To the Editor
In the United States, reducing new HIV infections will require a determined focus on primary HIV prevention among young Black men who have sex with men (YBMSM) who represent the only group in the United States where HIV incidence has increased over the past decade.1 Through 2011, effective clinic-based HIV prevention interventions that target YBMSM have been virtually non-existent.2 In 2012, Pre-exposure prophylaxis (PrEP), consisting of daily oral tenofovir disoproxil fumarate and emtricitabine was approved by the FDA. With an estimated efficacy of over 90% in persons adherent to treatment,3 PrEP has HIV prevention impact potential for several domestic HIV epicenters.4
Methods
The South Side of Chicago represents the largest contiguous Black community in the US. Despite its many assets, this community is burdened a high HIV prevalence. uConnect is a population-based cohort study of YBMSM that examines how sociodemographic, health, behavioral and social factors drive new HIV prevention including PrEP.
Using Respondent Driven Sampling (RDS), a sample of 622 eligible YBMSM were recruited between June 2013 and July 2014. Study participants were eligible to be interviewed if they: 1) self-identified as African American or Black, 2) were born male, 3) were between 16 and 29 years of age; and 4) reported oral or anal sex with a male within the past 24 months. The sample was weighted using general probability estimates5 using the RDS package in R6. We examined the relationship of a set of sociodemographic, healthcare engagement, behavioral, and social characteristics with PrEP awareness and uptake.
Results
A final analytic sample of eligible participants (n=622) was generated through RDS chains of up to 13 waves in length and with a median of 2 recruits per participant. The mean age of the sample was 22.7 years (standard deviation 3.2 years). Approximately 39% had high-school/GED as terminal education, 79.3% reported an income of less than $20,000 per year. Nearly half (48%) of HIV-negative (PrEP-eligible) individuals reported having some health coverage (either government or private).
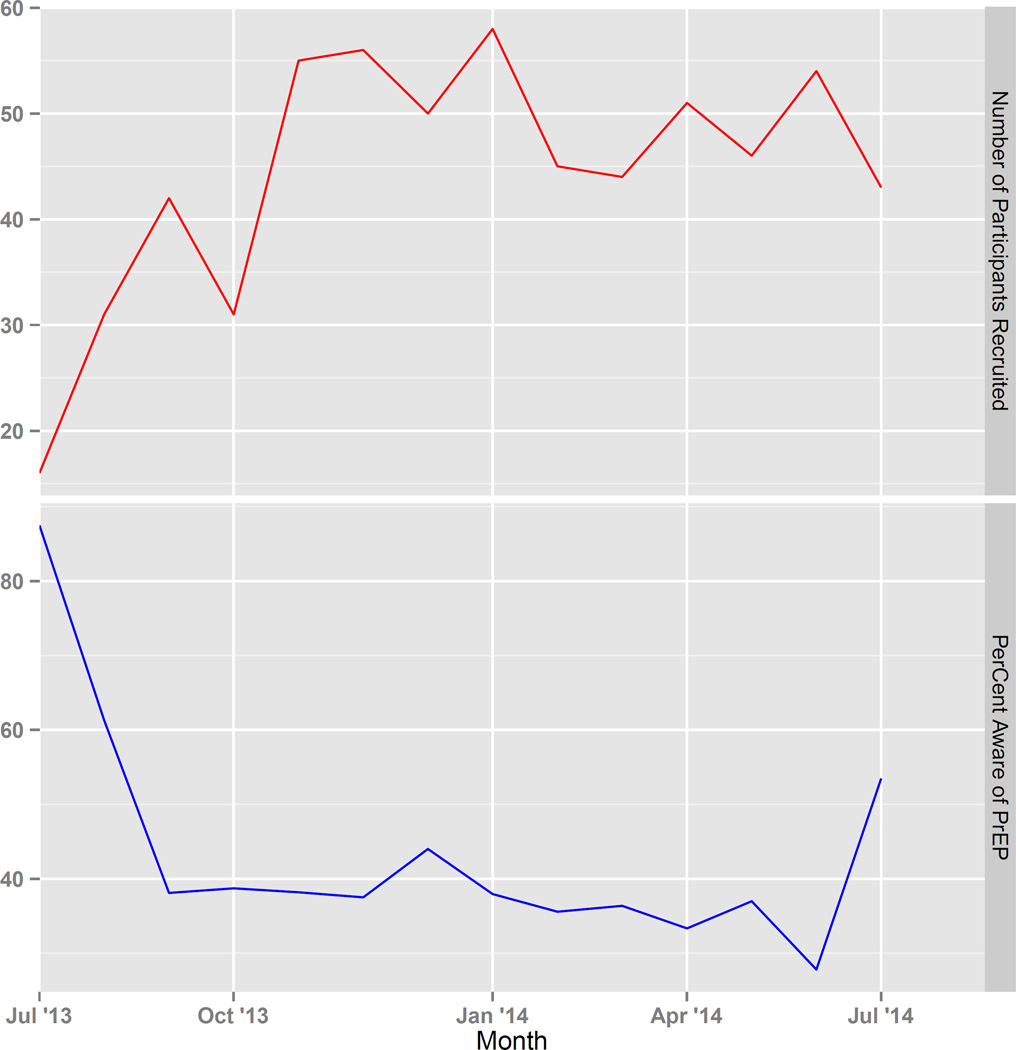
PrEP awareness was low at 40.5% which remained relatively stable over the recruitment period (Figure 1); and 12.1% knew others who had used PrEP. Approximately 72.1% of the sample was HIV-uninfected, 3.6% of whom had ever used PrEP. Having a primary care provider, participation in an HIV prevention program or research study, having had an anorectal STI test, and membership in the House/Ball community were significantly associated with PrEP awareness (Table 1). Additionally, among PrEP-eligible participants, meeting with an HIV outreach worker (<12 months) was also significantly associated with PrEP awareness (aOR 2.02; 95% CI: [1.29, 3.16]).
Figure 1.
Study respondent flow and PrEP awareness by month, UConnect, 2013–2014.
Table 1.
Multivariable Logistic Regression of factors associated with PrEP awareness (n=622), uConnect Study, Chicago, 2014.1
| N (%) | Adjusted Odds Ratio |
p-value | |
|---|---|---|---|
| Clinical | |||
| Has Primary Health Care Provider | |||
| No | 274 (44) | Ref. | |
| Yes | 342 (55) | 1.62 (1.17–2.53) | 0.04* |
| Depressed2 | |||
| No | 553 (88) | Ref. | |
| Yes | 69 (11) | 0.92 (0.49–1.71) | 0.78 |
| Conversation with HIV Outreach worker in past year | |||
| No | 331 (53) | Ref. | |
| Yes | 277 (45) | 1.39 (0.93–2.08) | 0.12 |
| Syphilis seropositive | |||
| No | 302 (49) | Ref. | |
| Yes | 143 (23) | 1.68 (0.91–3.10) | 0.10 |
| Ever participated in an HIV prevention program or research study | |||
| No | 446 (72) | Ref. | |
| Yes | 172 (28) | 3.93 (2.04–7.56) | <0.001* |
| Anorectal STI test (ever) | |||
| No | 458 (74) | Ref. | |
| Yes | 158 (25) | 1.85 (1.0–2.85) | 0.01* |
| Behavioral | |||
| Have a primary sex partner | |||
| No | 340 (55) | Ref. | |
| Yes | 259 (42) | 1.03 (0.69–1.36) | 0.87 |
| Group sex in past year | |||
| No | 488 (78) | Ref. | |
| Yes | 128 (20) | 1.54 (0.74–1.44) | 0.12 |
| One or more partners of HIV+ or unknown status | |||
| No | 349 (56) | Ref. | |
| Yes | 255 (41) | 1.41 (0.81–0.46) | 0.23 |
| Sex-drug use in past year | |||
| No | 432 (69) | Ref. | |
| Yes | 149 (24) | 1.33 (0.76–2.32) | 0.32 |
| Social | |||
| Close to gay community | |||
| Not close at all | 78 (13) | Ref. | |
| Not very/ somewhat close | 404 (65) | 0.71 (0.39–1.32) | 0.29 |
| Very Close | 140 (23) | 1.09 (0.55–2.20) | 0.81 |
| House Ball or gay family membership | |||
| Neither | 415 (67) | Ref. | |
| Ballroom | 95 (15) | 2.68 (1.63–4.42) | <0.001* |
| Gay family only | 112 (18) | 1.43 (0.86–2.38) | 0.18 |
Bivariate models were used to select variables for the final multivariate model (alpha-level = 0.05). Common confounders such as age, education, and employment status were adjusted for. Missing values for independent variables were imputed using the median for that variable, to avoid the biases associated with a complete-case analysis.
Brief Symptom Inventory (BSI)-18 to assess depression of respondent as a dichotomous variable.
Comment
uConnect is the first examination of relevant drivers of PrEP engagement from a population-based sample of YBMSM. Low PrEP awareness and uptake among YBMSM parallels earlier HIV treatment disparities. While PrEP is promising, this population-based cohort study illustrates that real-world PrEP utilization by those with highest HIV incidence, faces major implementation challenges that require purposeful and sustained engagement with Black communities and their healthcare providers. We find that PrEP awareness is associated with a diverse range of clinical engagement activities among YBMSM. The Affordable Care Act (ACA) represents one potential opportunity to increase such clinical engagement; however, ACA benefits are not realized in all US regions and in our cohort, only half had any type of health care coverage. Ongoing work should include scientific assessment of strategies to mobilize networks of YBMSM around PrEP as part of a comprehensive health care program. Concomitantly, efforts to mitigate the structural barriers that prevent PrEP uptake among YBMSM may greatly improve the public health impact potential of this promising HIV prevention intervention.
Acknowledgments
This study was supported by NIH grant R01 DA 083775. The funding organization had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. We also acknowledge computing support from University of Chicago’s Research Computing Center, the UConnect Community Advisory Board, and study participants for their time, effort and dedication. We gratefully acknowledge the contributions of Dexter Voisin, School of Social Service Administration, University of Chicago, and Kenneth Mayer, Fenway Institute.
References
- 1.Prejean J, Song R, Hernandez A, et al. Estimated HIV incidence in the United States, 2006–2009. PLoS One. 2011;6 doi: 10.1371/journal.pone.0017502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hemmige V, McFadden R, Cook S, Tang H, Schneider JA. HIV prevention interventions to reduce racial disparities in the United States: A systematic review. J Gen Intern Med. 2012;27:1047–1067. doi: 10.1007/s11606-012-2036-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Anderson PL, Glidden DV, Liu A, et al. Emtricitabine-Tenofovir Concentrations and Pre-Exposure Prophylaxis Efficacy in Men Who Have Sex with Men. Sci Transl Med. 2012;4:151ra125–ra151ra125. doi: 10.1126/scitranslmed.3004006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Office of National AIDS Policy. National HIV/AIDS Strategy for the United States: Updated to 2020. Washington: https://aids.gov/federal-resources/national-hiv-aids-strategy/nhas-update.pdf. [Google Scholar]
- 5.Gile KJ. Improved Inference for Respondent-Driven Sampling Data With Application to HIV Prevalence Estimation. J Am Stat Assoc. 2011;106(493):135–146. [Google Scholar]
- 6.Handcock MS, Gile KJ, Fellows IE, Neely WW. RDS: Respondent-Driven Sampling. 2015 [Google Scholar]