Abstract
The aim:
of the study was to determine the situation of preterm births and early neonatal mortality during 2007-2014 in Tuzla Canton, Bosnia and Herzegovina.
Methods:
The study covers a 8-year period and is based on the protocols at the Tuzla Clinic for Gynecology and Obstetrics that covers all birth in Tuzla Canton area. We analyzed the gestational age of all newborns and recorded the number of neonatal deaths in the first week after birth. Demographics, pregnancy and birth characteristics were collected from the maternal records.
Results:
The total number of births in the period was 32738. Preterm birth was identified in 2401 (7.3%) cases with 12,5% occurring before 32 gestational weeks and 64% in 35-36 gestational weeks. The mothers of the 24-31 gws preterm group were significantly younger that those in the 32-36 group. In the 32-36 group there were significantly greater proportions of mothers with assisted reproductive technology and pre-eclampsia and 16.7% was medical induced preterm births versus 11.4 % in the 24-31 PTB group, p<0.05. The incidence of PTB did no vary significantly during the period, the lowest rate was found in 2010 (6.4%). A total of 221 children died giving a early mortality rate of 6.8 per 1000 live born over the 8 years. The majority 156 dying infants (70.6%) were preterm, only 5.7% died being born in the 35-36 gestational week (5.9 per 1000). Overall the preterm early mortality (7.3 per 1000) has shown a decreasing tendency during the latter years.
Conclusion:
During the last 8 years there have been no significant decline in preterm birth in the Tuzla region while a decline in early neonatal death has been registered.
Keywords: preterm birth, premature, early neonatal mortality
1. INTRODUCTION
Preterm delivery of infants remains one of the most intractable problems that contributes to perinatal morbidity and mortality in obstetric practice in developed countries (1, 2). Preterm births (PTB) account for 75% of perinatal mortality and more than half the long-term infant morbidity (3). Although most preterm babies survive, they are at increased risk of neurodevelopmental impairments and respiratory and gastrointestinal complications (4). Worldwide, the rate of PTB is rising and currently represents 9.6% of all births (5). In the USA, the preterm delivery rate is 12–13%; in Europe and other high income countries, reported rates are generally 5–9% (4,6). Preterm birth is a broad outcome measure resulting from heterogeneous influences. These include infection (25% of PTB), multiple gestations (3% of all pregnancies and 15%–20% of PTB), and induced delivery for medical indications related to maternal or fetal complications such as preeclampsia or growth restriction (30% of PTB) (2). A number of risk factors have been linked to PTB in general, including ethnicity (2), social disadvantage (7), maternal age, infertility (8), multiple births, previous PTB (9), stress (10), maternal smoking (11) and genetic factors (12). Neonatal management has made significant progress in recent years and has resulted in substantial improvement in the outcomes of preterm babies. The diverse etiology of preterm birth makes its prediction difficult. Therapeutic regimens to prevent preterm birth are limited in efficacy. Obstetric and public health interventions aimed at preventing PTB have so far been relatively ineffective (13).
2. THE AIM
The aim of the present study was to evaluate the situation of preterm births and early neonatal mortality during 2007-2014 in Tuzla Canton, Bosnia and Herzegovina.
3. PATIENTS AND METHODS
The study covers an 8-year period (2007-2014) and all the births in Tuzla Canton, Federation of Bosnia and Herzegovina. On the basis of the protocols at the Ob/Gyn Clinic we analyzed all births, preterm births, gestational age of newborns and newborn deaths in the first week after delivery. The demographics, pregnancy and birth characteristics were collected from the maternal records. Tuzla Canton has 510 353 inhabitants and the Ob/Gyn Clinic in Tuzla is the only teaching city hospital which is serving the canton (14).
Preterm birth was defined as birth before 37 completed weeks of gestation. Gestational age in weeks was estimated from the first day of the last menstrual period to the date of birth or from ultrasound examination if performed. If these data were not available, gestational age was assessed on the basis of external physical characteristics of the newborn (15). Early neonatal mortality was defined as the number of liveborn babies who died within the first 7 days after birth. Exclusion criteria included stillbirths and terminations of pregnancy due to lethal fetal anomalies.
The statistical analysis was conducted using the SPSS statistics software (SPSS V.11.5SPSS Inc., Chicago, IL, USA) with the level of significance set at 0.05.
4. RESULTS
Over the 8-year period the total number of births was 32738. Preterm birth was identified in 2401 (7.3%) births. Of the PTBs 12.5% occurred in 24-31 gestational week, while 63.8% in the gestational week of 35-36. There were no significant changes over the years (Figure 1) neither in total frequency of PTB nor in the proportions between the gestational weeks.
Figure 1.
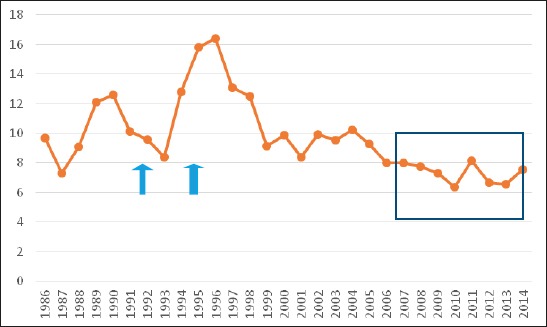
Annual incidence of preterm births in Tuzla canton, Bosnia and Herzegovina in the years 1986-2014 covering the war period (1992-1995) and our study period 2007-2014
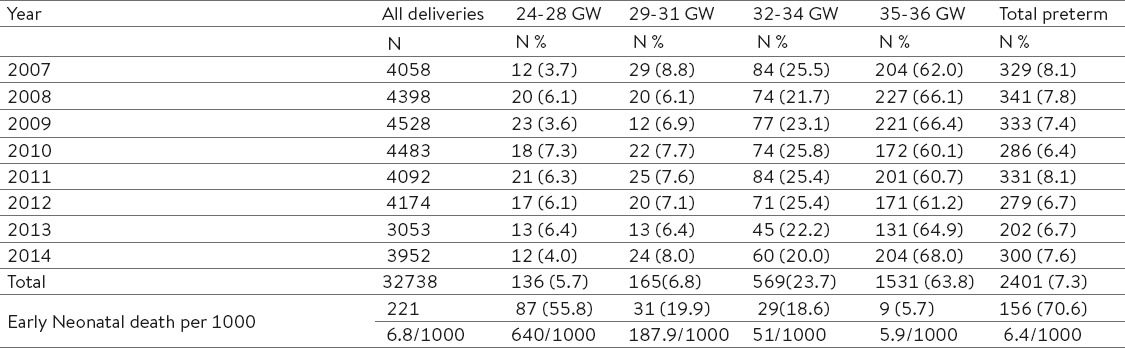
In total 221 death was recorded in early neonatal period giving an overall early mortality rate of 6.4 per 1000 live born over the 8 years (Table 2). The majority–156 dying infants (70.6%) were preterm, only 9 of these died being born in the 35-36 gestational week indicating a early neonatal mortality rate of 5.9 per 1000 born in 35-36 gw which was almost 3 times the mortality rate of term children (65/30337 = 2.1 per 1000). In fact most of the early neonatal death occurred in infants born before gestational week 32. The average early neonatal death was 6.4 per 1000 for all preterm babies.
Table 1.
Demographic and pregnancy characteristics of 2401 preterm birth (PTB) in Tuzla Canton, Bosnia Herzegovina 2008-2014. *ATR- assisted reproductive technology
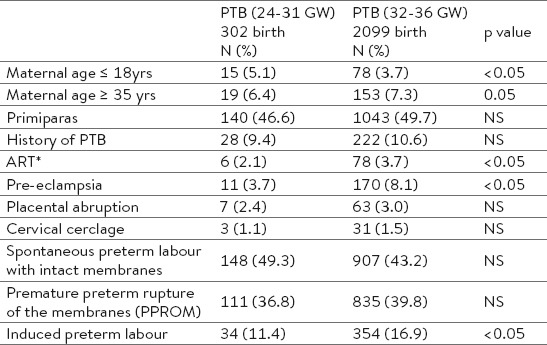
Table 2.
Preterm births in the different gestational weeks during 2007-2014 in Tuzla Canton
By analyzing early neonatal mortality over the years there seems to be a decreasing trend (p<.05) (Figure 2).
Figure 2.
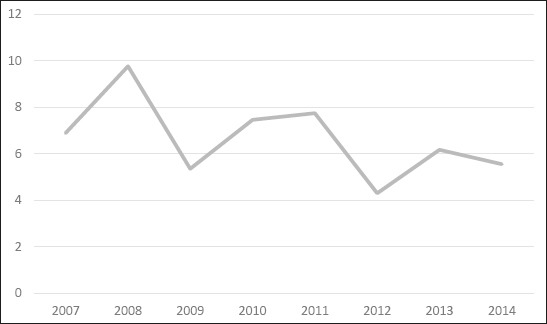
Early neonatal mortality per 1000 for all live birth (32738) in Tuzla Canton
A for the mothers, they were significantly younger in the preterm group with birth between 24-31 gws, while no difference was observed in the mothers above 35 years. The percentage of primiparas were similar in both groups. There were significantly greater proportions of women with assisted reproductive technology and pre-eclampsia in the 32-36 gws PTB group compared to the 24-31 gws PTB group. The proportions of women with placenta praevia, history of preterm birth or cervical cerclage in the groups were not different. The number of induced medical indicated preterm births was significantly highest in the 32-26 gws PTB group (Table 1).
5. DISCUSSION
Our study showed preterm birth rate of 7.3% over the last 8-year period indicating a lower preterm birth rate compared to preterm studies from Europe and other developed countries (2). Furthermore, looking back last 30 years, the PTB rate has been around 10-13% while it increased during the last year of the war period in Bosnia and Herzegovina with the highest incidence (16.4%) in the first post-war year (1996), while in 1997 it was 13.1%. These higher incidences in PTB in post war period occurred in conjunction with markedly increase in number of births and can be explained by the poor economic and social conditions as the result of the war.
In many places of the world, the increase in the preterm birth rate can be explained by rising numbers of indicated preterm births, a high number of preterm multiple gestations associated with assisted reproductive technologies and singleton pregnancies after in-vitro fertilization. In the USA, increasing indicated preterm births mask a small, but important, reduction in spontaneous preterm births (2, 16, 17, 18). By using modern diagnostic methods, we are able to recognize the signs of vulnerability of the foetus early, and are more likely to decide upon termination of pregnancy before the term with the aim of preventing foetal death.
In fact, there may be a reducing threshold for tolerance of maternal and fetal complications leading to induction of early labour.
We found in our study that 16.9% were medically induced preterm births in the 32-36 gws PTB group, which is lower than in previous studies (19). Our mothers in this group had suffered from pre-eclampsia and had conceived by assisted reproductive technology which is in agreement with other studies (19, 20). However, we found that even in the late 35-36 gws PTB group, the early neonatal mortality was 5.7 per 1000 or significantly higher than term children. So we agree with the emerging evidence that late PTB may have a significant adverse effect on neonatal health and long-term sequelae suggesting that we should return to watchful management of pregnancy complications rather than to early delivery at this late gestational age (19).
We found a lower rate of early neonatal mortality compared to the war (1992 and 1994) period, 16.9 and 19.3 per 1000 live births respectively (14). The highest prevalence (9.8 per 1000) in our study period was recorded in 2008. By analysis of our data it was concluded that the cause of death in most cases was respiratory distress syndrome related to prematurity. If we assess early neonatal mortality trends, with the exception of 2008, we can observe a considerable and steady decline. This can be due to a significant improvement in antenatal care and the development of intensive care facilities within our clinic which is in concordance with our previously published reports (14, 21, 22). Prevention of preterm births, especially before 32 gestational weeks, has lead to a significant decrease in neonatal mortality (21). In fact, in our area three out of four death in our preterm groups occurred in the 24-31 gws group.
Despite the considerable improvement in the standard of living, better nutrition of pregnant women, improved medical care, the incidence of children born with low gestation weeks did not significantly change over the observed period. The reason for the high incidence can be explained by the existence of causes that cannot be influenced (placenta previa, placenta abruption, premature rupture of membranes, uterine abnormalities, multiple pregnancy, etc.).
We can notice that the incidence of children born with low gestation weeks is similar to that in Croatia, which to some extent can be explained by similar socio-economic conditions and lifestyle in the two neighboring countries (14).
6. CONCLUSION
During the last 8 years there have been no significant decline in preterm birth in Tuzla region while a decline of early neonatal death has been registered.
Footnotes
• Author’s contribution: All authors in this paper have contributed in all phases in it’s preparing. First author made final proof reading.
• Conflict of interest: none declared.
REFERENCES
- 1.Anon. Practice bulletin ACOG:clinical management guidelines for obstetrician-gynecologists number 31 - assessment of risk factors for preterm birth. Obstet Gynecol. 2001;98:709–16. [PubMed] [Google Scholar]
- 2.Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. Lancet. 2008;371:75–843. doi: 10.1016/S0140-6736(08)60074-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McCormick MC. The contribution of low birth weight to infant mortality and childhood morbidity. N Engl J Med. 1985;312:82–90. doi: 10.1056/NEJM198501103120204. [DOI] [PubMed] [Google Scholar]
- 4.Hamilton BE, Martin JA, Ventura SJ. Births:preliminary data for 2005. Hyattsville, MD: Health E-Stats; 2006. [(accessed July 15 2007)]. http://www.cdc.gov/nchs/products/pubs/pubd/hestats/prelimbirths05/prelimbirths05.htm . [Google Scholar]
- 5.Jennifer J, Henderson, Owen A. McWilliam, John P. Newnham, Craig E. Pennell. Preterm birth etiology 2004–2008. Maternal factors associated with three phenotypes:spontaneous preterm labour, preterm pre-labour rupture of membranes and medically indicated preterm birth. 2012 doi: 10.3109/14767058.2011.597899. [DOI] [PubMed] [Google Scholar]
- 6.Slattery MM, Morrison JJ. Preterm delivery. Lancet. 2002;360:1489–97. doi: 10.1016/S0140-6736(02)11476-0. [DOI] [PubMed] [Google Scholar]
- 7.Morgen CS, Bjørk C, Andersen PK, Mortensen LH, Nybo Andersen AM. Socioeconomic position and the risk of preterm birth–a study within the Danish National Birth Cohort. Int J Epidemiol. 2008;37:1109–20. doi: 10.1093/ije/dyn112. [DOI] [PubMed] [Google Scholar]
- 8.Baird DD, Wilcox AJ, Kramer MS. Why might infertile couples have problem pregnancies? Lancet. 1999;353:1724–5. doi: 10.1016/S0140-6736(99)90050-8. [DOI] [PubMed] [Google Scholar]
- 9.Esplin MS, O'Brien E, Fraser A, Kerber RA, Clark E, Simonsen SE, Holmgren C, et al. Estimating recurrence of spontaneous preterm delivery. Obstet Gynecol. 2008;112:516–23. doi: 10.1097/AOG.0b013e318184181a. [DOI] [PubMed] [Google Scholar]
- 10.Ellman LM, Schetter CD, Hobel CJ, Chicz-Demet A, Glynn LM, Sandman CA. Timing of fetal exposure to stress hormones:effects on newborn physical and neuromuscular maturation. Dev Psychobiol. 2008;50:232–41. doi: 10.1002/dev.20293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kyrklund-Blomberg NB, Cnattingius S. Preterm birth and maternal smoking:risks related to gestational age and onset of delivery. Am J Obstet Gynecol. 1998;179:1051–5. doi: 10.1016/s0002-9378(98)70214-5. [DOI] [PubMed] [Google Scholar]
- 12.Svensson AC, Sandin S, Cnattingius S, Reilly M, Pawitan Y, Hultman CM, Lichtenstein P. Maternal effects for preterm birth:a genetic epidemiologic study of 630,000 families. Am J Epidemiol. 2009;170:1365–72. doi: 10.1093/aje/kwp328. [DOI] [PubMed] [Google Scholar]
- 13.Muglia LJ, Katz M. The enigma of spontaneous preterm birth. N Engl J Med. 2010;362:529–35. doi: 10.1056/NEJMra0904308. [DOI] [PubMed] [Google Scholar]
- 14.Radončić F, Hudić I, Balić A, Fatusić Z. Perinatal outcomes during 1986-2005 in Tuzla Canton, Bosnia and Herzegovina. J Matern Fetal Neonatal Med. 2008;21:567–72. doi: 10.1080/14767050802165935. [DOI] [PubMed] [Google Scholar]
- 15.Farr V, Kerridge DF, Mitchell RG. The value of some external characteristics in the assessment of gestational age at birth. Dev Med Child Neurol. 1996;8:657–60. doi: 10.1111/j.1469-8749.1966.tb01823.x. [DOI] [PubMed] [Google Scholar]
- 16.Ananth CV, Joseph KS, Oyelese Y, Demissie K, Vintzileos AM. Trends in preterm birth and perinatal mortality among singletons:United States 1989 through 2000. Obstet Gynecol. 2005;105:1084–91. doi: 10.1097/01.AOG.0000158124.96300.c7. [DOI] [PubMed] [Google Scholar]
- 17.Jackson RA, Gibson KA, Wu YW, Croughan MS. Perinatal outcomes in singletons following in vitro fertilization:a meta–analysis. Obstet Gynecol. 2004;103:551–63. doi: 10.1097/01.AOG.0000114989.84822.51. [DOI] [PubMed] [Google Scholar]
- 18.Demissie K, Rhoads GG, Ananth CV. Trends in preterm birth and neonatal mortality among blacks and whites in the United States from 1989 to 1997. Am J Epidemiol. 2001;154:307–15. doi: 10.1093/aje/154.4.307. [DOI] [PubMed] [Google Scholar]
- 19.Henderson JJ, McWilliam OA, Newnham JP, Pennell CE. Preterm birth aetiology. 2004-2008. Maternal factors associated with three phenotypes:spontaneous preterm labour, preterm pre-labour rupture of membranes and medically indicated preterm birth. J Matern Fetal Neonatal Med. 2012;25:587–94. doi: 10.3109/14767058.2011.597899. [DOI] [PubMed] [Google Scholar]
- 20.Ananth CV, Vintzileos AM. Epidemiology of preterm birth and its clinical subtypes. J Matern Fetal Neonatal Med. 2006;19:773–82. doi: 10.1080/14767050600965882. [DOI] [PubMed] [Google Scholar]
- 21.Fatusic J, Hudic I, Fatusic Z. Perinatal mortality during fifteen-year period in Tuzla Canton, Bosnia and Herzegovina. Med Arch. 2012;66:258–61. doi: 10.5455/medarh.2012.66.258-261. [DOI] [PubMed] [Google Scholar]
- 22.Skokić F, Muratović S, Radoja G. Perinatal and maternal outcomes in Tuzla Canton during 1992-1995 war in Bosnia and Herzegovina. Croat Med J. 2006;47:714–21. [PMC free article] [PubMed] [Google Scholar]


