Abstract
Introduction:
embarrassed emotional experience may affect the ability to oncology patient effectively cope with cancer, symptoms and treatment. Distress extends a long period, from common, normal feelings of vulnerability, sadness and fears to problems of PTSD, depression, anxiety, panic, social isolation and the perception of spiritual crisis. The aim of the research is to determine the level of distress and PTSD in cancer patients.
Patients and Methods:
In a prospective, cohort study cases from 2011- 2014 were included patients with cancer who are treated under the supervision of his chosen family medicine doctor. Including a factor for the participation of patients in the study is that from the moment of diagnosis of malignant disease passed <12 months. The total sample was 174 of the planned 200 (response rate=87%). The subjects were divided into three groups. A key factor in the creation of the group was the time elapsed from the moment of acknowledgment and confirmation of the diagnosis: T1 <14 days, n=56 patients; T2>14 days-<6 months, n=79 patients; T3>6 months n=39 patients. To achieve the set goals of the research was used instruments of 3 questionnaires: Questionnaire on the clinical characteristics of patients with malignant disease, demographic and individual characteristics; questionnaire distress oncology patient–hospital scales of depression and anxiety, HADS scale (Hospital Anxiety and Depression Scale - HADS) and a rapid test for self-assessment of the symptoms of PTSD.
Results:
Age of patients was 54.63 ± 11:46 years, and the age of the respondents when they were diagnosed with cancer 54.34 ± 11.26 years. The prevalence of distress was a high 76% 82x higher than expected), and PTSD 55%. Predictors of burnout syndrome in cancer patients are all important determinants of malignant disease: the time elapsed since the diagnosis of the disease which determines the clinical status of malignant disease (β=0.280; P=0.001; 95% CI, 0742-2259), discovered metastases (β=0.304; P=0.001; 95% CI -2621 to 0978) and treatments (β=0.160; P=0.031, 95% CI 0050 to 1.060).
Conclusion:
The problem of distress in cancer patients is widespread and has a high prevalence of 76% in our environment, while still absent intervention and treatment.
Keywords: distress, post-traumatic stress disorder, cancer patients, psycho-oncology
1. INTRODUCTION
Distress, post-traumatic stress disorder (PTSD) and depressive disorders are common in cancer, but are unfortunately often unrecognized and untreated (1). Many researchers have come to the conclusion that the oncology patients common difficulty expressing emotions, inability to open expression of aggression and suppression of depressive moods. In short, these people are well adapted to others, and alienated from himself (2-3). One third of patients with cancer develops a mental disorder for which there is a necessity of treatment (4). Diagnosing mental disorders is difficult because the clinical picture superimposed psychic and somatic symptoms, particularly in relation to pain (2). Patients are often anxious, but at the time they submit to treatment when a doctor suspected malignant disease (5). These insights have developed a new medical discipline of psycho-oncology. It was first on the psychological impact of cancer spoken in 1970 in the United States (US). Psycho-oncology can be viewed in terms of two dimensions. The first examines the psychological reactions of patients in all stages of the disease, as well as family members and oncology healthcare staff. The second refers to the study of psychological, social and behavioral risk factors that influence the course of the disease itself, metastases and survival (2). Centuries old stigma about cancer prevents patients to talk about their diagnosis, but also slows down the development of psycho-oncology (3). A first encounter with the diagnosis of malignant disease puts people in intense emotional reactions than in the encounter with any other disease. The assumption is that the knowledge that a patient suffering from cancer as a direct threat to life and early death, represents the exposure to catastrophic traumatic event or stressor strong high intensity that results in acute stress reaction or powerful stressor exposure acute catastrophic situation (7-9). At the moment of awareness of his cancer, the patient must use a series of adaptive defense to maintain psychological balance. The situation is comparable to dealing with death. Under the influence of stress will weaken the defense forces of the organism in which not only important intensity stressors, but also a person’s ability to cope with it (9). The aim of the research is to determine the level of distress and PTSD in cancer patients.
2. METHODS AND SUBJECTS
In a prospective, cohort study of the case of the 2011 -2014 were included patients with cancer who are treated under the supervision of his chosen family doctor/family medicine in Tuzla, Zivinice and Celic. Including a factor for the participation of patients in the study is that from the moment of diagnosis of malignant disease passed <12 months. The total sample size was n = 200, and the participation is voluntarily them n = 174 (response rate in the study, 87%, 174 of 200). The survey was conducted by interviewing, and survey instrument were questionnaires. The subjects were divided into three groups. A key factor in the creation of the group was the time elapsed from the moment of acknowledgment and confirmation of the diagnosis of disease: T1 <14 days; T2> 14 days- <6 months; T3> 6 months questionnaire, used in this study, the subjects filled in anonymously with the help of FM team or caregivers. The criteria for exclusion of patients from the study were cancer patients who were diagnosed chronic psychiatric illness that needed monitoring and treating psychiatrist in >3 different time intervals. To achieve the set goals of the research was used instruments of 3 questionnaires: Questionnaire on clinical characteristics of malignant disease patients with demographic and individual characteristics; questionnaire distress oncology patients, hospital scales of depression and anxiety, HADS scale (Hospital Anxiety and Depression Scale) (10) and a rapid test for self-assessment of the symptoms of PTSD (11). HADS scale measures distress in cancer patients, anxiety and depression. For cancer specific questionnaire consists of two subscales: subscale anxiety and depression subscale. It contains 14 items that describe potential everyday stress in cancer patients in all spheres of life. The answers to every problem item-respondents can answer in two ways according to the Likert scale of 1-4 (never, rarely, usually, almost always) (13). Answers to questions 2,4,7.9, 12 and 14 are inverted. Score distress to questions 1.3.5., 6, 8,10,11,13 8-16 = (a) + score of distress for questions 2,4,7,9,12,14 = 18-23 (HADS b) score distress HADS first distress 8-16 points 2. Not> 17 points; Distress score a first distress 18-23 points 2. Not <17 points (10). A short (“quick”) PTSD questionnaire contains 13 questions drafted in a yes or negation (11). Statistical analysis was made by SPSS 18.0 (Chicago, IL, USA) and MedCalc 9.2.0.1 (MedCalc, Belgium). There have been basic tests of descriptive statistics, showing the measures of central tendency and dispersion. By comparing the two average values will be, given the nonparametric distribution variables was performed using the Mann-Whitney test. Quantitative variables if necessary comparisons 3 mean values were conducted one-way ANOVA, where the same were distributed by the normal distribution. For variables that were not distributed by the normal distribution was used nonparametric alternative - Kruskal-Wallis test. Categorical variables were analyzed by χ2-test. It was used Spearman correlation test and multiple logistic regression analysis to test the predictive potential demographic (individual) characteristics and medical characteristics of the disease, the value of HADS and PTSD. All statistical tests were carried out with a level of statistical probability of 95% (p <0.05).
3. RESULTS
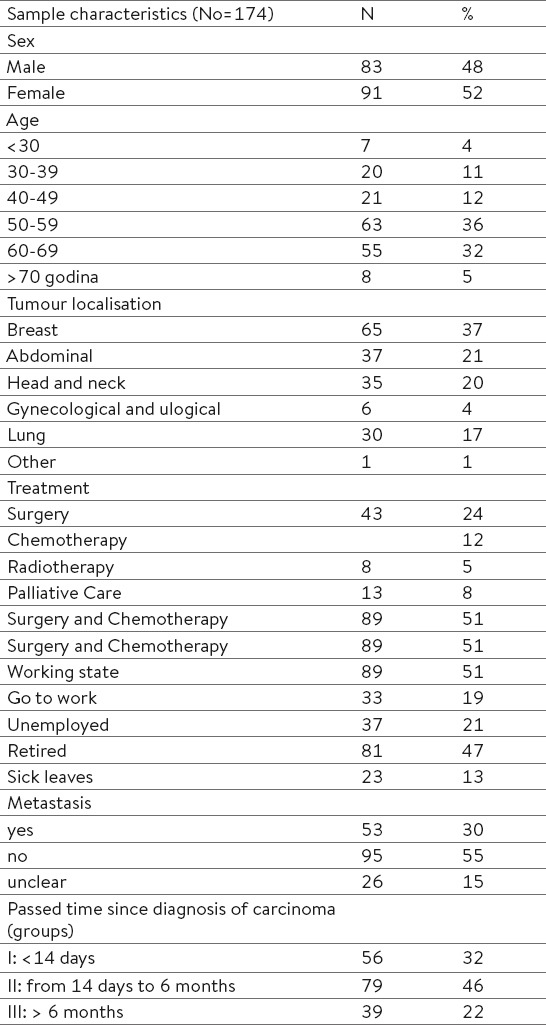
In the total sample (N = 200), adequate answers to the questionnaires gave the 174 participants, 83 men and 91 women (response rate = 87%). Among them were 91 women (51%) and by gender no statistically significant differences between subjects (P = 0.332). The mean age of patients was 54.63 ± 11:46 years, and the mean age of the respondents when they were diagnosed with cancer 54.34 ± 26.11 years. The most common cancer in our patients are breast cancer n = 65 (37%), malignant diseases of stomach body n = 37 (21%), the incidence of malignant neoplasms unexpected cranium n = 35 (20%) and lung n = 30 (17%) and only n = 6 (3%) are malignant diseases of the genitourinary tract. But in the age of 28- 35 years we found: 3 cases of breast cancer, 7 cases of lung cancer and 6 malignancies cranium. Among the sick unemployed is 21%, and 47% of retired respondents. Metastases are not developed in 55% of cases. Most patients were treated with combined chemotherapy and surgical treatment 89 (51%), only operative treatment had 43 (24%) patients, and oncology radiotherapy was used in 8 (5%) of the respondents. Palliative care is treatment in 13 (8%) respondents. The first group consists of 56 subjects where the knowledge from the moment they are suffering from malignant diseases have been less than 14 days. The second group includes respondents who have cancer for a period of 14 days to 6 months, 79 (Group II), and III group 39 patients whose disease has a history of more than 6 months (Table 1).
Table 1.
Sample Characteristics
The most common perception of distress of cancer patients reported in the perception of discomfort in the stomach 63%; do not care about their appearance 61%; emotionally and physically exhausted as they are burnout (60%); feel they were stopped and captured 58%; have the discomfort associated with a feeling that should be on the move (58%); suddenly feel the panic 57% and were constantly worried about 46%. With fearful anticipation of the worst present in 31% of subjects. Self-motivations to help them in a situation of distress and burnout are sometimes: enjoy everyday things 50%, laughing and looking at things from the bright side, 67%, are full of life 72%, it is easy to settle down and relax 47%, let them rejoice events 68 %, and can relax with a radio, TV or a good book (57%) (Figure 1).
Figure 1.
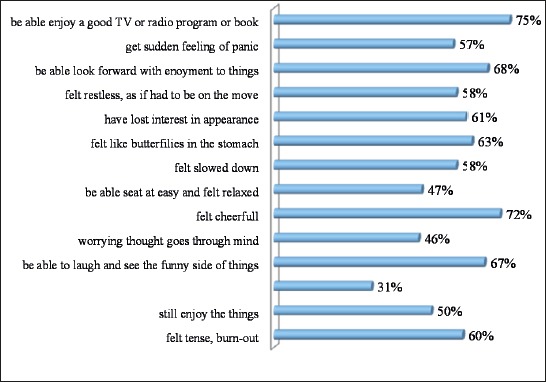
The prevalence of significant distress symptoms and some motivators to carrying with distress (HADS Scale)
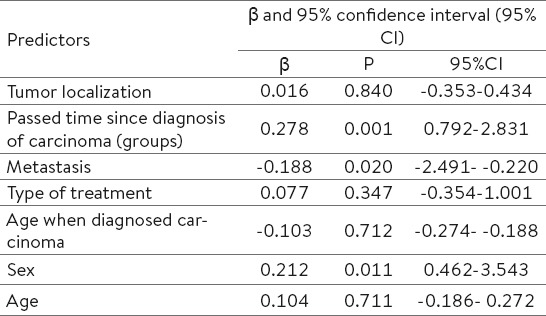
According to the average values of the HADS score captures the dominance of distress compared to self-motivating factors. Distress suffered 76% of respondents (132 of 174): aHADS = 19:24 ± 4.804 compared to bHADS = 12:48 ± 3,927. According aHADS in the first group, 14 in relation to the remaining 42 (n = 56) subjects adapts to acute stress situation. In the second group (prolonged stress responses) 28 successfully overcomes the problems with the perception of events in connection with a malignant disease as compared to 51, which can not (n = 79). Unfortunately, in the third group, motivators are off (0 respondents have self motivation). According to discover groups distress I: II: III = 42: 51: 39 = 75%: 65%: 100%. The difference between the groups was highly statistically significant, Pearson χ2 test = 17.946, P = 0.001. Predictors of distress in cancer patients as time elapsed since diagnosis of the disease (duration of exposure “cancer” (P = 0.001), discovered metastases (P = 0.020), and being male (P = 0.011; multivariate regression analysis ANOVA) (Table 2).
Table 2.
Predictors of distress (aHADS-scale as dependent variable); independent variables: tumor localization, passed time since diagnosis of carcinoma, metastasis, type of treatment, age when diagnosed carcinoma, sex and age among oncological patients (n=174)
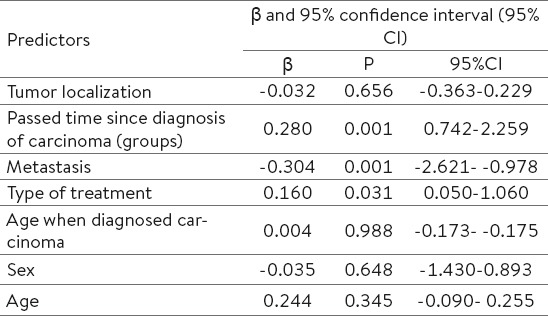
Predictors of burnout syndrome in cancer patients are all important determinants of malignant disease: the time elapsed since the diagnosis of the disease which determines the clinical status of malignant disease (P = 0.001), discovered metastases (P = 0.001) and treatments (P = 0.031; multivariate regression analysis ANOVA) (Table 3).
Table 3.
Predictors of distress (bHADS scale as dependent variable); independent variables: tumor localization, passed time since diagnosis of carcinoma, metastasis, type of treatment, age when diagnosed carcinoma, sex and age among oncological patients (n=174)
Constantly survives in the minds of events in connection with its malignant disease (PTSD) 55% of respondents. The mean PTSD score in all patients was 3.480 ± 2.486 (on a scale of 1-7). Number of 87 of total 174 (50%) patients have PTSD score ≥ 4 (37%, 21 out of 56 in group I, 46%, 36 out of 79 in Group II, 77%, 30 out of 39 in Group III). There is a statistically significant difference in the value of recent PTSD according to the groups (χ2 test = 40.582, P = 0.001). Dichotomized score PTSD (PTSD not) reveal precisely 72 (41%) of those with PTSD (Figure 2).
Figure 2.
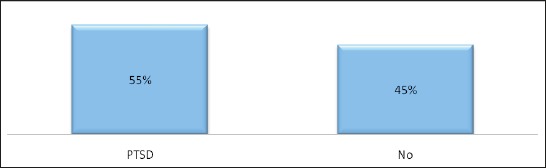
The prevalence of Postraumatic stress disorders (PTSD) among oncological patients (N=174)
The difference frequency of PTSD according to the groups is statistically significant: 19: 37 (I) vs. 29:50 (II) Vs. 24: 15, χ2 test = 8.526, P = 0.014 (Figure 3).
Figure 3.
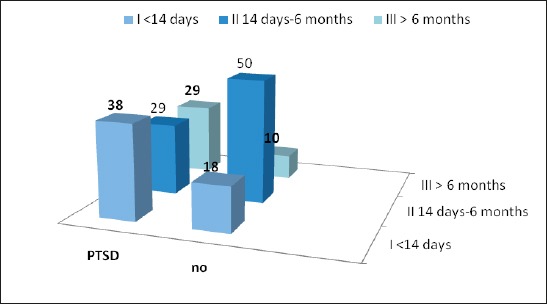
Distribution of PTSD between groups related passed time since diagnosis of carcinoma
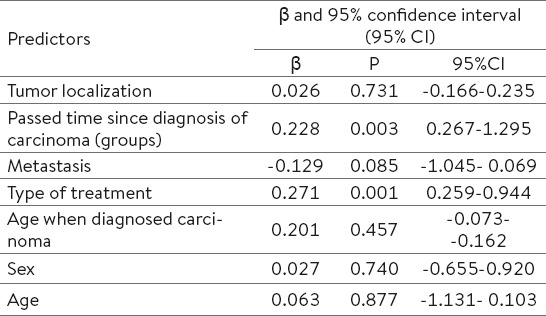
As expected the highest prevalence of PTSD in the third group. What patients are more exposed to the stressor, which can be defined as malignancy increases in comorbidity and PTSD. Predictors of PTSD established multivariate regression analysis ANOVA in cancer patients as the duration of illness as a stressor (P = 0.003) and treatment (P = 0.001), which further depletes self motivating, contributes to the development and worsening of PTSD (Table 4).
Table 4.
Predictors of PTSD as dependent variable; independent variables: tumor localization, passed time since diagnosis of carcinoma, metastasis, type of treatment, age when diagnosed carcinoma, sex and age among oncological patients (n=174)
4. DISCUSSION
Centuries old stigma about cancer prevents patients to talk about their diagnosis. There is a real risk of distress and mental disorders a patient. Selye stress is seen as a non-specific result (psychic and somatic) any claim in the body, which goes beyond the adaptive capabilities of the organism. The psycho-oncology talking about exposure to malignant diseases such stressor (14, 15, 17). The psychological adaptation of patients with malignant disease passes through three stages. Acute phase occurs during the diagnosis, followed by prolonged stress reaction during treatment and the third chronic phase occurs after treatment (15, 16). Often the hardest just the third phase which showed the results of our study because of the patient with cancer changed everything, and fear of recurrence is very high. This is confirmed in the results of this research. Of the 39 patients in the third group (the third stage of the disease) in all 39 subjects was recorded distress (100%). On the other hand, long maintained the stigma related to mental illness is further complicated by the situation, but cancer patients do not want to admit their psychological problems (2). Therefore, patients are without timely and adequate treatment effect of anxiety that usually turns into chronic suffering burn-out syndrome, post-traumatic stress disorder or severe episodes of depression (1). General distress suffered 76% of respondents (132 of 174). It’s actually more than twice the prevalence of which are found by other authors. According to previous research, one third of cancer patients suffer distress (7, 8, 18). The degree of economic and cultural development of the country reduces the frequency of perception distress of cancer patients (7). Research has shown that 58% of patients in palliative care, in the terminal stage of disease in North America suffers emotional distress (19), in respect of our patients in distress which is present in this phase, 100% (42% + trend). The prevalence of distress in our respondents approximates the prevalence of distress cancer patients in Jordan, 70% (76% in the US, the trend +6) (20). Predictors of distress cancer patients have the time elapsed since the diagnosis of cancer or I status malignancy and metastasis detected. Nearly a quarter of women diagnosed with breast cancer has symptoms of post-traumatic stress disorder (PTSD) (21, 22). Results of research in Jordan reveal that 50% of cancer patients had PTSD which is in agreement with our results, 45% had PTSD. After 13 years of exposure to cancer and dealing with PTSD disease disappeared after 13 years only 12% of respondents, while 37% of them are kept or worsened after several years of treatment (20). They kept survived the events surrounding the cancer type “flash back” three-quarters of our respondents who have knowledge of the disease> 6 months, and half of the respondents that the disease is diagnosed in the period from 14 days to 6 months. Slightly less than one-half of respondents knowing that cancer has experienced such severe stress, crisis or catastrophic situation. They soon developed symptoms of PTSD.
5. CONCLUSION
There is still a high degree of stigma associated with cancer and mental health disorders, not only among the ill, but also among health care workers. Distress, burnout syndrome and PTSD are not yet included in clinical procedures oncology patients. The problem is widespread and has a high prevalence in our environment.
Footnotes
• Author’s contribution: All authors in this paper have contributed in all phases in it’s preparing. First author made final proof reading.
• Conflict of interest: The authors declare that there is no conflict of interest.
REFERENCES
- 1.Reiche EM, Morimoto HK, Nunes SM. Stress and depression-induced immune dysfunction:implications for the development and progression of cancer. Int Rev Psychiatry. 2005;17(6):515–27. doi: 10.1080/02646830500382102. [DOI] [PubMed] [Google Scholar]
- 2.Holland JC. History of psycho-oncology:overcoming attitudinal and conceptual barriers. Psychosom Med. 2002;64:206–21. doi: 10.1097/00006842-200203000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Holland JC. Psychological Care of Patients:Psycho- Oncology's Contribution. Journal of Clinical Oncology. 2003;21(23):253s–65s. doi: 10.1200/JCO.2003.09.133. [DOI] [PubMed] [Google Scholar]
- 4.Gregurek R, Braš M, Đorđević V, Ratković AS, Brajković L. Psychological problems of patients with cancer. Psychiatria Danubina. 2010;22(2):227–30. [PubMed] [Google Scholar]
- 5.Khatib J, Salhi R, Awad G. Distress in cancer patients in King Hussein Cancer Center (KHCC):A study using the Arabic-modified version of the Distress Thermometer. Prof Psychol Res Pr. 2001;32:52–8. [Google Scholar]
- 6.Tope DM, Ahles TA, Silberfarb PM. Psycho-oncology:psychological well-being as one component of quality of life. Psychother Psychosom. 1993;60:129–47. doi: 10.1159/000288688. [DOI] [PubMed] [Google Scholar]
- 7.Carlson LE, Angen M, Cullum J, et al. High levels of untreated distress and fatigue in cancer patients. Br J Cancer. 2004;90:2297–304. doi: 10.1038/sj.bjc.6601887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Carlson LE, Bultz BD. Cancer distress screening:Needs, methods and models. J Psychosom Res. 2003;55:403–9. doi: 10.1016/s0022-3999(03)00514-2. [DOI] [PubMed] [Google Scholar]
- 9.Pranjić N, Nuhbegović S, Brekalo-Lazarević S, Kurtić A. Adrenal Exhaustion Synonym of Syndrome Burnout at Workplace. Coll Antropol. 2012;36(3):911–9. [PubMed] [Google Scholar]
- 10.Hersbach P, Book K, Brandl T, Keller M, Marten- Mittag The Basic Documentation for Psycho-Oncology (PO-Bado):an expert rating scale for the psychosocial experience of cancer patients. Onkologie. 2008;31(11):591–6. doi: 10.1159/000162287. [DOI] [PubMed] [Google Scholar]
- 11.American Psychiatric Assiciation. Diagnostic and statistical manual of mental disorders DSM-IV. Fourth Wahington DC: american Psychiatric Association; 1994. [Google Scholar]
- 12.Freudenberger H. Burnout:Symptoms of Burnout. Bantum, NY (ed) 1981:18. [Google Scholar]
- 13.Herrmann C. International experiences with the Hospital Anxiety and Depression Scale:review of validation data and clinical results. J Psychosom Res. 1997;42:17–41. doi: 10.1016/s0022-3999(96)00216-4. [DOI] [PubMed] [Google Scholar]
- 14.Bultz BD, Carlson LE. Emotional Distress:The Sixth Vital Sign in Cancer Care Journal of Clinical Oncology. 2005;23(26):6440–1. doi: 10.1200/JCO.2005.02.3259. [DOI] [PubMed] [Google Scholar]
- 15.Selye H. The general adaptation syndrome and the disease of adaptation. J Clinical Endocrinology. 1946;6:117–30. doi: 10.1210/jcem-6-2-117. [DOI] [PubMed] [Google Scholar]
- 16.Kadan-Lottick NS, Vanderwerker LC, Block SD, Zhang B, Prigerson HG. Psychiatric disorders and mental health service use in patients with advanced cancer:a report from the coping with cancer study. Cancer. 2005;104(12):2872–81. doi: 10.1002/cncr.21532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Reich M. Depression and cancer:recent data on clinical issues, research challanges and treatment approaches. Curr Opin Oncol. 2008;20(4):353–9. doi: 10.1097/CCO.0b013e3282fc734b. [DOI] [PubMed] [Google Scholar]
- 18.Zabora J, Brintzenhofe SK, Curbow B. The prevalence of psychological distress by cancer site. Psychooncology. 2001;10:19–28. doi: 10.1002/1099-1611(200101/02)10:1<19::aid-pon501>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 19.Potash M, Breitbart W. Affective disorders in advanced cancer. Hematol Oncol Clin North Am. 2002;16:671–700. doi: 10.1016/s0889-8588(02)00013-8. [DOI] [PubMed] [Google Scholar]
- 20.Khatib J, Salhi R, Awad G. Distress in cancer in-patients in King Hussein Cancer Center (KHCC):A study using the Arabic-modified version of the Distress Thermometer. Prof Psychol Res Pr. 2001;32:52–8. [Google Scholar]
- 21.Lauver D, Ho CH. Explaining delay in care seeking for breast cancer symptoms. J Appl Soc Psychol. 1993;23(21):1806–25. [Google Scholar]
- 22.MacFarlane ME, Sony SD. Women, breast lump discovery, and associated stress. Health Care Women Int. 1992;13(1):23–32. doi: 10.1080/07399339209515975. [DOI] [PubMed] [Google Scholar]


