Abstract
Background
Little is known about to what extent treatment-seeking behavior varies across individuals with alcohol abuse, alcohol dependence, drug abuse, and drug dependence.
Methods
The sample included respondents from the Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) who reported a lifetime diagnosis alcohol abuse, alcohol dependence, drug abuse, or drug dependence. Unadjusted and adjusted hazard ratios are presented for time to first treatment contact by sociodemographic characteristics and comorbid psychiatric disorders. Individuals were censored from the analyses if their condition remitted prior to seeking treatment.
Results
In the first year after disorder onset, rates of treatment-seeking were 13% for drug dependence, 5% for alcohol dependence, 2% for drug abuse, and 1% for alcohol abuse. The lifetime probability of seeking treatment among individuals who did not remit was also highest for drug dependence (90%), followed by drug abuse (60%), alcohol dependence (54%), and alcohol abuse (16%). Having had previous treatment contact for a substance use disorder (SUD) increased the probability of seeking treatment for another SUD. By contrast, an early age of SUD onset, belonging to an older cohort, and a higher level of education decreased the lifetime probability of treatment contact for SUD. The role of comorbid mental disorders was more complex, with some disorders increasing and other decreasing the probability of seeking treatment.
Conclusions
Given high rates of SUD and their substantial health and economic burden, these patterns suggest the need for innovative approaches to increase treatment access for individuals with SUD.
Keywords: Treatment-seeking, Substance use disorders, Comorbidity, NESARC
1. Introduction
Substance use disorders (SUDs) are pervasive in the general population and result in critical threats to health and well-being, substantial family distress, and a massive societal economic burden (Blanco et al., 2013c; Compton et al., 2007; Hasin et al., 2007; Mokdad et al., 2004; Rubio et al., 2014, 2013). Alcohol consumption ranks third among preventable causes of death (Mokdad et al., 2004) and drug offenses are the leading cause of incarceration with half of federal inmates reporting illegal drug use in the month before their offense (Mumola and Karberg, 2004). Illicit drug use accounts for nearly two hundred billion dollars each year in healthcare, lost productivity, incarceration, and drug enforcement costs (NDIC, 2014).
Despite their high prevalence and numerous associated adverse health consequences (Aharonovich et al., 2002; Blanco et al., 2014b; Degenhardt and Hall, 2012; García-Rodrígueza et al., 2014), many individuals with SUD do not receive treatment (Blanco et al., 2013a; Compton et al., 2007; Edlund et al., 2012; Hasin et al., 2007; Kessler et al., 1999; Olfson et al., 1998; Regier et al., 1993). The great extent of unmet need for substance abuse treatment underscores the critical public health importance of understanding factors that promote the flow of individuals with SUDs into treatment. Although there are important differences between perceived and objective need for substance abuse treatment (Mojtabai et al., 2002), quality of life substantially declines following the onset of SUD (Rubio et al., 2014). Because individuals with SUDs who receive treatment increase their likelihood of remission and decrease their likelihood of developing new SUDs, increasing access to SUD treatment tends to improve outcome (Blanco et al., 2014a). Of course, SUD treatment is often court mandated or occurs following the pressure exerted by friends or family members (Cook and Alegria, 2011).
Epidemiological research has sought to identify personal characteristics that either facilitate or impede treatment-seeking for SUD. Among individuals with SUDs, factors that have been associated with lower rates of SUD treatment include an earlier age of SUD onset, being married, membership in an older cohort, minority racial/ethnic ancestry, and having attained less than a high school education (Alegria et al., 2002; Gee et al., 2007; Grant, 1996; Sue et al., 1991; Sussman et al., 1987; Wang et al., 2005, 2004, 2002). Although adults with SUDs commonly have comorbid of Axis II and other Axis I psychiatric disorders (Armstrong and Costello, 2002; Blanco et al., 2013b, 2015; Havassy et al., 2004; Kessler et al., 1997; Merikangas et al., 1998; Mertens et al., 2003), the effect of psychiatric comorbidity on treatment-seeking for SUD has not been previously examined. Furthermore, despite wide variation in prevalence, severity, and associated adverse consequences (Compton et al., 2007; Hasin et al., 2007), differences in treatment seeking behavior of people with alcohol abuse, alcohol dependence, drug abuse, and drug dependence have not been extensively characterized (Wang et al., 2005).
This study draws on data from a large nationally representative sample of US adults with SUD to evaluate treatment-seeking for SUDs. Our goal is to assess the effects of type of SUD, treatment history, comorbid psychiatric disorders, and sociodemographic characteristics lifetime probability of SUD treatment.
2. Methods
2.1. Sample
The 2004–2005 Wave 2 NESARC (Grant et al., 2007b) is the second wave of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) (Grant et al., 2003a). The target population was the civilian non-institutionalized population, 18 years and older residing in households and group quarters (e.g., college quarters, group homes, boarding houses, and non-transient hotels). In Wave 2, attempts were made to conduct face-to-face re-interviews with all 43,093 respondents to the Wave 1 interview. Excluding respondents ineligible for the Wave 2 interview (e.g., deceased), the Wave 2 response rate was 86.7%; thus, 34,653 respondents completed Wave 2 interviews. Sample weights were developed to additionally adjust to Wave 2 non-response (Ruan et al., 2008). Comparisons between Wave 2 respondents and the target population (comprising Wave 2 respondents and eligible non-respondents) indicated that there were no significant differences in baseline (Wave 1) sociodemographic measures or the presence of any lifetime substance, mood, anxiety, or personality disorder (Grant et al., 2007a).
2.2. Assessment
Extensive AUDADIS-IV questions probed DSM-IV criteria for alcohol and drug-specific abuse and dependence for 10 classes of substances, aggregated in this report to yield diagnoses of any drug abuse and any drug dependence (Compton et al., 2007). Among individuals with drug abuse, the most commonly abused drugs were cannabis (77.8% of individuals), cocaine (19.5%), and hallucinogens (15.3%), whereas among those with dependence, the most common drugs were cannabis (51.6%), cocaine (35.0%), and amphetamine (21.1%). Good to excellent (k = 0.70–0.91) test–retest reliability of AUDADIS-IV SUD diagnoses have been documented in clinical and general population samples (Canino et al., 1999; Chatterji et al., 1997; Grant et al., 2003b, 1995; Hasin et al., 1997a). Convergent, discriminant and construct validity of AUDADIS-IV SUD criteria, and diagnoses were good to excellent (Cottler et al., 1997; Hasin et al., 1997b; Hasin and Paykin, 1999; Hasin et al., 1990, 1994, 2003, 1997c; Nelson et al., 1999; Pull et al., 1997; Ustun et al., 1997; Vrasti et al., 1998).
2.3. Statistical Analyses
Weighted cross-tabulations were used to calculate the proportion of respondents with lifetime alcohol abuse, alcohol dependence, drug abuse, and drug dependence who had ever sought treatment for their disorder. The tabulations were stratified by sociodemographic and clinical characteristics. Kaplan–Meier analyses were conducted to estimate the cumulative probability of treatment-seeking for each disorder. For all analyses, consistent with DSM-IV, abuse and dependence were treated hierarchically.
To assess the effects of sociodemographic and clinical characteristics on probability of SUD treatment contact among those with lifetime diagnoses of SUD, Cox proportional hazards models with time-varying covariates were performed. Retrospective follow-up time started at age of disorder onset and terminated at age of first treatment contact or remission of the disorder. The probabilities of treatment-seeking for alcohol abuse, alcohol dependence, drug abuse, and drug dependence were first modeled separately for each individual sociodemographic and diagnostic predictor and again in a single model that controlled for the potentially confounding effects of sex, race/ethnicity, nativity, age at disorder onset, education years, marital status, and each of the other Axis I and II categories. Comorbid mental disorders, marital status, and educational level were also added as time varying variables. Comorbid disorders were coded as absent until their first occurrence, and then coded as present until the observation was censored. Marital status was coded as single until the individual was married for the first time (or coded as single until the observation was censored) and then modified each year the individual changed marital status. For each participant, a maximum of two changes were coded, including the first and most recent change in marital status. Educational level was coded as starting at age six and increasing each year by one until the highest level of education was achieved. For example, an individual completing high school would be coded starting at age six with one additional year of education until age 18.
Personality disorders were coded as lifetime disorders with onset at age 18. The variance inflation factor (VIF) was used to assess possible collinearity among the variables included in the multivariable models. For all analyses, individuals were censored at the time of remission if remission occurred before seeking treatment. Results are reported as hazard ratios and adjusted hazard ratios with associated 95% confidence intervals (95% CI). Standard errors and 95% CI for all analyses were estimated using SUDAAN to adjust for the complex design of the NESARC.
3. Results
3.1. Cumulative lifetime probability of treatment-seeking for substance use disorders
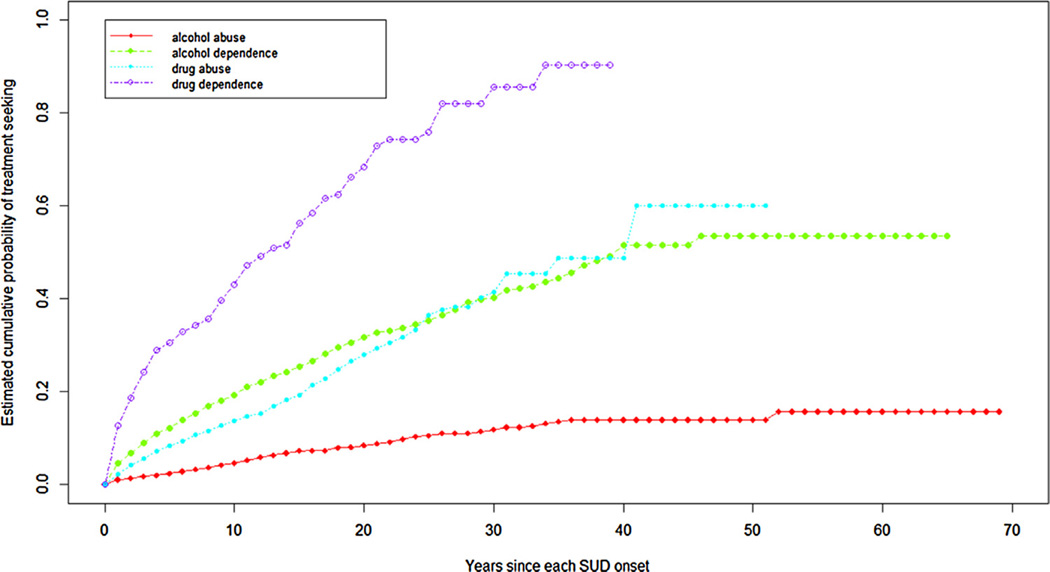
Regardless of the timeframe considered (one year after disorder onset, first 10 years after onset, or lifetime), the probability of treatment-seeking was highest for drug dependence followed by alcohol dependence, drug abuse, and alcohol abuse. In the first year after disorder onset, rates of treatment-seeking among individuals who did not remit were 13% for drug dependence, 5% for alcohol dependence, 2% for drug abuse, and 1% for alcohol abuse. After 10 years, the highest rates of seeking treatment continued to be among those with drug dependence (43%) followed by those with alcohol dependence (19%). Less common was the treatment seeking for drug abuse (14%) and for alcohol abuse (5%). The lifetime probability of seeking treatment among individuals who did not remit was also highest for those with drug dependence (90%), followed by drug abuse (60%), alcohol dependence (54%), and alcohol abuse (16%). Among those who sought treatment, the midpoints in the cumulative probability distributions were 12 years for drug dependence, 18 years for alcohol dependence, 20 years for alcohol abuse, and 23 years for drug abuse (Fig. 1).
Fig. 1.
Cumulative probability of treatment for substance use disorders.
3.2. Univariate Analyses
In the univariate analyses, an increased likelihood of treatment across for all disorders was related to later onset of disorder, belonging to a more recent cohort, having never been married, and having sought treatment previously for another mental or substance use disorder. Having a change in marital status increased the probability of treatment across all disorders except alcohol abuse, whereas having less than a high school education and being widowed, separated or divorced, increased the probability of treatment for all disorders except for drug dependence. Being Black, Hispanic, or foreign-born increased the likelihood of treatment for alcohol abuse. Males had a greater probability of treatment than females for alcohol abuse, but a decreased probability compared with females of treatment for drug abuse (Table 1).
Table 1.
Sociodemographic predictors of first treatment contact in individuals with each SUD (univariate analyses).
| Variable | Alcohol abuse (N = 5947) | Alcohol dependence (N = 4863) | Drug abuse (N = 3228) | Drug dependence (N = 1062) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HR | 95% CI | HR | 95% CI | HR | 95% CI | HR | 95% CI | |||||
| Sex | ||||||||||||
| Male | 1.39 | 1.01 | 1.90 | 1.08 | 0.90 | 1.28 | 0.75 | 0.57 | 0.98 | 0.90 | 0.64 | 1.26 |
| Female | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Race/ethnicity | ||||||||||||
| White | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Blacks | 1.42 | 0.89 | 2.26 | 1.08 | 0.85 | 1.38 | 0.81 | 0.56 | 1.17 | 0.75 | 0.55 | 1.04 |
| Native | 1.07 | 0.46 | 2.52 | 1.49 | 0.97 | 2.31 | 0.34 | 0.11 | 1.00 | 0.54 | 0.24 | 1.22 |
| Americans | ||||||||||||
| Asians | 1.57 | 0.41 | 6.01 | 0.41 | 0.13 | 1.30 | 1.52 | 0.48 | 4.78 | 0.93 | 0.25 | 3.42 |
| Hispanic | 2.28 | 1.46 | 3.56 | 1.06 | 0.81 | 1.38 | 1.40 | 0.96 | 2.04 | 1.05 | 0.66 | 1.67 |
| Nativity | ||||||||||||
| US born | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Foreign born | 1.90 | 1.14 | 3.16 | 0.87 | 0.57 | 1.31 | 1.65 | 0.90 | 3.00 | 1.71 | 0.93 | 3.13 |
| Age at onset | 1.06 | 1.04 | 1.08 | 1.05 | 1.04 | 1.06 | 1.02 | 0.99 | 1.05 | 1.05 | 1.02 | 1.08 |
| Educational years | ||||||||||||
| 0–11 | 3.76 | 2.18 | 6.47 | 1.75 | 1.28 | 2.39 | 2.08 | 1.18 | 3.65 | 1.01 | 0.53 | 1.92 |
| 12 | 2.22 | 1.41 | 3.50 | 1.67 | 1.30 | 2.14 | 1.40 | 0.80 | 2.43 | 1.14 | 0.67 | 1.95 |
| 13–15 | 1.86 | 1.16 | 2.99 | 1.55 | 1.22 | 1.98 | 1.69 | 1.01 | 2.83 | 1.00 | 0.58 | 1.73 |
| >16 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Cohort | ||||||||||||
| 1976–1985 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 1966–1975 | 0.63 | 0.36 | 1.12 | 0.73 | 0.54 | 1.01 | 0.40 | 0.26 | 0.61 | 0.44 | 0.30 | 0.66 |
| 1956–1965 | 0.35 | 0.20 | 0.62 | 0.76 | 0.56 | 1.03 | 0.27 | 0.18 | 0.41 | 0.25 | 0.15 | 0.41 |
| 1946–1955 | 0.23 | 0.13 | 0.40 | 0.62 | 0.45 | 0.86 | 0.13 | 0.07 | 0.22 | 0.17 | 0.09 | 0.32 |
| 1936–1945 | 0.20 | 0.11 | 0.36 | 0.56 | 0.38 | 0.83 | 0.09 | 0.03 | 0.22 | 0.24 | 0.11 | 0.50 |
| 1901–1935 | 0.10 | 0.05 | 0.20 | 0.37 | 0.21 | 0.65 | <0.01 | <0.01 | <0.01 | 0.05 | <0.01 | 0.52 |
| Marital status | ||||||||||||
| Married | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Widowed/separated/divorced | 2.20 | 1.51 | 3.20 | 1.77 | 1.45 | 2.15 | 0.93 | 0.55 | 1.60 | 0.89 | 0.54 | 1.48 |
| Never married | 3.43 | 2.53 | 4.64 | 1.75 | 1.41 | 2.16 | 1.40 | 0.97 | 2.02 | 1.42 | 0.92 | 2.18 |
| Marital transition (any change in marital status) | 1.01 | 0.64 | 1.59 | 1.29 | 1.06 | 1.57 | 1.95 | 1.39 | 2.73 | 1.65 | 1.22 | 2.23 |
| Past substance use disorder treatment | 11.32 | 6.22 | 20.61 | 7.55 | 5.89 | 9.69 | 15.59 | 11.41 | 21.30 | 9.43 | 6.67 | 13.32 |
| Past mental health treatment | 2.57 | 1.67 | 3.95 | 1.84 | 1.51 | 2.24 | 3.02 | 2.10 | 4.35 | 2.32 | 1.67 | 3.23 |
Most comorbid Axis I disorders increased the probability of treatment for alcohol dependence, drug abuse, and dependence. However, the effect of personality disorders was less consistent. The likelihood of treatment for alcohol abuse was increased by comorbid drug abuse and dependence, major depressive disorder, bipolar disorder, and four personality disorders (avoidant, borderline, histrionic, and antisocial; Table 2).
Table 2.
Comorbidity predictors of first treatment contact in individuals with substance use disorders (univariate analyses).
| Alcohol abuse (N = 5947) | Alcohol dependence (N = 4863) | Drug abuse (N = 3228) | Drug dependence (N = 1062) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | HR | 95% CI | HR | 95% CI | HR | 95% CI | HR | 95% CI | ||||
| Alcohol abuse | N/A | N/A | N/A | 1.02 | 0.62 | 1.68 | 0.44 | 0.27 | 0.71 | 0.77 | 0.46 | 1.30 |
| Alcohol dependence | N/A | N/A | N/A | N/A | N/A | N/A | 1.58 | 1.23 | 2.03 | 1.17 | 0.89 | 1.55 |
| Any drug abuse | 2.37 | 1.52 | 3.70 | 1.66 | 1.34 | 2.05 | N/A | N/A | N/A | 0.90 | 0.66 | 1.24 |
| Any drug dependence | 3.78 | 1.76 | 8.14 | 3.28 | 2.55 | 4.21 | N/A | N/A | N/A | N/A | N/A | N/A |
| Nicotine dependence | 1.22 | 0.82 | 1.81 | 1.46 | 1.22 | 1.73 | 2.05 | 1.43 | 2.94 | 1.31 | 0.96 | 1.77 |
| Mood disorders | 3.02 | 2.02 | 4.51 | 1.94 | 1.58 | 2.37 | 2.70 | 1.93 | 3.77 | 1.85 | 1.36 | 2.51 |
| Dysthymia | 2.36 | 0.62 | 9.00 | 2.02 | 1.48 | 2.76 | 4.15 | 2.38 | 7.24 | 1.71 | 1.08 | 2.71 |
| MDD | 2.17 | 1.22 | 3.86 | 1.48 | 1.14 | 1.94 | 1.89 | 1.19 | 3.00 | 1.28 | 0.81 | 2.01 |
| Bipolar disorder | 4.64 | 2.78 | 7.73 | 2.03 | 1.56 | 2.64 | 2.33 | 1.46 | 3.70 | 1.76 | 1.16 | 2.67 |
| Any anxiety disorder | 0.68 | 0.43 | 1.10 | 1.28 | 1.06 | 1.55 | 1.60 | 1.17 | 2.20 | 1.40 | 1.01 | 1.93 |
| Generalized anxiety disorder | 1.61 | 0.58 | 4.47 | 2.14 | 1.48 | 3.10 | 2.43 | 1.32 | 4.47 | 1.73 | 1.07 | 2.81 |
| Social anxiety disorder | 0.59 | 0.22 | 1.57 | 1.24 | 0.93 | 1.64 | 1.17 | 0.70 | 1.94 | 0.87 | 0.53 | 1.44 |
| Panic disorder | 0.83 | 0.25 | 2.78 | 1.95 | 1.35 | 2.80 | 1.90 | 1.02 | 3.56 | 1.79 | 1.16 | 2.75 |
| Specific phobia | 0.53 | 0.29 | 0.96 | 1.02 | 0.79 | 1.30 | 1.50 | 0.97 | 2.30 | 1.36 | 0.93 | 2.00 |
| PTSD | 1.80 | 0.72 | 4.51 | 1.89 | 1.35 | 2.64 | 2.55 | 1.38 | 4.70 | 1.57 | 0.86 | 2.88 |
| Pathological gambling | 3.28 | 0.43 | 25.38 | 0.70 | 0.23 | 2.13 | <0.01 | <0.01 | <0.01 | 0.66 | 0.16 | 2.74 |
| ADHD | 1.95 | 0.54 | 7.07 | 1.57 | 1.10 | 2.25 | 1.84 | 1.17 | 2.89 | 1.07 | 0.61 | 1.88 |
| Any personality disorder | 1.45 | 1.10 | 1.90 | 1.29 | 1.09 | 1.51 | 1.46 | 1.05 | 2.02 | 1.14 | 0.80 | 1.62 |
| Avoidant | 2.44 | 1.02 | 5.82 | 1.80 | 1.30 | 2.48 | 1.08 | 0.56 | 2.07 | 1.63 | 1.06 | 2.53 |
| Dependant | 2.31 | 0.33 | 16.19 | 3.27 | 1.96 | 5.47 | 0.39 | 0.05 | 3.34 | 1.24 | 0.54 | 2.86 |
| Obsessive–compulsive | 1.01 | 0.62 | 1.63 | 0.95 | 0.74 | 1.22 | 0.98 | 0.64 | 1.51 | 0.64 | 0.40 | 1.04 |
| Paranoid | 1.71 | 0.95 | 3.09 | 1.30 | 0.97 | 1.75 | 1.10 | 0.63 | 1.91 | 0.83 | 0.54 | 1.28 |
| Schizoid | 1.34 | 0.75 | 2.39 | 1.24 | 0.91 | 1.68 | 1.71 | 0.99 | 2.97 | 1.21 | 0.75 | 1.93 |
| Schizotypical | 1.36 | 0.73 | 2.52 | 1.66 | 1.28 | 2.17 | 1.23 | 0.79 | 1.93 | 1.21 | 0.79 | 1.84 |
| Narcissistic | 0.87 | 0.52 | 1.46 | 1.19 | 0.90 | 1.58 | 1.10 | 0.73 | 1.64 | 1.10 | 0.75 | 1.61 |
| Borderline | 2.51 | 1.59 | 3.96 | 1.80 | 1.44 | 2.25 | 1.73 | 1.23 | 2.43 | 1.60 | 1.11 | 2.31 |
| Histrionic | 2.62 | 1.11 | 6.17 | 1.37 | 0.96 | 1.98 | 1.34 | 0.65 | 2.79 | 0.78 | 0.40 | 1.53 |
| Antisocial | 1.68 | 1.04 | 2.70 | 1.48 | 1.16 | 1.88 | 1.36 | 0.94 | 1.96 | 0.73 | 0.52 | 1.03 |
3.3. Multivariable Analyses
After adjusting for the effects of other covariates, fewer factors significantly predicted treatment-seeking. Across all SUDs, having previously sought treatment for another SUD-predicted treatment. In the multivariable models, a history of prior mental health treatment also predicted treatment for alcohol abuse and drug dependence. A later age of onset, having never been married and receiving less than a college education continued to increase the probability of treatment-seeking for alcohol abuse and dependence, but not for drug abuse or dependence.
Younger cohorts had a greater probability of seeking treatment for drug and alcohol abuse, whereas there was no cohort effect for treatment of alcohol or drug dependence. Being widowed, separated, or divorced was associated greater probability of treatment for alcohol abuse and dependence, whereas changes in marital status were associated with lower probability of treatment for alcohol abuse. Male sex was associated with an increased probability for treatment of alcohol abuse but a decreased probability for treatment of alcohol dependence, whereas being Native American was associated with a lower probability of treatment of drug abuse (Table 3).
Table 3.
Sociodemographic predictors of first treatment contact in individuals with substance use disorders (multivariable analyses).
| Alcohol abuse (N = 5947) | Alcohol dependence (N = 4863) | Drug abuse (N = 3228) | Drug dependence (N = 1062) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | AHR | 95% CI | AHR | 95% CI | AHR | 95% CI | AHR | 95% CI | ||||
| Sex | ||||||||||||
| Male | 1.73 | 1.23 | 2.42 | 1.20 | 0.99 | 1.45 | 0.69 | 0.52 | 0.91 | 0.88 | 0.64 | 1.22 |
| Female | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Race/ethnicity | ||||||||||||
| White | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Blacks | 0.91 | 0.57 | 1.46 | 0.88 | 0.68 | 1.13 | 0.88 | 0.57 | 1.37 | 0.69 | 0.46 | 1.02 |
| Native Americans | 0.73 | 0.29 | 1.83 | 1.38 | 0.94 | 2.04 | 0.25 | 0.08 | 0.79 | 0.66 | 0.34 | 1.28 |
| Asians | 0.91 | 0.15 | 5.40 | 0.57 | 0.20 | 1.60 | 1.47 | 0.48 | 4.54 | 1.11 | 0.43 | 2.87 |
| Hispanic | 1.51 | 0.86 | 2.64 | 1.05 | 0.78 | 1.40 | 1.01 | 0.66 | 1.54 | 0.90 | 0.61 | 1.33 |
| Nativity | ||||||||||||
| US born | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Foreign born | 1.00 | 0.45 | 2.19 | 0.70 | 0.41 | 1.20 | 1.29 | 0.65 | 2.60 | 1.59 | 0.88 | 2.85 |
| Age at onset | 1.06 | 1.04 | 1.07 | 1.05 | 1.03 | 1.06 | 1.01 | 0.98 | 1.04 | 1.01 | 0.99 | 1.04 |
| Educational years | ||||||||||||
| 0–11 | 4.33 | 2.49 | 7.54 | 1.71 | 1.26 | 2.32 | 1.86 | 1.02 | 3.39 | 1.25 | 0.67 | 2.34 |
| 12 | 2.40 | 1.54 | 3.74 | 1.37 | 1.05 | 1.77 | 1.31 | 0.74 | 2.32 | 1.51 | 0.85 | 2.68 |
| 13–15 | 1.98 | 1.28 | 3.06 | 1.25 | 0.97 | 1.61 | 1.26 | 0.74 | 2.14 | 1.30 | 0.76 | 2.22 |
| 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |
| > 16 | ||||||||||||
| Cohort | ||||||||||||
| 1976–1985 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 1966–1975 | 0.68 | 0.36 | 1.29 | 0.88 | 0.63 | 1.23 | 0.70 | 0.48 | 1.04 | 0.73 | 0.47 | 1.14 |
| 1956–1965 | 0.40 | 0.21 | 0.74 | 0.96 | 0.68 | 1.34 | 0.49 | 0.31 | 0.77 | 0.46 | 0.28 | 0.78 |
| 1946–1955 | 0.27 | 0.14 | 0.50 | 0.78 | 0.54 | 1.13 | 0.38 | 0.22 | 0.66 | 0.38 | 0.18 | 0.78 |
| 1936–1945 | 0.27 | 0.14 | 0.50 | 0.81 | 0.54 | 1.22 | 0.37 | 0.15 | 0.90 | 1.11 | 0.46 | 2.68 |
| 1901–1935 | 0.12 | 0.06 | 0.25 | 0.66 | 0.40 | 1.11 | <0.01 | <0.01 | <0.01 | 0.26 | 0.03 | 2.09 |
| Marital status | ||||||||||||
| Married | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Widowed/separated/divorced | 2.10 | 1.40 | 3.16 | 1.39 | 1.12 | 1.72 | 0.90 | 0.52 | 1.57 | 0.95 | 0.59 | 1.53 |
| Never married | 2.98 | 2.13 | 4.17 | 1.57 | 1.25 | 1.97 | 1.40 | 0.94 | 2.08 | 1.36 | 0.92 | 2.00 |
| Marital transition (any change in marital status) | 0.58 | 0.34 | 0.97 | 0.93 | 0.76 | 1.15 | 1.41 | 0.99 | 2.00 | 1.03 | 0.76 | 1.39 |
| Past substance use disorder treatment | 6.15 | 3.21 | 11.76 | 5.38 | 4.16 | 6.96 | 12.53 | 9.01 | 17.41 | 10.64 | 7.73 | 14.65 |
| Past mental health treatment | 2.11 | 1.36 | 3.29 | 1.20 | 0.96 | 1.52 | 1.38 | 0.87 | 2.17 | 1.44 | 1.03 | 2.03 |
Among Axis I disorders, alcohol abuse decreased the probability of treatment of drug abuse, whereas alcohol dependence decreased the probability of treatment of drug abuse and dependence. Complementary analyses indicated that among individuals with drug dependence, the adjusted hazard ratio for treatment of drug dependence was 1.04 (95% CI: 0.79, 1.36) among individuals who did not seek treatment for alcohol dependence and 0.58 (95% CI: 0.42, 0.80) among individuals with treated alcohol dependence. Dysthymia increased the probability of treatment of alcohol dependence and drug abuse, comorbid major depressive disorder was associated with greater probability of treatment of alcohol abuse and comorbid bipolar disorder was associated with increased probability of treatment of alcohol abuse and dependence. Comorbid-specific phobia was associated with a lower probability of treatment of alcohol abuse and comorbid pathological gambling with a lower probability of treatment of drug abuse, whereas comorbid PTSD increased the probability of treatment of alcohol dependence.
Among personality disorders, dependent personality disorder increased the probability of treatment of alcohol dependence, schizoid personality disorder was associated with increased treatment of drug abuse, and avoidant personality disorder increased the probability of treatment for drug dependence. By contrast, narcissistic personality disorders lowered the probability of treatment of alcohol abuse and antisocial personality disorder lowered the probability of treatment of drug dependence (Table 4). VIFs for all variables in the multivariable model were less than two, indicating there were not substantial collinearity problems in the estimations.
Table 4.
Comorbidity predictors of first treatment contact for substance use disorders (multivariable analyses).
| Alcohol abuse (N = 5947) | Alcohol dependence (N = 4863) | Drug abuse (N = 3228) | Drug dependence (N = 1062) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | AHR | 95% CI | AHR | 95% CI | AHR | 95% CI | AHR | 95% CI | ||||
| Any alcohol abuse | N/A | N/A | N/A | 1.00 | 0.65 | 1.54 | 0.51 | 0.31 | 0.84 | 0.60 | 0.36 | 1.01 |
| Any alcohol dependence | N/A | N/A | N/A | N/A | N/A | N/A | 0.62 | 0.47 | 0.82 | 0.59 | 0.45 | 0.77 |
| Any drug abuse | 1.52 | 0.89 | 2.58 | 1.21 | 0.96 | 1.51 | N/A | N/A | N/A | 0.79 | 0.62 | 1.01 |
| Any drug dependence | 0.85 | 0.24 | 3.05 | 1.24 | 0.91 | 1.69 | N/A | N/A | N/A | N/A | N/A | N/A |
| Nicotine dependence | 0.85 | 0.55 | 1.31 | 1.08 | 0.90 | 1.29 | 1.23 | 0.86 | 1.77 | 0.87 | 0.66 | 1.16 |
| Mood disorders | ||||||||||||
| Dysthymia | 1.19 | 0.36 | 3.91 | 1.51 | 1.02 | 2.25 | 2.74 | 1.50 | 4.99 | 1.22 | 0.71 | 2.12 |
| MDD | 1.67 | 1.06 | 2.64 | 1.08 | 0.77 | 1.52 | 0.97 | 0.62 | 1.51 | 0.76 | 0.50 | 1.16 |
| Bipolar disorder | 3.95 | 2.26 | 6.92 | 1.45 | 1.09 | 1.94 | 1.36 | 0.80 | 2.33 | 1.27 | 0.89 | 1.82 |
| Any anxiety disorder | ||||||||||||
| Generalized anxiety disorder | 0.71 | 0.27 | 1.85 | 0.98 | 0.68 | 1.40 | 0.92 | 0.52 | 1.63 | 1.15 | 0.70 | 1.91 |
| Social anxiety disorder | 0.51 | 0.17 | 1.57 | 0.98 | 0.75 | 1.27 | 0.82 | 0.45 | 1.46 | 0.65 | 0.43 | 1.01 |
| Panic disorder | 0.37 | 0.11 | 1.25 | 1.14 | 0.76 | 1.69 | 0.98 | 0.51 | 1.89 | 1.12 | 0.73 | 1.72 |
| Specific phobia | 0.48 | 0.25 | 0.93 | 0.91 | 0.72 | 1.14 | 1.22 | 0.79 | 1.88 | 1.39 | 0.95 | 2.04 |
| PTSD | 1.22 | 0.56 | 2.68 | 1.43 | 1.05 | 1.96 | 1.02 | 0.56 | 1.86 | 0.79 | 0.45 | 1.40 |
| Pathological gambling | 3.13 | 0.43 | 23.01 | 0.71 | 0.23 | 2.22 | <0.01 | <0.01 | <0.01 | 0.56 | 0.25 | 1.25 |
| ADHD | 1.48 | 0.39 | 5.56 | 1.12 | 0.79 | 1.58 | 0.99 | 0.58 | 1.68 | 0.87 | 0.51 | 1.48 |
| Any personality disorder | ||||||||||||
| Avoidant | 0.90 | 0.36 | 2.24 | 0.98 | 0.68 | 1.42 | 1.22 | 0.60 | 2.46 | 1.59 | 1.01 | 2.52 |
| Dependant | 0.74 | 0.08 | 6.45 | 1.90 | 1.09 | 3.33 | 0.26 | 0.03 | 2.50 | 0.73 | 0.30 | 1.77 |
| Obsessive–compulsive | 0.94 | 0.57 | 1.54 | 0.78 | 0.60 | 1.02 | 0.95 | 0.58 | 1.57 | 0.73 | 0.45 | 1.18 |
| Paranoid | 1.11 | 0.56 | 2.22 | 0.94 | 0.68 | 1.29 | 0.77 | 0.41 | 1.45 | 0.99 | 0.64 | 1.53 |
| Schizoid | 1.08 | 0.52 | 2.25 | 1.04 | 0.75 | 1.43 | 1.95 | 1.20 | 3.16 | 1.29 | 0.82 | 2.05 |
| Schizotypical | 0.86 | 0.48 | 1.54 | 0.94 | 0.71 | 1.25 | 0.64 | 0.36 | 1.13 | 0.83 | 0.57 | 1.22 |
| Narcissistic | 0.51 | 0.29 | 0.90 | 0.90 | 0.68 | 1.20 | 0.88 | 0.56 | 1.40 | 0.91 | 0.64 | 1.32 |
| Borderline | 1.33 | 0.77 | 2.31 | 1.15 | 0.89 | 1.48 | 1.49 | 0.99 | 2.24 | 1.18 | 0.79 | 1.77 |
| Histrionic | 1.98 | 0.71 | 5.49 | 1.03 | 0.74 | 1.44 | 0.58 | 0.30 | 1.10 | 0.74 | 0.45 | 1.20 |
| Antisocial | 1.20 | 0.76 | 1.90 | 1.06 | 0.84 | 1.33 | 0.93 | 0.64 | 1.36 | 0.50 | 0.35 | 0.72 |
4. Discussion
In a large nationally representative sample, the lifetime probability of treatment-seeking was highest for drug dependence, followed by drug abuse, alcohol dependence, and alcohol abuse. A history of SUD treatment increased the probability of treatment for all SUD disorders while a history of mental health treatment only increased the probability of treatment for alcohol abuse and drug dependence. A later age of onset and not receiving a college education increased the likelihood of treatment for alcohol abuse and dependence. The effects of comorbid psychiatric disorders on treatment-seeking were more complex and varied by disorder.
In keeping with prior US studies (Olfson et al., 1998; Wang et al., 2005), the rates of treatment-seeking were low for the first several years after onset of the disorder for all SUDs. A novel finding of our study was that time to first treatment contact varied substantially across SUD diagnoses in the year after diagnosis and over the lifetime of the individual. There was a lower probability of treatment, regardless of the timeframe considered, for drug dependence followed by alcohol dependence, drug abuse, and alcohol abuse. This ordering is consistent with the extent of their overall impact on quality of life and daily function (Compton et al., 2007; Hasin et al., 2007; Rubio et al., 2014). Symptoms of withdrawal, which are common to dependence but not of abuse criteria (Compton et al., 2007; Hasin et al., 2007; Hedden and Gfroerer, 2011), may also lead to greater perceived need among individuals with substance dependence than abuse and motivate greater treatment-seeking behavior. As compared to individuals with abuse, those with dependence might also experience greater social pressure to seek treatment exerted by family, economic realities, or legally-related consequences of their behavior.
Stigma (Farley-Toombs, 2012), a tendency to externalize responsibility for their behavior (Olfson et al., 1998; Wang et al., 2005), low perceived need for treatment (Mojtabai et al., 2002), and limited availability of treatment facilities (Cummings et al., 2014) may contribute to low treatment-seeking by individuals with SUD. A focus on the short-term euphoric effects of drug use and negligence of longer-term negative consequences may also diminish motivation to seek treatment. In contrast to the dysphoric states that coincide with onset of mood and anxiety disorders, substantial delays may occur in the onset of adverse subjective states in drug use (Arria et al., 2012; Zuvekas and Hill, 2000). It is also possible that treatments for SUD may be perceived as not efficacious as treatments for mental disorder, which may further impede treatment-seeking for SUDs (Mojtabai and Crum, 2012). In addition, some mental health professionals may be reluctant to treat individuals with SUDs (Moodley-Kunnie, 1988).
In accord with prior research on help seeking for behavioral health care (Christiana et al., 2000; Kessler et al., 1998; Wang et al., 2005), an earlier age of onset tended to decrease the probability of treatment-seeking. Younger individuals often depend on their parents to recognize their symptoms and assist them into care (Dakwar et al., 2014). However, many parents are not aware of the extent and deleterious effects of substance use by their children (Green et al., 2011). Nevertheless, given the strong association of earlier age of onset with greater disorder severity and functional limitations, the lower likelihood of treatment-seeking among younger individuals represents an important challenge for health planners. Higher rates of treatment-seeking among people who were members of more recent cohorts could be due to increased perceived need for treatment among these individuals, less stigma, and greater knowledge of treatment availability or effectiveness (Kessler et al., 1998; Mackenzie et al., 2012; Wang et al., 2005).
Prior treatment of SUDs markedly increased the likelihood of treatment following onset of new SUDs. Familiarity with the treatment system may contribute to treatment seeking when new SUDs arise. By serving as a marker of severity, comorbid SUDs may also increase the likelihood of treatment-seeking (Chiappetta et al., 2014; Compton et al., 2007; Garcia-Rodriguez et al., 2013; Hasin et al., 2007; Rubio et al., 2014, 2013).
A history of mental health treatment was less robustly related to treatment seeking for new SUDs. Pervasive problems exist in integrating substance abuse treatment with other mental health services (Drake et al., 1998, 1996; McGovern and McLellan, 2008; McGovern et al., 2007; Watkins et al., 2005). Screening for SUD remains uneven (Pilowsky and Wu, 2012); some mental health professionals receive only limited training in SUD treatment and/or lack confidence in their ability to treat SUD. Negative perceptions of individuals with SUD may further impede referrals from general mental health to SUD treatment. Although screening, brief intervention, and referral for treatment (SBIRT) models (Babor et al., 2007; Bernstein et al., 2009) have shown some promise, our data suggests that the integration of treatment for SUD and other psychiatric disorders continues to be an area with great opportunities for improving access to care.
Individuals who had not attended college were more likely to seek treatment for alcohol abuse and dependence than their college-educated peers. This contrasts with findings in mood and anxiety disorders (Olfson et al., 2012; Wang et al., 2005), but is in accord with recent findings from the National Survey on Drug Use and Health indicating that socioeconomically less-advantaged groups are more likely to receive treatment for SUD (Cook and Alegria, 2011). A similar education effect was not observed for treatment of drug use and dependence, which might be related to the greater role of mandated treatment in drug versus alcohol use disorders.
The effects of comorbid psychiatric disorders on treatment-seeking for SUD was substantially smaller than previously reported corresponding effects on treatment-seeking for mood (Moreno et al., 2012; Olfson et al., 2012) or anxiety disorders (Iza et al., 2013). The smaller effects on treatment-seeking for SUD are consistent with a predominance of external factors, rather than internal motivation on treatment-seeking for SUD. In the multivariable models, bipolar disorder increased the likelihood of treatment-seeking for alcohol abuse and dependence, but not for drug abuse or dependence. The reason for these associations may be related to the differences in the pharmacological effects of alcohol and drugs or their effects on bipolar symptoms. It is also possible that alcohol abuse and dependence are perceived as more severe in the presence of mood swings, whereas comorbidity of bipolar disorder does not increase the perceived severity of drug abuse and dependence. Furthermore, individuals with bipolar and alcohol use disorders, which commonly co-occur (Blanco et al., 2002; Hasin et al., 2007; Oquendo et al., 2010), may enter the treatment system through the treatment of bipolar disorder and then be referred for the treatment of their alcohol abuse or dependence, while individuals with bipolar disorder and drug abuse or dependence seek help directly in substance abuse treatment-settings.
Increased probability of treatment-seeking among individuals with avoidant and schizoid personality disorder may be related to their high degree of social isolation (Davis et al., 2013). The reasons for the association between dysthymia and increase treatment-seeking for alcohol dependence and drug abuse, but not for alcohol abuse or drug dependence are less clear and deserve further study.
In the adjusted models, several disorders decreased the likelihood of treatment-seeking. These included specific phobia and narcissistic personality disorder for alcohol abuse as well as alcohol dependence, alcohol abuse for drug abuse, antisocial personality for drug dependence, and alcohol dependence for drug abuse and dependence. Fears regarding the health care system (specific phobias), increased interpersonal sensitivity to rejection (narcissistic personality disorder), comorbidity with other SUD (alcohol abuse and dependence), or a heightened tendency to externalize problems (antisocial personality disorder) may contribute to avoidance of help-seeking. The findings about pathological gambling may be related to the low treatment-seeking rates for this disorder (Blanco et al., 2006).
The findings of this study should be interpreted in light of several limitations. First, as in previous studies of probability of treatment-seeking (Wang et al., 2004; Olfson et al., 2012), information about health insurance coverage, income, and geographic location for each year of the person’s life was not available. Second, we examined patterns of treatment-seeking among all individuals with SUD. Because many individuals achieve remission without accessing treatment (Blanco et al., 2013c; Lopez-Quintero et al., 2011), it is possible that some individuals with SUD may not require treatment, although recent data suggest that treatment for SUD increases the probability of remission and decreases the probability of new onset of other SUDs (Blanco et al., 2014a). There is a need to systematically examine how to most appropriately define objective need for the treatment. Third, information on some potentially important determinants of help-seeking, such as local availability of SUD treatment services (Cummings et al., 2014), was not available. Fourth, we based our analyses in DSM-IV categories. Recent work proposes cross-walks between DSM-IV and DSM-5 disorders and suggests different potential thresholds (Compton et al., 2013). Our analyses, indicating that more severe SUD categories are associated with greater likelihood of treatment suggest that higher thresholds in those cross-walks tend to be associated with greater rates of treatment. Future studies, collecting information on DSM-5 categories should test this prediction. Fifth, to maximize statistical power and increase the stability of the estimates, we examined jointly bipolar I and II disorders, although SUDs are more strongly associated with bipolar I than bipolar II disorder and they may differ in their clinical characteristics, patterns of comorbidity, course, and prognostic implications (Chamorro et al., 2012; Moreno et al., 2012; Sala et al., 2014, 2012). Similarly, we examined all drugs together, although patterns of treatment-seeking may vary by drug.
Seeking help for substance use disorders is a complex process that involves individual, clinical, social, economic, cultural, and, sometimes, legal determinants. We found that greater severity of substance use severity as measured by dependence rather than abuse and having received previous SUD treatment markedly increase the likelihood of seeking treatment for a new SUD. Past treatment of psychiatric disorders modestly increased treatment of alcohol abuse. Early age of SUD onset, belonging to an earlier birth cohort, and receiving higher education all decreased the probability of SUD treatment contact. Psychiatric comorbidity operated in a more complex manner with some disorders increasing and other decreasing the probability of treatment-seeking. Given the high rates of SUD, their substantial toll on the individual and society, and the importance of external rather than internal motivators for treatment, these patterns suggest the need for innovative approaches to increase timely access to care for individuals with SUD.
Acknowledgments
Role of Funding Sources
Funding for this study was provided in parts by NIH grants DA019606 and CA133050 and the New York State Psychiatric Institute (Dr. Blanco). The NIH and the NYSPI had no further role in the study design, collection, analysis or interpretation of the data, the writing of the manuscript or the decision to submit the paper for publication.
Footnotes
Contributors
Carlos Blanco designed the study and wrote the initial draft of the manuscript. Shuai Wang undertook the statistical analysis. All authors contributed to and have approved the final manuscript.
Conflict of Interest Statement
All the authors declare that they have no conflicts of interest.
References
- Aharonovich E, Liu X, Nunes E, Hasin DS. Suicide attempts in substance abusers: effects of major depression in relation to substance use disorders. Am. J. Psychiatry. 2002;159:1600–1602. doi: 10.1176/appi.ajp.159.9.1600. [DOI] [PubMed] [Google Scholar]
- Alegria M, Canino G, Rios R, Vera M, Calderon J, Rusch D, Ortega AN. Inequalities in use of specialty mental health services among Latinos, African Americans, and non-Latino whites. Psychiatr. Serv. 2002;53:1547–1555. doi: 10.1176/appi.ps.53.12.1547. [DOI] [PubMed] [Google Scholar]
- Armstrong TD, Costello EJ. Community studies on adolescent substance use, abuse, or dependence and psychiatric comorbidity. J. Consult. Clin. Psychol. 2002;70:1224–1239. doi: 10.1037//0022-006x.70.6.1224. [DOI] [PubMed] [Google Scholar]
- Arria AM, Garnier-Dykstra LM, Cook ET, Caldeira KM, Vincent KB, Baron RA, O’Grady KE. Drug use patterns in young adulthood and post-college employment. Drug Alcohol Depend. 2012;127:23–30. doi: 10.1016/j.drugalcdep.2012.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babor TF, McRee BG, Kassebaum PA, Grimaldi PL, Ahmed K, Bray J. Screening, brief intervention, and referral to treatment (SBIRT): toward a public health approach to the management of substance abuse. Subst. Abuse. 2007;28:7–30. doi: 10.1300/J465v28n03_03. [DOI] [PubMed] [Google Scholar]
- Bernstein E, Bernstein JA, Stein JB, Saitz R. SBIRT in emergency care settings: are we ready to take it to scale? Acad. Emerg. Med. 2009;16:1072–1077. doi: 10.1111/j.1553-2712.2009.00549.x. [DOI] [PubMed] [Google Scholar]
- Blanco C, Hasin DS, Petry N, Stinson FS, Grant BF. Sex differences in subclinical and DSM-IV pathological gambling: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychol. Med. 2006;36:943–954. doi: 10.1017/S0033291706007410. [DOI] [PubMed] [Google Scholar]
- Blanco C, Iza M, Schwartz RP, Rafful C, Wang S, Olfson M. Probability and predictors of treatment-seeking for prescription opioid use disorders: a national study. Drug Alcohol Depend. 2013a;131:143–148. doi: 10.1016/j.drugalcdep.2012.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanco C, Krueger RF, Hasin DS, Liu SM, Wang S, Kerridge BT, Saha T, Olfson M. Mapping common psychiatric disorders: structure and predictive validity in the National Epidemiologic Survey on Alcohol and Related Conditions. JAMA Psychiatry. 2013b;70:199–208. doi: 10.1001/jamapsychiatry.2013.281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanco C, Laje G, Olfson M, Marcus SC, Pincus HA. Trends in the treatment of bipolar disorder by outpatient psychiatrists. Am. J. Psychiatry. 2002;159:1005–1010. doi: 10.1176/appi.ajp.159.6.1005. [DOI] [PubMed] [Google Scholar]
- Blanco C, Okuda S, Wang SM, Liu G, Olfson M. Testing the drug substitution switching-addictions hypothesis. A prospective study in a nationally representative sample. JAMA Psychiatry. 2014a;71:1246–1253. doi: 10.1001/jamapsychiatry.2014.1206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanco C, Rafful C, Wall MM, Ridenour TA, Wang S, Kendler KS. Towards a comprehensive developmental model of cannabis use disorders. Addiction. 2014b;109:284–294. doi: 10.1111/add.12382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanco C, Secades-Villa R, Garcia-Rodriguez O, Labrador-Mendez M, Wang S, Schwartz RP. Probability and predictors of remission from life-time prescription drug use disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J. Psychiatr. Res. 2013c;47:42–49. doi: 10.1016/j.jpsychires.2012.08.019. [DOI] [PubMed] [Google Scholar]
- Blanco C, Wall MM, He JP, Krueger RF, Olfson M, Jin CJ, Burstein M, Merikangas KR. The space of common psychiatric disorders in adolescents: comorbidity structure and individual latent liabilities. J. Am. Acad. Child Adolesc. Psychiatry. 2015;54:45–52. doi: 10.1016/j.jaac.2014.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canino G, Bravo M, Ramirez R, Febo VE, Rubio-Stipec M, Fernandez RL, Hasin D. The Spanish Alcohol Use Disorder and Associated Disabilities Interview Schedule (AUDADIS): reliability and concordance with clinical diagnoses in a Hispanic population. J. Stud. Alcohol. 1999;60:790–799. doi: 10.15288/jsa.1999.60.790. [DOI] [PubMed] [Google Scholar]
- Chamorro J, Bernardi S, Potenza MN, Grant JD, Marsh R, Wang S, Blanco C. Impulsivity in the general population: a national study. J. Psychiatr. Res. 2012;46:994–1001. doi: 10.1016/j.jpsychires.2012.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chatterji S, Saunders JB, Vrasti R, Grant BF, Hasin D, Mager D. Reliability of the alcohol and drug modules of the Alcohol Use Disorder and Associated Disabilities Interview Schedule—Alcohol/Drug-Revised (AUDADIS-ADR): an international comparison. Drug Alcohol Depend. 1997;47:171–185. doi: 10.1016/s0376-8716(97)00088-4. [DOI] [PubMed] [Google Scholar]
- Chiappetta V, García-Rodrígueza O, Jin CJ, Secades-Villa R, Blanco C. Predictors of quit attempts and successful quit attempts among individuals with alcohol use disorders in a nationally representative sample. Drug Alcohol Depend. 2014;141:134–144. doi: 10.1016/j.drugalcdep.2014.05.019. [DOI] [PubMed] [Google Scholar]
- Christiana JM, Gilman SE, Guardino M, Mickelson K, Morselli PL, Olfson M, Kessler RC. Duration between onset and time of obtaining initial treatment among people with anxiety and mood disorders: an international survey of members of mental health patient advocate groups. Psychol. Med. 2000;30:693–703. doi: 10.1017/s0033291799002093. [DOI] [PubMed] [Google Scholar]
- Compton WM, Dawson DA, Goldstein RB, Grant BF. Crosswalk between DSM-IV dependence and DSM-5 substance use disorders for opioids, cannabis, cocaine and alcohol. Drug Alcohol Depend. 2013;132:387–390. doi: 10.1016/j.drugalcdep.2013.02.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton WM, Thomas YF, Stinson FS, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV drug abuse and dependence in the United States: results from the national epidemiologic survey on alcohol and related conditions. Arch. Gen. Psychiatry. 2007;64:566–576. doi: 10.1001/archpsyc.64.5.566. [DOI] [PubMed] [Google Scholar]
- Cook BL, Alegria M. Racial-ethnic disparities in substance abuse treatment: the role of criminal history and socioeconomic status. Psychiatr. Serv. 2011;62:1273–1281. doi: 10.1176/appi.ps.62.11.1273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cottler LB, Grant BF, Blaine J, Mavreas V, Pull C, Hasin D, Compton WM, Rubio-Stipec M, Mager D. Concordance of DSM-IV alcohol and drug use disorder criteria and diagnoses as measured by AUDADIS-ADR, CIDI and SCAN. Drug Alcohol Depend. 1997;47:195–205. doi: 10.1016/s0376-8716(97)00090-2. [DOI] [PubMed] [Google Scholar]
- Cummings JR, Wen HF, Ko M, Druss BG. Race/ethnicity and geographic access to medicaid substance use disorder treatment facilities in the United States. JAMA Psychiatry. 2014;71:190–196. doi: 10.1001/jamapsychiatry.2013.3575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dakwar E, Olfson M, Wang S, Blanco C. First treatment contact for attention-deficit hyperactivity disorder (adhd): predictors of treatment-seeking and gender differences. Psychiatr. Serv. 2014 doi: 10.1176/appi.ps.201300298. http://dx.doi.org/10.1176/appi.ps.201300298 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis GP, Compton M, Levin FR, Wang S, Blanco C. Association between cannabis use, psychosis, and schizotypal personality disorder: findings from the National Epidemiologic Survey of Alcohol and Related Conditions. Schizophr. Res. 2013;151:197–202. doi: 10.1016/j.schres.2013.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degenhardt L, Hall W. Extent of illicit drug use and dependence, and their contribution to the global burden of disease. Lancet. 2012;379:55–70. doi: 10.1016/S0140-6736(11)61138-0. [DOI] [PubMed] [Google Scholar]
- Drake RE, Mercer-McFadden C, Mueser KT, McHugo GJ, Bond GR. Review of integrated mental health and substance abuse treatment for patients with dual disorders. Schizophr. Bull. 1998;24:589–608. doi: 10.1093/oxfordjournals.schbul.a033351. [DOI] [PubMed] [Google Scholar]
- Drake RE, Mueser KT, Clark RE, Wallach MA. The course, treatment, and outcome of substance disorder in persons with severe mental illness. Am. J. Orthopsychiatry. 1996;66:42–51. doi: 10.1037/h0080153. [DOI] [PubMed] [Google Scholar]
- Edlund MJ, Booth BM, Han X. Who seeks care where? Utilization of mental health and substance use disorder treatment in two national samples of individuals with alcohol use disorders. J. Stud. Alcohol Drugs. 2012;73:635–646. doi: 10.15288/jsad.2012.73.635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farley-Toombs C. The stigma of a psychiatric diagnosis: prevalence, implications and nursing interventions in clinical care settings. Crit. Care Nurs. Clin. North Am. 2012;24:149–156. doi: 10.1016/j.ccell.2012.01.009. [DOI] [PubMed] [Google Scholar]
- Garcia-Rodriguez O, Secades-Villa R, Florez-Salamanca L, Okuda M, Liu S, Blanco C. Probability and predictors of relapse to smoking: results of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Drug Alcohol Depend. 2013;132:479–785. doi: 10.1016/j.drugalcdep.2013.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- García-Rodrígueza O, Blanco C, Wall MM, Wang S, Jin CJ, Kendler KS. Towards a comprehensive developmental model of smoking initiation and nicotine dependence. Drug Alcohol Depend. 2014;144:160–169. doi: 10.1016/j.drugalcdep.2014.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gee GC, Spencer M, Chen J, Yip T, Takeuchi DT. The association between self-reported racial discrimination and 12-month DSM-IV mental disorders among Asian Americans nationwide. Soc. Sci. Med. 2007;64:1984–1996. doi: 10.1016/j.socscimed.2007.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant B, Kaplan K, Moore T, Kimball J. Bethesda, MD: NIH; 2007a. 2004–2005 Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions: Source and Accuracy Statement. [Google Scholar]
- Grant B, Moore T, Shepard J, Kaplan K. Bethesda, MD: NIH; 2003a. Source and Accuracy Statement: Wave 1 of the 2001–2002 National Epidemiologic Survey of Alcohol and Related Conditions (NESARC) [Google Scholar]
- Grant BF. Toward an alcohol treatment model: a comparison of treated and untreated respondents with DSM-IV alcohol use disorders in the general population. Alcohol Clin. Exp. Res. 1996;20:372–378. doi: 10.1111/j.1530-0277.1996.tb01655.x. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou PS, Kay W, Pickering R. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug Alcohol Depend. 2003b;71:7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- Grant BF, Harford TC, Dawson DA, Chou PS, Pickering RP. The Alcohol Use Disorder and Associated Disabilities Interview Schedule (AUDADIS): reliability of alcohol and drug modules in a general population sample. Drug Alcohol Depend. 1995;39:37–44. doi: 10.1016/0376-8716(95)01134-k. [DOI] [PubMed] [Google Scholar]
- Grant BF, Kaplan KK, Stinson FS. Bethesda: NIAAA; 2007b. Source and Accuracy Statement: The Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. [Google Scholar]
- Green AE, Bekman NM, Miller EA, Perrott JA, Brown SA, Aarons GA. Parental awareness of substance use among youths in public service sectors. J. Stud. Alcohol Drugs. 2011;72:44–52. doi: 10.15288/jsad.2011.72.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin D, Carpenter KM, McCloud S, Smith M, Grant BF. The Alcohol Use Disorder and Associated Disabilities Interview Schedule (AUDADIS): reliability of alcohol and drug modules in a clinical sample. Drug Alcohol Depend. 1997a;44:133–141. doi: 10.1016/s0376-8716(97)01332-x. [DOI] [PubMed] [Google Scholar]
- Hasin D, Grant BF, Cottler L, Blaine J, Towle L, Ustun B, Sartorius N. Nosological comparisons of alcohol and drug diagnoses: a multisite, multi-instrument international study. Drug Alcohol Depend. 1997b;47:217–226. doi: 10.1016/s0376-8716(97)00092-6. [DOI] [PubMed] [Google Scholar]
- Hasin D, Paykin A. Alcohol dependence and abuse diagnoses: concurrent validity in a nationally representative sample. Alcohol Clin. Exp. Res. 1999;23:144–150. [PubMed] [Google Scholar]
- Hasin DS, Grant B, Endicott J. The natural history of alcohol abuse: implications for definitions of alcohol use disorders. Am. J. Psychiatry. 1990;147:1537–1541. doi: 10.1176/ajp.147.11.1537. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Muthuen B, Wisnicki KS, Grant B. Validity of the bi-axial dependence concept: a test in the US general population. Addiction. 1994;89:573–579. doi: 10.1111/j.1360-0443.1994.tb03333.x. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Schuckit MA, Martin CS, Grant BF, Bucholz KK, Helzer JE. The validity of DSM-IV alcohol dependence: what do we know and what do we need to know? Alcohol. Clin. Exp. Res. 2003;27:244–252. doi: 10.1097/01.ALC.0000060878.61384.ED. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch. Gen. Psychiatry. 2007;64:830–842. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Van Rossem R, McCloud S, Endicott J. Differentiating DSM-IV alcohol dependence and abuse by course: community heavy drinkers. J. Subst. Abuse. 1997c;9:127–135. doi: 10.1016/s0899-3289(97)90011-0. [DOI] [PubMed] [Google Scholar]
- Havassy BE, Alvidrez J, Owen KK. Comparisons of patients with comorbid psychiatric and substance use disorders: implications for treatment and service delivery. Am. J. Psychiatry. 2004;161:139–145. doi: 10.1176/appi.ajp.161.1.139. [DOI] [PubMed] [Google Scholar]
- Hedden SL, Gfroerer JC. Correlates of perceiving a need for treatment among adults with substance use disorder: results from a national survey. Addict. Behav. 2011;36:1213–1222. doi: 10.1016/j.addbeh.2011.07.026. [DOI] [PubMed] [Google Scholar]
- Iza M, Olfson M, Vermes D, Hoffer M, Wang S, Blanco C. Probability and predictors of first treatment contact for anxiety disorders in the United States: analysis of data from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) J. Clin. Psychiatry. 2013;74:1093–1100. doi: 10.4088/JCP.13m08361. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Crum RM, Warner LA, Nelson CB, Schulenberg J, Anthony JC. Lifetime co-occurrence of DSM-III-R alcohol abuse and dependence with other psychiatric disorders in the National Comorbidity Survey. Arch. Gen. Psychiatry. 1997;54:313–321. doi: 10.1001/archpsyc.1997.01830160031005. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Olfson M, Berglund PA. Patterns and predictors of treatment contact after first onset of psychiatric disorders. Am. J. Psychiatry. 1998;155:62–69. doi: 10.1176/ajp.155.1.62. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Zhao S, Katz SJ, Kouzis AC, Frank RG, Edlund M, Leaf P. Past-year use of outpatient services for psychiatric problems in the National Comorbidity Survey. Am. J. Psychiatry. 1999;156:115–123. doi: 10.1176/ajp.156.1.115. [DOI] [PubMed] [Google Scholar]
- Lopez-Quintero C, Hasin DS, De Los Cobos JP, Pines A, Wang S, Grant BF, Blanco C. Probability and predictors of remission from life-time nicotine, alcohol, cannabis or cocaine dependence: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Addiction. 2011;106:657–669. doi: 10.1111/j.1360-0443.2010.03194.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackenzie CS, Reynolds K, Cairney J, Streiner DL, Sareen J. Disorder-specific mental health service use for mood and anxiety disorders: associations with age, sex, and psychiatric comorbidity. Depress. Anxiety. 2012;29:234–242. doi: 10.1002/da.20911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGovern MP, McLellan AT. The status of addiction treatment research with co-occurring substance use and psychiatric disorders. J. Subst. Abuse Treat. 2008;34:1–2. doi: 10.1016/j.jsat.2007.03.007. [DOI] [PubMed] [Google Scholar]
- McGovern MP, Xie H, Acquilano S, Segal SR, Siembab L, Drake RE. Addiction treatment services and co-occurring disorders: the ASAM-PPC-2R taxonomy of program dual diagnosis capability. J. Addict. Dis. 2007;26:27–37. doi: 10.1300/J069v26n03_04. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, Mehta RL, Molnar BE, Walters EE, Swendsen JD, Aguilar-Gaziola S, Bijl R, Borges G, Caraveo-Anduaga JJ, DeWit DJ, Kolody B, Vega WA, Wittchen HU, Kessler RC. Comorbidity of substance use disorders with mood and anxiety disorders: results of the International Consortium in Psychiatric Epidemiology. Addict. Behav. 1998;23:893–907. doi: 10.1016/s0306-4603(98)00076-8. [DOI] [PubMed] [Google Scholar]
- Mertens JR, Lu YW, Parthasarathy S, Moore C, Weisner CM. Medical and psychiatric conditions of alcohol and drug treatment patients in an HMO: comparison with matched controls. Arch. Intern. Med. 2003;163:2511–2517. doi: 10.1001/archinte.163.20.2511. [DOI] [PubMed] [Google Scholar]
- Mojtabai R, Crum RM. Perceived unmet need for alcohol and drug use treatments and future use of services: results from a longitudinal study. Drug Alcohol Depend. 2012;127:59–64. doi: 10.1016/j.drugalcdep.2012.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mojtabai R, Olfson M, Mechanic D. Perceived need and help-seeking in adults with mood, anxiety, or substance use disorders. Arch. Gen. Psychiatry. 2002;59:77–84. doi: 10.1001/archpsyc.59.1.77. [DOI] [PubMed] [Google Scholar]
- Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. JAMA. 2004;291:1238–1245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- Moodley-Kunnie T. Attitudes and perceptions of health professionals toward substance use disorders and substance-dependent individuals. Int. J. Addict. 1988;23:469–475. doi: 10.3109/10826088809039212. [DOI] [PubMed] [Google Scholar]
- Moreno C, Hasin DS, Arango C, Oquendo MA, Vieta E, Liu SL, Grant B, Blanco C. Depression in bipolar versus major depressive disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Bipolar Disord. 2012;14:271–282. doi: 10.1111/j.1399-5618.2012.01009.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mumola CJ, Karberg JC. Special Report October 2006. Washington, DC: US Department of Justice. Bureau of Justice Statistics; 2004. Drug use and dependence, state and federal prisoners. [Google Scholar]
- National Drug Intelligence Center. United States Department of Justice; Washington, D.C: 2014. [Accessed March 10, 2014]. The economic impact of illicit drug use on American society. Retrieved from http://www.justice.gov/ndic/pubs44/44731/44731p.pdf. [Google Scholar]
- Nelson CB, Rehm J, Ustun TB, Grant B, Chatterji S. Factor structures for DSM-IV substance disorder criteria endorsed by alcohol, cannabis, cocaine and opiate users: results from the WHO reliability and validity study. Addiction. 1999;94:843–855. doi: 10.1046/j.1360-0443.1999.9468438.x. [DOI] [PubMed] [Google Scholar]
- Olfson M, Blanco C, Shuai W, Correll C. National trends in the office-based treatment of children, adolescents, and adults with antipsychotics. Arch. Gen. Psychiatry. 2012;69:1247–1256. doi: 10.1001/archgenpsychiatry.2012.647. [DOI] [PubMed] [Google Scholar]
- Olfson M, Kessler RC, Berglund PA, Lin E. Psychiatric disorder onset and first treatment contact in the United States and Ontario. Am. J. Psychiatry. 1998;155:1415–1422. doi: 10.1176/ajp.155.10.1415. [DOI] [PubMed] [Google Scholar]
- Oquendo MA, Currier D, Liu S, Hasin D, Grant B, Blanco C. Increased risk for suicidal behavior in comorbid bipolar disorder and alcohol use disorders. J. Clin. Psychiatry. 2010;71:902–909. doi: 10.4088/JCP.09m05198gry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pilowsky DJ, Wu LT. Screening for alcohol and drug use disorders among adults in primary care: a review. Subst. Abuse Rehabil. 2012;3:25–34. doi: 10.2147/SAR.S30057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pull CB, Saunders JB, Mavreas V, Cottler LB, Grant BF, Hasin DS, Blaine J, Mager D, Ustun BT. Concordance between ICD-10 alcohol and drug use disorder criteria and diagnoses as measured by the AUDADIS-ADR, CIDI and SCAN: results of a cross-national study. Drug Alcohol Depend. 1997;47:207–216. doi: 10.1016/s0376-8716(97)00091-4. [DOI] [PubMed] [Google Scholar]
- Regier DA, Narrow WE, Rae DS, Manderscheid RW, Locke BZ, Goodwin FK. The de facto US mental and addictive disorders service system. Epidemiologic catchment area prospective 1-year prevalence rates of disorders and services. Arch. Gen. Psychiatry. 1993;50:85–94. doi: 10.1001/archpsyc.1993.01820140007001. [DOI] [PubMed] [Google Scholar]
- Ruan WJ, Goldstein RB, Chou SP, Smith SM, Saha TD, Pickering RP, Dawson DA, Huang B, Stinson FS, Grant BF. The Alcohol Use Disorder And Associated Disabilities Interview Schedule-IV (AUDADIS-IV): reliability of new psychiatric diagnostic modules and risk factors in a general population sample. Drug Alcohol Depend. 2008;92:27–36. doi: 10.1016/j.drugalcdep.2007.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubio JM, Olfson M, Perez-Fuentes G, Garcia-Toro M, Wang S, Blanco C. Effect of first episode axis i disorders on quality of life. J. Nerv. Ment. Dis. 2014;202:271–274. doi: 10.1097/NMD.0000000000000117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubio JM, Olfson M, Villegas L, Perez-Fuentes G, Wang S, Blanco C. Quality of life following remission of mental disorders: findings from the National Epidemiologic Survey on Alcohol and Related Conditions. J. Clin. Psychiatry. 2013;74:E445–E450. doi: 10.4088/JCP.12m08269. [DOI] [PubMed] [Google Scholar]
- Sala R, Goldstein B, Wang S, Blanco C. Childhood maltreatment and the course of bipolar disorders among adults: epidemiologic evidence of dose-response effects. J. Affect. Disord. 2014;165:74–80. doi: 10.1016/j.jad.2014.04.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sala R, Goldstein BI, Morcillo C, Liu SM, Castellanos M, Blanco C. Course of comorbid anxiety disorders among adults with bipolar disorder in the US population. J. Psychiatr. Res. 2012;46:865–872. doi: 10.1016/j.jpsychires.2012.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sue S, Fujino DC, Hu LT, Takeuchi DT, Zane NW. Community mental health services for ethnic minority groups: a test of the cultural responsiveness hypothesis. J. Consult. Clin. Psych. 1991;59:533–540. doi: 10.1037//0022-006x.59.4.533. [DOI] [PubMed] [Google Scholar]
- Sussman LK, Robins LN, Earls F. Treatment-seeking for depression by black and white Americans. Soc. Sci. Med. 1987;24:187–196. doi: 10.1016/0277-9536(87)90046-3. [DOI] [PubMed] [Google Scholar]
- Ustun B, Compton W, Mager D, Babor T, Baiyewu O, Chatterji S, Cottler L, Gogus A, Mavreas V, Peters L, Pull C, Saunders J, Smeets R, Stipec MR, Vrasti R, Hasin D, Room R, Van den Brink W, Regier D, Blaine J, Grant BF, Sartorius N. WHO Study on the reliability and validity of the alcohol and drug use disorder instruments: overview of methods and results. Drug Alcohol Depend. 1997;47:161–169. doi: 10.1016/s0376-8716(97)00087-2. [DOI] [PubMed] [Google Scholar]
- Vrasti R, Grant BF, Chatterji S, Ustun BT, Mager D, Olteanu I, Badoi M. Reliability of the Romanian version of the alcohol module of the WHO Alcohol Use Disorder and Associated Disabilities: Interview Schedule—Alcohol/Drug-Revised. Eur. Addict. Res. 1998;4:144–149. doi: 10.1159/000018947. [DOI] [PubMed] [Google Scholar]
- Wang PS, Berglund P, Olfson M, Pincus HA, Wells KB, Kessler RC. Failure and delay in initial treatment contact after first onset of mental disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry. 2005;62:603–613. doi: 10.1001/archpsyc.62.6.603. [DOI] [PubMed] [Google Scholar]
- Wang PS, Berglund PA, Olfson M, Kessler RC. Delays in initial treatment contact after first onset of a mental disorder. Health Serv. Res. 2004;39:393–415. doi: 10.1111/j.1475-6773.2004.00234.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang PS, Demler O, Kessler RC. Adequacy of treatment for serious mental illness in the United States. Am. J. Public Health. 2002;92:92–98. doi: 10.2105/ajph.92.1.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watkins KE, Hunter SB, Burnam MA, Pincus HA, Nicholson G. Review of treatment recommendations for persons with a co-occurring affective or anxiety and substance use disorder. Psychiatr. Serv. 2005;56:913–926. doi: 10.1176/appi.ps.56.8.913. [DOI] [PubMed] [Google Scholar]
- Zuvekas SH, Hill SC. Income and employment among homeless people: the role of mental health, health and substance abuse. J. Ment. Health Policy Econ. 2000;3:153–163. doi: 10.1002/mhp.94. [DOI] [PubMed] [Google Scholar]