Abstract
Background:
Pain is one of the most common symptoms experienced by patients after surgeries. Inadequate postoperative pain management is an international problem and the need to improve its management is well documented. The aim of the study was to assess nursing reports related to the patients’ pain intensity and quality, concomitant symptoms, use of scales in pain assessment, and compliance with the national guideline after surgery.
Methods:
This study was a retrospective cohort; samples were nurse records of patients who had elective surgery.
Result:
Only 6% of the patients’ pain records included pain intensity which was not measured with standard scales. More than half of all injections were opioid analgesic which is in contrast to the guidelines of the Iranian Ministry of Health. Pain assessment was higher in women and by nurses with more than 15 years of working experience.
Conclusion:
to conclude, the patients’ pain was not assessed properly in terms of intensity, quality, and associated symptoms. Therefore, training and motivating nurses is very important in this context and should be incorporated in nurses’ academic and continuous educational courses.
Keywords: Nursing, Pain, Patient Records, Postoperative
1. INTRODUCTION
There has been a growing recognition that pain is a complex perceptual experience influenced by a wide range of psychosocial factors including emotions, social and environmental context, socio cultural background, the meaning of pain to the person, beliefs, attitudes, and expectations, as well as biological factors (1). In fact, pain is one of the most common symptoms that cause patients to seek health care and a chief problem in surgical patients; thus, it should be managed (2, 3). Successful pain management depends on health care personnel’s cooperative effort in assessing and controlling the pain (4). Management of postoperative pain relieves suffering and leads to earlier mobilization, shorter hospital stay, reduced hospital costs, and increased patient satisfaction (5).
Ineffective management of pain is a world-wide phenomenon. When pain is not effectively managed during the hospital stay; both patients and the organization may suffer. Activation of sympathetic system, increased readmissions, prolonged length of stays and poor clinical outcomes are possible outcomes (6-10). Despite advances in recent researches, availability of a large amount of analgesic medications and increased emphasis on pain management including enhanced awareness and the development of tools and scales to assist nurses in the care of patients, many patients still experience moderate to severe pain (11-13). Seventy-four percent of patients discharged from emergency departments tolerate moderate to severe levels of pain (14), and more than 50% of cancer patients report ineffective management of pain (15).
Postoperative pain management is an essential care component in surgical wards. As such, it should receive particular attention when identifying potential areas for improvement (16). The content of the documentation includes explanation about the patient’s condition, responses to illness, and the care that is provided. Finally, the definitive purpose of pain assessment, recording and management is promotion of the quality of care. Findings show that patients may avoid to express their pain or consider pain an inevitable consequence of surgery; therefore, nurses should asses the patients’ pain and their knowledge about pain control methods. Therapeutic pain management is divided into two main groups: pharmacologic and non-pharmacologic or alternatives (17). Non pharmacologic measures used by nurses to alleviate pain include positioning, music therapy, distraction, massage and other non-invasive methods (18, 19).
The pain management guideline that was published in 2004 is the only standard protocol in Iran by Iran Ministry of Health and Medical Education (Figure 1). Other available protocols are not popular and may be administered in regional hospitals.
Figure 1.
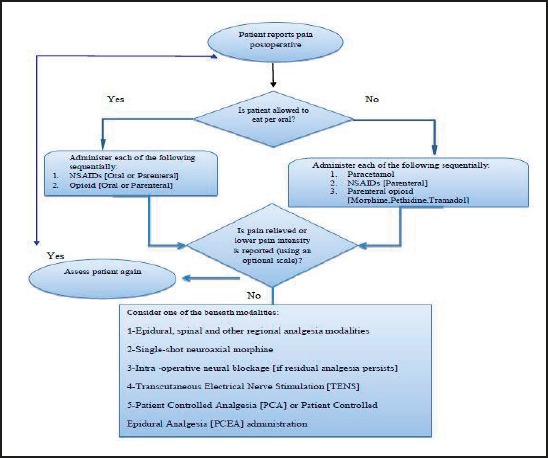
Postoperative Pain Management Guideline by Iran Ministry of Health and Medical Education
In our country, physicians usually do not assess pain comprehensively and order analgesics to be used when required. There is also no formal audit to report and document pain postoperatively in Iran (20). Considering the importance of pain management as one of principle patient rights, it is very important to assess pain and pain management alternatives.
2. METHOD
A descriptive and retrospective approach was used in assessing the records and collecting information about Postoperative pain, management and Documentation by nurses.
2. 1.Sample, Patients
The study population comprised 1540 patient charts in general surgery, ENT and orthopedic wards from March to August 2012 in Imam Khomeini Hospital of Jiroft, a southeast city of Iran. The sample size was calculated 385 patient records using SSC software (Precision=5%, expected ratio= 50, confidence level= 95%, population size= 1540) for statistical analysis among the total 1540 existing records.
Patients who were selected for this study had an elective admission and underwent general anesthesia and neither to have history of diabetes nor cancer. Besides, the patients who were investigated in this study were hospitalized at least for 48 hour. Our data were based on the hospital statics and documentation of database department.
2. 2.Instrument
Researchers made the check list after reviewing literatures and Iran Ministry of Health and Medical Education guideline for postoperative pain management (Figure 1). The checklist consisted of items like assessment of pain intensity, quality, location and concomitant symptoms by nurses, type of analgesic medication, route of drug administration (for the first and the second time if the pain did not alleviate), and the patient’s(age, gender and type of the surgery) and nurse’s demographic information. Whether pain intensity and quality was assessed by the nurse and use of a standard scale was evaluated with yes/no questions. If the answer was yes, then the method of pain assessment, type of analgesic medication, route and frequency of drug administration according to the patient’s diet (allowance to eat) were included in the checklist.
2. 3.Data Collection
Three hundred eighty five subjects were assessed randomly among the first 48 hours postoperative. This period of time describes postoperative duration. Patients, anonymity was observed during the study. Data was collected by a member who was blind to the methodology and aim of the study and was not employed at the hospital. Finally, the nurses ‘demographic factors (like age, education level and years of working in surgery ward) was asked from nurses who documented pain and still were working at the hospital after finishing retrospective chart review.
2. 4.Data analysis
Data were analyzed using descriptive statistics (mean and standard deviation (SD)), Chi squared, Independent Kendal test, spearman and Pearson correlation tests to compare the relationship between patient’s and nurses demographic factors with type of the analgesics. For estimating the odds ratio and factors affecting the assessment of pain intensity by nurses, a binary logistic and backward method was used. All statistical analyses were performed using SPSS software (v21.0; PASW Statistics). A p value of less than 0.05 was considered statistically significant.
3. RESULT
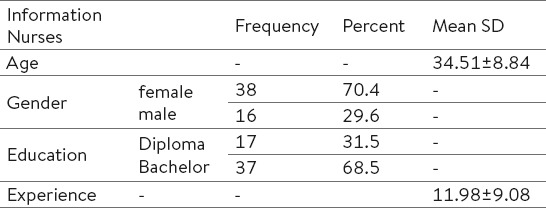
A total of 385 records were assessed. About 48.6% of the records belonged to orthopedic patients, 35.5% to general surgery, and 15.8% were ENT and urology surgery record. The mean age of the patients was 34.55 ±11.94 years, and 22.3% were female and 77.7% were male. Forty five nurses who wrote down the notes had an age range of 21 to 50 years old (Table 1).
Table 1.
Nurse’s demographic factors
Findings revealed that opioids were administered more than other drugs that it is contrary to the Iran Ministry of Health and Medical Education guideline (Figure 2). There was a significant relationship between the patient’s sex and type of the medication, using k2 test (p< 0.001). Women administered parenteral opioids more frequently.
Figure 2.
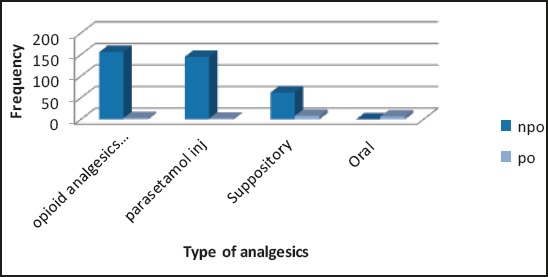
Type Of The Analgesics
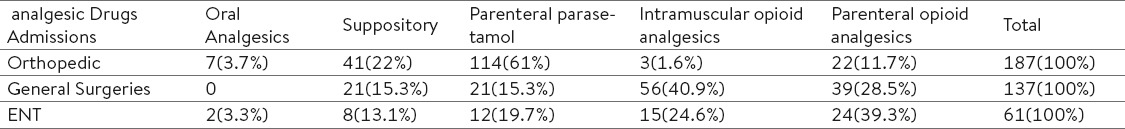
There was a significant relationship between the type of surgery and medication administered (p< 0.001) (Table 2). Pearson correlation test showed a negative relation between the patient’s age and use of opioids. It means that opioid administration reduced in older ages (p< 0.001, r =- 0.214).
Table 2.
Type of the analgesics and type of the surgery
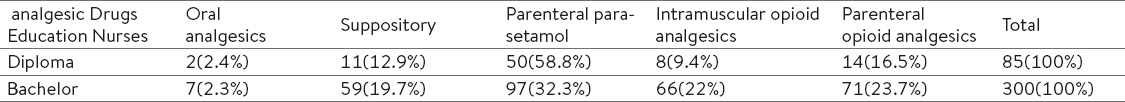
Analysis of the relationship between the nurse’s educational level and compliance with the guideline indicated a significant difference using k2 test (p= 0.01). The compliance of the nurses with a bachelor’s degree was poor and they used opioid medications for the first time after the patient’s pain report (Table 3). In addition, the difference between the nurse’s age and the type of analgesics was significant (p=0.04, r= 0.1). Non opioid analgesic administration was more common among older nurses who were more experienced. Actually, the more experienced the nurse was, the more compliance was observed with the national guideline (p=0.024, r=0.11).
Table 3.
Analgesics drugs and level of nursing education
Symptom and signs related to pain were not mentioned in 281 records (73%) and were less documented at night shifts when tested with spearman regression (p<0.01, r =–0.13). Pain intensity was recorded only in 23 (6%) cases but standard scales were not used for assessing the level of pain intensity. Pain intensity was represented with general terms and subjectively. The patient’s age and pain intensity assessment were positively correlated (p=0.049, r=0.142).
The quality of pain was documented in only 20 patients (5.2%). In contrast, the pain location was documented in almost all of the records. Non pharmacological pain management methods were used in none of the cases. In addition, a correlation was found between the patient’s sex and pain intensity (p= 0.04, r=–0.102) and quality (p= 0.013, r=–0.127) via Kendal test. There was no relationship among the nurse’s sex and education level, pain intensity and quality assessment, and associated symptoms.
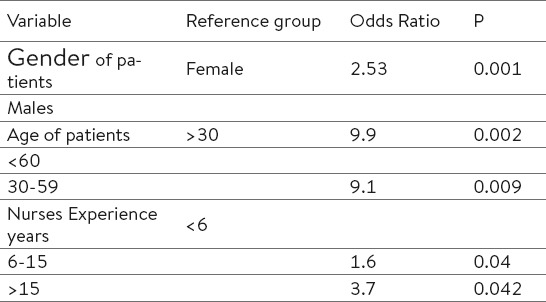
Finally, for estimating the odds ratio and factors affecting the assessment of pain intensity by nurses, a binary logistic and backward method was used. Variations like the patient’s age, sex, and nurse’s experience were introduced to the model after six steps (Table 4). According to the Table 4, the odds of assessing pain in women were 2.53 times more than men. It was also 2.37 times higher in nurses with more than 15 years of working experience than nurses with 6 years of experience or less. Logistic regression was also repeated for pain quality. The patient’s sex was the only variation introduced after six steps. The odds of the assessment of the quality of their pain were 2.62 times higher in women than men.
Table 4.
Results of binary logistic regression for estimating factors that aff ect pain intensity assessment
4. DISCUSSION
Findings showed that opioid analgesics were the most frequent drugs used postoperatively, which is contrary to the guideline. A study by Idvall and Ehrenberg who worked retrospectively on patients’ records by nurses revealed about 73% compliance with the local guideline (21). The reason for this diversity in our study is possibly the unfamiliarity of physicians with the protocol, shortage of knowledge about pain management amongst nurses, and authorities’ lack of concern.
Female patients received more analgesics than male patients in the present study. One possible interpretation is that women usually express their feelings more than men and the other is the homogeneousness of nurses and patients which results in a type of sympathy. Another point of view is that restriction in the relationship of the opposite sexes in the Muslim context can be a potential obstacle for men to complain about their pain to female nurses, especially if they are both young, since 98%of the Iranians are Muslim. The number of the female patients was also higher in our study. Negative misperceptions and biases was introduced a preventive factor for the provision of adequate pain control in other studies as well (22)
Collectively, nurses with bachelor’s degrees did most of the opioid drugs administration that may be due to their engagement in practical aspects and documentation other than nurses with lower levels of education. Moreover, the pain location was recorded in most cases, which was similar to other studies (23, 24). However, the nurses did not use a scale for assessing pain in almost none of the records. It might be the consequence of shortage of knowledge among nurses although assessment is the most important part of pain management. In fact, pain is a subjective experience and reporting the patients’ own words for describing their pain is the best method for documentation (25). Patients usually avoid expressing their pain in the fear of drugs side effects or being popular as the bothering client among busy nurses (26). Chon et.al result was far more different from ours. They found that 45.5% of the nurses used numerical scales for rating the pain level (23). Edder also revealed that 23% of the nurses used scales in patients suffering pain after surgery (27). However, the current results showed the Iranian nurse’s poor function in pain management and documentation.
In our study, only 6% of the records included the intensity of pain using general terms. Guning and Idvall found that 41% of the records in general surgery ward and 6% in thoracic surgery ward included pain intensity (28). They reported that 73% of the concomitant symptoms and 94.8% of quality of pain was not documented by nurses. These statistics represent a huge difficulty for health care personnel in promoting health and quality of life among post-operative patients. Review of the literature suggests that pain should be assessed and document so that it can be understandable for all of team members (21). Scott demonstrated that nursing records of pain would increase patient satisfaction with his or her pain management process. Although sometimes nurses act appropriately to manage patient’s pain but they are too busy to record what they have done in their notes by detail (29). Reports of the pain decreased at night shifts in our study that was similar to the results of a study by Brigs (30).
Nurses’ demographic factors had no relationship with any category of pain management, probably because the nurses are not well trained in this regard in the university and continuing education courses in our country; therefore years of working or age did not influence nurse’s skills for assessment, management and documentation about pain. Some studies identify the lack of formal education nurses receive in pain and pain management (31, 32). While pain assessment and management is taught as part of the curricula of many nursing programs, it is often not enough in terms of time allotted and depth of academic inquiry to be effective (33). It is unfortunately the same in Iran. Thus, it is important to set up educational courses for pain management in the university and then during the work and strict protocols must be followed in hospitals to improve the quality of care in our country.
5. CONCLUSIONS
Nursing documentation concerning postoperative pain management showed many shortcomings in term of content and comprehensiveness. These findings draw attention to the fact that nurses face lack of knowledge in this field. To maintain a professional role in future health care, nurses have to be accountable for their practice and provide good care and information to the patient. To improve the quality of pain management, continuous feedback to clinicians based on record audits may be a useful method. A comprehensive review of the literature suggests that barriers to providing good pain control may be the lack of ongoing educational experience for health care providers and innovations related to the management of pain, advances in pharmacology, and improvements in assessment techniques need to be taught on a regular basis in post-operative care settings (34).
Acknowledgment
Researchers of the Kerman University of Medical Sciences do appreciate the research assistant for their financial support of this research project. They also thank the nurses and hospital archive staff for their collaboration.
Footnotes
• Author’s contribution: All authors in this paper have contributed in all phases in it’s preparing. First author made final proof reading.
• Conflict of interest: none declared.
REFERENCES
- 1.Turk DC, Okifuji A. Psychological factors in chronic pain:evolution and revolution. Journal of consulting and clinical psychology. 2002;70(3):678. doi: 10.1037//0022-006x.70.3.678. [DOI] [PubMed] [Google Scholar]
- 2.Brunner LS, Smeltzer SCC, Bare BG, Hinkle JL, Cheever KH. Brunner & Suddarth's textbook of medical-surgical nursing. Vol. 1. Lippincott Williams & Wilkins; 2010. [Google Scholar]
- 3.Al-Shaer D, Hill PD, Anderson MA. Nurses' knowledge and attitudes regarding pain assessment and intervention. Medsurg nursing:official journal of the Academy of Medical-Surgical Nurses. 2010;20(1):7–11. [PubMed] [Google Scholar]
- 4.Harkreader HC, Hogan MA, Thobaben M. Fundamentals of nursing:caring and clinical judgement:Elsevier Saunders. 2007 [Google Scholar]
- 5.Recart A, Duchene D, White PF, Thomas T, Johnson DB, Cadeddu JA. Efficacy and safety of fast-track recovery strategy for patients undergoing laparoscopic nephrectomy. Journal of Endourology. 2005;19(10):1165–9. doi: 10.1089/end.2005.19.1165. [DOI] [PubMed] [Google Scholar]
- 6.Dunwoody CJ, Krenzischek DA, Pasero C, Rathmell JP, Polomano RC. Assessment, physiological monitoring, and consequences of inadequately treated acute pain. Journal of PeriAnesthesia Nursing. 2008;23(1):S15–S27. doi: 10.1016/j.jopan.2007.11.007. [DOI] [PubMed] [Google Scholar]
- 7.Gillaspie M. Better pain management after total joint replacement surgery:a quality improvement approach. Orthopaedic Nursing. 2010;29(1):20–4. doi: 10.1097/NOR.0b013e3181c8cd32. [DOI] [PubMed] [Google Scholar]
- 8.Gupta A, Daigle S, Mojica J, Hurley RW. Patient perception of pain care in hospitals in the United States. Journal of pain research. 2009;2:157. doi: 10.2147/jpr.s7903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Michaels TK, Hubbartt E, Carroll SA, Hudson-Barr D. Evaluating an educational approach to improve pain assessment in hospitalized patients. Journal of nursing care quality. 2007;22(3):260–5. doi: 10.1097/01.NCQ.0000277784.14310.66. [DOI] [PubMed] [Google Scholar]
- 10.Polomano RC, Dunwoody CJ, Krenzischek DA, Rathmell JP. Perspective on pain management in the 21st century. Pain management nursing. 2008;9(1):3–10. doi: 10.1016/j.pmn.2007.11.002. [DOI] [PubMed] [Google Scholar]
- 11.Mac Lellan K. Postoperative pain:strategy for improving patient experiences. Journal of Advanced Nursing. 2004;46(2):179–85. doi: 10.1111/j.1365-2648.2003.02977.x. [DOI] [PubMed] [Google Scholar]
- 12.Salinas GD, Abdolrasulnia M. Effectiveness of INROADS into pain management, a nursing educational intervention. Journal of continuing education in nursing. 2011;42(7):328–36. doi: 10.3928/00220124-20101201-02. [DOI] [PubMed] [Google Scholar]
- 13.Wysong PR. Nurses' Beliefs and Self-Reported Practices Related to Pain Assessment in Nonverbal Patients. Pain Management Nursing. 2012 doi: 10.1016/j.pmn.2012.08.003. [DOI] [PubMed] [Google Scholar]
- 14.Nursing IoMCotRWJFIotFo. The future of nursing:Leading change, advancing health:National Academies Press. 2011 [PubMed] [Google Scholar]
- 15.Van den Beuken-van Everdingen M, De Rijke J, Kessels A, Schouten H, Van Kleef M, Patijn J. Prevalence of pain in patients with cancer:a systematic review of the past 40 years. Annals of oncology. 2007;18(9):1437–49. doi: 10.1093/annonc/mdm056. [DOI] [PubMed] [Google Scholar]
- 16.Idvall E, Berg A. Patient assessment of postoperative pain management - Orthopaedic patients compared to other surgical patients. Journal of Orthopaedic Nursing. 2008;12(1):35–40. [Google Scholar]
- 17.Taylor A, Stanbury L. A review of postoperative pain management and the challenges. Current Anaesthesia & Critical Care. 2009;20(4):188–94. [Google Scholar]
- 18.Bernatzky G, Presch M, Anderson M, Panksepp J. Emotional foundations of music as a non-pharmacologic pain management tool in modern medicine. Neuroscience and Biobehavioral Reviews. 2011;35:1989–99. doi: 10.1016/j.neubiorev.2011.06.005. [DOI] [PubMed] [Google Scholar]
- 19.Jensen KB, Berna C, Loggia ML, Wasan AD, Edwards RR, Gollub RL. The use of functional neuroimaging to evaluate psychological and other non-pharmacological treatments for clinical pain. Neuroscience letters. 2012;520(2):156–64. doi: 10.1016/j.neulet.2012.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Saeedi M. Investigation on the effects of pain assessment workshop on knowledge, attitude, and practice of nurses in Valie-Asr Hospital in Arak. Modern Care Journal. 2014;10(3):183–91. [Google Scholar]
- 21.Berry PH, Dahl JL. The new JCAHO pain standards:implications for pain management nurses. Pain Management Nursing. 2000;1(1):3–12. doi: 10.1053/jpmn.2000.5833. [DOI] [PubMed] [Google Scholar]
- 22.Pizzo PA, Clark NM. Alleviating suffering 101–pain relief in the United States. N Engl J Med. 2012;366(3):197–9. doi: 10.1056/NEJMp1109084. [DOI] [PubMed] [Google Scholar]
- 23.Chanvej L, Petpichetchian W, Kovitwanawong N, Chaibandit C, Vorakul C, Khunthong T. A chart audit of postoperative pain assessment and documentation:the first step to implement pain assessment as the fifth vital sign in a University Hospital in Thailand. Journal of the Medical Association of Thailand. Chotmaihet thangphaet. 2004;87(12):1447–53. [PubMed] [Google Scholar]
- 24.Ene KW, Nordberg G, Bergh I, Johansson FG, Sjöström B. Postoperative pain management - the influence of surgical ward nurses. Journal of clinical nursing. 2008;17(15):2042–50. doi: 10.1111/j.1365-2702.2008.02278.x. [DOI] [PubMed] [Google Scholar]
- 25.Sloman R, Rosen G, Rom M, Shir Y. Nurses' assessment of pain in surgical patients. Journal of Advanced Nursing. 2005;52(2):125–32. doi: 10.1111/j.1365-2648.2005.03573.x. [DOI] [PubMed] [Google Scholar]
- 26.Manias E, Botti M, Bucknall T. Observation of pain assessment and management - the complexities of clinical practice. Journal of clinical nursing. 2002;11(6):724–33. doi: 10.1046/j.1365-2702.2002.00691.x. [DOI] [PubMed] [Google Scholar]
- 27.Eder SC, Sloan EP, Todd K. Documentation of ED patient pain by nurses and physicians. The American journal of emergency medicine. 2003;21(4):253–7. doi: 10.1016/s0735-6757(03)00041-x. [DOI] [PubMed] [Google Scholar]
- 28.Gunningberg L, Idvall E. The quality of postoperative pain management from the perspectives of patients, nurses and patient records. Journal of nursing management. 2007;15(7):756–66. doi: 10.1111/j.1365-2934.2006.00753.x. [DOI] [PubMed] [Google Scholar]
- 29.Scott IE. Effectiveness of documented assessment of postoperative pain. British journal of nursing (Mark Allen Publishing) 1993;3(10):494–501. doi: 10.12968/bjon.1994.3.10.494. [DOI] [PubMed] [Google Scholar]
- 30.Briggs M, Dean KL. A qualitative analysis of the nursing documentation of post-operative pain management. Journal of clinical nursing. 1998;7(2):155–63. [PubMed] [Google Scholar]
- 31.Abdalrahim MS, Majali SA, Stomberg MW, Bergbom I. The effect of postoperative pain management program on improving nurses' knowledge and attitudes toward pain. Nurse education in practice. 2011;11(4):250–5. doi: 10.1016/j.nepr.2010.11.016. [DOI] [PubMed] [Google Scholar]
- 32.Siedlecki SL, Modic MB, Bernhofer E, Sorrell J, Strumble P, Kato I. Exploring how Bedside Nurses Care for Patients with Chronic Pain:A Grounded Theory Study. Pain Management Nursing. 2013 doi: 10.1016/j.pmn.2012.12.007. [DOI] [PubMed] [Google Scholar]
- 33.Goodrich C. Students' and faculty members' knowledge and attitudes regarding pain management:a descriptive survey. The Journal of nursing education. 2006;45(3):140–2. doi: 10.3928/01484834-20060301-09. [DOI] [PubMed] [Google Scholar]
- 34.Grinstein-Cohen O, Sarid O, Attar D, Pilpel D, Elhayany A. Improvements and difficulties in postoperative pain management. Orthopaedic Nursing. 2009;28(5):232–9. doi: 10.1097/NOR.0b013e3181b579ec. [DOI] [PubMed] [Google Scholar]


