Google Scholar]
- 13.Jaiswal AK. Nrf2 signaling in coordinated activation of antioxidant gene expression. Free Radical Biology and Medicine. 2004;36:1199–1207. doi: 10.1016/j.freeradbiomed.2004.02.074. [DOI] [PubMed] [Google Scholar]
- 14.National Toxicology Program. NTP Toxicology and Carcinogenesis Studies of t-Butylhydroquinone (CAS No. 1948-33-0) in F344/N Rats and B6C3F(1) Mice (Feed Studies) Natl Toxicol Program Tech Rep Ser. 1997;459:1–326. [PubMed] [Google Scholar]
- 15.Sun J, Ren X, Simpkins JW. Sequential Upregulation of Superoxide Dismutase 2 and Heme Oxygenase 1 by tert-Butylhydroquinone Protects Mitochondria during Oxidative Stress. Mol Pharmacol. 2015;88:437–449. doi: 10.1124/mol.115.098269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shih AY, Li P, Murphy TH. A small-molecule-inducible Nrf2-mediated antioxidant response provides effective prophylaxis against cerebral ischemia in vivo. J Neurosci. 2005;25:10321–10335. doi: 10.1523/JNEUROSCI.4014-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Doll DN, Hu H, Sun J, Lewis SE, Simpkins JW, Ren X. Mitochondrial crisis in cerebrovascular endothelial cells opens the blood-brain barrier. Stroke. 2015;46:1681–1689. doi: 10.1161/STROKEAHA.115.009099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kamada H, Yu F, Nito C, Chan PH. Influence of hyperglycemia on oxidative stress and matrix metalloproteinase-9 activation after focal cerebral ischemia/reperfusion in rats: relation to blood-brain barrier dysfunction. Stroke. 2007;38:1044–1049. doi: 10.1161/01.STR.0000258041.75739.cb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Denes A, Ferenczi S, Kovacs KJ. Systemic inflammatory challenges compromise survival after experimental stroke via augmenting brain inflammation, blood-brain barrier damage and brain oedema independently of infarct size. J Neuroinflammation. 2011;8:164-2094-8-164. doi: 10.1186/1742-2094-8-164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Olmez I, Ozyurt H. Reactive oxygen species and ischemic cerebrovascular disease. Neurochem Int. 2012;60:208–212. doi: 10.1016/j.neuint.2011.11.009. [DOI] [PubMed] [Google Scholar]
- 21.Chen H, Yoshioka H, Kim GS, Jung JE, Okami N, Sakata H, Maier CM, Narasimhan P, Goeders CE, Chan PH. Oxidative stress in ischemic brain damage: mechanisms of cell death and potential molecular targets for neuroprotection. Antioxid Redox Signal. 2011;14:1505–1517. doi: 10.1089/ars.2010.3576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Niizuma K, Endo H, Chan PH. Oxidative stress and mitochondrial dysfunction as determinants of ischemic neuronal death and survival. J Neurochem. 2009;109(Suppl 1):133–138. doi: 10.1111/j.1471-4159.2009.05897.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Peters O, Back T, Lindauer U, Busch C, Megow D, Dreier J, Dirnagl U. Increased formation of reactive oxygen species after permanent and reversible middle cerebral artery occlusion in the rat. J Cereb Blood Flow Metab. 1998;18:196–205. doi: 10.1097/00004647-199802000-00011. [DOI] [PubMed] [Google Scholar]
- 24.Melov S. Mitochondrial oxidative stress. Physiologic consequences and potential for a role in aging. Ann N Y Acad Sci. 2000;908:219–225. doi: 10.1111/j.1749-6632.2000.tb06649.x. [DOI] [PubMed] [Google Scholar]
- 25.Rubin LL, Staddon JM. The cell biology of the blood-brain barrier. Annu Rev Neurosci. 1999;22:11–28. doi: 10.1146/annurev.neuro.22.1.11. [DOI] [PubMed] [Google Scholar]
- 26.Yang Y, Rosenberg GA. Blood-brain barrier breakdown in acute and chronic cerebrovascular disease. Stroke. 2011;42:3323–3328. doi: 10.1161/STROKEAHA.110.608257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kastrup A, Engelhorn T, Beaulieu C, de Crespigny A, Moseley ME. Dynamics of cerebral injury, perfusion, and blood-brain barrier changes after temporary and permanent middle cerebral artery occlusion in the rat. J Neurol Sci. 1999;166:91–99. doi: 10.1016/s0022-510x(99)00121-5. [DOI] [PubMed] [Google Scholar]
- 28.Evaluation of certain food additives and contaminants. Forty-ninth report of the Joint FAO/WHO Expert Committee on Food Additives. World Health Organ Tech Rep Ser. 1999;884:i–viii. 1–96. [PubMed] [Google Scholar]