Abstract
Introduction:
Wellens Syndrome (WS) is a condition characterized by typical changes in ECG, which are biphasic T-wave inversions (less common) or symmetric and deeply inverted T waves (including 75%) in lead V2–V3 chest derivations. WS is considered important because it has not only diagnostic value but also prognostic value.
Case report:
A 52-year-old male patient without cardiovascular disease or risk factors was admitted to the emergency department (ED) suffering with chest pain and syncope, just after having been involved in a discussion at work. Chest pain was radiating to the left arm and was not precipitated by exertion. Shortness of breath was not accompanied by angina. The patient underwent cardiac catheterization at Department of Cardiology. Stents were positioned in both LADA and a severe lesion in the left main coronary artery. The patient was discharged two days following catheterization, due to no chest pain and hemodynamic instability during the hospitalization. The patient has approved the inform consent for to be used for this case report.
Keywords: coronary artery, Wellens Syndrome, ECG, stents
1. INTRODUCTION
Wellens Syndrome (WS) is a condition characterized by typical changes in ECG, which are biphasic T-wave inversions (less common) or symmetric and deeply inverted T waves (including 75%) in lead V2–V3 chest derivations (1). WS is considered important because it has not only diagnostic value but also prognostic value. Severe negative outcomes may occur, provided that changes in ECG are not rapidly identified, and intervention is not performed (2). Since WS is highly likely to cause anterior myocardial infarction (MI), it is very important that WS is not underdiagnosed. WS patients should be quickly directed to cardiac catheterization within a cardiology department (3). Here we reported a rare case of a WS patient showing a biphasic T-wave under electrocardiogram. Although rare, such cases should not be ignored by emergency physicians.
2. CASE REPORT
A 52-year-old male patient without cardiovascular disease or risk factors was admitted to the emergency department (ED) suffering with chest pain and syncope, just after having been involved in a discussion at work. Chest pain was radiating to the left arm and was not precipitated by exertion. Shortness of breath was not accompanied by angina. He had a history of smoking but no alcohol usage history. The patient’s relatives knew of no history of cardiac events. The patient’s respiratory rate was 18/min, with an oxygen saturation rate of 94% with room air. The patient was asymptomatic during examining. Cardiac and pulmonary auscultations were normal, and vital signs were otherwise within normal limits. A normal sinus rhythm and biphasic T waves in the V2 and v3 derivations were observed in 12 derivation ECG. There was no previous ECG to allow comparison of the current. The patient was placed on O2 support with cardiac monitoring, while proper intravenous access and monitoring were established. Serially measured Troponin-I and cardiac enzyme levels were within normal ranges. The initial high-sensitive cardiac troponin level was 0.008 ng/ml (normal level <0.006 ng/ml). There were no pathological changes seen in the chest x-ray. Finally, because of clinical concerns with initial diagnosis of WS, the patient was referred for consultation to the department of cardiology. There, the patient underwent cardiac catheterization. Stents were positioned in both LADA and a severe lesion in the left main coronary artery (Figure 1). The patient was discharged two days following catheterization, due to no chest pain and hemodynamic instability during the hospitalization. The patient has approved the inform consent for to be used for this case report.
Figure 1.

CAG showing a severe stenosis of the left main coronary artery
3. DISCUSSION
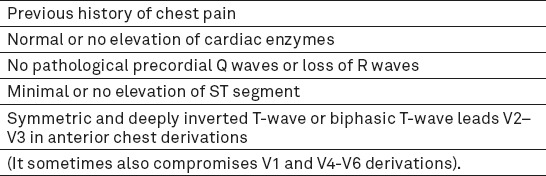
Chest pain is one of the major complaints among patients attending ED. Emergency physicians must be able to evaluate these patients and identifying those with underlying life-threatening causes (4). In patients with possible acute coronary syndrome, ECG is a better predictor of adverse events than either history or presenting symptoms, and it has an important role for emergency physicians in decision-making about discharge. ECG findings in the precordial leads are characteristic for patients with WS. Sometimes WS presents with more subtle changes (5). The aim of reporting this rare case was to underline that WS is a situation presenting with biphasic T wave in electrocardiogram that should not be ignored by emergency physicians. The relationship between severe obstructions of the left anterior descending artery (LADA) and ECG changes in patients who suffer from unstable angina pectoris was first reported by Zwaan et al. in 1982 (6). A related but larger prospective study carried out in 1988 demonstrated that LADA was at least 50% narrowed in all the patients on whom coronary angiography was performed (7). Those studies have demonstrated that up to 87% of the patient populations with isolated precordial T wave inversions in cardiac care units have LADA stenosis reported during angiography. In 1982, Zwaan et al. described a characteristic ECG pattern associated with a serious stenosis of the LADA and impending myocardial infarction. Tilkian first used the term WS to describe the group of ECG findings seen during a painless period of unstable angina pectoris. When pathologic Q waves are not present, these changes in ECG are prognostic of a serious proximal LADA stenosis(6, 7). These changes result from a minimally elevated or isoelectric line ST segment, followed by a concave or straight ST segment and symmetrically biphasic T waves in the precordial leads, particularly in V2–V3 (8). This report is a similar case to that of our patient. WS T wave pattern is valuable in identifying high-risk patients. WS criteria are shown in Table 1. Biphasic T waves in leads V2-V3 in anterior chest derivations of ECG (24% of WS), and symmetrical and deeply inverted T wave in same derivations (76% of WS), are the two types into which WS are divided. The timely recognition of WS is important both for diagnosis and treatment (10). Emergency Physicians (EPs) must be aware of T wave abnormalities in patients who admit to ED suffering chest pain, especially in anterior derivations of ECG. Because the risk of fatal myocardial infarction during testing, these patients should undergo coronary angiography before having an exercise stress test. EPs consider that the differential diagnosis for acute chest pain with similar ECG changes includes myopericarditis and pulmonary embolic disease. In this case we determined that any delay in the recognition of ECG findings could have fatal results. If there any suspicion of WS, it would be better to keep in mind that the risk of anterior myocardial infarction increases over time.
Table 1.
Criteria for Wellens Syndrome
Footnotes
• Conflict of interest: No conflict of interest was declared by the authors.
• Financial Disclosure: The authors declared that this study has received no financial support.
REFERENCES
- 1.Kardesoglu E, Celik T, Cebeci BS, Cingozbay BY, Dincturk M, Demiralp E. Wellens' syndrome: a case report. The Journal of International medical research. 2003;31:585–90. doi: 10.1177/147323000303100615. [DOI] [PubMed] [Google Scholar]
- 2.Basbug HS, Bitargil M, Ozisik K. A case of invisible vena cava filter: Can intravascular implants always be identified? Ulutas Med J. 2015;1(2):44–6. [Google Scholar]
- 3.Parikh KS, Agarwal R, Mehrotra AK, Swamy RS. Wellens syndrome: a life-saving diagnosis. The American journal of emergency medicine. 2012;30:255–5. doi: 10.1016/j.ajem.2010.10.014. [DOI] [PubMed] [Google Scholar]
- 4.Amin AA, Ammar WA, Farrag AA. Impact of glycemic status on left ventricular systolic function in patients with acute coronary syndrome. Ulutas Med J. 2015;1(3):58–63. [Google Scholar]
- 5.Lin KB, Shofer FS, McCusker C, Meshberg E, Hollander JE. Predictive value of T-wave abnormalities at the time of emergency department presentation in patients with potential acute coronary syndromes. Academic emergency medicine. 2008;15:537–43. doi: 10.1111/j.1553-2712.2008.00135.x. [DOI] [PubMed] [Google Scholar]
- 6.de Zwaan C, Bar FW, Wellens HJ. Characteristic electrocardiographic pattern indicating a critical stenosis high in left anterior descending coronary artery in patients admitted because of impending myocardial infarction. American heart journal. 1982;103:730–6. doi: 10.1016/0002-8703(82)90480-x. [DOI] [PubMed] [Google Scholar]
- 7.de Zwaan C, Bar FW, Janssen JH, de Swart HB, Vermeer F, Wellens HJ. Effects of thrombolytic therapy in unstable angina: clinical and angiographic results. Journal of the American College of Cardiology. 1988;12:301–9. doi: 10.1016/0735-1097(88)90398-1. [DOI] [PubMed] [Google Scholar]
- 8.Javillier B, Jacquet C, Legrand V. Wellens syndrome: a poorly known yet significant electrocardiographic entity. Revue medicale Liege. 2012;67:527–30. [PubMed] [Google Scholar]
- 9.Singh B, Singh Y, Singla V, Nanjappa MC. Wellens'syndrome: a classical electrocardiographic sign of impending myocardial infarction. BMJ case report. 2013 doi: 10.1136/bcr-2012-008513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Patane S, Marte F. Wellens'syndrome and other electrocardiographic changes in a patient with a left anterior descending artery subocclusion associated with a left main coronary artery subocclusion. International journal of cardiology. 2011;151:37–41. doi: 10.1016/j.ijcard.2009.03.014. [DOI] [PubMed] [Google Scholar]


