Abstract
In some societies, medical pluralism has been demonstrated to delay access to care. We identified sources of health care, and explored utilization patterns and triggers of care-seeking behavior among HIV/AIDS patients in rural South Africa. A longitudinal qualitative study consisting of in-depth interviews was conducted. We purposively sampled thirty-two adult HIV clinic attendees. A high degree of medical pluralism occurred among participants before initiation of antiretroviral treatment (ART). After ART initiation, participants predominantly used the HIV/ART clinic, and utilization of private and traditional facilities decreased. Patterns included both concurrent and sequential pathways to public, private and traditional health sectors. HIV diagnosis and treatment were delayed despite early contact with health systems. Therefore, use of multiple health care modalities before ART initiation can lead to delayed HIV testing and ART initiation. Integrated-care has the potential to mitigate the impact of medical pluralism on access to HIV-related services over the longer term.
Keywords: HIV, Medical pluralism, Health system, Antiretroviral treatment, South Africa
Introduction
HIV remains a public health challenge in much of Sub-Saharan Africa [1]. South Africa has the highest number of HIV infections in the world, with over 10% of the population living with HIV [1–3]. HIV-related mortality remains high with an estimated 1,000 people dying each day [1, 3, 4]. However, as a result of recent policy shifts to support widespread treatment access, mirrored by increased support from both government and external donors [5], HIV has become a chronic manageable condition [3, 6]. There have been increases in uptake of HIV testing in the general population [2], access to prevention and management of opportunistic infections, psychosocial support made available, and more patients are initiating antiretroviral treatment [5, 7]. Despite these encouraging signs of progress, only one-third of those in need of antiretroviral treatment (ART) are currently receiving it in South Africa [1, 3].
There are a number of obstacles to accessing effective HIV care and support services. The health system in post-apartheid South Africa is fragmented and inequitable, comprised of an under-resourced hierarchical public sector, expensive private specialist care that caters to the well-insured, and an ambulatory private primary care sector which has emerged in remote areas [8]. For the rural poor with limited options, the public sector remains the mainstay of basic health care [9]. Other well-documented barriers to treatment access include poor supply chain management, high opportunity costs for patients, long distances to district hospitals which remain the main source of HIV care, persistent stigma associated with care, and traditional health beliefs that place access to modern medicine as just one choice alongside a host of competing alternatives [10–14]. Traditional practitioners operate largely outside of the formal systems. While their fee-for-service approach can be expensive, they nonetheless remain a frequent source of care for patients in rural areas [15].
The array of competing options has the potential to result in medical pluralism, which refers to the diverse ways in which illness can be perceived, understood and treated [16–18]. Switching or ‘shopping’ of health providers is a well-known and complex phenomenon, which has the potential to delay access to essential care and support services [19–22]. Mixed messages from an array of providers may result in conflicting influence and mistrust in the health care delivery systems [22]. Despite the potential for pluralism to affect treatment outcomes, its interaction with HIV/AIDS remains poorly understood, particularly in relation to the pre-and post treatment initiation periods.
Understanding patterns of medical pluralism among people infected with HIV may serve to increase access and utilization of appropriate health care. There are two main approaches to conceptualizing health-seeking behavior— one that focuses on determinants, and another on pathways of care [23, 24]. In this study, we sought to describe the latter amongst rural HIV-infected people in South Africa. Our primary aim was to capture the complex nature of care pathways inherent in utilization of HIV-related health care [25, 26]. The objectives were to identify sources of healthcare before and after initiation of ART, explore patterns of healthcare use and triggers of care-seeking behavior. Using qualitative research methods, we tracked patients retrospectively from the onset of their HIV-related illness throughout their journeys of illness experience. For this we used ‘pathways of care analyses’— a methodology previously used for other medical conditions in Africa such as malaria [20] and psychiatric illness [27]. We are not aware of any study that examines pathways of care amongst HIV-infected patients.
Methods
Study Design and Sampling Procedures
A longitudinal qualitative study was conducted using in-depth interviews. Purposive sampling methods were used to recruit 32 adult HIV positive participants. The study sample was selected from a population of HIV-infected individuals attending support groups at a rural HIV clinic of a remote hospital in Bushbuckridge, Mpumalanga Province, South Africa. Bushbuckridge is a densely settled sub-district situated in South Africa’s rural northeast. This previous apartheid-delineated ‘homeland’ area has 523,000 inhabitants with unemployment rates of up to 80%. More than 52% of households live on less than USD100 per month [28].
Antenatal HIV prevalence in the Bushbuckridge area is 34%, much higher than the national average of 28% [29]. Bushbuckridge is served by three hospitals, two health centers and 37 primary health care clinics. Currently, over 7,000 patients have been placed on ART by 2 accredited hospitals. However, an estimated 20,000 patients require ART under national guidelines which call for ART initiation once CD4 cell counts fall below 200 µl−1. With coverage rates of only 30%, HIV-related mortality remains high. Therefore, increasing access to therapy is a major health concern and a high priority issue among authorities in this area.
Our participant selection specifically aimed to include a diverse group of HIV-infected individuals in order to capture a wide range of perspectives. Criteria included a representative mix of gender and age, ART-initiated and non-initiated, patients with clinical evidence of treatment failure, and those who were likely to provide information-rich interviews.
Data Collection Procedures and Ethical Considerations
For a month prior to data collection, a qualitative researcher and a trained assistant observed daily HIV support groups to identify potential participants. Verbal informed consent for the research team to attend support groups was obtained prior to each session. Selected participants were invited to attend an interview session in a secluded area. Written informed consent was obtained from each respondent, and it was emphasized that refusal to participate at any stage would not affect services they received. Interviews were conducted, with the aid of an interpreter, in the preferred language of the participant. Follow-up interviews were conducted once per month to capture the continuum of the HIV illness experience. At follow up, missing information was completed, new information was obtained, and member-checking or respondent validation [30] was done to increase reliability and validity. Data collection took place over 10 months from June 2006 to March 2007. On average, four interviews were conducted per participant. The number of interviews ranged from three to seven when loss to follow up (1/32) and death (1/32) were excluded. The duration of interviews ranged from 20 min to 2 h. Interviews were conducted in private within the premises of the hospital. Alternate meeting times and locations were arranged based on participant preferences, while still ensuring participant anonymity and confidentiality. Interviews explored patterns of access to public, private, non-formal and household level care and support services in the period leading up to diagnosis and subsequent to initiation of antiretroviral therapy (ART).
Notes were collected by both the interviewer and the interpreter. Field notes were combined, compiled and checked at the end of the interview session. Audio-recording was not utilized, because the majority of patients chose not to be voice-recorded at initial recruitment. Ethical approval was obtained from the Human Research Ethics Committee at the University of Witwatersrand and from the Institutional Review Board at Brown University.
Data Reduction and Analysis
Text files were imported into and managed using NUD*IST (N6). Analysis was conducted in two stages. Thematic content analysis was used throughout data collection to achieve familiarization and allow validation by respondents during follow-up interviews. Additionally, we conducted a pathway of care analysis for each participant by tracking their experiences of illness and health care service utilization [23, 24]. We summarized the illness experience of individual participants from their onset of AIDS-related symptoms to the day of their final interview. Pseudonyms were used in all case summaries. The term ‘onset’ of AIDS-related symptoms refers to a symptomatic point at which participants recognized and acknowledged the need to receive health care. The timing of AIDS-related symptoms onset was identified irrespective of actual HIV diagnosis or health care use. Two other crucial stages identified during data reduction were HIV testing and ART initiation. Date estimates for these major events were provided by participants. We calculated time differences between illness onset and initial use of health care in any sector- formal or informal. Any delay in using health care beyond 1 month of illness was considered important in this study as previously used in other chronic illness studies [10]. Whilst there was little emphasis on self-medication at the time of initial symptoms, deliberate self-medication was taken into account once initial use of health care was achieved. We assumed that definitive care for these participants included HIV diagnosis and eventually ART initiation in addition to treatment of symptoms and opportunistic illnesses, hence the emphasis placed on health care service use rather than self-medication at the time of initial access to health care. Furthermore, where patients received medication from other service providers to take at home, this was not regarded as self-medication. Instead, the particular provider was captured on the pathway of care. We further assumed that HIV testing should have been offered at the time of presentation for initial care. Therefore, any delay in testing beyond initial use of health care was considered important regardless of the type of health service provider visited. When the need for ART use was identified, any delay beyond 3 months was considered significant. In relation to these three major events, we investigated potential triggers of access based on the emphasis placed by the participant. Furthermore, we documented events that occurred in between these events.
Using participants’ pathways of care, the various sources of health care within the broader health system were mapped out for each of the 32 participants, and were later categorized by health sector type. With respect to patterns of initial use of health care and assuming a step-wise approach, we ordered service providers according to particular levels of care. These levels of care were dependant on which provider was seen first by the participant. Notably, the flow patterns identified here were only followed for the first three levels of care occurring in the period prior to ART initiation, but all the service points beyond the third level of care were recorded in the study. Transitions made between the first three levels of care were identified. We tracked transitions between sectors, between facilities within sectors and between providers within facilities or sectors where applicable. Furthermore, we classified participants according to the sectors visited, and identified any exclusive or combined patterns before and after initiation of ART. These were termed degrees of pluralism. We also investigated whether these providers were used sequentially or concurrently, referred here as types of pluralism. These types of pluralism were classified according to behavior and were not necessarily time-bound. An emphasis was placed on participant’s decision to stay with, leave or combine providers rather than the number of consultation with a provider or intervals between providers. As a result, some types were difficult to discern, whereby participants moved back and forth in shorter intervals— random, and others dropped out of care before returning into care at a later stage—inconsistent. However, dominant patterns were chosen in such challenging cases based on participants’ accounts.
Results
Characteristics of Participants
The total sample size of 32 participants was made up of 20 (63%) females and 12 (37%) males. Age ranged from 25 to 57 years (mean 40 years), 34% of participants were married, 25% divorced, and 9% separated from their spouses. 16% were single and 16% widowed. Most participants had received some secondary education (61%), with 32% having completed only primary education. 7% reported no schooling, and none had completed any tertiary education. About three-quarters of the participants were unemployed (72%). On their first interview, 24 participants (75%) had already initiated ART. In addition, 5 participants (16%) transitioned onto ART during the course of the study and 3 (9%) were never placed on ART during the study.
Sources of Health Care for HIV-Infected Rural People
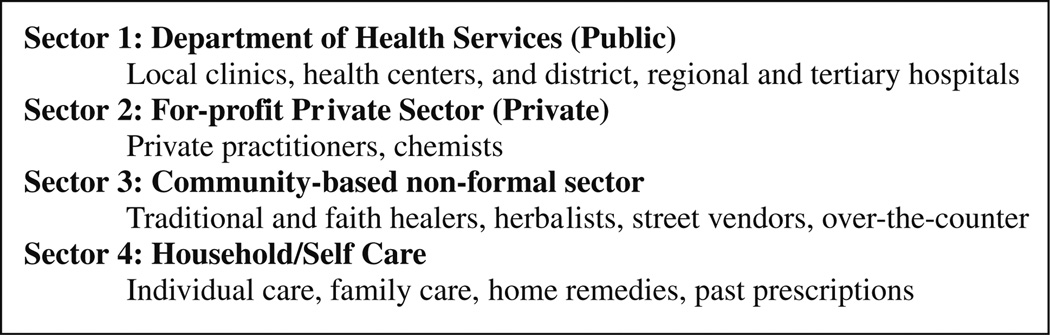
The health care system in this area was found to consist of four sectors, within which several sources of health care were identified (Fig. 1). The most frequently utilized was the public sector. The second source of health care was the for-profit private sector. Third was the community-based non-formal sector. The fourth sector was the household or self-care sector, where health care was provided by the individuals themselves, family, neighbors and friends.
Fig. 1.
Identified sources of healthcare grouped per sector
The First Level of Contact with the Health System for Rural HIV-Infected Patients
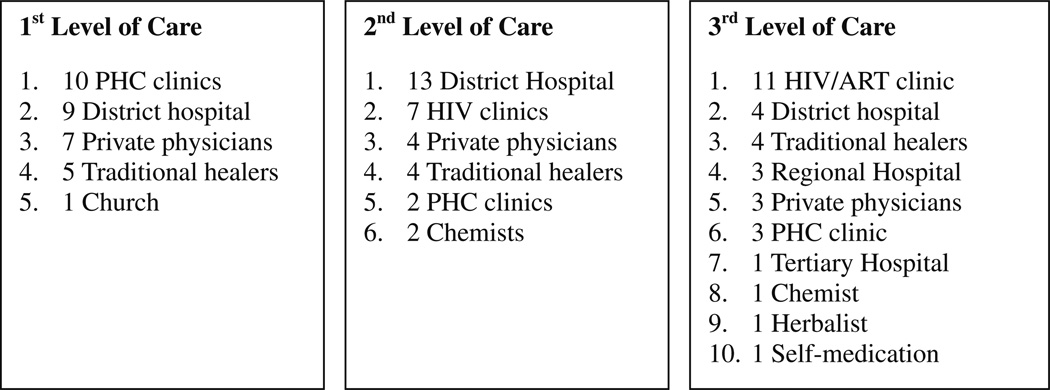
On average, ten different service points were used among the participants. Patterns of healthcare use varied widely between participants, and showed a wide range of routes to HIV testing and ART access. Figure 2 presents the levels of care in a hierarchical order aggregated for all participants. As noted, the principal first level of care prior to HIV diagnosis was the primary health care service (10/32), followed very closely by the district hospital (9/32). Some participants visited private physicians first (7/32), while others first sought care from traditional healers (5/32), and one visited the church as a primary source of healthcare.
Fig. 2.
Aggregated levels of care with escalating utilization based on choice and referral
As participants enter their second and third levels of care over time, their options showed a broadening, but more defined pattern. The district (level 1) hospital was a common second level of care (13/32), while the HIV/ART clinic was used more often as the third level of care. Higher levels of care were predominant in the third level of care, as evidenced by the increased use of regional and tertiary hospitals. In the period prior to ART initiation and using aggregated numbers in Fig. 2, the use of primary health care clinics and private physicians decreased over time. However, use of traditional healers remained steady, and public sector hospital use increased.
Switching of Health Care Sectors, Facilities and Providers Following Initial Use
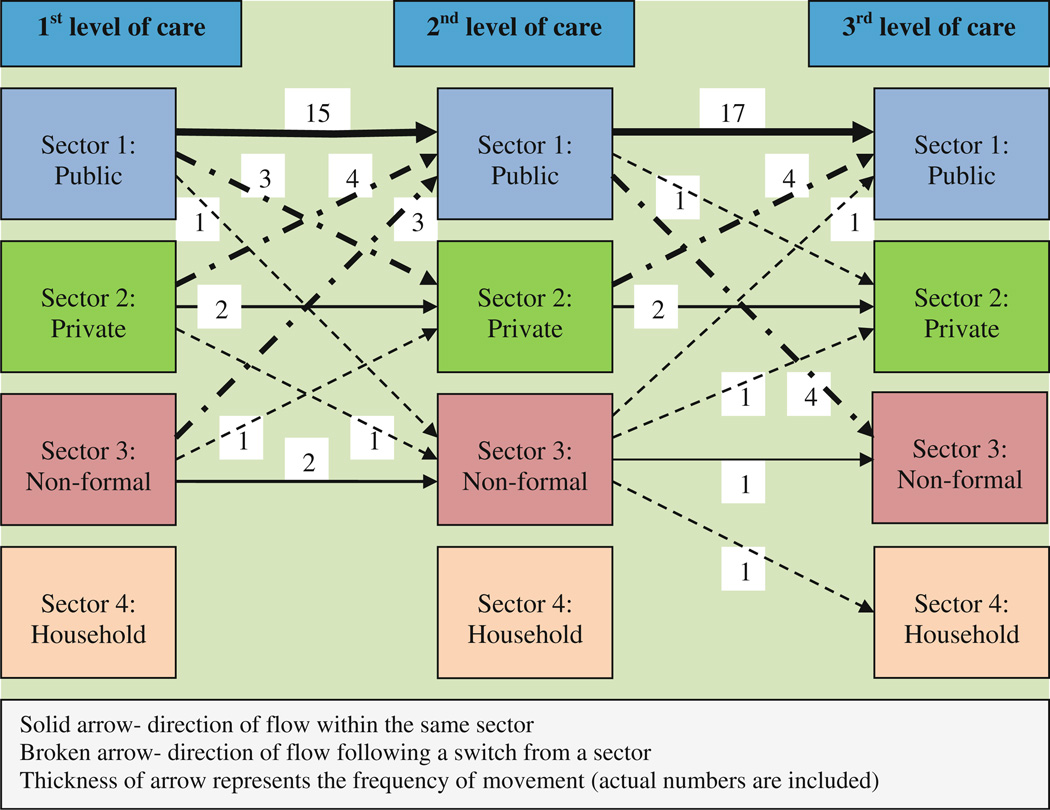
When transitioning from the first to second level of care (Fig. 3), the majority of participants returned to the same sector they initially visited (19/32). Some participants returned to the same facility (6/32), but used a different service point within the facility, typically the more specialized HIV services. Among participants who changed facilities within the public sector, the majority transitioned appropriately through the referral system from the primary health care clinic to the district hospital (9/32). Others switched practitioners within the private (2/32) and non-formal (2/32) sectors. Switches between sectors were also observed. The most common of which involved moving from the private to the public sector (4/32), non-formal to the public sector (3/32), or public to the private sector (3/32). Others were changes from public to non-formal (1/32), private to non-formal (1/32), and non-formal to private (1/32) sectors. Overall, most switching participants transitioned into the public sector.
Fig. 3.
Switching health care sources between levels of care
Transitions between the second and third points of care were also tracked, whereby participants appeared to chiefly return to the same sector (20/32). An even higher proportion of participants remained within the same facility (11/ 32), and 3 of them returned to the same service point, the HIV clinic. Although certain participants returned to the same hospital facility, they used the HIV service point rather than the out-patient department (9/32). Some returned to the same sector, but altered service providers (9/32). Within the public sector, the flow of participants through the system was representative of the available health system infrastructure. While one participant self-referred from a district hospital to a primary health care clinic, others transitioned from the primary health care clinic to the district (level 1) hospital (1/32), and district to regional (level 2) (3/32) and tertiary hospital (level 3) (1/32). The private sector retained (2/32) participants, whereas (1/32) remained in the non-formal sector.
Between the second and third points of care, a switch from one sector to another largely involved participants changing from the public sector into the community-based non-formal sector (4/32). However, 3 participants left the non-formal sector to enter the public (1/32), private (1/32), and household (1/32) sectors. Also, some (4/32) moved from the private (chemists 2/32 and private physicians 2/32) into the public sector, while 1 participant went the opposite direction.
Patterns of Pluralism for Each Individual Pre and Post ART Initiation
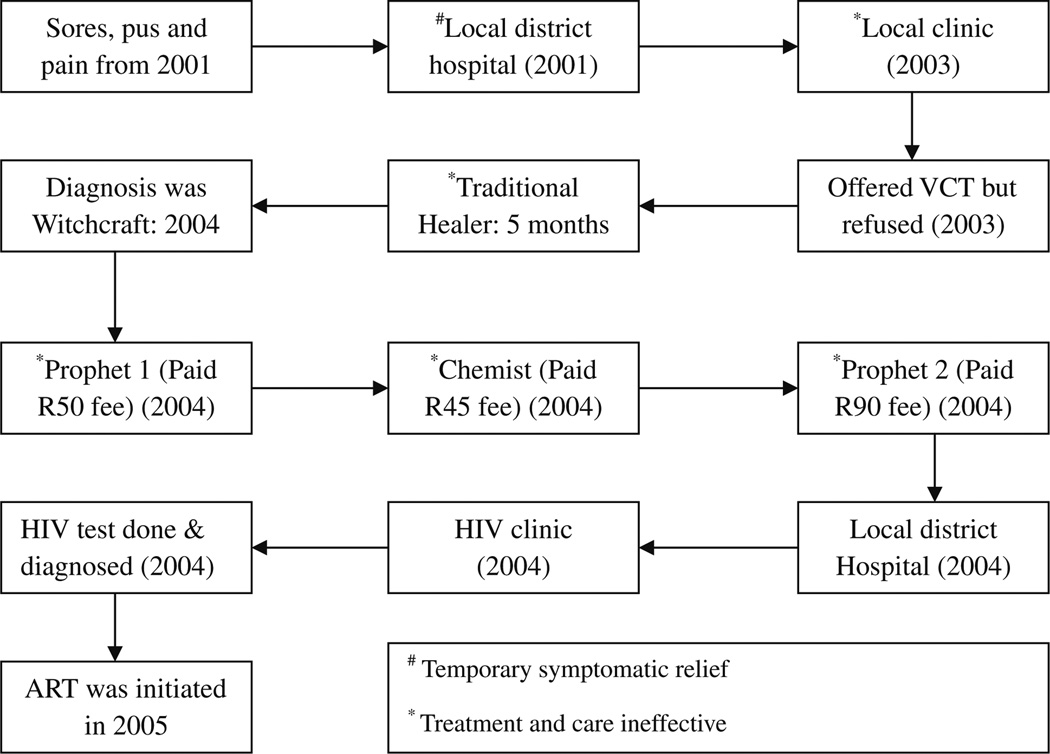
Once ART was initiated, participants used predominantly the HIV/ART clinic for all their health needs (30/32). Some participants occasionally sought healthcare from their local clinics while on ART, but very rarely. Pluralistic patterns of varying degrees were shown for the majority of participants (22/32) within the period prior to ART initiation (Fig. 4). Three groupings were identified. The first degree of medical pluralism involved use of multiple service providers within the Department of Health Services and Self-care (1/32). The second degree included those participants who utilized private physicians and chemists in addition to Department of Health Services (9/32). Lastly, the third degree of medical pluralism captured all the participants who additionally sourced help from the non-formal sector during the course of their illness (12/22). However, post-ART initiation patterns showed very little medical pluralism (2/32), and it was the third degree of medical pluralism noted at this stage.
Fig. 4.
Mabuti’s pathway to HIV care: Pluralism in a male participant aged 47 years
Two types of pluralism were predominant among those showing variations in the sources of health care for their illnesses (22/32). Eleven participants showed a sequential pattern of use, whereby participants visited different service providers in succession without returning to the previous one. For 11 other participants, concurrency was identified among those who tended to see different providers over the same period of time. However, due to the chronic nature of the participants’ illness experiences, some utilization patterns were difficult to categorize. For some participants, the patterns of utilization could not be characterized as concurrent or sequential, and rather appeared inconsistent or random. Inconsistent users dropped out of care systems temporarily, while random users switched erratically between sectors and service providers. In certain cases, both sequential and concurrent patterns were seen at different points over time. In these cases, participants were categorized based on their most dominant pattern exhibited.
Delays in Reaching Definitive HIV Testing and ART Care
The delay in the use of health care emerged as a crucial factor in the pathways of care (Table 1). In the absence of medical pluralism, exclusive use of the public sector resulted in early access to HIV testing services (70%). However, when the public sector was combined with traditional healers concurrently or sequentially, delayed utilization of HIV testing services resulted (86%). Among those who used private physicians and chemists, combined with the public sector in sequential and concurrent patterns, surprising levels of delayed HIV testing (78%) were observed.
Table 1.
Summary of medical pluralism types and degrees, triggers for care-seeking and milestones of care emphasizing delays
| Medical pluralism type (n) |
Pluralism degree (n) |
Delay in seeking healthcare after initial sickness in months (n) |
Trigger for seeking initial care |
Delay in HIV diagnosis in months (n) |
Trigger for HIV testing |
Delay in ART initiation from diagnosis in months (n) |
|---|---|---|---|---|---|---|
| Sequential (11) | None (10) 1 st degree (1) |
None (19) Delayed: |
Illness Radio |
None (9) Delayed: |
Health talk HIV education |
None (17) Delayed: |
| Concurrent (11) | 2nd degree (9) | 1–3 (2) | Neighbor | 0–3 (1) | Employer | 3–6 (3) |
| Non-pluralism (10) | 3rd degree (12) | 3–6(4) 6–12 (1) 12–24 (2) >24 (1) Range 2–24 Median 4 Mean 7 |
Pregnancy Advice |
3–6(1) 6–12 (5) 12–24 (4) >24 (12) Range 2–72 Median 24 Mean 25 |
Nurse referral Sick child (TB) Co-morbidity (TB) Doctor referral Husband referral Neighbor Radio Pregnancy (PMTCT) Warning by ex- partner Family advice Rape |
6–12 (2) 12–24 (6) >24 (4) Range 4–48 Median 12 Mean 15 |
| Pre-ART pluralism | 1st: public 2nd : 1st + private 3rd: 2nd + informal |
Delay (>1 month of illness onset) |
Illness most common (29/32) | Any delay beyond 1st contact with the health system |
Husband referred wife for HIV testing |
Delay >3 months since HIV testing when indicated |
Data must be read in columns only, and not in rows
For most participants (29/32), initial contact with the health system was triggered by symptoms. Among symptomatic participants (29/32), one-third delayed health-seeking at least 1 month from the onset of symptoms to initial consultation with any health provider, while two-thirds sought some form of health care within a month. Pregnancy emerged as a reason to use health services through which care could be received for other illnesses (1/32). For two participants, the initial consultation was prompted by advice, one from an ex-husband, and the other from a neighbor together with information heard over the radio.
Approximately 2 months after Phumzile separated from her husband; he rang and told her she was going to die, because she had AIDS. She was hurt and afraid that she was indeed going to die. Five months later, she opted for an HIV test at her local hospital. She waited that long because she was fearful. When she learned her HIV status, she felt stressed and confused. She asked, “How long do I have to live?”
Transitioning from a state of well-being to ill-health was a significant event in the lives of most HIV-infected patients. Also, diagnosis of HIV and initiation of antiretroviral treatment appeared to represent crucial milestones in the illness experience. When initial contact with the health system was used as a starting point, the majority of the participants (23/29) were found to have experienced delayed HIV-testing. The delay ranged from 2 months to 6 years, with a median and mean of 24 and 25 months, respectively. In more than half of those who experienced late HIV testing, participants showed delays of more than 2 years. HIV-testing by participants was triggered by several factors, most notably co-morbidity, medical referral, pregnancy and family advice (Table 1). Fifteen participants showed patterns suggestive of delayed ART initiation for a minimum period of 3 months. Among those who needed ART, two-thirds experienced delayed initiation for over 1 year. As depicted in Fig. 4, it took Mabuti a total of 4 years to move from the point of symptom onset to ART initiation. Furthermore, he had been visiting health providers during this period and paying for services despite his lack of income. Relief of symptoms and effectiveness of treatment appeared to influence choice of his next level of care. He refused an HIV test at a primary health care clinic, but was not offered a test or encouraged to test for HIV by his other health providers.
Discussion
HIV/AIDS patients in this study identified multiple sources of health care, indicating a wide-range of options for health care services. These options include public and private sector health services, but also community and household ‘lay’ services. Previous studies have already established these patterns of medical pluralism in developing countries, but this is the first study to examine medical pluralism amongst HIV/AIDS patients in care and on treatment in South Africa. Of note, the patterns of health system utilization differ depending on whether patients have initiated ART or not, with high levels of medical pluralism in the period prior to ART initiation. Before ART initiation, establishing a HIV diagnosis is delayed long after the onset of HIV/AIDS-related symptoms, with an average delay of 2 years. The delay may be caused by factors such as lack of information, refusal of testing, limited resources, high cost barriers, stigma, and other factors. Meanwhile, patients seek care or cure for their opportunistic infections from various providers, depending on their health beliefs and suspected health conditions. The care seeking patterns are also influenced by their social sources of support and information, such as families, friends, partners, and media. Furthermore, accessibility to available health care options may determine utilization patterns.
Concerns of attrition, mortality and loss to follow up, once patients initiate ART are valid [31, 32]. However, for a number of reasons this study suggests that more attention has to be paid to patients in the pre-ART initiation period. Firstly, ‘shopping’ practices are common and range from use of traditional and faith healers, medicines obtained from chemists and herbalists, to the use of private physicians and public health facilities in varying degrees. Existing literature indicates that healers have an important role to play in facilitating access to appropriate care for the HIV-infected, and the scale up of ART [33–36]. Although community and household-based care may prove fundamental to successful scale-up and universal access to HIV/ AIDS care [37, 38], caution has to be exercised when these sectors are mobilized. Issues of safety, regulation and efficacy are yet to be resolved despite existing wide use of these non-formal sectors [39]. Although the health system is currently understood to consist of the public and private sectors only, HIV/AIDS patients perceive a broader health system inclusive of non-formal sector in the rural South African context. Tilburt and Miller argue for recognition of medical pluralism, in that acknowledging diverse health beliefs and practices reflects respect for patient autonomy [40]. Coordinated and integrated efforts between the public and private sectors and formal and informal systems are necessary to turn medical pluralism into a positive force of easily accessible HIV/AIDS services in rural South Africa.
Secondly, care-seeking patterns in this study indicate a predominant use of the public sector. Primary health care clinic is a popular first choice as a source of health care. This contrasts to the only other relevant Sub-Saharan study conducted in Malawi, in which traditional approaches were used first for AIDS-related illness [41]. The Malawian study was conducted in the era before ART was made widely available in Malawi. In-line with our findings, a Ghanaian study on diabetes mellitus found that chronically ill patients engage in medical pluralism and healer shopping practices, but biomedical management was their primary choice [21]. We further found that increasing use of health care overtime resulted in more centralized, higher level, specific and well-defined service points, thereby suggesting a transition from undifferentiated to more specific health problems and possibly targeted referrals or choices. These patterns are in-keeping with the hospital-centered nature of the HIV/ART care programs in South Africa, and may place a burden on the public health system [42]. Therefore, decentralizing HIV/ART services to the primary health care clinics may help to facilitate early access to ART for most people in rural areas. Furthermore, with the pressing need for HIV/ART care scale-up in order to reach universal access, the public sector may benefit from collaboration with the other existing sectors.
Thirdly, medical pluralism occurred in two-thirds of our HIV-infected participants prior to ART initiation, with an equal distribution of concurrent and sequential types of pluralism. Similar types have been described by others, and explained through patients’ disease explanatory models and rationing of care [22, 43–45]. The identified complexity in classifying types of pluralism in chronically ill HIV-infected patients necessitates better descriptions. Emerging patterns of medical pluralism will need to be carefully characterized in future studies of care pathways. We show in this study that most patients remain in their original sector visited, although they may switch facilities and providers within the sector. The health care switching practices in our study appear to draw patients away from the private and informal sectors into the public sector, indicating further risk of burdening the public health system. Some of the reasons for switching care may include lack of accessible services and diagnosis, lack of information and knowledge, stigma and denial, and high cost barriers [20–22, 43]. Furthermore, the need for affordable and effective treatment and relief from physical and psychosocial burden of chronic illness may shape care-seeking behavior [21]. Mediating factors for these switches require further exploration as they may impact on HIV/ART care access and scale-up, as well as future efforts to coordinate pluralistic care pathways.
Fourthly, the patterns of care delay in this study are overwhelming and indicative of utilization barriers to HIV/ ART care despite early use of health care. The majority of participants entered the broader health system soon after the onset of their symptoms, but only a small proportion received HIV testing and treatment in a timely manner. HIV testing is almost always delayed, and medical referral is a key factor leading to detection of infected patients. This is a problem, because recent data from South Africa showed that only about 24% of people know their HIV status [2]. Furthermore, the observation that rural people infected with HIV largely present to the broader health system when they are already symptomatic creates challenges to early detection. Similar findings were presented by Goudge et al. [10] in their household survey of chronically ill patients in rural South Africa, highlighting the need for improved access and a stronger health system. Since the health system prioritizes and arguably exclusively accommodates sick people, those who are well are unlikely to be identified within the health system [37]. Therefore, HIV education, testing, and care may need to be implemented horizontally across all sections of the public sector regardless of specialty for better access to be achieved. Furthermore, the need to detect people living with HIV before they develop symptoms necessitates the availability of screening mechanisms outside the health system [38].
Lastly, once ART is initiated, patients evidently adhere to the HIV/ART service point, and the extent of medical pluralism is drastically reduced. This pattern may be explained by comprehensive and patient-centered care services, as well as the almost immediate improvement or relief from HIV symptoms experienced when ART is initiated [5]. As patients with correct diagnoses of their medical problems receive appropriate information and care, and experience subsequent improvements in health, they may establish trust and remain adherent to the service provider [10, 46].
In light of the dominant view that HIV patients present late for care or not at all and the degree of poor health outcomes thereof [21, 24, 47], we argue here for a closer look at the design of health systems in South Africa. Most patients are entering health care services early and tend to use the public sector services where HIV services are rendered, but pluralistic patterns emerge and identification of their HIV-infection is delayed within the broader health system. These delays to definitive HIV/AIDS care may be attributed to healer shopping practices. Previous pluralism studies on malaria have also identified this potential consequence [20, 44].We agree that medical inaction by patients is a problem, and many access barriers are patient related [10, 21]. We recognize that patients may also delay care on purpose in order to minimize uncertainty by refusing care or waiting to identify particular illness types that may require health action [43]. However, missed HIV infection testing opportunities may delay access to care, perpetuate use of multiple service providers, and deplete personal and national resources for healthcare [36]. Many barriers are beyond patient control, such as resource limitations in the rural context. We also have to take into account the limitations of fit between Western biomedical health systems and local contextual illness beliefs and practices. Future research has to establish whether or not the current health care system is suited to meet the needs of these rural patients. All service points considered sources of health care by patients should be capable of rendering appropriate HIV services or advice to patients, and early access to care in the pre ART period may be achieved. Failing which, conflicting messages may be provided to patients by the different healers and providers, resulting in confusion and delays in definitive HIV/ AIDS care. If care is distributed to other sectors, most people are likely to receive care early, and still remain in their preferred sectors of care. These efforts may increase the likelihood of achieving universal access in resource-limited settings.
This study had several limitations. As participants were recruited from a HIV clinic in a public sector hospital, respondents may be considered successful users of HIV care. Thus the study did not include those who had never accessed HIV or ART care. However, this study aimed to understand routes to eventual ART use, and future research could valuably explore reasons for failure to ever access appropriate care. Due to the retrospective generation of care pathways in our study, most patients reported initial utilization patterns without the knowledge that they were HIV-infected at the time of falling ill and choosing to use health care. Data collection methods may have resulted in recall, under-reporting and social desirability biases, but the longitudinal design and validation processes were intended to minimize these forms of biases. In particular, under-reporting or lack of emphasis on self-care may have been a problem as participants were sampled from an ART clinic, assuming that they were more enlightened or informed about definitive therapies at this stage. However, the coding procedure also limited self-care as sources of medicines were captured and not necessarily the process of medicine use by patients. The categorization of ART initiation delay was limited by the challenge of correctly identifying need for ART from self-reports. The study consists largely of poor, rural patients sampled from a public sector, and a sample of private patients may have shown a different trend.
In conclusion, the nature of medical pluralism observed in this study highlights important patterns and implications. Rural people living with HIV and AIDS exhibit multiplicity in sources of health care, including formal and informal providers. The various pluralistic patterns occur in varying degrees and are potentially guided by a wide range of factors working in tandem. In addition, health care switching practices occur between formal and informal sectors, and within sectors but between health care providers. Finally, HIV diagnosis and treatment continues to be delayed despite patients’ early contact with the health system, necessitating strategies to increase the health system’s capacity to detect HIV early and retain patients in care. Without any intervention, medical pluralism and healer shopping practices may delay care and act as barriers to definitive HIV/AIDS care. However, the diversified availability of medical systems provides an opportunity for improved access to HIV/AIDS care in rural South Africa. Due to the chronic and largely asymptomatic nature of HIV, the need for household and community-based HIV detection and referral is evident. Taken together, the study suggests that in much of this poor rural community, the public sector remains the primary source for HIV testing, care and support. Efforts to accelerate access to care and strengthen the quality of services seem to offer the best option for reducing death and disability from HIV/AIDS in the region.
Acknowledgments
This research was funded in part by a 2005 minority supplement to the Lifespan/Tufts/Brown Center for AIDS Research (P30AI042853) from the National Institute of Allergy And Infectious Diseases. Authors would like to acknowledge the contribution of our research assistant Ms Thembi Matokane, the support offered by staff at Rixile clinic, and we thank all patients who took part in the study.
Contributor Information
M. Moshabela, Rural AIDS and Development Action Research (RADAR), University of Witwatersrand, Johannesburg, South Africa School of Public Health, University of Witwatersrand, Johannesburg, South Africa; RADAR, Po Box 02, Acornhoek, Mpumalanga 1360, South Africa, mosa@agincourt.co.za.
P. Pronyk, Rural AIDS and Development Action Research (RADAR), University of Witwatersrand, Johannesburg, South Africa Earth Institute, Columbia University, New York, USA.
N. Williams, University of Pittsburgh School of Medicine, Pittsburgh, USA
H. Schneider, Department of Public and Family Medicine, University, of Cape Town, Cape Town, South Africa
M. Lurie, Brown University Medical School, Rhode Island, USA
References
- 1.UNAIDS. Report on the global AIDS epidemic. Geneva: Joint United Nations Programme on HIV/AIDS (UNAIDS); 2008. [Google Scholar]
- 2.Shisana O, Rehle T, Simbayi L, et al. South African national HIV prevalence, incidence, behaviour and communication survey 200: a turning tide among teenagers? Cape Town: HSRC Press; 2009. [Google Scholar]
- 3.UNAIDS. Epidemiological fact sheet on HIV and AIDS, South Africa, September 2008 Update. Geneva: UNAIDS/WHO Working Group on Global HIV/AIDS and STI Surveillance; 2009. [Google Scholar]
- 4.Kahn K, Garenne ML, Collinson MA, Tollman SM. Mortality trends in a new South Africa: hard to make a fresh start. Scand J Public Health. 2007;35(Suppl 69):26–34. doi: 10.1080/14034950701355668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.National Department of Health. South African national Antiretroviral treatment guidelines. Pretoria: NDOH; 2004. [Google Scholar]
- 6.Montaner J, Hogg R, Wood E, et al. The case for expanding access to highly active antiretroviral therapy to curb the growth of the HIV epidemic. Lancet. 2006;368:531–536. doi: 10.1016/S0140-6736(06)69162-9. [DOI] [PubMed] [Google Scholar]
- 7.De Cock K, Grubb I. Towards Universal access: WHO’s role in HIV prevention, treatment and care. Bull World Health Organ. 2006;84(7):506–507. doi: 10.2471/blt.06.0339104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Coovadia H, Jewkes R, Barron P, Sanders D, McIntyre D. Health in South Africa 1. The health and health system of South Africa: historical roots of current public health challenges. Lancet. 2009;374(9692):817–834. doi: 10.1016/S0140-6736(09)60951-X. [DOI] [PubMed] [Google Scholar]
- 9.Mcintyre D, Gilson L, Wadee H, Thiede M, Okarafor O. Commercialisation and extreme inequality in health: The policy challenge in South Africa. J Int Dev. 2006;18:435–446. [Google Scholar]
- 10.Goudge J, Gilson L, Russell S, Gumede T, Mills A. Affordability, availability and acceptability barriers to health care for the chronically ill: longitudinal case studies from South Africa. BMC Health Serv Res. 2009;9:75. doi: 10.1186/1472-6963-9-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Habtom KG, Ruys P. The choice of a health care provider in Eritrea. Health Policy. 2007;80:202–217. doi: 10.1016/j.healthpol.2006.02.012. [DOI] [PubMed] [Google Scholar]
- 12.Maman S, Abler L, Parker L, et al. A comparison of HIV stigma and discrimination in five international sites: the influence of care and treatment resources in high prevalence settings. Soc Sci Med. 2009;68:2271–2278. doi: 10.1016/j.socscimed.2009.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Natrass N. The (political) economics of antiretroviral treatment in developing countries. Trends Microbiol. 2008 doi: 10.1016/j.tim.2008.08.012. [DOI] [PubMed] [Google Scholar]
- 14.Tsai AC, Chopra M, Pronyk PM, Martinson NA. Socioeconomic disparities in access to HIV/AIDS treatment programs in resource-limited settings. AIDS Care. 2009;21(1):59–63. doi: 10.1080/09540120802068811. [DOI] [PubMed] [Google Scholar]
- 15.Department of Health. Government Gazette. Pretoria: Department of Health; 2008. Draft policy on African traditional medicine for South Africa. [Google Scholar]
- 16.Cant S, Sharma U. A new medical pluralism? Alternative medicine, doctors, patients and the state. London: UCL Press; 1999. [Google Scholar]
- 17.Gilbert L. Medical pluralism in action? A case study of community pharmacies in Johannesburg, South Africa. J Altern Complement Med. 2004;10(3):547–555. doi: 10.1089/1075553041323777. [DOI] [PubMed] [Google Scholar]
- 18.Gilbert L, Selikow T, Walker L. Society, health and disease. Johannesburg: Raven Press/McMillan; 2002. [Google Scholar]
- 19.Janzen JM. The quest for therapy: medical pluralism in lower Zaire. California: University of California Press; 1982. [Google Scholar]
- 20.Nyamongo I. Health care switching behaviour of Malaria patients in a Kenyan rural community. Soc Sci Med. 2002;54:377–386. doi: 10.1016/s0277-9536(01)00036-3. [DOI] [PubMed] [Google Scholar]
- 21.De Graft Aikins A. Healer Shopping in Africa: new evidence from rural-urban qualitative study of Ghanaian Diabetes experiences. Br Med J. 2005;331(7519):737–742. doi: 10.1136/bmj.331.7519.737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hausmann-Muela S, Muela-Ribera J, Mushi AK, Tanner M. Medical Syncretism with reference to Malaria in a Tanzanian community. Soc Sci Med. 2002;55:403–413. doi: 10.1016/s0277-9536(01)00179-4. [DOI] [PubMed] [Google Scholar]
- 23.Kroeger A. Anthropological and socio-medical health care research in developing countries. Soc Sci Med. 1983;17(3):147–161. doi: 10.1016/0277-9536(83)90248-4. [DOI] [PubMed] [Google Scholar]
- 24.Mackian S, Bedri N, Lovel H. Up the garden path and over the edge: where might health-seeking behaviour take us? Health Policy Plan. 2004;19(3):137–146. doi: 10.1093/heapol/czh017. [DOI] [PubMed] [Google Scholar]
- 25.Uphold C, Mkanta W. Use of health care services among persons living with HIV infection: state of the science and future directions. AIDS Patient Care STDS. 2005;19(8):473–485. doi: 10.1089/apc.2005.19.473. [DOI] [PubMed] [Google Scholar]
- 26.Mkanta W, Uphold C. Theoretical and methodological issues in conducting research related to health care system utilization among individuals with HIV infection. AIDS Patient Care STDS. 2006;20(4):293–303. doi: 10.1089/apc.2006.20.293. [DOI] [PubMed] [Google Scholar]
- 27.Okello E, Neema S. Explanatory models and help-seeking behavior: pathways to psychiatric care among patients admitted for depression in Mulago Hospital, Kampala, Uganda. Qual Health Res. 2007;17(1):14–25. doi: 10.1177/1049732306296433. [DOI] [PubMed] [Google Scholar]
- 28.Moodley K. Mpumalanga Province. In: Barron P, Day C, Monticelli F, editors. The district health barometer 2007/08. Durban: Health Systems Trust; 2007. [Google Scholar]
- 29.National Department of Health. The national HIV and syphilis prevalence survey of South Africa. Pretoria: Department of Health; 2008. [Google Scholar]
- 30.Creswell JW, Miller DL. Determining validity in qualitative inquiry. Theory Practice. 2000;39(3):124–130. [Google Scholar]
- 31.Rosen S, Fox M, Gill C. Patient retention in antiretroviral therapy programs in Sub-Saharan Africa: a systematic review. PLoS Med. 2007;4(10):1691–1700. doi: 10.1371/journal.pmed.0040298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.MacPherson P, Moshabela M, Martinson N, Pronyk P. Mortality and loss to follow-up among HAART initiators in rural South Africa. Trans R Soc Med Hyg. 2009;103(6):588–593. doi: 10.1016/j.trstmh.2008.10.001. [DOI] [PubMed] [Google Scholar]
- 33.MacLachlan M, Carr S. Managing the AIDS crisis in Africa: in support of pluralism. J Manag Med. 1994;8(4):45. doi: 10.1108/02689239410068552. [DOI] [PubMed] [Google Scholar]
- 34.Ross E. Traditional healing in South Africa. Soc Work Health Care. 2007;46(2):15–33. doi: 10.1300/j010v46n02_02. [DOI] [PubMed] [Google Scholar]
- 35.Liddell C, Barrett L, Bydawell M. Indigenous representations of illness and AIDS in Sub-Saharan Africa. Soc Sci Med. 2005;60:691–700. doi: 10.1016/j.socscimed.2004.06.020. [DOI] [PubMed] [Google Scholar]
- 36.Plummer M, Mshana G, Wamoyi J, et al. ‘The man who believed he had AIDS was cured’: AIDS and sexually-transmitted infection treatment-seeking behaviour in rural Mwanza, Tanzania. AIDS Care. 2006;18(5):460–466. doi: 10.1080/09540120500220367. [DOI] [PubMed] [Google Scholar]
- 37.Girardi E, Sabin C, Monforte A. Late diagnosis of HIV infection: epidemiological features, consequences and strategies to encourage earlier testing. J Acquir Immune Defic Syndr. 2007;46(S1):S3–S8. doi: 10.1097/01.qai.0000286597.57066.2b. [DOI] [PubMed] [Google Scholar]
- 38.Matovu JK, Makumbi FE. Expanding access to voluntary HIV counselling and testing in sub-Saharan Africa: alternative approaches for improving uptake, 2001–2007. Trop Med Int Health. 2007;12(11):1315–1322. doi: 10.1111/j.1365-3156.2007.01923.x. [DOI] [PubMed] [Google Scholar]
- 39.Bodeker G, Carter G, Burford G, Dvorak-Little M. HIV/AIDS: traditional systems of health care in the management of a global epidemic. J Altern Complement Med. 2006;12(6):563–576. doi: 10.1089/acm.2006.12.563. [DOI] [PubMed] [Google Scholar]
- 40.Tilburt JC, Miller FG. Responding to medical pluralism in practice: a principled ethical approach. J Am Board Fam Med. 2007;20:489–494. doi: 10.3122/jabfm.2007.05.060205. [DOI] [PubMed] [Google Scholar]
- 41.Hatchett L, Kaponda C, Chihana C, et al. Health-seeking patterns for AIDS in Malawi. AIDS Care. 2004;16(7):827–833. doi: 10.1080/09540120412331290112. [DOI] [PubMed] [Google Scholar]
- 42.Cleary S, Boulle A, Castillo -Riquelme M, Mcintyre D. The burden of HIV/AIDS in the public healthcare system. S Afr J Econ. 2008;76(01):S3–S14. [Google Scholar]
- 43.Ryan G. What do sequential behavioral patterns suggest about the medical decision-making process? Modelling home case management of acute illnesses in a rural Cameroonian village. Soc Sci Med. 1998;46(2):209–225. doi: 10.1016/s0277-9536(97)00151-2. [DOI] [PubMed] [Google Scholar]
- 44.Hausmann-Muela S, Muela-Ribera J, Tanner M. Fake malaria and hidden parasites-the ambiguity of malaria. Anthropol Med. 1998;5(1):43–61. doi: 10.1080/13648470.1998.9964548. [DOI] [PubMed] [Google Scholar]
- 45.Kleinman A. Patients and healers in the context of culture. Berkeley: University of California Press; 1980. [Google Scholar]
- 46.Peltzer K. Patient experiences and health system responsiveness in South Africa. BMC Health Serv Res. 2009;9:117. doi: 10.1186/1472-6963-9-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bonjour MA, Montagne M, Zambrano M, et al. Determinants of late disease-stage presentation at diagnosis of HIV infection in Venezuela: a case-case comparison. AIDS Res Ther. 2008;5:6. doi: 10.1186/1742-6405-5-6. [DOI] [PMC free article] [PubMed] [Google Scholar]