Abstract
Objectives
To determine the feasibility and acceptability of traditional Chinese medicine (TCM) acupuncture and pelvic floor muscle training (PFMT) in reducing symptoms and bothersomeness in women with mixed urinary incontinence (MUI); and to estimate the sample size for a full scale trial.
Methods
Thirty-four women with MUI were randomly assigned to either 12 sessions of TCM acupuncture, 12 sessions of PFMT, or to a waiting list control group. Outcome measures included an assessment of interest to participate in the trial, identification of successful recruitment strategies, the appropriateness of eligibility criteria, and compliance with treatment. Clinical outcomes were assessed at baseline and 12 weeks, and included the International Consultation on Incontinence Questionnaire-Urinary Incontinence-Short Form (ICIQ-UI SF), expectations of treatment effect, and adverse events.
Results
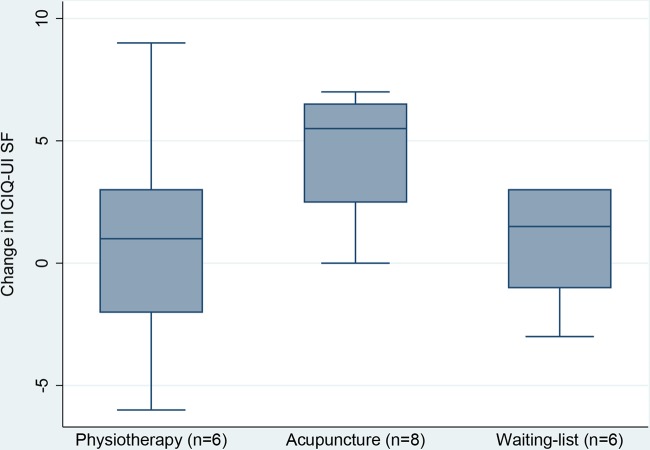
Recruitment was feasible and randomisation worked adequately by means of SurveyMonkey. SurveyMonkey does not permit stratification by ICIQ-UI SF baseline score. Fourteen of 22 women found the treatment options acceptable. The dropout rate was high, especially in the control group (6/12). Outcome forms were completed by 20 of 34 women. The median (IQR) changes of the ICIQ-UI SF scores in the acupuncture, physiotherapy, and waiting list group were 5.5 (2.3 to 6.8), 1.0 (−3.0 to 4.5), and 1.5 (−1.5 to 3.0), respectively, suggesting the need for a full scale trial.
Conclusions
Women with MUI were willing to participate in this study. There is a need for adjusting eligibility criteria. A sample size of 129 women, 43 in three arms, is required. No major adverse events occurred.
Keywords: ACUPUNCTURE, PHYSIOTHERAPY, UROLOGY
Introduction
Urinary incontinence affects women of all ages. The prevalence in Norway is between 20% and 25%,1 2 and one-third have mixed urinary incontinence (MUI).1 MUI is defined as a complaint of involuntary loss of urine associated with urgency, and also with effort on physical activity or exertion, or upon sneezing or coughing.3 MUI is a mix of urgency urinary incontinence and stress urinary incontinence. Between 7%1 and 19%4 of women with urinary incontinence define themselves as bothered with either decreased self-esteem, reduced social life or being less physically active as a result of their urinary incontinence.
The costs associated with urinary incontinence are substantial; about 2% of the healthcare budget in Sweden and the USA is allocated to incontinence problems.5 Urinary incontinence is undertreated and <50% of housebound women seek help for their incontinence, which they believe is part of the ageing process.6
The aetiology of MUI is unclear. Urgency urinary incontinence is characterised by instability of the muscle that empties the bladder, termed detrusor instability. Stress urinary incontinence is characterised by a weakened urethral sphincter or closure mechanisms at the urinary bladder neck. Births, oestrogen deficiency or prolapse of the uterus are often contributing factors, and the condition is most prevalent around menopause, with another peak later in old age.7
The standard treatment of MUI is currently pelvic floor muscle training (PFMT), electrostimulation (biofeedback and feedback), and medication (eg, oestrogens or anticholinergics). Surgery is adequate treatment only for women where leakage during coughing and sneezing are more dominant than the urge symptoms.8
Pelvic floor muscle training
There is level 1 evidence that PFMT is better than no treatment for women with urinary incontinence.9 10
There are no side effects of PFMT, and it has been shown to be cost-effective compared to tension-free vaginal tape surgery.11
Acupuncture
Few scientific studies have found positive effects of acupuncture on different types of urinary incontinence,12–15 although Wang et al16 concluded that more studies are warranted to show whether acupuncture is effective for different types of incontinence. In general, acupuncture is viewed as a safe treatment in the hands of well-qualified practitioners.17
The aim of this pilot study was to estimate an adequate sample size for a full-scale trial, and to investigate the interest to participate in such a trial, the appropriateness of eligibility criteria, and compliance with treatment attendance and completion of outcome forms.
Methods
Study design
A three-armed randomised controlled trial was conducted, comparing 12 sessions of traditional Chinese medicine (TCM) acupuncture in one group, 12 h of PFMT in a second group, including one individual consultation with a specialised physiotherapist before group training, and a waiting list control group for women with MUI. The women were randomised by SurveyMonkey, a web-based survey tool.
Recruitment
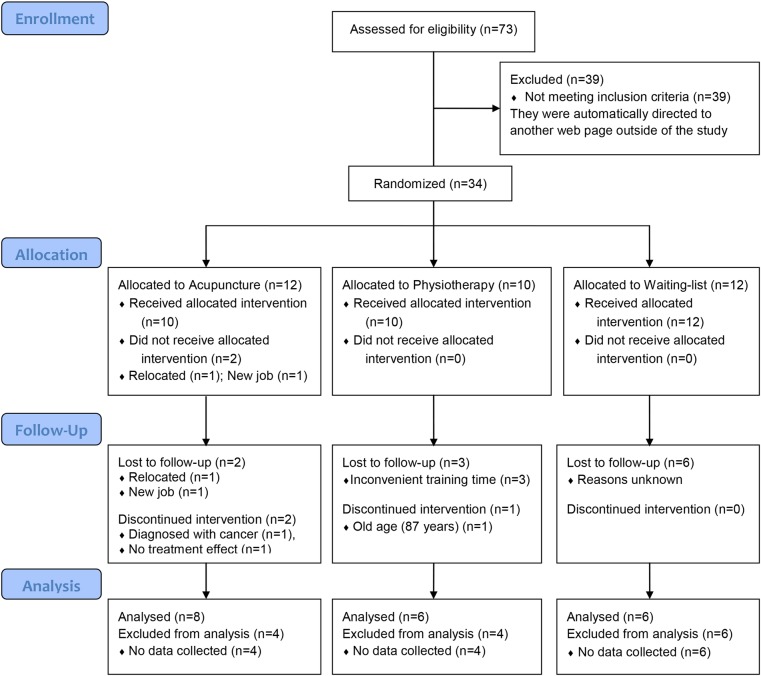
Leaflets in the waiting area in five local medical practices, together with leaflets in local yoga centres, chiropractors, swimming pools, senior centres, and gyms recruited no participants. ‘Tear-out’ leaflets in the changing room in two local gyms recruited only three participants. A note in a newspaper resulted in seven new participants, and 24 women were recruited after an ‘interview article’ with one of the authors (MS) in a local newspaper. Four women were refused because we had reached the planned number of participants we had applied for. Seventy-three unique IP (internet protocol) addresses gave 34 eligible participants (figure 1).
Figure 1.
Flowchart of the study.
In all, 34 women with MUI who lived in the Oslo area in Norway were recruited in August and September 2012. The median age of the participants was 62.5 years (range 29–87 years) (table 1).
Table 1.
Baseline characteristics of the study participants
| Treatments | ||||
|---|---|---|---|---|
| Acupuncture | Physiotherapy | Waiting list | p Value | |
| n | 12 | 10 | 12 | |
| Median (range) | ||||
| Age (years) | 66 (31 to 80) | 63.5 (40 to 87) | 52.5 (29 to 76) | 0.49 |
| Weight (kg) | 66 (52 to 93) | 67 (48 to 80) | 66 (53 to 120) | 0.91 |
| Height (cm) | 169 (158 to 174) | 167 (157 to 177) | 169 (158 to 178) | 0.57 |
| Number of births | 2 (0 to 3) | 2 (0 to 4) | 2 (0 to 3) | 0.21 |
| ICIQ-UI SF baseline | 13 (4 to 14) | 6 (5 to 12) | 10.5 (6 to 16) | 0.02 |
ICIQ-UI SF, International Consultation on Incontinence Questionnaire-Urinary Incontinence-Short Form.
Inclusion and exclusion criteria
All women above 18 years of age with MUI, who were not pregnant or planning to become pregnant during the study, were considered eligible for inclusion. Women who had given birth within 12 months before the onset of the current study were excluded. Women using medication for the urinary incontinence, or who had undergone surgery for incontinence, were not eligible.
Enrolment in SurveyMonkey
SurveyMonkey is a web-based survey tool that includes semi-structured and structured templates. We added the International Consultation on Incontinence Questionnaire-Urinary Incontinence-Short Form (ICIQ-UI SF) to a semi-structured template. This template included boxes for inclusion criteria, exercise diary, questions about expectation of treatment effect, adverse events, satisfaction with the treatment, and whether the women would recommend the treatment for others with MUI (the latter three in questionnaire 2, after 12 weeks). SurveyMonkey supplies a unique web address for all surveys. This address was referred to in the recruitment channels. If a woman did not meet eligibility criteria because, for example, she had stress urinary incontinence and not MUI, she was automatically directed to a separate page outside the study before entering her name and contact.
Consent was obtained first by ticking a box in the web survey, and then again with a signed consent form at the start of treatment with acupuncture or PFMT.
Randomisation
All women meeting the inclusion criteria were randomly assigned to the treatment groups using the SurveyMonkey tool. Four women were not internet users. They answered the questions by phone, and results were manually entered into SurveyMonkey by the first author (MS) before randomisation.
Interventions
Acupuncture group
Eight women received 12 sessions of TCM-based acupuncture within 12 weeks by an acupuncturist (MS) who had 4 years of full-time training and 9 years of clinical experience as an acupuncturist. The treatment regimen reflected the ‘real world’; hence some women came for treatment once a week, and others twice a week and then not for a month. The medical history was taken using a TCM interview based on the four interrogations, and the diagnostic system of pattern identification named eight principles. The points used were semi-standardised with alternation between front and back points. The points selected were based on four sources.16 18–20 CV3, CV4, CV6, SP6, KI 3, KI7 (PC6, LR3 and SP3 with related symptoms) were used with patients in a supine position, and BL 31–34, BL 23, BL 28, SP6, GV4 and GV20 (forward needling) (BL 14, 18 and 20 with symptoms) were used when the patient was in prone position. Sterile, disposable, silver needles (Pharma West) were used, size 0.25 mm×25 mm and 0.25 mm×40 mm. After insertion, de qi was obtained in all needles, and de qi was obtained once more during the 30 min the needles were in situ. The needles were inserted to a depth in accordance with ‘A Manual of Acupuncture’.20
Pelvic floor muscle training group
Six women received one individual consultation with a specialist trained female physiotherapist before 12 weekly sessions of PFMT in their group. The individual consultation included vaginal examination to verify that the correct procedure of using the pelvic floor muscles was obtained. The regional ethics committee approved this procedure for this pilot study, and had no objection to this being performed. A systematic review shows that it is important that qualified personnel properly instruct the women, as 30% of them press downwards instead of lifting the pelvic floor muscles.6 The women were free to ask questions during the individual consultations, but also before and after each group session of PFMT. The exercises for the pelvic floor muscles takes approximately 25 min, following a general exercise programme for 20 min.6 The women wrote an exercise diary every day, which also included PFMT for 10 min a day.
Waiting list group
The women randomised to this group received no treatment, and were asked to fill in the questionnaires after 12 weeks. At the end of this trial they were offered a choice of either acupuncture or PFMT for free, and this was stated in the information leaflets and the first questionnaire. Of the six women completing the forms, two chose PFMT and two chose acupuncture, and two did not want treatment due to their working hours and change of work.
Outcome measures
ICIQ-UI SF is a well validated self-reporting outcome form translated into 38 languages.21 Both the National Institute for Health and Care Excellence (NICE) guidelines22 and the International Consultation on Incontinence (ICI) guidelines23 recommend the use of level 1 forms for research purposes on urinary incontinence. Urodynamic testing is no longer required for the diagnosis. ICIQ-UI SF takes less than 5 minutes to fill in and it has been tested for responsiveness to both surgery and PFMT interventions, but not acupuncture interventions.
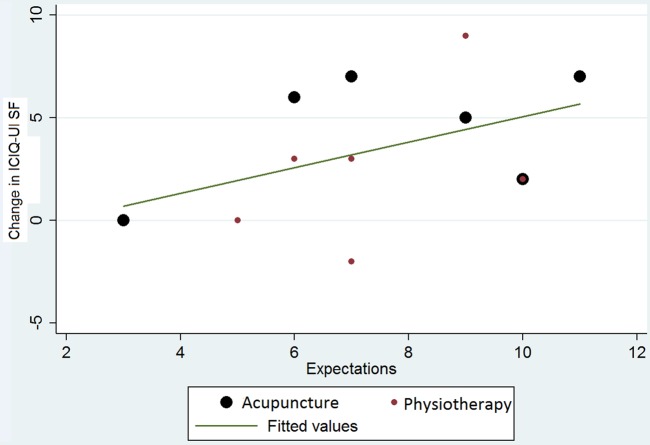
Correlation between expectations and the results after treatment
The expectations of treatment effect were measured using the following questions: (1) To what degree do you think acupuncture can help for your urinary incontinence? (2) To what degree do you think PFMT can help for your urinary incontinence? This was measured on a linear scale with values ranging from 1 to 11, 1 meaning ‘not at all’ and 11 meaning ‘to a large extent’.
Sample size and data analysis
As this was a pilot trial, it was estimated that 34 women would be sufficient to answer our questions on feasibility and to estimate a proper sample size for a full scale trial. SPSS V.22 was used for data analysis. SurveyMonkey encrypts the file before transferring it to SPSS.
The Kruskal-Wallis test was used to determine if there were statistically significant differences between the three treatments of the ICIQ-UI SF.
Results
Recruitment was judged feasible once a successful recruitment strategy was established. Seventy-three women wanted to attend (plus four more after closing inclusion), and of these 34 met the eligibility criteria. Randomisation worked adequately by means of SurveyMonkey. It was not possible to stratify by baseline ICIQ-UI SF score.
The number of dropouts was high in all groups: 50% in the waiting list group, 40% in the physiotherapy group, and 25% in the acupuncture group. Once the women had started the interventions, compliance was high in the physiotherapy and acupuncture groups, and the questionnaires were completed properly. In order to perform the power calculation of the full-scale study, the mean value of ICIQ-UI SF (N=34) was calculated to be 10.37 (SD 3.42). Clinical relevance is regarded as an improvement of 3 units on a scale of 0–21. With 80% power, a significance level of 5%, and an expected dropout rate of 20%, 129 women will need to be included in a full-scale three-armed trial, thus requiring 43 in each group.
Clinical outcome: ICIQ-UI SF
For clinical outcome see table 2 and figure 2.
Table 2.
Results of the Kruskal-Wallis H test comparing changes in ICIQ-UI SF in the three treatments
| Treatments | ||||
|---|---|---|---|---|
| Acupuncture | Physiotherapy | Waiting list | p Value | |
| Median (IQR) | ||||
| ICIQ-UI SF at end point | 6.5 (4.5 to 8.5) | 5.0 (3.0 to 8.3) | 10.0 (6.0 to 13.3) | 0.12 |
| ICIQ-UI SF change score | 5.5 (2.3 to 6.8) | 1.0 (−3.0 to 4.5) | 1.5 (−1.5 to 3.0) | 0.10 |
ICIQ-UI SF, International Consultation on Incontinence Questionnaire-Urinary Incontinence-Short Form.
Figure 2.
Boxplot showing International Consultation on Incontinence Questionnaire-Urinary Incontinence-Short Form (ICIQ-UI SF) change score in the three groups.
Expectations versus ICIQ-UI SF change score
Higher expectations for the two treatments at baseline were associated with higher values on the change score.
Adverse events
Adverse events were measured with two questions in SurveyMonkey at the endpoint: (1) Have you had any adverse events with treatment? (open box to answer); and (2) Did you perceive any worsening of symptoms of urinary leakage in the beginning of treatment? Answering options were: Yes, No, and Do not know. One woman in the acupuncture group got tired right after treatments. One woman in the acupuncture group and one in the PFMT group perceived more urinary incontinence symptoms after the first few treatments. This decreased as treatment persisted.
Discussion
The aims of this pilot study were to estimate the adequate sample size for a full-scale trial, and investigate the interest to participate in such a trial, the appropriateness of eligibility criteria, and compliance with treatment attendance and successful completion of outcome forms.
The questionnaires functioned adequately and all questions were filled in accordingly. SurveyMonkey worked adequately as a randomisation tool, but it was not feasible to stratify or cluster the randomisation based in the ICIQ-UI SF median score at baseline, resulting in the present difference in baseline score (table 1). In a full-scale trial, the groups would be more likely to be similar due to the effect of randomisation of more women. A difference in ICIQ-UI SF baseline score between the groups should be avoided, because we do not know if the severity of urinary incontinence matters for the treatment effect.
Dropout rates were high in all groups (see flowchart in figure 1). Three of the four dropouts in the physiotherapy group dropped out before attending the first session, due to the inconvenient training time of 09:00. Hence in a full scale trial we will offer women PFMT both in the morning and evening. Another woman, aged 87 years, dropped out after her first session of PFMT because she was not able to exercise. Of the six women who completed PFMT, four attended 12 sessions of PFMT, one attended 11, and one attended 10 sessions. All women completed the training diary of 10 min PFMT at home every day.
In the acupuncture group, only two women withdrew during the study, one due to no effect, and the other due to cancer. A further two dropped out before treatment, leaving eight women completing 12 sessions of acupuncture during 12 weeks. Once the women had started both treatments, the compliance was high in both groups, suggesting that the interventions should be kept as they are in a full-scale trial.
There is a need for better motivation especially in the waiting list group. This can be done by regular phone contact during the study by the investigator, including better explanation and provision of information throughout the study on the importance of their answers.
The acupuncture intervention being flexible for treatment time during the 12 weeks is compatible with a pragmatic approach. We think that this is close to everyday practice, and necessary for motivating the women in the trial to complete it.
In planning for a larger study, better information should be provided to all groups, adding an exclusion criterion of vaginal bleeding after menopause (cancer was detected in two women during this pilot) and offering two classes of PFMT a week (more compatible with working hours) to help reduce dropout.
Higher expectations for the treatments were associated with higher outcome scores in both the acupuncture and physiotherapy groups (figure 3). This may suggest that what the women think of the treatment before attending PFMT and acupuncture is important for the results of the treatment when it comes to MUI. This finding is supported by other acupuncture trials on chronic pain24 and menopause.25 The second question concerning adverse events─whether the urinary incontinence symptoms worsened at the beginning of treatment─was included because, to our knowledge, this has not been measured for PFMT before. One woman in both treatment groups perceived a worsening of incontinence symptoms after the first two treatments, but this disappeared as treatment persisted.
Figure 3.
Regression on expectations and changes in International Consultation on Incontinence Questionnaire-Urinary Incontinence-Short Form (ICIQ-UI SF).
This study has limitations. Firstly, we had too short a follow-up period. The effect of treatment should be measured immediately after and then at 6 months and 1 year after the intervention, to see if the intervention effects persist, and also to see whether any of the participants are continuing to undertake treatment on their own. A 3-year follow-up would be the best. This is also important for the cost-effectiveness comparison we want to perform following a full-scale trial.
A three-day bladder diary will be used in a full-scale trial, to perceive objective measurements as suggested by the NICE guidelines of 2013.22
This trial could be biased by the fact that the acupuncturist and the investigator were the same person. In a full-scale trial with funding, this will not occur.
Conclusion
Recruitment was feasible and randomisation worked adequately by means of SurveyMonkey. Adding regular phone contact during the study by the investigator to the waiting list group, introducing evening classes of PFMT and acupuncture, and adding menopausal bleeding to the exclusion criteria and general health to be able to perform PFMT to the inclusion criteria will all help in reducing dropout. The sample size for a full-scale three-armed trial was estimated at 129 women with 43 in each group. Further research is warranted in terms of determining which treatment is most effective for reducing symptoms and bothersomeness of MUI (table 2 and figure 2).
Footnotes
Twitter: Follow Atle Klovning at @atleklovning
Contributors: MS initiated the study, AK and TA helped in planning the study. IM and MS performed the statistical analysis, and all authors contributed to the initial draft of the manuscript and to its final version.
Funding: The Norwegian Acupuncture Association funded open access fee.
Competing interests: None declared.
Patient consent: Obtained.
Ethics approval: 2012/912/REK sør-øst D
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Because this is a pilot study, this is the only work that will be published from this data.
References
- 1.Hannestad YS, Rortveit G, Sandvik H, et al. A community-based epidemiological survey of female urinary incontinence: the Norwegian EPINCONT study. Epidemiology of Incontinence in the County of Nord-Trondelag. J Clin Epidemiol 2000;53:1150–7. 10.1016/S0895-4356(00)00232-8 [DOI] [PubMed] [Google Scholar]
- 2.Klovning A, Sandvik H, Hunskaar S. Web-based survey attracted age-biased sample with more severe illness than paper-based survey. J Clin Epidemiol 2009;62:1068–74. 10.1016/j.jclinepi.2008.10.015 [DOI] [PubMed] [Google Scholar]
- 3.Haylen BT, De Ridder D, Freeman RM, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn 2010;29:4–20. [DOI] [PubMed] [Google Scholar]
- 4.Perry S, Shaw C, Assassa P, et al. An epidemiological study to establish the prevalence of urinary symptoms and felt need in the community: the Leicestershire MRC Incontinence Study. J Public Health Med 2000;22:427–34. 10.1093/pubmed/22.3.427 [DOI] [PubMed] [Google Scholar]
- 5.Reeves P, Irwin D, Kelleher C, et al. The current and future burden and cost of overactive bladder in five European countries. Eur Urol 2006;50:1050–7. 10.1016/j.eururo.2006.04.018 [DOI] [PubMed] [Google Scholar]
- 6.Bø K. Bekkenbunnstrening og urininkontinens - tren deg tett! Tidsskrift for den Norske laegeforening: tidsskrift for praktisk medicin, ny raekke 2000;120:3583–9. [PubMed] [Google Scholar]
- 7.Klovning A. Validations of research methods for urinary incontinence in women. Bergen, Norway: University of Bergen, 2010. [Google Scholar]
- 8.Kulseng-Hanssen S, Husby H, Schiotz HA. Follow-up of TVT operations in 1,113 women with mixed urinary incontinence at 7 and 38 months. Int Urogynecol J Pelvic Floor Dysfunct 2008;19:391–6. 10.1007/s00192-007-0449-y [DOI] [PubMed] [Google Scholar]
- 9.Herderschee R, Hay-Smith EJ, Herbison GP, et al. Feedback or biofeedback to augment pelvic floor muscle training for urinary incontinence in women. Cochrane Database Syst Rev 2011;6:CD009252. [DOI] [PubMed] [Google Scholar]
- 10.Greer JA, Smith AL, Arya LA. Pelvic floor muscle training for urgency urinary incontinence in women: a systematic review. Int Urogynecol J 2012;23:687–97. 10.1007/s00192-011-1651-5 [DOI] [PubMed] [Google Scholar]
- 11.Bø K. Is there still place for physiotherapy in the treatment of female incontinence? EAU Update Series 2003;1:145–53. 10.1016/S1570-9124(03)00037-0 [DOI] [Google Scholar]
- 12.Bergstrom K, Carlsson CP, Lindholm C, et al. Improvement of urge- and mixed-type incontinence after acupuncture treatment among elderly women—a pilot study. J Auton Nerv Syst 2000;79:173–80. 10.1016/S0165-1838(99)00077-6 [DOI] [PubMed] [Google Scholar]
- 13.Emmons S, Otto L. Acupuncture for overactive bladder: a randomized controlled trial. Obstet Gynecol 2005;106:138–43. 10.1097/01.AOG.0000163258.57895.ec [DOI] [PubMed] [Google Scholar]
- 14.Song FJ, Zhang H, Zheng SL, et al. [Research review on apoplectic urinary incontinence treated with acupuncture-moxibustion in recent 5 years]. Zhongguo Zhen Jiu 2011;31:957–60. [PubMed] [Google Scholar]
- 15.Engberg SC, Cohen S, Sereika SM. The efficacy of acupuncture in treating urge and mixed incontinence in women: a pilot study. J Wound Ostomy Continence Nurs 2009;36:661–70. 10.1097/WON.0b013e3181bd82dd [DOI] [PubMed] [Google Scholar]
- 16.Wang Y, Zhishun L, Peng W. Acupuncture for stress urinary incontinence in adults. Cochrane Database Syst Rev 2013;7:CD009408 10.1002/14651858.CD009408.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Melchart D, Weidenhammer W, Streng A, et al. Prospective investigation of adverse effects of acupuncture in 97 733 patients. Arch Intern Med 2004;164:104–5. 10.1001/archinte.164.1.104 [DOI] [PubMed] [Google Scholar]
- 18.Heyerdahl O, Lystad N. Tradisjonell kinesisk akupunktur. Dens filosofi og anvendelse i moderne medisin. Trondheim: Wennberg Trykkeri AS, 2000:396p. [Google Scholar]
- 19.Maciocia G. Obstetrics and gynecology in Chinese medicine. 2nd edn. New York: Churchill Livingstone, 1999. [Google Scholar]
- 20.Deadman P, Al-Khafaji M. A manual of acupuncture, 2 edn. Press NAbE, editor Oxford, England: Journal of Chinese Medicine, 2007. [Google Scholar]
- 21.Coyne K, Kelleher C. Patient reported outcomes: the ICIQ and the state of the art. Neurourol Urodyn 2010;29:645–51. 10.1002/nau.20911 [DOI] [PubMed] [Google Scholar]
- 22.National Collaborating Center for Women's and Children's Health. Urinary incontinence: the management of urinary incontinence in women. Royal College of Obstetricians and Gynaecologist, 2013.
- 23.Abrams P, Andersson KE, Birder L, et al. Fourth International Consultation on Incontinence Recommendations of the International Scientific Committee: evaluation and treatment of urinary incontinence, pelvic organ prolapse, and fecal incontinence. Neurourol Urodyn 2010;29:213–40. 10.1002/nau.20870 [DOI] [PubMed] [Google Scholar]
- 24.Linde K, Witt CM, Streng A, et al. The impact of patient expectations on outcomes in four randomized controlled trials of acupuncture in patients with chronic pain. Pain 2007;128:264–71. 10.1016/j.pain.2006.12.006 [DOI] [PubMed] [Google Scholar]
- 25.Borud E. The ACUFLASH study. Acupuncture treatment for postmenopausal hot flashes: can traditional Chinese acupuncture in addition to self-care reduce hot flash frequency and intensity, compared with self-care alone? UiT Norges Arktiske Universitet, 2010. [Google Scholar]