Abstract
Fish bone is one of the most common accidentally ingested foreign bodies, and patients commonly present to the emergency department with nonspecific symptoms. Fortunately, most of them are asymptomatic and exit the gastrointestinal tract spontaneously. However, fish bones can get impacted in any part of the aerodigestive tract and cause symptoms. Occasionally, they are asymptomatic initially after ingestion and may present remotely at a later date with serious complications such as gastrointestinal tract perforation, obstruction, and abscess formation. Radiographs are most often negative. High degree of clinical suspicion and familiarity with CT appearance can help to detect fish bone along with any associated complications, and direct further management. We describe and illustrate various CT presentations of ingested fish bone and its complications.
Fish bone is one of the most common accidentally ingested foreign bodies. They may account for up to 84% of the foreign bodies ingested accidentally (1). Majority of them are eliminated from the gastrointestinal system without any symptoms (2, 3). Complications are seen in less than 1% of the cases (3). Complications range from mild inflammatory changes to abscess formation, viscus perforation, intestinal obstruction, and bleeding. CT with intravenous contrast administration is the imaging modality of choice, as it can detect very small and even radiolucent fish bones. The multiplanar capability of CT further improves the diagnostic accuracy and may also help in management.
Predisposing factors
The predisposing factors for accidental fish bone ingestion include use of dentures, which impair palatal sensory feed back required to identify sharp objects, old age, alcoholism, mental retardation, eating rapidly, and talking while eating (3, 4). Most fish bones get lodged in the oral cavity or pharynx (5), especially in the tonsils or at the base of the tongue (1). They can also lodge in any other part of the gastrointestinal tract or rarely in trachea or major bronchi (6).
Neck
The uncomplicated cases in oral cavity or pharynx are easily visualized by the ear, nose and throat surgeon and can be removed by a scope. However, fish bones can also penetrate into deeper spaces of the neck (Fig. 1) causing edema, inflammation, airway narrowing, and abscess formation. The authors also encountered a rare case of fish bone causing perforation of the pharynx and reaching to the skin surface (Fig. 2). Rare complications like vascular perforation, thyroid abscess, and neural injury have been reported (4, 6–8). Plain radiographs are commonly employed as the first line of imaging in patients with suspected foreign body ingestion. As the vast majority of fish bones are radiolucent, a negative soft tissue radiograph cannot completely exclude the presence of one (1). A potential pitfall on plain radiographs is the presence of partial calcifications of the various normal cartilages in the neck, which can mimic a foreign body. Accurate knowledge of the precise anatomical location of various cartilages can help to solve this conundrum. Doubtful cases warrant further evaluation and CT can clarify the diagnosis (Fig. 3). CT of the neck with contrast can accurately localize the fish bone and detect any associated complications (Fig. 1).
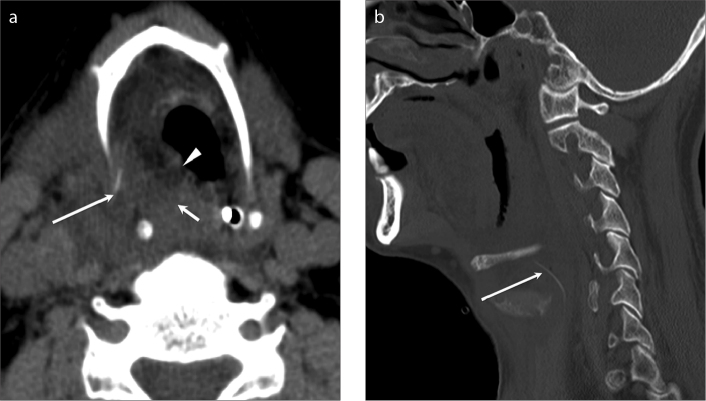
Figure 1.
a, b. Ingested fish bone with perforation of the right hypopharynx. Axial (a) and sagittal (b) contrast-enhanced CT images of the neck demonstrate a linear hyperdensity lying in the right extra laryngeal space (long arrows) suggestive of ingested fish bone. There is significant edema in the right paralaryngeal area (a, short arrow) resulting in mild narrowing of the airway (a, arrowhead).
Figure 2.

Fish bone causing perforation of the pharynx and reaching the skin surface of the neck. Coronal unenhanced CT of the neck demonstrates a linear hyperdensity in the left submandibular region, in keeping with a fish bone (arrow).
Figure 3.
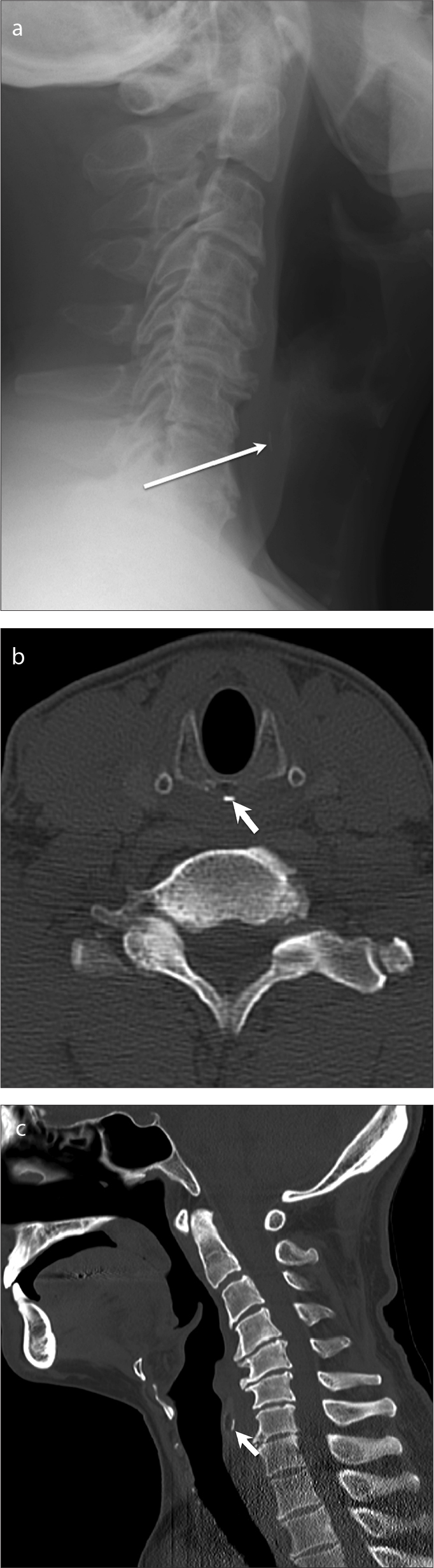
a–c. Cricoid cartilage mimicking an ingested fish bone. There is a linear hyperdensity in the prevertebral soft tissue of the neck (long arrow) on the radiograph (a) suggesting an ingested fish bone. On unenhanced CT of the neck, axial (b) and sagittal (c) reconstructed images confirm the linear density to represent dense calcification of the posterior aspect of the cricoid cartilage (b, c, short arrows) mimicking a fish bone on plain radiograph.
Upper and lower gastrointestinal tract
The most common site of impaction in the esophagus is within the cervical portion (9), mostly within the cricopharyngeus muscle at C5/C6 level (Fig. 4). The other sites of impaction within the esophagus are at the level of aortic arch, gastroesophageal junction, where normal extrinsic impression or anatomical narrowing is expected (Fig. 5). Such patients with fish bone impaction in the pharynx and esophagus usually present with symptoms like foreign body sensation, pain, and swelling. Hence, diagnosis, especially by CT scan, is not very difficult as definitive clinical history is usually present. Fish bone impaction at these sites can be complicated by esophageal perforation, bleeding, hematoma, and abscess formation. Rarely, fistulation into the adjacent trachea or great vessels can be seen (6). Thin wall, lack of adventitia, and relatively poor vascularity of the esophagus makes it more susceptible to perforation and necrosis (2) (Fig. 6).
Figure 4.

Uncomplicated ingested fish bone in the upper esophagus. Unenhanced axial CT of the neck demonstrates a linear hyperdensity (arrow) at C5/C6, approximately at the cricopharyngeous muscle level.
Figure 5.
Uncomplicated ingested fish bone at the gastroesophageal junction. Axial unenhanced CT of the abdomen demonstrates a linear hyperdensity (arrow) at the gastroesophageal junction suggestive of ingested fish bone.
Figure 6.
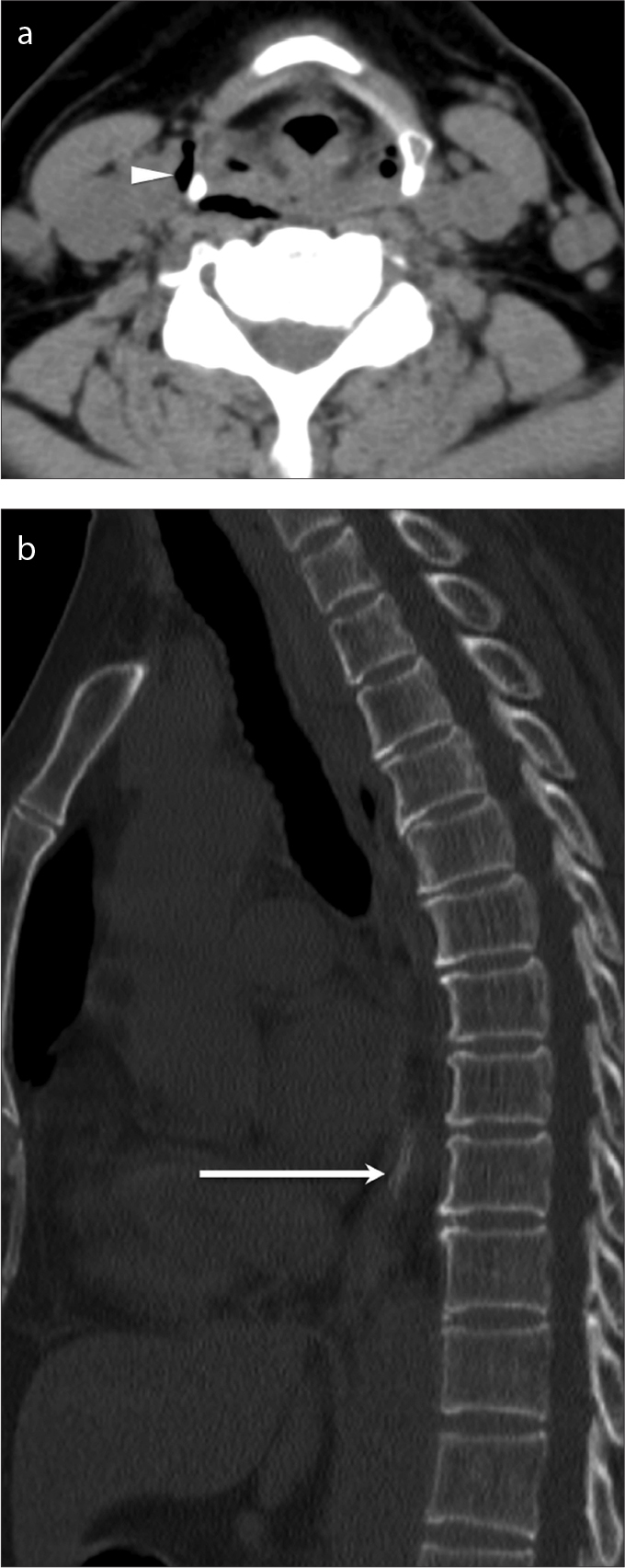
a, b. Ingested fish bone with perforation of the upper esophagus, and air in the deep spaces of the neck. Axial unenhanced CT of the neck (a) and sagittal unenhanced CT of the thorax (b) demonstrate a linear hyperdensity (b, arrow) in the distal esophagus suggestive of an ingested fish bone causing perforation of the upper esophagus resulting in air in the deep spaces of the neck (a, arrowhead). The perforation of upper esophagus was confirmed by esophagoscopy; the fish bone itself had moved into distal esophagus as seen on CT.
Perforations and complications below the level of cricopharyngeus are relatively rare (6, 10). The clinical diagnosis in these cases may be challenging, especially if the clinical history of accidental fish bone ingestion is not forthcoming. Patients may present with nonspecific acute abdomen mimicking relatively common pathologies like acute cholecystitis and peptic ulcer disease. Diagnosis on plain radiography is difficult since the vast majority of fish bones are radiolucent, and the presence of fluid collection and overlapping soft tissues of the abdomen commonly obscure the fish bone (2, 6). In these cases, the ingested fish bone may be detected in any part of the upper gastrointestinal tract, and the definitive diagnosis is established on CT by demonstrating a hyperdense linear foreign body, which is best shown on bone window settings. (11).
In the stomach, because of the natural anatomical angularity of the lesser curvature, perforation is commonly seen at this location. The fish bone may partially perforate the stomach wall, causing perigastric inflammatory changes (Fig. 7) and perigastric abscess. It may sometimes penetrate the entire thickness of stomach wall migrating into the adjacent hepatic parenchyma and cause hepatic abscess (Fig. 8) (12). The perforations of the stomach and duodenum (Fig. 9) are reported to present with prolonged and less severe clinical features than the perforations located in other parts of the bowel (13).
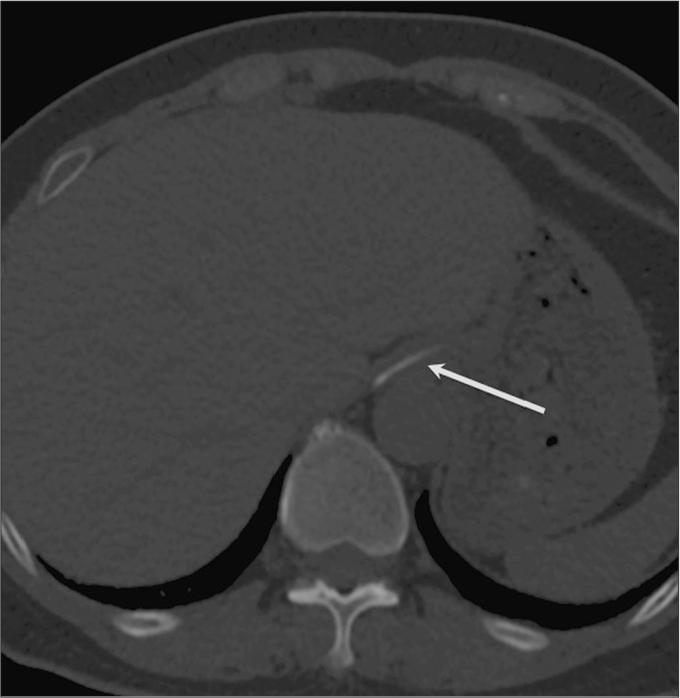
Figure 7.
Ingested fish bone complicated by gastric perforation and perigastric inflammation. Axial contrast-enhanced CT of the abdomen demonstrates a linear fish bone (arrow) with transmural perforation of the posterior wall of the stomach with associated perigastric inflammatory changes.
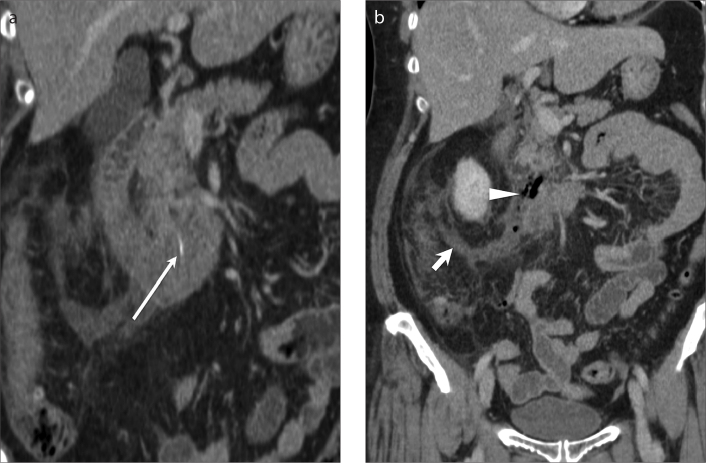
Figure 8.
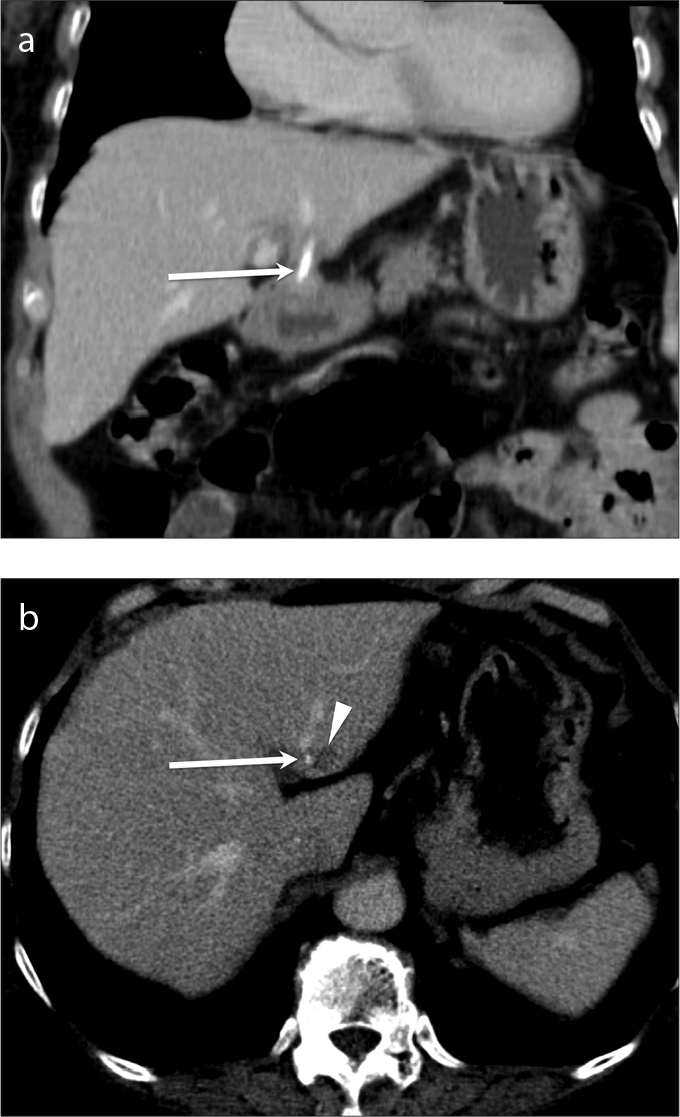
a, b. Ingested fish bone migrating into the liver from perforation of the stomach resulting in a hepatic abscess. Contrast-enhanced coronal (a) and axial (b) CT of the abdomen demonstrates a linear hyperdensity suggestive of ingested fish bone (arrows) within the liver parenchyma with small surrounding hypodensity suggestive of developing abscess (b, arrowhead).
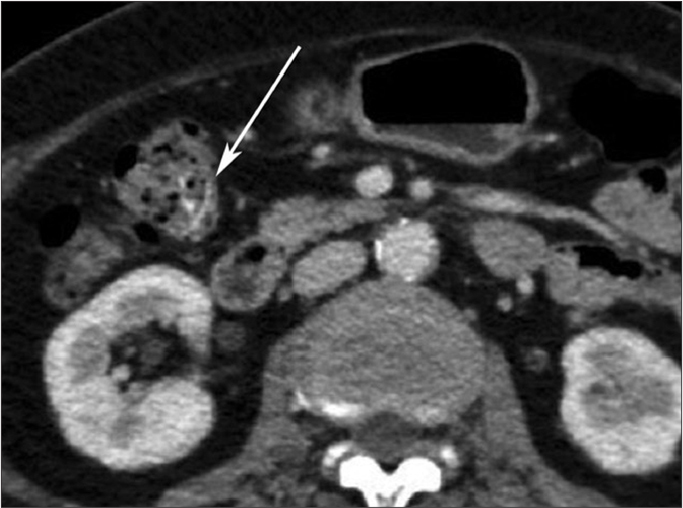
Figure 9.
a, b. Ingested fish bone complicated by duodenal perforation. Coronal contrast-enhanced CT of the abdomen demonstrates a linear hyperdensity in the duodenum suggestive of a fishbone (a, long arrow) with associated wall thickening suggestive of inflammation. There is localized pneumoperitoneum (b, arrowhead) and adjacent extensive inflammatory changes (b, short arrow) from transmural perforation.
In the small bowel, the most common sites of perforation include the less mobile segments of bowel or those with acute angulations such as ileum (11) (Fig. 10). The rectosigmoid junction is the most common site of fish bone impaction in the large bowel. Jejunum is an uncommon site of perforation (Fig. 11). The common findings seen on CT include localized pneumoperitoneum, localized bowel wall thickening, localized mesenteric fat stranding, and abscess formation (Fig. 12). In some cases, the fish bone may be seen remote from the site of bowel perforation, lying free within the peritoneum (Fig. 11). Free pneumoperitoneum is rare as bowel perforation occurs by gradual erosion through the wall, which is spontaneously sealed by fibrin and omentum (3, 11). Occasionally, marked inflammatory narrowing of the involved bowel segment may result in bowel obstruction (Fig. 13).
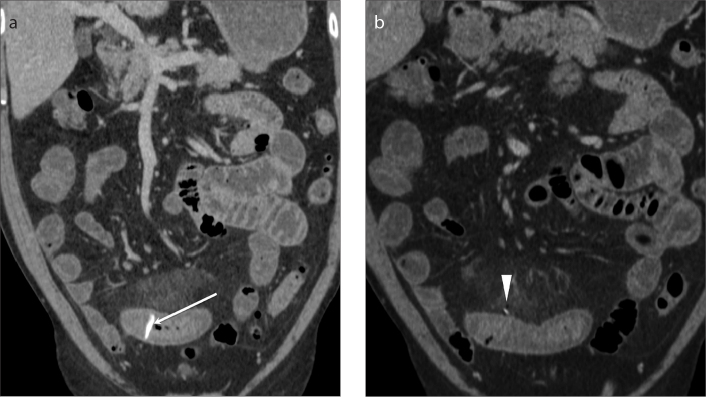
Figure 10.
a, b. Ingested fish bone causing perforation of the ileum. Coronal contrast-enhanced CT of the abdomen demonstrates a linear hyperdensity (a, arrow) indicative of an ingested fish bone causing bowel wall thickening, mesenteric fat stranding, and a small locule of free gas within the peritoneum (b, arrowhead) indicative of a perforated ileum.
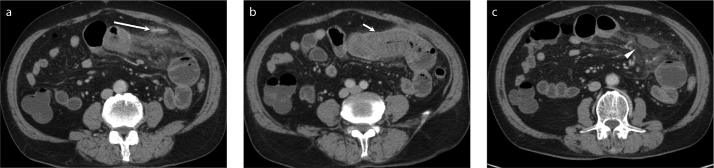
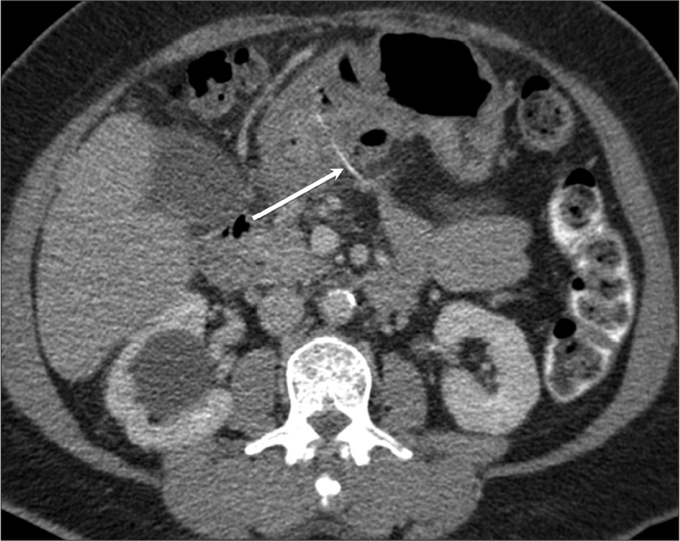
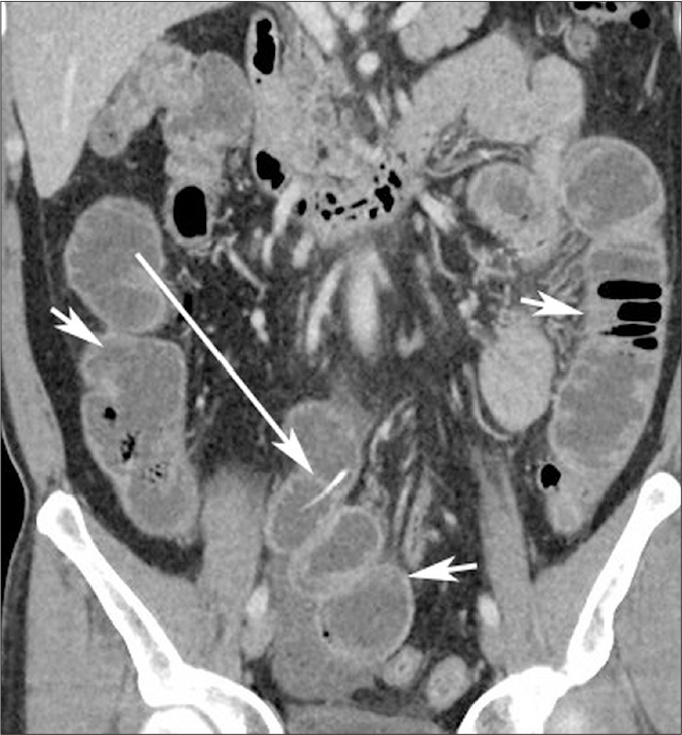
Figure 11.
a–c. Ingested fish bone causing transmural perforation of the jejunum. Axial contrast-enhanced CT of the abdomen demonstrates a fish bone (a, long arrow) lying free within the peritoneum after transmural jejunal perforation. Note the marked thickening of the adjacent jejunal wall and associated stranding of the mesenteric and omental fat (b, short arrow) and small fluid collection (c, arrowhead).
Figure 12.

Fish bone ingestion complicated by perforation of the ascending colon with a complex pericolonic abscess. Coronal contrast-enhanced CT of the abdomen demonstrates a linear hyperdensity indicative of a perforated fish bone (arrow) within the complex pericolonic abscess (arrowheads).
Figure 13.
Ingested fish bone causing small bowel obstruction. Coronal contrast-enhanced CT of the abdomen shows linear hyperdensity embedded within the distal ileum (long arrow) causing high-grade small bowel obstruction (short arrows) with transition at the distal ileum.
Airway
Tracheobronchial foreign body aspiration is rare in adults. Fish bones may be found in the right bronchial tree because anatomically right bronchus is in line with trachea (Fig. 14). They can be asymptomatic or present with cough. Fish bone impaction can also lead to lung collapse and obstructive pneumonia.
Figure 14.
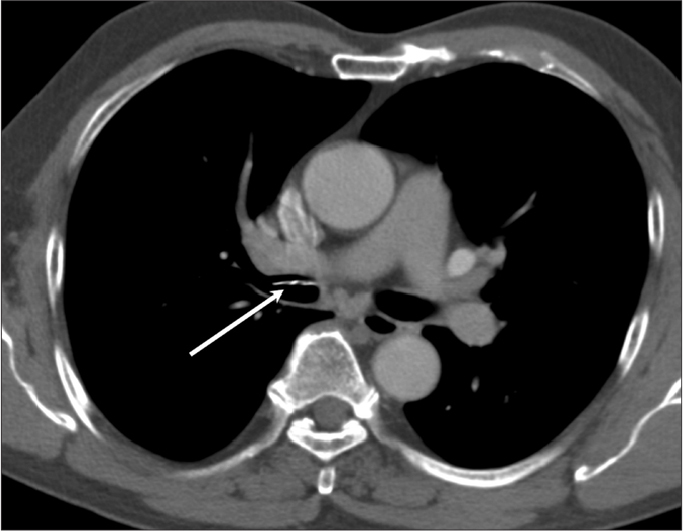
Accidental fish bone aspiration into the large airway. Axial CT of the thorax demonstrates a linear hyperdensity (arrow) consistent with an aspirated fish bone within the lumen of right main bronchus. This was removed via a bronchoscope.
Differential diagnosis
Fish bone perforations can occasionally simulate malignancy (14, 15) and other acute and chronic inflammatory processes. This is commonly due to significant inflammatory thickening or mass-like appearance of the involved structures, lack of background history of fish bone ingestion and unfamiliarity with varied imaging appearance of the fish bones. CT is highly sensitive, and a definitive diagnosis can be established by identification of the fish bone. Careful attention to technical factors like thin slice thickness [1.5–2 mm], presence of negative bowel contrast and evaluation of reformats in multiple planes can aid accurate diagnosis.
Pitfalls
Potential pitfalls on CT include the presence of positive bowel contrast, which can completely obscure or mimic the fish bone (Fig. 15), cricoid cartilage calcification simulating the fish bone (Fig. 3), artifacts related to fecal material within the colon, and contrast opacified small blood vessels, which can mimic the fish bone (3, 6). Clinical history and multiplanar reformat images confirm artifacts from the fish bone.
Figure 15.
Bowel contrast or fecal material mimicking intraluminal fish bone seen on CT performed for other indications. Axial CT demonstrates an intraluminal linear hyperdensity within the colon (arrow), likely representing ingested oral contrast or dense fecal material, which can mimic a fish bone.
Conclusion
Familiarity with various imaging features and relevant clinical history can establish the diagnosis of accidental fish bone ingestion. CT with its multiplanar capability is highly valuable to diagnose and accurately localize the ingested fish bone. In addition, CT can also provide a comprehensive evaluation of the complications of fish bone ingestion including those that may be seen remote from the site of bowel perforation.
Main points.
Fish bone is one of the most common accidentally ingested foreign bodies. It usually presents with nonspecific symptoms.
As the vast majority of fish bones are radiolucent, a negative soft tissue radiograph cannot completely exclude the presence of one.
Perforations and complications below the level of cricopharyngeus are relatively rare. Such patients may present with nonspecific acute abdomen mimicking relatively common pathologies.
CT is a highly sensitive method for detecting fish bones; a definitive diagnosis is established by identification of the fish bone.
Potential pitfalls on CT include the presence of positive bowel contrast, cricoid cartilage calcification, artifacts related to fecal material within the colon and contrast opacified small blood vessels which can mimic a fish bone.
Footnotes
Conflict of interest disclosure
The authors declared no conflicts of interest.
References
- 1.Leong HK, Chan RK. Foreign bodies in the upper digestive tract. Singapore Med J. 1987;28:162–165. [PubMed] [Google Scholar]
- 2.Young CA, Menias CO, Bhalla S, Prasad SR. CT features of esophageal emergencies. Radiographics. 2008;28:1541–1553. doi: 10.1148/rg.286085520. http://dx.doi.org/10.1148/rg.286085520. [DOI] [PubMed] [Google Scholar]
- 3.Goh BK, Tan YM, Lin SE, how PK, Cheah FK, Ooi LL. CT in the preoperative diagnosis of fish bone perforation of the gastrointestinal tract. AJR Am J Roentgenol. 2006;187:710–714. doi: 10.2214/AJR.05.0178. http://dx.doi.org/10.2214/AJR.05.0178. [DOI] [PubMed] [Google Scholar]
- 4.Foo TH. Migratory fish bone in the thyroid gland. Singapore Med J. 1993;34:142–144. [PubMed] [Google Scholar]
- 5.Ngan JH, Fok PJ, Lai EC, Branicki FJ, Wong J. A prospective study on fish bone ingestion. Experience of 358 patients. Ann Surg. 1989;211:459–462. doi: 10.1097/00000658-199004000-00012. http://dx.doi.org/10.1097/00000658-199004000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bathla G, Teo LL, Dhanda S. Pictorial essay. Complications of a swallowed fish bone. Indian J Radiol Imaging. 2011;21:63–68. doi: 10.4103/0971-3026.76061. http://dx.doi.org/10.4103/0971-3026.76061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jemerin EF, Arnoff JS. Foreign body in the thyroid following perforation of oesophagus. Surgery. 1949;25:52–59. [PubMed] [Google Scholar]
- 8.al Muhanna A, Abu Chra KA, Dashti H, Behbehani A, al-Naqeeb N. Thyroid lobectomy for removal of a fish bone. J Laryngol Otol. 1990;104:511–512. doi: 10.1017/s0022215100113039. http://dx.doi.org/10.1017/S0022215100113039. [DOI] [PubMed] [Google Scholar]
- 9.Yang CY. The management of ingested foreign bodies in the upper digestive tract: a retrospective study of 49 cases. Singapore Med J. 1991;32:312–315. [PubMed] [Google Scholar]
- 10.Coulier B, Tancredi MH, Ramboux A. Spiral CT and multidetector-row CT diagnosis of perforation of the small intestine caused by ingested foreign bodies. Eur Radiol. 2004;14:1918–1925. doi: 10.1007/s00330-004-2430-1. http://dx.doi.org/10.1007/s00330-004-2430-1. [DOI] [PubMed] [Google Scholar]
- 11.Zissin R, Osadchy A, Gayer G. Abdominal CT findings in small bowel perforation. Br J Radiol. 2009;82:162–171. doi: 10.1259/bjr/78772574. http://dx.doi.org/10.1259/bjr/78772574. [DOI] [PubMed] [Google Scholar]
- 12.Masunaga S, Abe M, Imura T, Asano M, Minami S, Fujisawa I. Hepatic abscess secondary to a fishbone penetrating the gastric wall-CT demonstration. Comput Med Imaging Graph. 1991;15:113–116. doi: 10.1016/0895-6111(91)90034-s. http://dx.doi.org/10.1016/0895-6111(91)90034-S. [DOI] [PubMed] [Google Scholar]
- 13.Goh BKP, Chow PKH, Quah HM, et al. Perforation of the gastrointestinal tract secondary to ingestion of foreign bodies. World J Surg. 2006;30:372–377. doi: 10.1007/s00268-005-0490-2. http://dx.doi.org/10.1007/s00268-005-0490-2. [DOI] [PubMed] [Google Scholar]
- 14.Bajwa A, Seth H, Hughes F. Ingested fishbone mimicking a gastric submucosal tumour. Grand Rounds. 2007;7:42–44. [Google Scholar]
- 15.Kim HJ, Lee BJ, Kim SJ, Shim WY, Baik SK, Sunwoo M. Tongue abscess mimicking neoplasia. AJNR Am J Neuroradiol. 2006;27:2202–2203. [PMC free article] [PubMed] [Google Scholar]