Abstract
Objective
To determine whether a web-based, interactive, breastfeeding monitoring system increased breastfeeding duration, exclusivity, and intensity as primary outcomes and decreased symptoms of postpartum depression as a secondary outcome.
Methods
A two arm randomized controlled trial took place in three Midwestern hospitals. Postpartum women were randomly assigned to the control or intervention group. Women in the control group (n=57) followed the standard hospital protocol, while women in the intervention group (n= 49) were given access to an online, interactive, breastfeeding monitoring system and prompted to record breastfeeding and infant output data for 30 days. A follow-up online survey was sent to both groups at 1, 2, and 3 months to assess breastfeeding outcomes and postpartum depression.
Results
For mothers and infants, there were no significant differences in demographics between groups. No significant differences in breastfeeding outcomes were found between groups at discharge (p = 0.707). A significant difference in breastfeeding outcomes was found between groups at 1, 2, and 3 months (p = 0.027, p = 0.000 and p = 0.002). Members of the intervention group had higher exclusive breastfeeding rates at 1, 2, and 3 months. By the end of the third month, 84% of the intervention group was breastfeeding compared to 66% in the control group. Postpartum depression symptom scores decreased for both groups at 1, 2, and 3 months (4.9±3.9, 4.3±4.9, and 3.2±3.9 for control and 4.7±4.5, 3.0±3.4, and 2.8±3.6 for intervention). However, there was no significant difference between groups at 1, 2, and 3 months (p= 0.389, 0.170, and 0.920) for depression.
Conclusion
The web-based interactive breastfeeding monitoring system may be a promising intervention to improve breastfeeding duration, exclusivity, and intensity.
Keywords: Web-based interactive monitoring, Breastfeeding, e-health, Breastfeeding support
The benefits of breastfeeding and the risks associated with formula feeding are well known. Infants who are not breastfed are at increased risk for infections that include otitis media and diarrhea, elevated risks of childhood obesity, type 1 and type 2 diabetes, leukemia, and sudden infant death syndrome (Dieterich, Felice, O'Sullivan, & Rasmussen, 2013; Hauck, Thompson, Tanabe, Moon & Vennemann, 2011; Horta et al., 2015; Ip, et al., 2009; Johnston, Landers, Noble, Szucs, & Viehmann,2012; Stuebe, 2009; Yan, Liu, Zhu, Huang, &Wang, 2014). Exclusively breastfed infants experience lower hospitalization rates than formula fed infants (Ajetunmobi et al., 2015). Women who do not breastfeed have a higher incidence of premenopausal breast cancer, ovarian cancer, retained gestational weight gain, type 2 diabetes, myocardial infarction, and metabolic syndrome (Stuebe, 2009).
Improving breastfeeding continuation and exclusivity after hospital discharge and were stressed in the Surgeon General's Call to Action to Promote Breastfeeding, and post-discharge home monitoring and lactation counseling are critical to ensure that adequate breastfeeding is established during the first month (Surgeon General, 2011). Despite efforts to improve breastfeeding duration, the breastfeeding rate is still 49.4% at 3 months and 26.7% at 12 months, with 40.7% exclusively breastfeeding at 3 months and 18.8% at 6 months (Centers for Disease Control and Prevention [CDC], 2014).
CALLOUT 1
Researchers have documented that early postpartum breastfeeding challenges may negatively affect breastfeeding success. Breastfeeding concerns, including difficulty with latching, nipple pain, and perceived insufficient milk supply during the first week postpartum, were highly prevalent and associated with as much as a ninefold greater risk of discontinuation earlier than intended among primiparous mothers (Wagner, Chantry, Dewey, & Nommsen-Rivers, 2013). Lack of lactation support and breastfeeding problems were among the main reasons for breastfeeding cessation after hospital discharge among new lactating mothers with gestational diabetes (Gerd, Bergman, Dahlgren, Roswall, & Alm 2012; Morrison, Collins, Lowe, & Giglia, 2015). Paper and pencil diaries may improve breastfeeding exclusivity; however, breastfeeding diaries may not foster communication between lactation specialists and mothers post-discharge (Pollard, 2011). Given the proven value of breastfeeding and the challenge of supporting women post-discharge, there is a need for innovative and improved strategies to foster longer-term communication between mothers and lactation specialists post-discharge to ensure successful breastfeeding.
One potential way to foster long term communication is to incorporate Web and mobile health interventions; the use of these interventions is becoming an integral component of daily activities of national and global populations (World Health Organization [WHO], 2011). In recent years, many researchers have employed mobile phones as tools for symptom management and monitoring in heart disease, diabetes, and a range of different health problems (Huang et al., 2007; Klasnja & Pratt, 2012). Current web-based breastfeeding interventions are focused mainly on providing education for mothers and providers, or providing lactation support by electronic mail and social media (Thomas & Shaikh, 2012). In another example, breastfeeding Internet web-based education and support improved breastfeeding exclusivity at six months among Australian mothers (Giglia, Cox, Zhao, & Binns, 2015). A web-based intervention for breastfeeding mothers could provide continuous monitoring after discharge to maintain communication between mothers and lactation specialists. Such continuity of care can optimize the infant's intake and minimize the risk of dehydration, hypoglycemia, jaundice, weight loss, and re-hospitalization within the first 30 days after discharge in case of breastfeeding problems (Seagraves, Brulte, McNeely, & Pritham, 2013). In an attempt to address this communication gap, our interdisciplinary research team developed an interactive web-based breastfeeding monitoring system that was feasible, usable, and acceptable among breastfeeding mothers. This intervention was based on a self-regulation model from Bandura's Social cognitive Theory as explained in our previous work (Ahmed & Ouzzani, 2012; Ahmed & Ouzzani, 2013). Previous studies supported the effect of education and lactation support by phone and peer counseling in improving breastfeeding outcomes for term and preterm infants (Chapman, Morel, Anderson, Damio, & Pérez-Escamilla, 2010; Reeder, Joyce, Sibley, Arnold, & Altindag, 2014). No studies, however, tested the effect of online web-based breastfeeding monitoring with tailored education on breastfeeding outcomes.
One of the factors that may negatively affect breastfeeding outcomes is postpartum depression (PPD). Postpartum depression is defined as a major depressive disorder in the Diagnostic and Statistical Manual of Mental Disorders (DSM-V), with a specifier of postpartum onset four weeks after childbirth (American Psychiatric Association, 2013). The effect of breastfeeding on the risk of PPD is not clear. The association between longer breastfeeding duration and lower prevalence of PPD has been reported. In contrast, other studies have suggested no association with breastfeeding mothers and an increased risk of PPD (Annagür, Annagür, Şahin, Örs, & Kara, 2013; Dennis, & McQueen, 2007).
The purpose of this study was to determine whether an interactive web-based breastfeeding monitoring system during the first month after hospital discharge increased breastfeeding exclusivity, intensity, and duration as primary outcomes and decreased symptoms of postpartum depression as a secondary outcome. We hypothesized that mothers in the intervention group would have higher rates of exclusive breastfeeding and would breastfeed more frequently and for a longer duration. Further, we hypothesized that mothers in the intervention group would have fewer symptoms of postpartum depression compared to the usual care group.
Methods
Design, Settings and Participants
We conducted a two arm randomized controlled trial in three Midwest Hospitals. A research scientist and a lactation consultant recruited participants (141 mother/infant dyads) before hospital discharge. Eligibility criteria for mothers included the ability to read and speak English, ≥ 18 years old, an intention to continue breastfeeding after discharge, no serious medical condition that prevents breastfeeding (e.g. HIV positive), basic knowledge of how to use the Internet, and access to electronic mail and the Internet through either a standard PC or a smartphone. Eligibility criteria for infants included singleton full-term (≥37 gestational weeks) while exclusion criteria included infants born with cleft lip/palate, congenital heart defects, Down Syndrome, neural tube defects, or other conditions that either require the newborn's admission to a neonatal intensive care unit or interfere with breastfeeding.
Randomization
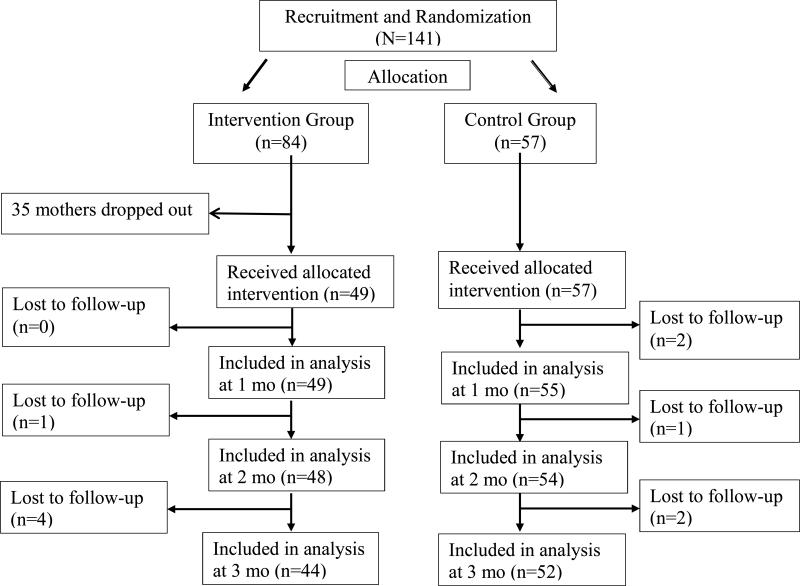
Participants were allocated to the usual care group and intervention group by computer-generated random numbers using mode of delivery and parity as stratifying factors to control for these variables (Figure 1). Mode of delivery and parity were found to be related to breastfeeding initiation, duration, and exclusivity (Haucky, Fenwich, Dhaliwal, & Butt, 2011). Mothers assigned to the usual care group followed the standard care of the hospital unit, which consisted of breastfeeding support and education before discharge, one phone call within the first week after hospital discharge, and a list of community breastfeeding resources. Mothers were encouraged to contact the lactation specialist with any breastfeeding problems.
Figure 1.
Subject Recruitment, Dropout, and Completion of the Study
Mothers assigned to the intervention group received the same support and education prior to discharge as the usual care group. Additionally, the lactation specialist/research scientist gave the mothers access to the computer application for the interactive breastfeeding monitoring system before hospital discharge and explained how to use the system. Mothers were asked to enter their breastfeeding data, infant's wet and dirty diapers, and any problems for at least 30 days. The system automatically sent feedback via notifications with tailored interventions if the mother entered data that indicated breastfeeding problems, including the infant's inability to latch, latching with nipple shields, difficulty waking up for feedings, jaundice, mothers’ sore nipples, engorgement or insufficient feeding (less than 6 times per day). The system also alerted the research team about mothers’ problems. The notifications were developed to target the most common breastfeeding problems during the first week after hospital discharge. The system also provided positive notifications when the mother breastfed 8 to 10 times per day and read the notifications (Ahmed & Ouzzani, 2013). Participants were given a study folder with handouts that explained how to use the system and how to benefit from it. The handouts were written at 5th grade reading level. Professional educational resources were also available through the system for the mother to read, including feeding cues information, milk supply management, jaundice management, correct latching, pumping, and returning to work/school. The mothers’ data were monitored by research assistants and a lactation specialist. Mothers were encouraged to contact their lactation specialist with any breastfeeding problems.
Sample calculation
The sample size was calculated based on the exclusive breastfeeding rate at 6 months of 11.4% in Indiana (CDC, 2014). A sample size of 50 mothers per group was calculated to allow us to detect a 20.3% increase with a power > 0.8 when alpha was set to 0.05 and using a one-sided test. We added 30 additional mothers to the intervention group to allow for an attrition rate of 35%.
Outcome Measures
Primary outcome
Pattern of breastfeeding (exclusive, predominant, partial) was assessed on discharge and then at 1, 2, and 3 months post discharge. Breastfeeding pattern was assessed using the WHO definition (WHO, 2010). Exclusive breastfeeding was defined as no other food or drink, not even water, except breast milk (including milk expressed), but allows the infant to receive vitamins, minerals and medicines. Predominant breastfeeding was defined as breast milk was the predominant source of nourishment (including milk expressed as the predominant source of nourishment). However, the infant may also receive liquids (water and water-based drinks, fruit juice) ritual fluids and vitamins, minerals and medicines. Partial breastfeeding referred to mixed feeding of breast milk and other food or food-based fluids, such as formula milk or weaning foods (WHO, 2010).
A follow-up form composed of 12 questions was developed for the purpose of the study based on an evidence based literature review. The form included questions about feeding patterns, number of breastfeeding sessions per day, number of supplementation feedings, types of supplementation, reasons for supplementation, and reasons for stopping breastfeeding. Content validity was assessed by a panel of four lactation specialists using the content validly index (CVI) (Polit, Beck, & Owen, 2007). There was universal agreement on the content among the panel members. The calculated CVI value was 0.79. Breastfeeding intensity was calculated as the number of breast milk feedings per day (direct breastfeeding + expressed breast milk), divided by the total number of feeding sessions per day (breast milk + formula feedings). “Breastfeeding intensity was categorized as ≥ 50% (High intensity) vs < 50% (low intensity)” (Chapman, Morel, Bermúdez-Millán, Young, Damio, & Pérez-Escamilla, 2013).
Secondary outcome
The Edinburgh Postpartum Depression Scale (EPDS) was used to assess mothers’ risk for postpartum depression. The reported overall reliability (Cronbach's alpha) of EPDS was 0.79 (Wisner, Parry, & Piontek, 2002). The EPDS Cronbach's alpha for our sample was calculated and it was 0.70. The scale consisted of 10 short statements. The mothers were asked to check off one of four possible answers that was closest to how she has felt during the past week. Responses were scored 0, 1, 2 and 3 based on the seriousness of the symptom. Items 3, 5 to 10 are reverse scored (i.e., 3, 2, 1, and 0). The total score was calculated by adding together the scores for each of the 10 items. Scores ranged from 0 to 30 with score 10 or more indicated depression.
Data Collection
Prior to beginning subject recruitment Institutional Review Board approval was received from Purdue University and each hospital. Eligible mothers were approached about the study by trained research teams in collaboration with the hospital unit's lactation consultant before hospital discharge. Once the mother agreed to participate in the study, she was asked to sign the consent form and complete the paper-based socio-demographic, infant profile, and breastfeeding baseline forms prior to hospital discharge. Mothers then were randomly assigned to the intervention or control group. Mothers assigned to the intervention group were trained to use the computer system application and enter their data before discharge and were asked to enter their 24-hour breastfeeding data daily in the system for 30 days.
An electronic welcome message from the research team was sent to the mothers in both groups to welcome them to the study and explain the study protocol according to their assigned group. The researcher and a trained research assistant monitored the mothers’ data online through the system's lactation specialist portal two times daily, once in the morning and another time in the late afternoon, and contacted the mothers with any breastfeeding problems.
All mothers in both groups submitted the follow-up form and postpartum depression scale online at 1, 2 and 3 months through an online survey. A thank-you letter with a $30 gift card was sent to each mother after completing the survey for month 1, and a $10 gift card was sent after each of the second and third month surveys were completed. Mothers were considered subjects in the study if they completed at least 2 weeks of online data entry (if in the intervention group) and submitted the follow-up forms. Although participants from the feasibility and acceptability study (Ahmed and Ouzzani, 2012) reported that the data entry was not overwhelming or time consuming, data entry could be a burden for mothers who have just given birth and are caring for themselves and their newborn postpartum needs. To ease the burden of data entry, the mobile version of the system was available on smartphones for the mothers’ convenience to enter data from anywhere. We asked the participants to either write down their data and enter it at a convenient time or enter their data immediately after the breastfeeding sessions. Husbands, partners, or significant others were encouraged to help mothers in data entry. Technical support was provided 24/7 for any system technical problems through online web-support. Mothers were reminded every other day via email and phone if they did not enter their data and/or submit the surveys.
Data Analysis
All analyses were conducted using Statistical Analysis System version 9.3. The primary dependent variables were breastfeeding rates of exclusivity, intensity, and any breastfeeding at discharge, 1 month, 2 months, and 3 months postpartum. Descriptive statistics were computed for demographic factors and infants’ profile data. Differences between groups were assessed by using Chi-square analyses or Fisher's Exact test for proportion, Student t-tests (if normally distributed) or Mann-Whitney U tests (if not) for other continuous variables. All analyses at baseline were done by intention-to-treat. An interaction effect model was conducted to examine the interaction between breastfeeding patterns and confounding variables such as mode of delivery, past breastfeeding experience, and history of taking a breastfeeding class during pregnancy.
CALLOUT 2
Results
Figure 1 explains subjects’ recruitment and drop out based on mobile Consolidated Standards of Reporting Trials (CONSORT) e-health criteria (Eysenbach, 2011). We over-recruited in the intervention group to accommodate an attrition rate of 35%, which is common in online intervention studies (Eysenback, 2005; Wangberg, Bergmo, & Johnsen, 2008). Thirty-five participants dropped out of the intervention group. Seventeen participants did not access the system (non-use drop out), and 10 mothers accessed the system once or twice and then reported that they were busy with family and older children and did not have any problems with breastfeeding. Five participants had computer and Internet problems and three reported re-hospitalization (one maternal hospitalization and two for infants). There was a 96% response rate for the first month survey among the control group, with 91% and 80% response rates for the second and third month, respectively, while the response rates for the first, second, and third month among the intervention group were 100%, 92% and 88%, respectively (n= 49).
Participant Characteristics
The demographic characteristics of the participants are displayed in Table 1. There was no significant difference between the control and intervention groups in the mothers’ demographic information, including maternal age, race, education, occupation, residency, and past breastfeeding experience. However, when participants who dropped from the intervention group were compared to participants who completed the study, a significant difference was found in the age and income categories. Participants who dropped out from the study were younger (p = 0.059) and had a lower income (p = 0.029). A higher rate of African American participants dropped out from the study (34%) compared to those who completed (18%), but was not statistically significant.
Table 1.
Mothers’ Demographics for Control and Intervention groups (completed and dropped out)
| Variables | Control Group N=57 | Intervention Completed N=49 | Fisher's exact test | Intervention Dropped out N= 35 | Fisher's exact test | |||
|---|---|---|---|---|---|---|---|---|
| Age | n | % | n | % | P | n | % | P |
| < 20 | 4 | 7.0 | 4 | 8.2 | 5 | 14.3 | ||
| 20 – 29 | 25 | 43.9 | 17 | 34.7 | 19 | 54.3 | ||
| ≥ 30 | 28 | 49.1 | 28 | 57.1 | 0.658 | 11 | 31.4 | 0.059 |
| Mean±SD | 29.2±6.3 | 29.9±6.5 | 26.6±6.6 | |||||
| Race/ethnicity | ||||||||
| Hispanic | 3 | 5.3 | 1 | 2.0 | 1 | 2.9 | ||
| Asian | 1 | 1.9 | 2 | 4.0 | 0 | 0.0 | ||
| Black or African American | 15 | 28.3 | 9 | 18.4 | 12 | 34.3 | ||
| White | 36 | 67.9 | 36 | 73.5 | 21 | 60.0 | ||
| More than one race | 1 | 1.9 | 2 | 4.1 | 0.635 | 2 | 5.7 | 0.375 |
| Income | ||||||||
| Less than $10,000 | 11 | 19.3 | 4 | 8.2 | 8 | 22.9 | ||
| $10,000 to < $24,999 | 11 | 19.3 | 4 | 8.2 | 4 | 11.4 | ||
| $25,000 - to $49,999 | 8 | 14.0 | 6 | 12.2 | 9 | 25.7 | ||
| $50,000 or more | 27 | 47.4 | 35 | 71.4 | 0.065 | 14 | 40.0 | 0.029 |
| Education | ||||||||
| Lower than High school Graduate | 19 | 33.3 | 15 | 30.6 | 13 | 37.1 | ||
| Associate degree | 8 | 14.0 | 4 | 8.2 | 5 | 14.3 | ||
| BA / BS degree | 20 | 35.1 | 15 | 30.6 | 9 | 25.7 | ||
| Graduate degree | 10 | 17.5 | 15 | 30.6 | 0.427 | 8 | 22.9 | 0.673 |
| Occupation | ||||||||
| Homemaker | 20 | 35.1 | 18 | 36.7 | 13 | 37.1 | ||
| Machine operator/ semiskilled Worker | 8 | 14.0 | 1 | 2.0 | 0 | 0.0 | ||
| Clerical/sales, Small business owner, farm owner | 5 | 8.8 | 4 | 8.2 | 4 | 11.4 | ||
| Technicians / semiprofessional | 4 | 7.0 | 3 | 6.1 | 5 | 14.3 | ||
| Mid-level manager or Professional | 19 | 33.3 | 19 | 38.8 | 9 | 25.7 | ||
| Senior manager or Professional | 1 | 1.8 | 4 | 8.2 | 0.212 | 4 | 11.4 | 0.616 |
| Parity | ||||||||
| First infant | 33 | 57.9 | 21 | 42.9 | 20 | 57.1 | ||
| Second infant | 16 | 28.1 | 16 | 32.7 | 12 | 34.3 | ||
| Third infant | 6 | 10.5 | 8 | 16.3 | 3 | 8.6 | ||
| Fourth infant or more | 2 | 3.5 | 4 | 8.2 | 0.393 | 0 | 0.0 | 0.235 |
| Delivery mode | ||||||||
| Vaginal | 42 | 73.7 | 36 | 73.5 | 25 | 71.4 | ||
| Not vaginal | 15 | 26.3 | 13 | 26.5 | 1.000 | 10 | 28.6 | 1.000 |
| Past breastfeeding experience | ||||||||
| < 3 months | 9 | 15.8 | 3 | 6.1 | 4 | 11.4 | ||
| 3 - 6 months | 5 | 8.8 | 8 | 16.3 | 3 | 8.6 | ||
| 7 - 12 months | 8 | 14.0 | 8 | 16.3 | 4 | 11.4 | ||
| > 1 year | 5 | 8.8 | 8 | 16.3 | 4 | 11.4 | ||
| No experience | 30 | 52.6 | 22 | 44.9 | 0.289 | 20 | 57.1 | 0.608 |
| Breast feeding class | ||||||||
| Yes | 30 | 52.6 | 27 | 55.1 | 23 | 65.7 | ||
| No | 27 | 47.4 | 22 | 44.9 | 0.847 | 12 | 34.3 | 0.373 |
Note. Fisher's exact test was calculated for the intervention group who completed the study and who dropped out from the study.
The demographic characteristics of the infants are described in Table 2. There were no significant differences in the infants between the intervention and control groups in terms of gestational age, birth weight, and discharge weight (Table 2). All mothers, regardless of group assignment (100%) initiated breastfeeding. The majority of mothers in both groups started breastfeeding with their own breast milk by direct breastfeeding and three mothers in each group gave pumped expressed milk on hospital discharge (Table 3).
Table 2.
Gestational Age and weight of Infants at birth and discharge among Control and Intervention Groups
| Control N= 57 | Completed Intervention N= 49 | Dropped out Intervention N= 35 | ||||||
|---|---|---|---|---|---|---|---|---|
| Variables | Median | 95% CI | Median | 95% CI | P | Median | 95% CI | P |
| Gestational Age (wk) | 39.00 | 38.70 - 39.32 | 39.10 | 38.87 - 39.47 | 0.4018 | 39.20 | 39.09 - 39.71 | 0.4477 |
| Birth wt (kg) | 3.25 | 3.20 - 3.40 | 3.41 | 3.28 - 3.56 | 0.1795 | 3.47 | 3.30 - 3.58 | 0.8869 |
| Discharge wt (kg) | 3.02 | 3.02 - 3.21 | 3.23 | 3.06 - 3.32 | 0.1913 | 3.20 | 3.10 - 3.35 | 0.7044 |
Note. Fisher's exact test was calculated to test the differences between groups.
Table 3.
Infant Profile for Control and Intervention Groups (completed and dropped out)
| Control Group N=57 | Intervention Completed N=49 | Fisher's exact test | Intervention Dropped out N=35 | Fisher's exact test | ||||
|---|---|---|---|---|---|---|---|---|
| N | % | N | % | P | N | % | P | |
| First feeding | N = 50 | |||||||
| Mother's own milk | 54 | 94.8 | 47 | 94.0 | 34 | 97.1 | ||
| Formula | 3 | 5.3 | 3 | 6.0 | 1.000 | 1 | 2.9 | 0.3403 |
| Morbidities | N = 59 | |||||||
| Jaundice | 5 | 8.5 | 5 | 10.2 | 4 | 11.4 | ||
| Decrease body temp | 1 | 1.7 | 1 | 2.0 | 1 | 2.9 | ||
| Decrease in blood glucose | 2 | 3.4 | 2 | 4.1 | 1 | 2.9 | ||
| Difficult or trouble breathing | 4 | 6.8 | 1 | 2.0 | 3 | 8.6 | ||
| None | 47 | 79.7 | 40 | 81.6 | 0.9727 | 26 | 74.3 | 0.7169 |
| Breastfeeding problem on discharge | N = 59 | |||||||
| Inability to latch | 2 | 3.4 | 5 | 10.2 | 5 | 14.3 | ||
| Latch with nipple shield | 5 | 8.5 | 8 | 16.3 | 3 | 8.6 | ||
| Inability to wake up for feeding | 8 | 13.6 | 4 | 8.1 | 1 | 2.9 | ||
| No problem | 44 | 75.6 | 32 | 65.3 | 0.3788 | 26 | 74.3 | 0.7031 |
Note. Fisher's exact test was calculated for the Intervention group who completed the study and who dropped out from the study. N varied based on infants’ first feeding, morbidity and problems.
Breastfeeding Outcomes
Due to low response rates in the predominant category, breastfeeding pattern was re-categorized as either exclusively breastfeeding (breast milk only), partial (includes predominant breastfeeding and formula feeding bedside breastfeeding), and formula (no breastfeeding). At the time of hospital discharge, no significant difference in breastfeeding pattern was found between the control and intervention groups (p = 0.892) for breastfeeding exclusivity or any breastfeeding. Eighty two percent in the control group and approximately 80% in intervention group were discharged exclusively breastfeeding. A significant difference in breastfeeding pattern was found between groups at 1 month (p = 0.027), 2 months (p = 0.000) and 3 months (p = 0.002). The intervention group had higher exclusive breastfeeding rates at 1 month, 2 months and 3 months (63%, 63% and 55%, respectively) compared to the control group (40%, 19%, and 19% respectively). Approximately 84% were still breastfeeding at 3 months within the intervention group compared to 66.7% in the control group (Table 4). There was a significant difference between the intervention and control groups in breastfeeding intensity (p= 0.002) using the Wilcoxon-Man Whitney test. Mothers in the intervention group had a greater than 50% breast-feeding frequency per day. A more comprehensive longitudinal model between breast-feeding frequency and several covariates (time, group and their interaction) was also investigated using Generalized Estimating Equation approach. The findings showed similar results as reported earlier, but no interaction between time and group was found.
Table 4.
Breastfeeding Pattern among Control and Intervention groups at Hospital Discharge 1, 2 and 3 months.
| Variable | Control | On Discharge Intervention |
Control | 1 Month Intervention |
Control | 2 Month Intervention |
Control | 3 Month Intervention |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | P | n | % | n | % | P | n | % | n | % | P | n | % | n | % | P | |
| Exclusive breastfeeding | 47 | 82.5 | 39 | 79.6 | 0.7071 | 23 | 40.4 | 31 | 63.3 | 0.0268 | 11 | 19.3 | 31 | 63.3 | <0.0001 | 11 | 19.3 | 27 | 55.1 | 0.0020 |
| Partial breastfeeding | 10 | 17.5 | 10 | 20.4 | 31 | 54.4 | 15 | 30.6 | 34 | 59.6 | 12 | 24.5 | 27 | 47.4 | 12 | 24.5 | ||||
| Exclusive formula | 0 | 0.0 | 0 | 0.0 | 1 | 1.8 | 3 | 6.1 | 7 | 12.3 | 2 | 4.1 | 8 | 14.0 | 4 | 8.2 | ||||
| No Response | 0 | 0.0 | 0 | 0.0 | 2 | 3.5 | 0 | 0.0 | 5 | 8.8 | 4 | 8.2 | 11 | 19.3 | 6 | 12.2 | ||||
| Total | 57 | 100 | 49 | 100 | 57 | 100 | 49 | 100 | 57 | 100 | 49 | 100 | 57 | 100 | 49 | 100 | ||||
Chi-square test for independence was used to test the difference between groups.
Postpartum Depression Symptoms Outcome
Postpartum depression symptoms scores showed a progressive decrease after giving birth in both groups at 1, 2, and 3 months. The control group means scores were 4.9±3.9, 4.3±4.9, and 3.2±3.9, respectively. Lower scores were found among the intervention group (4.7±4.5, 3.0±3.4, and 3.2±3.6, respectively). However, there was no statistically significant difference between the groups at 1, 2, and 3 months (P = 0.389, 0.170, and 0.920, respectively).
An interaction effect model was conducted to examine the interaction between breastfeeding pattern and mode of delivery, past breastfeeding experience, and history of taking a breastfeeding class during pregnancy. There was no significant interaction with all variables, but there was a weak effect with attending breastfeeding class during pregnancy (P =0.060).
Discussion
This randomized controlled trial was conducted to determine the effect of an interactive web-based breastfeeding monitoring system on breastfeeding outcomes and postpartum depression symptoms among breastfeeding mothers immediately after hospital discharge. The interactive web-based breastfeeding monitoring intervention had a significant effect on breastfeeding exclusivity, intensity, and duration among intervention group mothers at 1, 2, and 3 months, which supported our hypothesis related to breastfeeding exclusivity, intensity, and duration. There was no significant interaction of confounding variables that could affect breastfeeding pattern, such as past breastfeeding experience or attending a breastfeeding class during pregnancy. Our study was the first to test the effect of an interactive web-based breastfeeding monitoring intervention among lactating mothers. A recent systematic review indicated the lack of studies that test the effectiveness of the internet and mobile devices in improving breastfeeding outcomes (Giglia, & Binns, 2014). However, web-based interventions were effective in changing behaviors among adolescents with chronic conditions such as diabetes (Connelly, Kirk, Masthoff, & MacRury, 2013; Mulvaney, et al., 2012) and asthma (Araújo et al., 2012; Voorend-van Bergen et al., 2013). Also, web-based self-report assessments and educational interventions on symptom distress during cancer therapy reduced symptom distress in a multicenter sample of cancer patients (Berry et al., 2014). Young Adults Eating and Active for Health (YEAH) theory-based web-delivered intervention supported positive change in behaviors that may mediate excessive weight gain through healthful self-regulation mealtime behaviors immediately post intervention (Kattelmann et al., 2014).
Although there was continuous improvement of postpartum depression symptoms scores among the intervention group and a positive interaction effect between postpartum depression symptoms scores and breastfeeding pattern, there were no statistically significant differences between the control and intervention groups. These results are consistent with previous studies that reported no association between breastfeeding pattern and postpartum depression symptoms scores (Dennis & McQueen, 2007). However, a recent systematic review and previous evidence reported that postpartum depression symptoms predicts and is predicted by breastfeeding cessation (Dias & Figueiredo, 2015; Figueiredo, Dias, Brandão, Canário & Nunes-Costa, 2013).
Our study has several strengths and limitations. The intervention was theory-based and developed with a self-regulation model (Ahmed & Ouzzani, 2013). Our previous study revealed that breastfeeding monitoring through a web-based monitoring intervention and timely notifications with tailored education raised mothers’ awareness of their breastfeeding patterns and problems they were experiencing. Mothers reported that the notification system provided helpful hints to solve breastfeeding problems and maintain milk supply. The notifications also referred the mothers to their lactation specialists to avoid any confusion and maintain consistency and continuation in breastfeeding support (Ahmed & Ouzzani, 2012). There was no way of communication between participants while conducting the study that could lead to contamination. The mothers were recruited in the hospital, the surveys were submitted online, and the access to the system was password protected. Mothers’ responses to the follow-up surveys were very high at 1, 2 and 3 months with > 80% response rates among the intervention group participants.
CALLOUT 3
Although we recruited our sample from three different hospital settings to get a representative sample, Hispanic and Asian populations were not well represented in our study and that is explained by the nature of the women seen at these hospitals. Therefore, our findings may be applicable only to our current population, and the intervention needs to be tested among Hispanic and Asian populations. Therefore, generalizability of our findings may be limited to settings with a similar population. Thirty-five intervention group mothers dropped out of the study, with 17 not using the system (non-use dropout) and 18 not completing the interventions for several reasons as mentioned above. We expected a high attrition rate from our experience in our previous study and other web-based intervention studies (Ahmed & Ouzzani, 2012; van Bastelaar, Pouwer, Cuijpers, Riper & Snoek, 2011). Our attrition rate is less than or consistent with other web-based interventions studies (Carter, Burley, Nykjaer & Cade, 2013; Eysenback, 2005). Eysenback (2005) and Wangberg, Bergmo, and Johnsen (2008) reported that dropout from web-based intervention studies is substantial and related to subjects’ self-efficacy, age, and education. When we compared the characteristics of the mothers who completed and who dropped out from the study, the mothers who dropped out were younger with lower incomes. More African American mothers dropped out compared to those who completed the study. The CDC reported breastfeeding disparities among African American mothers with breastfeeding rates about 16% lower than for whites, plus a low rate of breastfeeding among young and low-income mothers (CDC, 2010).
Implications for Research
Our study has important implications for web-based/mobile health initiatives. Our results demonstrated that interactive web-based monitoring for breastfeeding is a promising intervention that provides two-way communication between mothers and lactation consultants and may improve breastfeeding outcomes. The intervention also supports the need for mobile-health and tele-health to improve health outcomes, especially among underserved, low-income families with limited access to lactation support, such as minority populations and those living in rural areas. While web-based and mobile phone technology continues to improve, more studies are needed to test their effectiveness on a larger scale. Implementing multisite studies and allowing for a longer follow-up that includes all races and ethnicities are needed to test the long-term effects of these web-based, tailored interventions. Different types of mobile technologies are widely available and can play an important role in healthcare at the regional, community, and individual levels (Habibi et al., 2012; WHO, 2011).
Conclusion
The interactive web-based breastfeeding intervention that maintains communication between the mother and her lactation specialist and provides tailored education could be a promising strategy to improve breastfeeding exclusivity, intensity, and duration. Studies that test its effectiveness on a large scale in multiple settings and test its cost effectiveness are needed.
Callout Statements.
Breastfeeding support during the first month post-discharge is associated with improved breastfeeding exclusivity and duration
A web-based intervention for breastfeeding mothers can provide continuous monitoring after discharge and a line of communication between mothers and lactation specialists.
Mothers who participated in the online breastfeeding monitoring program had higher exclusive breastfeeding rates at 1, 2, and 3 months than the usual care group.
Acknowledgement
This project was funded by Indiana CTSI Collaboration in Biomedical/Translational Research (CBR/CTR) Pilot Program Grants (Grant # UL1TR001108).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure The authors report no conflict of interest or relevant financial relationships.
Contributor Information
Azza H Ahmed, School of Nursing, Purdue University, West Lafayette, IN..
Ali M. Roumani, Department of Computer Science, Gulf University for Science & Technology, Mishref, Kuwait, and Discovery Park, Purdue University, West Lafayette, IN..
Kinga Szucs, Indiana University School of Nursing, Indianapolis, IN..
Lingsong Zhang, Department of Statistics, Purdue University, West Lafayette, IN..
Demetra King, Accenture, Chicago, IL..
References
- Ahmed A, Ouzzani M. Interactive web-based breastfeeding monitoring: Feasibility, usability and acceptability. Journal of Human Lactation. 2012;28(4):468–475. doi: 10.1177/0890334412451869. [DOI] [PubMed] [Google Scholar]
- Ahmed A, Ouzzani M. Development and assessment of an interactive web-based breastfeeding monitoring system. Maternal Child Health Journal. 2013;17(5):809–815. doi: 10.1007/s10995-012-1074-z. [DOI] [PubMed] [Google Scholar]
- Ajetunmobi OM, Whyte B, Chalmers J, Tappin DM, Wolfson L, Fleming M, MacDonald A, Stockton DL. Breastfeeding is associated with reduced childhood hospitalization: Evidence from a Scottish birth cohort (1997-2009). Journal of Pediatrics. 2015;166:620–625. doi: 10.1016/j.jpeds.2014.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 5th ed. American Psychiatric Press; Washington, DC: 2013. [Google Scholar]
- Annagür A, Annagür BB, Şahin A, Örs R, Kara F. Is maternal depressive symptomatology effective on success of exclusive breastfeeding during postpartum 6 weeks? Breastfeeding Medicine. 2013;8(1):53–57. doi: 10.1089/bfm.2012.0036. [DOI] [PubMed] [Google Scholar]
- Araújo L, Jacinto T, Moreira A, Castel-Branco MG, Delgado L, Costa-Pereira A, Fonseca J. Clinical Efficacy of Web-Based Versus Standard Asthma Self-management. Journal of Investigational Allergology Clinical Immunology. 2012;22(1):28–34. [PubMed] [Google Scholar]
- Berry DL, Hong F, Halpenny B, Partridge A, Fox E, Fann JR, Ford R. The electronic self-report assessment and intervention for cancer: Promoting patient verbal reporting of symptom and quality of life issues in a randomized controlled trial. BMC Cancer. 2014;14:513. doi: 10.1186/1471-2407-14-513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter MC, Burley VJ, Nykjaer C, Cade JE. Adherence to a smartphone application for weight loss compared to website and paper diary: Pilot randomized controlled trial. Journal of Medical Internet Research. 2013;15(4):e32. doi: 10.2196/jmir.2283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention 2009 pandemic influenza A (H1N1) in pregnant women requiring intensive care — New York City, 2009. Morbidity and Mortality Weekly Report. 2010;59(11):1–36. Retrieved from http://www.cdc.gov/mmwr/pdf/wk/mm5911.pdf. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention Breastfeeding report card, United States 2014. 2014 Retrieved from http://www.cdc.gov/breastfeeding/pdf/2014breastfeedingreportcard.pdf.
- Chapman DJ, Morel K, Anderson AK, Damio G, Pérez-Escamilla R. Breastfeeding peer counseling: From efficacy through scale-up. Journal of Human Lactation. 2010;26(3):314–326. doi: 10.1177/0890334410369481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman DJ, Morel K, Bermúdez-Millán A, Young S, Damio G, Pérez-Escamilla R. Breastfeeding education and support trial for overweight and obese women: a randomized trial. Pediatrics. 2013;131(1):e162–e170. doi: 10.1542/peds.2012-0688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connelly J, Kirk A, Masthoff J, MacRury S. The use of technology to promote physical activity in Type 2 diabetes management: A systematic review. Diabetes Medicine. 2013;30:1420–1432. doi: 10.1111/dme.12289. [DOI] [PubMed] [Google Scholar]
- Dennis CL, McQueen K. Does maternal postpartum depressive symptomatology influence infant feeding outcomes? Acta Paediatrica. 2007;96(4):590–594. doi: 10.1111/j.1651-2227.2007.00184.x. [DOI] [PubMed] [Google Scholar]
- Dias C. b. C., Figueiredo B. Breastfeeding and depression: A systematic review of the literature. Journal of Affective Disorders. 2015;171:142–154. doi: 10.1016/j.jad.2014.09.022. [DOI] [PubMed] [Google Scholar]
- Dieterich CM, Felice JP, O'Sullivan E, Rasmussen KM. Breastfeeding and health outcomes for the mother-infant dyad. Pediatric Clinics of North America. 2013;60(1):31–48. doi: 10.1016/j.pcl.2012.09.010. doi:10.1016/j.pcl.2012.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eysenbach G. CONSORT-EHEALTH: Improving and standardizing evaluation reports of Web-based and mobile health interventions. Journal of Medical Internet Research. 2011;13(4):e126. doi: 10.2196/jmir.1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eysenback G. The law of attrition. Journal of Medical Internet Research. 2005;7(1):e11. doi: 10.2196/jmir.7.1.e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Figueiredo B, Dias CC, Brandão S, Canário C, Nunes-Costa R. Breastfeeding and postpartum depression: state of the art review. Journal of Pediatrics. 2013;89(4):332–338. doi: 10.1016/j.jped.2012.12.002. [DOI] [PubMed] [Google Scholar]
- Giglia RI, Binns C. The effectiveness of the internet in improving breastfeeding outcomes: A systematic review. Journal of Human Lactation. 2014;30(2):156–160. doi: 10.1177/0890334414527165. [DOI] [PubMed] [Google Scholar]
- Giglia R1, Cox K, Zhao Y, Binns CW. Exclusive breastfeeding increased by an internet intervention. Breastfeeding Medicine. 2025;10:20–25. doi: 10.1089/bfm.2014.0093. [DOI] [PubMed] [Google Scholar]
- Gerd AT, Bergman S, Dahlgren J, Roswall J, Alm B. Factors associated with discontinuation of breastfeeding before 1 month of age. Acta Pediatrica. 2012;101(1):55–60. doi: 10.1111/j.1651-2227.2011.02405.x. [DOI] [PubMed] [Google Scholar]
- Habibi MF, Nicklas J, Spence M, Hedberg Sh., Magnuson E, Kavanagh KF. Remote lactation consultation: a qualitative study of maternal response to experience and recommendations for survey development. Journal of Human Lactation. 2012;28(2):211–217. doi: 10.1177/0890334411432716. [DOI] [PubMed] [Google Scholar]
- Hauck FR, Thompson JM, Tanabe KO, Moon RY, Vennemann MM. Breast-feeding and reduced risk of sudden infant death syndrome: A meta-analysis. Pediatrics. 2011;66(11):682–684. doi: 10.1542/peds.2010-3000. [DOI] [PubMed] [Google Scholar]
- Haucky YL, Fenwich J, Dhaliwal SS, Butt JA. Western Australian survey of breastfeeding initiation, prevalence and early cessation patterns. Maternal Child Health Journal. 2011;15(2):260–268. doi: 10.1007/s10995-009-0554-2. [DOI] [PubMed] [Google Scholar]
- Horta BL, de Mola VL, Victora CG. Long-term consequences of breastfeeding on cholesterol, obesity, systolic blood pressure, and type-2 diabetes: Systematic review and meta-analysis. Acta Pediatrica. 2015 doi: 10.1111/apa.13133. doi: 10.1111/apa.13133. [DOI] [PubMed] [Google Scholar]
- Huang MZ, Kuo SC, Avery MD, Chen W, Lin KC, Gau ML. Evaluating effects of a prenatal web-based breastfeeding education program in Taiwan. Journal of Clinical Nursing. 2007;16(8):1571–1579. doi: 10.1111/j.1365-2702.2006.01843.x. [DOI] [PubMed] [Google Scholar]
- Ip S, Chung M, Raman G, Chew P, Magula N, DeVine D, Lau J. Evidence report/technology assessment number 153. Agency for Healthcare Research and Quality; Rockville, MD: 2007. Breastfeeding and maternal and infant health outcomes in developed countries. Retrieved from http://archive.ahrq.gov/downloads/pub/evidence/pdf/brfout/brfout.pdf. [PMC free article] [PubMed] [Google Scholar]
- Johnston M, Landers S, Noble L, Szucs K, Viehmann L. Breastfeeding and the use of human milk. Pediatrics. 2012;129(3):e827–e841. doi: 10.1542/peds.2011-3552. [DOI] [PubMed] [Google Scholar]
- Kattelmann KK, Bredbenner CB, White AA, Greene G,W, Hoerr SL, Kidd T, Morrell JS. The effects of Young Adults Eating and Active for Health (YEAH): A theory-based web-delivered intervention. Journal of Nutrition Education and Behavior. 2014;46(6):S28–S41. doi: 10.1016/j.jneb.2014.08.007. [DOI] [PubMed] [Google Scholar]
- Klasnja P, Pratt W. Healthcare in the pocket: mapping the space of mobile-phone health interventions. Journal of Biomedical Informatics. 2012;45:184–198. doi: 10.1016/j.jbi.2011.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrison MK, Collins CE, Lowe JM, Giglia RC. Factors associated with early cessation of breastfeeding in women with gestational diabetes mellitus. Women Birth. 2015;28(2):143–147. doi: 10.1016/j.wombi.2014.12.002. doi: 10.1016/j.wombi.2014.12.002. [DOI] [PubMed] [Google Scholar]
- Mulvaney SA, Rothman RL, Dietrich MS, Wallston KA, Grove E, Elasy TA, Johnson KB. Using mobile phones to measure adolescent diabetes adherence. Health Psychology. 2012;31(1):43–50. doi: 10.1037/a0025543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polit DF, Beck CT, Owen SV. Is the CVI acceptable indicator of content validity? Appraisal and recommendations. Research n Nursing and Health. 2007;30:459–467. doi: 10.1002/nur.20199. [DOI] [PubMed] [Google Scholar]
- Pollard DL. Impact of a feeding log on breastfeeding duration and exclusivity. Maternal Child Health Journal. 2011;15(3):395–400. doi: 10.1007/s10995-010-0583-x. [DOI] [PubMed] [Google Scholar]
- Reeder JA, Joyce T, Sibley K, Arnold D, Altindag O. Telephone peer counseling of breastfeeding among WIC participants: A randomized controlled trial. Pediatrics. 2014;134(3):e700–e709. doi: 10.1542/peds.2013-4146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seagraves K, Brulte A, McNeely K, Pritham U. Supporting breastfeeding to reduce newborn readmissions for hyperbilirubinemia. Nursing for Women's Health. 2013;17(6):498–507. doi: 10.1111/1751-486X.12078. [DOI] [PubMed] [Google Scholar]
- Stuebe A. The risks of not breastfeeding for mothers and infants. Review in Obstetrics & Gynecology. 2009;2(4):222–231. [PMC free article] [PubMed] [Google Scholar]
- Surgeon General . The Surgeon General's call to action to support breastfeeding. Author; Washington, DC: 2011. Retrieved from http://www.surgeongeneral.gov/library/calls/breastfeeding/ [Google Scholar]
- Thomas JR, Shaikh U. Use of electronic communication by physician breastfeeding experts for support of the breastfeeding mother. Breastfeeding Medicine. 2012;7(6):393–396. doi: 10.1089/bfm.2011.0133. [DOI] [PubMed] [Google Scholar]
- Van Bastelaar KM, Pouwer F, Cuijpers P, Riper H, Snoek FJ. Web-based depression treatment for type 1 and type 2 diabetic patients. Diabetes Care. 2011;34:320–325. doi: 10.2337/dc10-1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voorend-van Bergen S, Vaessen-Verberne AA, Landstra AM, Brackel HJ, van den Berg NJ, Caudri D, Pijnenburg MW. Monitoring childhood asthma: Web-based diaries and the asthma control test. Journal of Allergy and Clinical Immunology. 2013;133(6):1599–1605. e2. doi: 10.1016/j.jaci.2013.10.005. [DOI] [PubMed] [Google Scholar]
- Wagner E, Chantry CJ, Dewey GD, Nommsen-Rivers LA. Breastfeeding concerns at 3 and 7 days postpartum and feeding status at 2 months. Pediatrics. 2013;132(4):e865–e875. doi: 10.1542/peds.2013-0724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wangberg SC, Bergmo TS, Johnsen JA. Adherence in internet-based interventions. Patient Preference and Adherence. 2008;2:57–65. [PMC free article] [PubMed] [Google Scholar]
- Wisner KL, Parry BL, Piontek CM. Postpartum Depression, the New England Journal of Medicine. 2002;347(3):194–199. doi: 10.1056/NEJMcp011542. [DOI] [PubMed] [Google Scholar]
- World Health Organization . Indicators for assessing infant and young child feeding Practices: Part 2 measurement. Author; Geneva, Switzerland: 2010. Retrieved from http://whqlibdoc.who.int/publications/2010/9789241599290_eng.pdf?ua=1. [Google Scholar]
- World Health Organization . mHealth: New horizons for health through mobile Technologies. Author; Geneva, Switzerland: 2011. Retrieved from http://www.who.int/goe/publications/goe_mhealth_web.pdf. [Google Scholar]
- Yan J, Liu L, Zhu Y, Huang G, Wang PP. The association between breastfeeding and childhood obesity: A meta-analysis. BMC Public Health. 2014;14(1):1267. doi: 10.1186/1471-2458-14-1267. [DOI] [PMC free article] [PubMed] [Google Scholar]