Abstract
Context:
Hypothermia and frostbite injuries occur in cold weather activities and sporting events.
Evidence Acquisition:
A PubMed search was used to identify original research and review articles related to cold, frostbite, and hypothermia. Inclusion was based on their relevance to prevention and treatment of cold-related injuries in sports and outdoor activities. Dates of review articles were limited to those published after 2010. No date limit was set for the most recent consensus statements or original research.
Study Design:
Clinical review.
Level of Evidence:
Level 5.
Results:
Frostbite and hypothermia are well-documented entities with good prevention strategies and prehospital treatment recommendations that have changed very little with time. A layered approach to clothing is the best way to prevent injury and respond to weather changes. Each athlete, defined as a participant in a cold weather sport or activity, will respond to cold differently depending on anthropometric measurements and underlying medical risk factors. An understanding of wind-chill temperatures, wetness, and the weather forecast allows athletes and event coordinators to properly respond to changing weather conditions. At the first sign of a freezing cold injury, ensure warm, dry clothes and move to a protected environment.
Conclusion:
Cold injuries can be prevented, and cold weather activities are safe with proper education, preparation, and response to changing weather conditions or injury.
Keywords: frostbite, hypothermia, event medicine, injury prevention
Athletes participating in cold weather activities or events, including cross-country skiing, downhill skiing, cold-weather running, triathlons, dog sled racing, and high-altitude mountaineering adventure races, are at risk for frostbite and hypothermia.8,9,11,25 While frostbite occurs in these events, the true incidence is difficult to identify. Frostbite and hypothermia incidence may be as high as 20% in cross-country skiing, but good studies have not been conducted.25 During the 2010 Iditarod dog sled race, frostbite was the most common injury reported, occurring in 31% of survey respondents, and is the most common cold injury seen in the US Armed Forces.4,8 Incidence of frostbite in mountaineers was 366 per 1000 individuals per year, with less severe injuries being the most common.11 The primary reason that mountaineers felt they developed frostbite was inappropriate clothing, followed by incorrect equipment and lack of knowledge on how to deal with cold exposure.11 The mountaineer survey study highlights the need for continued education of our cold-weather athletes. Frostbite and hypothermia are well-documented entities with good prevention strategies and prehospital treatment recommendations that have changed very little with time. Cold weather exercise can be done safely with education, proper preparation, and appropriate response to changing weather conditions.
Frostbite
Frostbite is a direct freezing injury to peripheral tissues that occurs when the skin temperature drops below −0.5°C.13 It most commonly occurs in cold-exposed areas of the body with less blood flow due to vascular anatomy or peripheral vasoconstriction.3,18 Common sites include the nose, ears, fingers, and toes, which are further from the body’s core and more susceptible to vasoconstriction. Contact frostbite can also occur when skin is exposed to a substance with a temperature below skin-freezing temperature (metal, gasoline, stove fuel, ice packs, or alcohol).7,18 Gasoline and other petroleum products are particularly risky as they have extremely low freezing points (–50°C range), and rapid evaporation adds to the tissue freezing potential. Athletes will feel a sense of skin cooling at skin temperatures of 28°C, pain at approximately 20°C, and numbness as skin temperatures drop below 10°C.3
There are many published frostbite classification schemes. Most follow the classification for burn injury and are based on initial presentation and advanced imaging after rewarming. These classifications are difficult to use on the sideline or in the field, and a simpler 2-tier classification scheme was recommended by the Wilderness Medical Society Practice Guidelines.17 The severity of frostbite injury is proportional to the temperature, duration of exposure, and amount and depth of frozen tissue. It is important to recognize skin changes that may present prior to true frostbite injury. Frostnip is a superficial nonfreezing injury of exposed skin. Athletes may feel skin numbness and the skin may appear pale or erythematous. Ice crystals may form on the surface of the skin. Importantly, these symptoms resolve quickly with skin covering or behavior modification, and no long-term damage occurs.17 Responding to frostnip and understanding the factors that predispose to freezing skin injuries will help prevent more significant injury. Superficial frostbite corresponds to a first- or second-degree injury with minimal tissue loss expected. In first-degree frostbite, patients present with numbness, erythema, a white or yellow plaque, and no obvious tissue loss. Second-degree frostbite results in superficial clear or milky blisters surrounded by erythema and edema.17 Deep frostbite corresponds to a third- or fourth-degree injury, and tissue loss is expected. In third-degree frostbite, patients develop hemorrhagic blisters, suggesting deeper injury. Initially, this injury may appear similar to second-degree frostbite, but the hemorrhagic blisters appear within 24 hours. In fourth-degree frostbite, injury extends through the dermis and results in necrosis of muscle and bone.17
The precise mechanism of frostbite injury is not fully understood. Cellular injury and ischemia result from direct and indirect effects of the freezing temperatures. Initially, as the skin cools, vasoconstriction and tissue ischemia occur resulting in pain, numbness, and edema. Ice crystals may then form in the intra- or extracellular spaces, causing changes in cell structure. This leads to electrolyte shifts that result in cellular dehydration from the outward diffusion of water. Cell membrane lysis and death may occur as the cell water expands and contracts in the freeze-thaw cycle. As tissues rewarm, the extracellular ice crystals melt and increase tissue edema and inflammation. Vessels alternate between vasodilation and vasoconstriction, resulting in increased vessel permeability or coagulation. This is followed by progressive tissue ischemia and infarction from inflammation, vasoconstriction, and destruction of microcirculation from thrombus formation. Studies suggest that this cascade of events is made worse if refreezing follows tissue thawing.17,18
Hypothermia
Hypothermia is defined as a core body temperature below 35°C (95°F) and occurs when total body heat loss exceeds physiologic heat production.1,2,3,18 Hypothermia is characterized as mild, moderate, or severe depending on core body temperature and symptoms. Mild hypothermia ranges from a core temperature of 32°C to 35°C (89.6°F-95°F) and can be recognized by increased shivering, social withdrawal, and other behavior changes.3,18 If cold exposure continues and an athlete’s core body temperature drops between 28°C to 32°C (82.4°F-89.6°F), moderate hypothermia occurs.3,18 At this temperature, pupils dilate and cardiac arrhythmias can occur. Athletes will lose the ability to shiver, become more confused, and ultimately lose consciousness. In severe hypothermia, with core body temperatures below 28°C (86°F), severe bradycardia and ventricular fibrillation become more likely, along with the loss of deep tendon reflexes and voluntary motion.3 The risk of cardiac arrest increases as the core temperatures drop below 32°C and is even more likely below 28°C.2 Despite worsening symptoms with lower core temperatures, the lowest documented survival from accidental hypothermia is 13.7°C.3 The symptoms of hypothermia vary from person to person, and early recognition is important for long-term recovery and survival.3 It is important to fully rewarm hypothermic patients before pronouncing death. When access to a thermometer is not available, medical providers and first responders should suspect hypothermia if the conditions are right and treat based on symptoms. It may be safer to transport the victim before beginning the rewarming process if the local environment is unsafe for responders or resources are not available to safely rewarm.
Body Response to Cold
To preserve core body temperature, the body’s first response to cold exposure is peripheral vasoconstriction. With blood more centrally localized, heat loss to the environment is decreased. This is effective for short durations as the outer body acts as insulation for the inner core.3,18 Peripheral vasoconstriction occurs when the mean skin temperature (not core temperature) drops below 34°C to 35°C.3,23 As exposure continues at or below these temperatures, the athlete loses muscle coordination and performance decreases, and they are at risk for freezing injuries. In an attempt to protect peripheral tissues, intermittent cold-induced vasodilation results in temporary increases in blood flow and skin temperature.3,5,18 As core temperature drops further, the vasodilation response decreases and frostbite risk increases.3
Increased metabolic heat production also helps to maintain core body temperatures through involuntary shivering, increased physical activity, and other behavior modification. Shivering is an involuntary response to cold temperatures that involves muscle contractions starting at the core and spreading to the extremities. The intensity of shivering depends on the level of cold exposure and anthropometric measurements. The peak shivering response seems to occur at a skin temperature of 17°C to 20°C and a core temperature of 32°C to 35°C.6 If the core temperature drops too far, the body’s ability to maintain the shivering response declines and core body temperature drops further. The maximum shivering response is dependent on the individual and correlates with a lower body mass index, suggesting that increased body fat decreases shivering intensity.6 Shivering can increase the basal metabolic rate by as much as 5 to 6 times, so proper fuel and energy stores are required to maintain this response.3,6
Risk Factors for Cold Injury
An increased risk for cold injury results from a combination of weather, preparedness, and an athlete’s underlying medical condition. A balance of heat production to heat loss is required to maintain a normal core body temperature and protect the extremities from frostbite. Heat loss can occur through evaporation, convection, and conduction. A change in temperature balance due to clothing choices, impaired thermoregulation from underlying medical conditions, cold water immersion, and prior cold injury increases the risk of hypothermia and frostbite.7
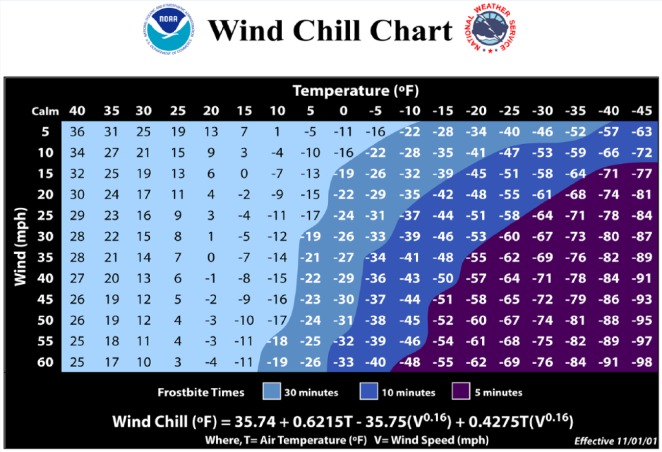
The weather combination of cold, wet, and wind is most likely to predispose an athlete to freezing injury. Therefore, temperature alone cannot be used to determine risk of cold injury. This is demonstrated in the wind-chill temperature index, which reflects convective heat loss rates (Figure 1).22 Convection results in heat loss through the direct transfer of heat from the body to moving currents, like wind or water.18
Figure 1.
Wind-chill temperature index with corresponding expected time to frostbite injury.
The wind-chill temperature estimates the temperature felt at the average human face that would result in the same heat loss rate in calm wind conditions.24 With wind speeds of 20 mph, frostbite can occur after 30 minutes of exposure to an ambient temperature of 0°F, 10 minutes at temperatures below −15°F, and 5 minutes below approximately −35°F.22 The time to frostbite is reduced as wind speeds increase. The risk of frostbite is less than 5% when the ambient temperature is greater than −15°C (5°F).3
Newer models of whole body thermoregulation suggest that the commonly used wind-chill temperature index may predict higher facial skin temperatures than are actually seen at that temperature, suggesting that frostbite could occur at higher temperatures than predicted.24 It is important to account for apparent (human-made) wind from activities like biking, skiing, and dog sledding. Wind does decrease the effective insulation of clothing if there is no vapor barrier.3
Water immersion and exposure results in a greater convective heat transfer than air, so swimmers and athletes exposed to rain are at risk for greater heat loss at higher temperatures than would be expected for dry-weather athletes.3 The American College of Sports Medicine consensus statement on the prevention of cold weather injuries suggests that the ambient temperature used when assessing wind-chill equivalent temperatures to assess frostbite risk should be 10°C lower than the actual ambient temperature when skin is wet and exposed to the wind.3 Colder water temperatures increase the body heat loss to the environment through both convection and conduction. Conduction is a direct transfer of body heat to a solid object like the ground or clothing.18 Heat loss is proportional to the amount of body surface area that is immersed or wet. Individual athletes vary in their ability to tolerate different water temperatures and maintain adequate core body temperatures.
Evaporation of water directly from the body increases the rate of heat loss due to the loss of energy needed to convert water to vapor.18 At an air temperature of 5°C, wet clothes may double the heat loss seen in dry conditions, highlighting the importance of proper clothing.3 Interestingly, exercise in cold water and rain increases the drop in core body temperature compared with not exercising in these same conditions.3 This is due in part to a loss of the insulating effect of muscle and increased blood flow from the core to the peripheral limb muscles and in part to increased convective losses of fluid flow over the skin.
Wet, windy conditions also increase the risk of frostbite. Wet skin cools faster, reaches a lower temperature, and freezes at a higher threshold than dry skin.3,13,20 Skin temperature in a forearm exposed to cold water immersion was inversely proportional to the forearm circumference of the individual, suggesting that higher body fat or muscle thickness may be protective.5
Each individual athlete has a different risk of cold injury during the same weather conditions. A higher percent body fat increases insulation. Athletes with a higher percent body fat, increased subcutaneous fat thickness, and higher muscle mass maintain their core temperature better than individuals with less muscle and fat.3 The US Armed Forces documents increased risk of cold injury in women compared with men.4 This is likely due to differences in anthropometric measurements, including an increased surface area and smaller total body mass in women compared with men.3 The US military also documents increased risk in the age group less than 20 years, which may be due to a lack of prior cold weather experience and education.4 Other studies would suggest that age >60 years is a risk factor for cold-induced injury due to reduced vasoconstriction and heat conservation and a decline in physical fitness.3 Younger children may also be at risk, particularly in cold water swimming, secondary to decreased subcutaneous fat.3 Physical fitness and training levels alone do not change risk for cold injury. Changes in tolerance are likely due to anthropometric differences. In addition, a physically fit individual may be able to maintain a higher metabolic rate for longer periods of time to help maintain a normal core body temperature.3
Underlying medical conditions can also predispose to cold injury if it interferes with total body heat production or thermoregulation. Hypoglycemia, various endocrine abnormalities, and low caloric intake decrease shivering response and heat production.3,7 Increased total body heat loss can occur with chronic skin conditions, hyperhidrosis, burns, and sunburns. The nervous and vascular systems are critical to thermoregulation, and medications that modify these systems by decreasing a patient’s response time (benzodiazepines) or increasing vasoconstriction (beta blockers) may increase the risk of cold injury.7 Raynaud syndrome has been shown to impair thermoregulatory mechanisms, resulting in decreased blood flow to the digits during cold exposure and prolonged rewarming, which may increase the risk of frostbite.10
A prior frostbite injury may be a risk factor for future injury. In a military study, soldiers were 1.68 times as likely to suffer a repeat cold injury when compared with military personnel without prior injury.26 Newer studies of Alpinists with and without prior frostbite injury show no difference in finger or toe skin temperature changes between digits with prior frostbite injury and a control group during cold water immersion.21 There were also no differences in the skin temperatures between previously injured and uninjured toes of the same individual.21 This suggests that a prior freezing cold injury may not alter vascular function and increase the risk of repeat frostbite injury as previously thought. Further studies are needed to determine the reason for the observed increased risks associated with prior freezing injuries.
Prevention of Cold Injury
Understanding the pathophysiology and risk factors for frostbite and hypothermia is critical when discussing prevention strategies. Injury will occur when tissue heat loss exceeds the ability of local tissue perfusion to prevent freezing of soft tissues and drop in core body temperatures. Understanding the weather conditions, air temperatures, wind chill, water temperatures, and the planned exercise will help to determine a participant’s risk of cold injury and whether the event is safe to continue. Responding to and alerting others to a change in weather conditions is critical.3 Event coordinators can also respond to changing weather temperatures through altered start times and a do-not-start temperature.
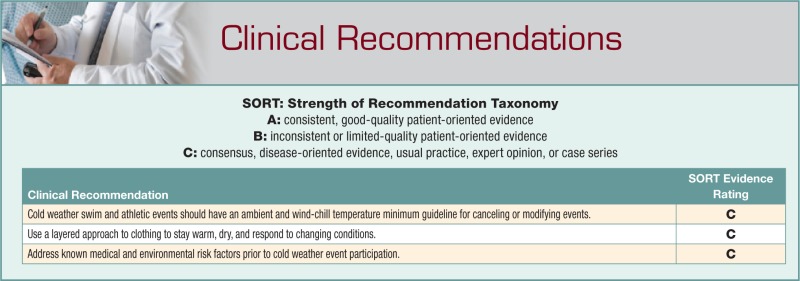
The Minnesota State High School League has guidelines for Nordic skiing that include race cancellations or training modifications for temperatures below −20°C (–4°F) and no practice or training at ambient temperatures of −23°C (–10°F) or wind chill of −40°C (–40°F).19 The International Ski Federation has set a temperature of −20°C (–4°F) as a no-start temperature and allows race judges to determine a higher no-start temperature if there are high winds or heavy snows.12 USA Triathlon updated their swim temperature recommendations for athletes and race directors in 2013. For events over 1500 meters, they recommend shortening swims for water temperatures of 53°F to 56°F (11.7°C-13.3°C) and cancelling events for water temperatures of less than 53°F (11.7°C).27 Event coordinators and medical directors should consider having an ambient and wind-chill temperature guideline for cold weather swim and organized athletic events to decrease risks of frostbite and hypothermia.
Preparation for environmental exposures is the most important thing an athlete and medical team can do to prevent frostbite and hypothermia. Mountaineers identified inappropriate clothing, lack or incorrect use of equipment, and lack of knowledge on cold preparation as the main 3 causes of developing frostbite in a survey-based study.11 Proper layering of clothing and rapid response to changing weather conditions can help maintain adequate core temperature and decrease heat loss in cold weather. Each individual will need different layers depending on their heat production and the weather conditions. Athletes should be encouraged to individualize layering based on past cold weather experience and training.3 Equally important to staying warm is limiting body sweat, which increases wetness and cold injury risk. The innermost layer, which is in direct contact with the skin, should wick moisture away from the body to maintain an insulating air layer next to the skin and transfer water to outer layers of clothing.3,7,18 The exception to this is wool, which can retain heat even when wet. Good base layers include polypropylene, polyester, and synthetic wool. Avoid cotton layers that trap moisture. The middle layer or layers are primarily for insulation and should be made of a material like fleece or wool. The number of layers is dictated by the temperature and exertion level. As exercise intensity increases, the amount of clothing insulation needed to maintain body heat at a given temperature decreases. The outer vapor layer must allow moisture transfer, allow ventilation, and protect against wind and rain.3,7,18 Hats or balaclavas can decrease heat loss from the head. Mittens protect the hands from frostbite better than gloves.11
It is often advisable to avoid exercising in the outer protective vapor layer unless it is wet or windy and instead use it for changes in weather conditions or during rest periods to prevent overheating and wetting of the inner layers.3,7 The risk of hypothermia and frostbite increases in wet conditions, making dry clothing essential. It is important for athletes to realize that most waterproof clothing is advertised as breathable, but exercise sweat rates easily exceed the breathability of many waterproof or water-resistant materials. These outer layers may become a vapor barrier that traps moisture next to athletes’ bodies. It is safe to assume that the more waterproof clothing is, the less it will breathe.7
Frostbite injury occurs when tissue heat loss is too great for local tissue perfusion. Minimizing restrictions in blood flow helps maintain peripheral blood flow and digit temperature. This requires well-fitted clothing, boots, and mittens and addressing known conditions or medications that restrict blood flow.7 Clothing or footwear that is too tight can constrict peripheral blood flow and increase the risk of frostbite injury.3 If more than 1 pair of socks is needed, an athlete should go up 1 shoe size. Adding an extra pair of socks for added insulation may actually constrict blood flow and decrease foot perfusion. Chemical hand and foot warmers can be used to maintain peripheral warmth but should not constrict blood flow. The use of skin-protecting emollients increases the risk of frostbite and should not be used.3,14,15 Subjects who used skin emollients doubled the incidence of facial frostbite in the areas where emollients were applied.14 This is due to subjective skin warmth, a false sense of protection, and neglect of other protective measures.13,14 Keeping the core and large heat-dissipating areas (eg, head, neck, armpits) covered and warm can prevent peripheral vasoconstriction of the distal extremity as well, making the hands and feet warmer. Avoiding alcohol, caffeine, and medications that increase vasoconstriction and good control of underlying medical risk factors for each athlete are important in modifying risk as well.3,7
Caloric intake is also important in the prevention of cold injury. Shivering, heavy clothing, equipment, and the increased work associated with walking in snow can increase energy expenditure by up to 10% to 40% in cold environments if the core temperature is not maintained above resting values.3 If increased energy expenditure above baseline is expected, the increased calories can be obtained through frequent snacks during the day. Carbohydrates tend to be the limiting factor, and carbohydrate-rich foods are recommended.3 While maintaining good hydration is important to maintain adequate performance, mild to moderate dehydration alone does not increase the risk of cold injury.3
Exercise can increase core body temperatures. Adequate training for a cold-weather exercise event is critical to ensure that the exercise can be completed safely and the activity is stopped in a warm, dry, and safe environment. Collapse from exhaustion in the cold can greatly increase hypothermia and frostbite risk. Exercise is an effective prevention strategy for frostbite in dry conditions when there is no wind. In wet and/or windy conditions, the increased metabolic heat production from exercise is not sufficient to increase the temperature of exposed or covered digits.3
All athletes can respond to a changing environment, layer clothing appropriately, and maintain adequate nutrition and hydration. Recognizing the signs and symptoms of early frostbite or hypothermia can prevent worsening of the condition by changes in layering, behavior changes, or increased caloric intake. Frequent cold checks, and if feasible, a buddy system, during the athlete’s exposure is important to recognize early skin and/or behavior changes. Treatment is more effective the earlier an injury is identified.
Treatment
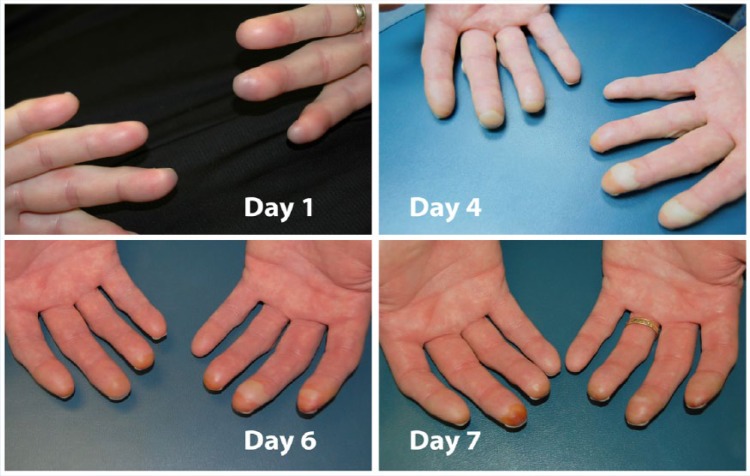
Athletes suspected of having a frostbite injury should remove wet clothing, protect the frozen tissue from further injury, and move to a warm and dry environment.17,18 Avoid weightbearing if possible to prevent avulsion fractures and worse injury.17,18 Rubbing frozen tissue to rewarm the area is not recommended.17 With studies suggesting much worse injury in thaw-refreeze injuries, the injured tissue should not be rewarmed until that athlete is in an environment with minimal risk of refreezing. Initial warming can be done using the athlete’s or first responder’s own body heat.18 Areas like the axilla tend to be the warmest. Care should be taken not to put yourself or others at risk for injury. Ideally, frostbite should be treated at a medical clinic or local medical facility where rapid rewarming and further assessment and treatment can be done. Rapid rewarming should be done in a warm-water bath at 37°C to 39°C (98.6°F-102.2°F).16,17 Spontaneous thawing of skin tissue should be allowed if rapid rewarming cannot be done. Avoid using fires or stoves to warm injured digits to prevent burn injuries.17 Warming of the injured tissue should be continued until the skin is red or purple in color and soft to touch.17 Rewarming can be painful and medications may be needed. Blisters should be left intact and may be covered with dry, loose bandages. Avoid circumferential bandages if possible to allow for swelling of the injured tissue.17 Antibiotics are not indicated unless complications of infection develop. Medical evaluation at a hospital should occur as soon as possible to further assess depth of injury and consider higher levels of treatment (Figure 2).
Figure 2.
Progression of second-degree frostbite injury from contact with fuel-soaked gloves at a wind-chill temperature of −10.3°F. The injury was treated with rapid rewarming in a warm water bath, dry loose bandages, and pain medications. Photo credit: Jessie R Fudge, MD.
Treatment for hypothermia also relies on moving an athlete to a warm and dry environment as quickly and gently as possible. Wet clothes should be replaced with dry clothing or blankets to allow passive external rewarming, and shivering should be allowed to continue. Passive rewarming is the treatment of choice for athletes with a perfusing cardiac rhythm and mild hypothermia (32°C-35°C).1,18 For more moderate cases of hypothermia with temperatures of 28°C to 32°C and a perfusing cardiac rhythm, active external rewarming may be initiated with heating pads, warm blankets, warm air through a Bair Hugger, or forced air.1,18 Some rescuers are concerned about a phenomenon called “afterdrop” in which the core body temperature drops further when cool peripheral blood is mobilized by external rewarming. This has been documented to occur in artificial cooling experiments and may explain the difference between rectal and true core temperatures.2 Recent studies with active rewarming during continuous esophageal temperature measurements suggest that active external rewarming is considered safe and effective without documented “afterdrop.”1,2 Treatment should not be delayed secondary to concerns for “afterdrop” cooling.1,2 In severe cases of hypothermia with temperatures <28°C, active internal rewarming will be needed at a center capable of higher levels of care.1,18 All athletes with moderate to severe hypothermia should be moved gently, as movement can cause ventricular fibrillation.1,18
Patients in cardiac arrest should have cardiopulmonary resuscitation (CPR) initiated immediately regardless of their temperature in addition to internal rewarming if available. Pulse and respirations will be slowed in hypothermia so longer pulse and respiratory checks may be needed to confirm a nonperfusing rhythm. CPR should not be delayed in the field.1,2 Defibrillation should be attempted, and intravenous medications should be spaced further apart than with conventional CPR.1 If an initial defibrillation attempt is not effective, CPR should be continued and further defibrillation attempts should be delayed until core body temperature increases to 30°C to 32°C.1 Aggressive rewarming techniques may not be possible in the field situation, and transport to a higher level of care is critical. First responders and medical providers should take care to avoid personal injury in these environments. Hypothermia may provide a protective effect for the brain and other organs, so transport to a higher level of care is appropriate if it is safe to do so.
Conclusion
Frostbite and hypothermia do occur in winter sports. However, they are preventable conditions and athletes should be able to participate in cold weather sporting events safely. While prevention is the most important “treatment,” field treatments for frostbite and hypothermia are effective, especially when detected early. Understanding wind-chill temperatures, wetness, and the weather forecast allows athletes and event coordinators to properly respond to changing weather conditions. A layered approach to clothing is the best way to respond to weather changes and early cold injury. At the first sign of freezing cold injury, ensure warm, dry clothes and move to a protected environment. With proper clothing and education, frostbite and hypothermia can be prevented.
Footnotes
The author reports no potential conflicts of interest in the development and publication of this article.
References
- 1. American Heart Association. 2005 American Heart Association (AHA) guidelines for cardiopulmonary resuscitation and emergency cardiovascular care Part 10.4: hypothermia. Circulation. 2005;112:IV-136-IV-138. [DOI] [PubMed] [Google Scholar]
- 2. Brown DJ, Brugger H, Boyd J, Paal P. Accidental hypothermia. N Engl J Med. 2012;367:1930-1938. [DOI] [PubMed] [Google Scholar]
- 3. Castellani JW, Young AJ, Ducharme MB, et al. American College of Sports Medicine Position Stand: prevention of cold injuries during exercise. Med Sci Sports Exerc. 2006;38:2012-2029. [DOI] [PubMed] [Google Scholar]
- 4. Connor RR. Update: cold weather injuries, active and reserve components, U.S. Armed Forces, July 2009-June 2014. MSMR. 2014;21(10):14-19. [PubMed] [Google Scholar]
- 5. Ducharme MB, VanHelder WP, Radomski MW. Cyclic intramuscular temperature fluctuations in the human forearm during cold-water immersion. Eur J Appl Physiol. 1991;63:188-193. [DOI] [PubMed] [Google Scholar]
- 6. Eyolfson DA, Tikuisis P, Xu X, Weseen G, Giesbrecht GG. Measurement and prediction of peak shivering intensity in humans. Eur J Appl Physiol. 2001;84:100-106. [DOI] [PubMed] [Google Scholar]
- 7. Fudge JR, Bennet BL, Simanis JP, Roberts WO. Medical evaluation for exposure extremes: cold. Clin J Sport Med. 2015;25:432-436. [DOI] [PubMed] [Google Scholar]
- 8. Gallea JW, Higgens GL, Germann CA, Strout TD. Injury and illness sustained by human competitors in the 2010 Iditarod sled dog race. Am J Emerg Med. 2014;32:780-784. [DOI] [PubMed] [Google Scholar]
- 9. Gammons M, Boynton M, Russell J, Wilkens K. On-mountain coverage of competitive skiing and snowboarding events. Curr Sports Med Rep. 2011;10:140-146. [DOI] [PubMed] [Google Scholar]
- 10. Greenstein D, Gupta NK, Martin P, Walker DR, Kester RC. Impaired thermoregulation in Raynaud’s phenomenon. Angiology. 1995;46:603-611. [DOI] [PubMed] [Google Scholar]
- 11. Haririchi I, Arvin A, Vash JH, Zafarmand V. Frostbite: incidence and predisposing factors in mountaineers. Br J Sports Med. 2005;39:898-901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. International Ski Federation (FIS). The International Ski Competition Rules (ICR). http://www.fis-ski.com/mm/Document/documentlibrary/Cross-Country/02/95/69/ICRCross-Country2013_clean_English.pdf. Accessed September 10, 2015.
- 13. Keatinge WR. Freezing-point of human skin. Lancet. 1960;1(7114):11-14. [DOI] [PubMed] [Google Scholar]
- 14. Lehmuskallio E. Cold protecting ointments and frostbite: a questionnaire study of 830 conscripts in Finland. Acta Derm Venereol. 1999;79:67-70. [DOI] [PubMed] [Google Scholar]
- 15. Lehmuskallio E, Rintamaki H, Anttonen H. Thermal effects of emollients on facial skin in the cold. Acta Derm Venereol. 2000;80:203-207. [DOI] [PubMed] [Google Scholar]
- 16. Malhotra MS, Mathew L. Effect of rewarming at various water bath temperatures in experimental frostbite. Aviat Space Environ Med. 1978;49:874-876. [PubMed] [Google Scholar]
- 17. McIntosh SE, Opacic M, Freer L, et al. Wilderness Medical Society practice guidelines for the prevention and treatment of frostbite: 2014 update. Wilderness Environ Med. 2014;25(4 suppl):S43-S54. [DOI] [PubMed] [Google Scholar]
- 18. McMahon JA, Howe A. Cold weather issues in sideline and event management. Curr Sports Med Rep. 2012;11:135-141. [DOI] [PubMed] [Google Scholar]
- 19. Minnesota State High School League (MSHSL) weather conditions and competition. http://www.mshsl.org/mshsl/news/weatherpolicies.pdf. Accessed September 7, 2015.
- 20. Molnar GW, Hughes AL, Wilson O, Goldman RF. Effect of skin wetting on finger cooling and freezing. J Appl Physiol. 1973;35:205-207. [DOI] [PubMed] [Google Scholar]
- 21. Morrison SH, Gorjanc J, Eiken O, Mekjavic IB. Finger and toe temperature responses to cold after freezing cold injury in elite Alpinists. Wilderness Environ Med. 2015;26:295-304. [DOI] [PubMed] [Google Scholar]
- 22. NOAA. National Weather Service. Office of Climate, Water and Weather Services. 2013. http://www.nws.noaa.gov/om/winter/windchill.html. Accessed September 13, 2015.
- 23. Savage MV, Brengelmann GL. Control of skin blood flow in the neutral zone of human body temperature regulation. J Appl Physiol (1985). 1996;80:1249-1257. [DOI] [PubMed] [Google Scholar]
- 24. Shabat YB, Shitzer A, Fiala D. Modified wind chill temperatures determined by a whole body thermoregulation model and human-based facial convection coefficients. Int J Biometeorol. 2014;58:1007-1015. [DOI] [PubMed] [Google Scholar]
- 25. Smith M, Matheson GO, Meeuwisse WH. Injuries in cross-country skiing: a critical appraisal of the literature. Sports Med. 1996;21:239-250. [DOI] [PubMed] [Google Scholar]
- 26. Sumner DS, Criblez TL, Doolittle WH. Host factors in human frostbite. Mil Med. 1974;141:454-461. [PubMed] [Google Scholar]
- 27. USA Triathlon race director toolbox: water temperature recommendations chart. http://www.usatriathlon.org/audience/race-directors/race-director-toolbox.aspx. Accessed September 7, 2015.