Abstract
Introduction
Insufficient sleep is associated with cardiometabolic risk and neurocognitive impairment. Determinants of insufficient sleep include many social and environmental factors. Assessment of geographic hot/coldspots may uncover novel risk groups and/or targets for public health intervention. The aim of this study was to discern geographic patterns in the first data set to include county-level sleep data.
Methods
The 2009 Behavioral Risk Factor Surveillance System was used. Insufficient sleep was assessed with a survey item and dichotomized. Data from n = 2231 counties were available. Tests for significant spatial concentrations of high/low levels of insufficient sleep (hotspots/coldspots) used the Getis-Ord G* statistic of local spatial concentration, chosen due to the nature of missing data.
Results
Eighty-four counties were hotspots, with high levels of insufficient sleep (P < .01), and 45 were coldspots, with low insufficient sleep (P < .01). Hotspots were found in Alabama (1 county), Arkansas (1), Georgia (1), Illinois (1), Kentucky (25), Louisiana (1), Missouri (4), Ohio (7), Tennessee (12), Texas (9), Virginia (6), and West Virginia (16). Coldspots were found in Alabama (1 county), Georgia (2), Illinois (6), Iowa (6), Michigan (2), Minnesota (1), North Carolina (1), Texas (7), Virginia (12), and Wisconsin (6). Several contiguous hotspots and coldspots were evident. Notably, the 17 counties with the highest levels of insufficient sleep were found in a contiguous set at the intersection of Kentucky, Tennessee, Virginia, and West Virginia (all P < .0002).
Conclusions
Geographic distribution of insufficient sleep in the United States is uneven. Some areas (most notably parts of Appalachia) experience disproportionately high amounts of insufficient sleep and may be targets of intervention. Further investigation of determinants of geographic variability needs to be explored, which would enhance the utility of these data for development of public health campaigns.
Introduction
Insufficient sleep is increasingly recognized as an important public health issue.1 Population-based studies have shown that short sleep duration, which may represent insufficient sleep for many individuals, is associated with elevated risk of obesity, cardiovascular disease, diabetes, and a number of other significant health outcomes.2–6 Self-reported insufficient rest or sleep, the outcome studied in this article, has been linked with obesity, hypertension, hyperlipidemia, heart attack, and stroke.7 To address this public health issue, the social and environmental determinants of insufficient sleep need further examination.2,3,8,9 One possible determinant that has received little attention is geographic location.
Several recent studies have examined social environmental influences on sleep at the national level,6,10–12 but these generally did not address geographic patterning insufficient sleep. Hale et al,13,14 Bird et al,15 and Hale and Do16,17 have examined whether unhealthy neighborhoods influence the relationship between sleep and physical and mental health, but those studies focused on the characteristics of neighborhoods, not on the geographic region in which they were located. However, 1 recent study used the 2006 Behavioral Risk Factor Surveillance System (BRFSS) data for 36 US states to show that those in southern states were more likely to report difficulty sleeping over the past 2 weeks. The states with the highest rates of sleep disturbance included West Virginia, Oklahoma, Missouri, Arkansas, Mississippi, and Alabama; but, notably, data on some nearby states (eg, Kentucky or Ohio) were unavailable, making it difficult to observe clustering of insufficient sleep across states.
One issue with the limited existing research that examines geographic patterning of insufficient sleep is that the state maybe too broad a level of geographic aggregation. There may be particular regions within a state that are particularly susceptible to sleep problems and also regions that are relatively free of problems. Studies of the links between neighborhood characteristics and sleep suggest that geographic patterning operates at a more local level than the state. Until recently, no data have been available to address the question of whether insufficient sleep is geographically patterned at the local level, using data that represent the entire United States. These findings would be relevant to many stakeholders, including members of the public and health authorities at the national, regional, and state levels, who could use these data to discern the public health burden of sleep disturbance relative to geography.
Accordingly, the present study leveraged a large, national sample of US adults to assess whether insufficient sleep is differentially reported across counties. Specifically, county-level data from the 48 mainland US states were examined to discern hotspots and coldspots of insufficient sleep. Hypotheses included that (1) regional differences in the percentage of adults reporting insufficient sleep would be evident and most prominent in those states previously identified as having high levels of sleep disturbance; and (2) these regional patterns would elucidate a number of hotspots of abnormally high insufficient sleep and coldspots of abnormally low insufficient sleep.
Methods
Data from the 2009 BRFSS were used.18 The BRFSS is an annual, state-based, random-digit-dialed telephone survey of adults in the United States. It is conducted by the Centers for Disease Control and Prevention and designed to monitor health-related behaviors in the general population. Data from all 48 contiguous states and Washington, DC, were included in these analyses. Response rates varied by state, with a median of 53.86% (range, 37.90% [Oregon] to 66.85% [Nebraska]).
The outcome of interest was perceived insufficient rest or sleep (insufficient sleep). This was measured using the item, “During the past 30 days, for approximately how many days have you felt you did not get enough rest or sleep?” Responses were dichotomized, with those reporting ≥15/30 days being categorized as reporting insufficient sleep. This dichotomization was chosen for several reasons. First, a dichotomized variable allows for much more interpretable prevalence estimates. Second, the cutoff of 15 days was chosen to mirror the diagnostic criteria for insomnia, which suggests that symptoms should exist for approximately half of nights to be clinically relevant.19 Second, this dichotomization at 50% of nights is consistent with other BRFSS studies that similarly dichotomized global sleep disturbance.20–25 Third, preliminary evaluation of different cutoffs (3, 7, 15, or 30 days) did not result in noticeably different patterns of findings regarding insufficient sleep and outcomes.
To examine the prevalence of insufficient sleep, the BRFSS data were analyzed in 3 ways. First, prevalence of insufficient sleep was estimated for all available counties and mapped at the county level. Second, these county-level prevalence estimates were evaluated using a spatial clustering technique to identify regionally anomalous areas of counties that demonstrate unusually high or low values (ie, “hotspots” and “coldspots”). Third, linear regression analyses aimed to assess characteristics of individuals who live in hotspots and coldspots Vs most counties, which were identified as neither.
Regarding the clustering analysis, tests for significant spatial concentrations of high percentage values (or low percentage values) were conducted. These tests evaluate the percentage of respondents within a specific county that reported insufficient sleep, relative to neighboring counties. Typically, this analysis would involve comparing frequency of insufficient sleep with immediate neighbors. However, there were many missing counties that would make this approach problematic because counties were not missing at random (because these were generally the most sparsely populated counties), and all counties neighboring one of these missing counties would typically be excluded. Furthermore, the number of responses per county was highly variable, generally in proportion with the population density of that county. Therefore, a method is needed to account for this variability and missing data. To address this, the Getis-Ord G* statistic of local spatial concentration was used.26 For any given set of n spatial units, this local statistic is constructed for each spatial unit, i, by first identifying some appropriate measure, wij, of “closeness” to each other unit j (including i). Here, we choose the standard contiguity measure defined by wij = 1 if counties i and j share a common border (including the case, i = j and wij = 0 otherwise). For any given set of nonnegative data (xi : i = 1, …, n) associated with these n spatial units, the G* statistic is then defined for each unit, i, by the following:
| (1) |
Equivalently, if the immediate neighborhood of i is denoted by Ni = {j : wij = 1} then in our case this statistic takes the more easily interpretable form as follows:
| (2) |
In these terms, is simply the fraction of all individuals reporting insufficient sleep in the immediate neighborhood of county i. If this fraction is “unusually high” (or “unusually low”) relative to levels that would be expected by chance alone, then it can reasonably be concluded that there is “significant insufficient sleep” (or “significant lack of insufficient sleep”) in the neighborhood of county i.
These notations can be made precise in terms of the null hypothesis that the observed value, say , is not statistically distinguishable from values that would be observed if the given percentages (xi : i = 1, …, n) were randomly distributed among spatial units. The actual distribution of under this null hypothesis can then be approximated by randomly reassigning these percentages to spatial units many times and computing the statistic in each case. More formally, if , k = 1,.., M, denotes the values obtained from M random reassignments (permutations) of percentages to spatial units, then this constitutes a sample of size M of under this null hypothesis. Assuming that the observed value, , is coming from the same population, this yields a sample [ ] of size M + 1. So if denotes the number of these samples with values at least as high as , then the chance of obtaining a value as high as is estimated by the following:
| (3) |
and yields a natural P value for an upper-tailed test of this null hypothesis. For example, if then there is only a 5% chance of observing a value as high as if this null hypothesis were true. Conversely, if denotes the number of these samples with values no higher than , then:
| (4) |
yields the equivalent P value for a lower tailed test of this hypothesis.
Finally, it should be noted this statistic is asymptotically normally distributed under the above null hypothesis26. However, the present approach is generally more reliable for small samples, such as those obtained for many of the counties in this study. Hence, the results reported below are for this direct-sampling approach. The asymptotic approach (as implemented in ArcGIS software) was assessed for purposes of comparison and was found to yield very similar results (not reported here).
These tests were applied using M = 9999 random permutations. A P value of <.01 was chosen to denote significant high or low levels of insufficient sleep, corresponding to a level in the top (or bottom) 100 values among the 10,000 permutations. A value in the top 100 would be considered a “hotspot,” and a value in the bottom 100 would be considered a “coldspot.” Confidence intervals around percentages were computed using the Clopper and Pearson exact method as implemented by the binofit program in MATLAB, based on the implementation by Daly.27
To examine differences between individuals who reside in a “hotspot” or “coldspot” county relative to counties that were not identified as either one, multinomial logistic regression analyses were used, with county type coded as hotspot, coldspot, or neither (reference) as the outcome variable and demographic, socioeconomic, and health variables from the BRFSS survey used as predictors. These included the following: age (18–24, 25–29, 30–34, 35–39, 40–44, 55–59, 60–64, 65–69, 70–74, 75–79, and 80+ [reference]), sex, education (college graduate [reference], some college, high school, and less than high school), race/ ethnicity, overall health (excellent [reference], very good, good, fair, and poor), consumption of ≥5 servings of fruits/vegetables per day (yes or no), sedentary lifestyle (any exercise within the past 30 days), employment (low intensity [reference], moderate intensity, manual labor, and unemployed), heavy alcohol use (≥2 drinks per day for women, ≥3 for men), current smoking, overall mental health (no. of days in the past month of poor mental health), household size, access to health insurance, and obesity. These variables were entered simultaneously, so that unique effects of each factor could be examined.
The present analysis allows for not only the enumeration of county-level prevalence estimates for insufficient sleep but also the spatial analysis of potential areas of the country with unusually high and low concentrations of insufficient sleep. There are a number of important limitations to this approach (see below), but there are also many distinct advantages. Importantly, this approach is unique in that it allows for spatial analysis in the presence of data that is not missing at random.
Results
Respondents and counties
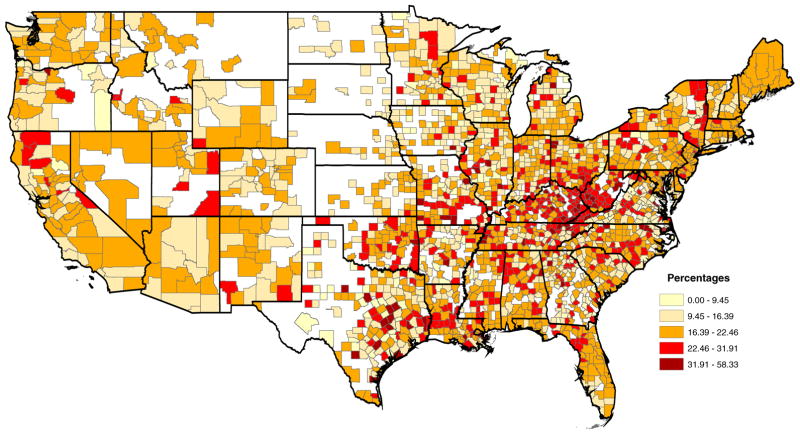
Data for the present study were drawn from 424,989 respondents to the 2009 BRFSS. Those who did not respond to the insufficient sleep item or responded “don’t know/not sure” or “refused” were excluded (7618 respondents, 1.76% of responses). Responses were aggregated by county. Of the 3109 counties/county equivalents in the mainland United States, n = 2231 counties were represented among respondents who participated in the BRFSS. Geographic distribution of insufficient sleep by quintile is reported in Fig. 1.
Fig. 1.
Percentages of insufficient sleep by county.
Hotspots of insufficient sleep
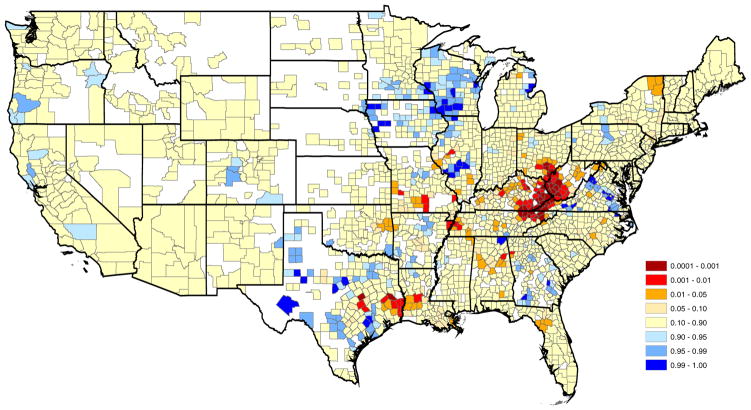
Table 1 lists the 84 counties identified as “hotspots,” reporting significantly high levels of insufficient sleep (P < .01 level). Table 1 includes the state and name of each county, the percentage of insufficient sleep observed, 95% confidence interval, the value for each county i, and the P value . The largest aggregation of counties identified as hotspots includes an area at the intersection of Kentucky, Tennessee, West Virginia, and Virginia. This area includes a contiguous set of counties that comprise the top 19 counties categorized as hotspots (all with P values ≤.0002). In addition, more than half of the 84 counties identified as hotspots come from this region. Other regions identified as hotspots include areas of Ohio and Texas and Missouri and single counties in other states. Fig. 2 presents a map of hotspots and coldspots. Fig. 3 shows the region with the largest number of hotspots in detail, including the 15 counties with P < .0001 for their G* value.
Table 1.
Counties identified as hotspots of insufficient sleep.
| State | County | % Insufficient sleep | 95% CI | G* | P+ | |
|---|---|---|---|---|---|---|
| Tennessee | Union | 14.29 | 0.36 | 57.87 | 0.0048 | .0001 |
| Kentucky | Whitley | 27.78 | 17.86 | 39.59 | 0.0057 | .0001 |
| Tennessee | Scott | 28.57 | 3.67 | 70.96 | 0.0054 | .0001 |
| Kentucky | Perry | 29.13 | 21.41 | 37.85 | 0.0047 | .0001 |
| West Virginia | Mingo | 29.79 | 20.79 | 40.10 | 0.0060 | .0001 |
| Kentucky | Bell | 30.00 | 18.85 | 43.21 | 0.0056 | .0001 |
| West Virginia | Logan | 30.00 | 20.79 | 40.57 | 0.0041 | .0001 |
| Virginia | Wise | 30.51 | 19.19 | 43.87 | 0.0063 | .0001 |
| Kentucky | Letcher | 30.56 | 22.05 | 40.16 | 0.0048 | .0001 |
| Kentucky | Pike | 30.60 | 25.14 | 36.49 | 0.0060 | .0001 |
| Virginia | Lee | 32.61 | 19.53 | 48.02 | 0.0047 | .0001 |
| Tennessee | Claiborne | 35.29 | 14.21 | 61.67 | 0.0059 | .0001 |
| Kentucky | Knott | 37.50 | 27.40 | 48.47 | 0.0052 | .0001 |
| West Virginia | Lincoln | 39.29 | 26.50 | 53.25 | 0.0057 | .0001 |
| Tennessee | Campbell | 52.17 | 30.59 | 73.18 | 0.0053 | .0001 |
| West Virginia | Kanawha | 24.54 | 20.99 | 28.38 | 0.0062 | .0002 |
| Kentucky | Magoffin | 25.58 | 13.52 | 41.17 | 0.0044 | .0002 |
| West Virginia | Boone | 32.14 | 22.36 | 43.22 | 0.0046 | .0002 |
| Kentucky | Harlan | 37.50 | 27.40 | 48.47 | 0.0046 | .0002 |
| Ohio | Vinton | 40.00 | 12.16 | 73.76 | 0.0050 | .0002 |
| West Virginia | Cabell | 24.27 | 18.58 | 30.72 | 0.0050 | .0003 |
| Virginia | Buchanan | 29.17 | 12.62 | 51.09 | 0.0051 | .0003 |
| West Virginia | Wayne | 29.91 | 21.80 | 39.07 | 0.0050 | .0003 |
| Kentucky | McCreary | 28.00 | 16.23 | 42.49 | 0.0049 | .0004 |
| Kentucky | Montgomery | 26.60 | 18.01 | 36.71 | 0.0032 | .0005 |
| Ohio | Meigs | 26.67 | 12.28 | 45.89 | 0.0049 | .0005 |
| Ohio | Gallia | 30.77 | 14.33 | 51.79 | 0.0048 | .0005 |
| West Virginia | Wyoming | 35.71 | 23.36 | 49.64 | 0.0048 | .0005 |
| Ohio | Hocking | 30.00 | 11.89 | 54.28 | 0.0049 | .0006 |
| Virginia | Dickenson | 26.09 | 10.23 | 48.41 | 0.0039 | .0007 |
| Virginia | Scott | 26.32 | 13.40 | 43.10 | 0.0048 | .0007 |
| Kentucky | Floyd | 32.95 | 26.00 | 40.49 | 0.0038 | .0007 |
| Texas | Falls | 0.00 | 0.00 | 33.63 | 0.0042 | .0008 |
| Tennessee | Hamblen | 28.57 | 14.64 | 46.30 | 0.0044 | .0008 |
| Texas | Angelina | 31.03 | 15.28 | 50.83 | 0.0053 | .0008 |
| Tennessee | Greene | 24.19 | 14.22 | 36.75 | 0.0047 | .0009 |
| Tennessee | Hawkins | 25.00 | 15.02 | 37.40 | 0.0048 | .0010 |
| Kentucky | Lawrence | 31.25 | 20.24 | 44.06 | 0.0042 | .0010 |
| Texas | Newton | 28.57 | 3.67 | 70.96 | 0.0048 | .0011 |
| Ohio | Athens | 31.82 | 18.61 | 47.58 | 0.0053 | .0012 |
| Arkansas | Mississippi | 21.13 | 12.33 | 32.44 | 0.0064 | .0013 |
| Kentucky | Laurel | 23.02 | 15.99 | 31.35 | 0.0052 | .0013 |
| Tennessee | Anderson | 31.58 | 17.50 | 48.65 | 0.0047 | .0013 |
| West Virginia | Raleigh | 27.70 | 20.67 | 35.65 | 0.0046 | .0015 |
| Kentucky | Knox | 35.71 | 23.36 | 49.64 | 0.0036 | .0015 |
| Texas | Jasper | 55.56 | 21.20 | 86.30 | 0.0042 | .0015 |
| West Virginia | Mercer | 20.81 | 14.60 | 28.21 | 0.0047 | .0016 |
| Kentucky | Johnson | 27.38 | 18.21 | 38.20 | 0.0036 | .0016 |
| Texas | Milam | 37.50 | 8.52 | 75.51 | 0.0046 | .0018 |
| Kentucky | Clark | 26.67 | 7.79 | 55.10 | 0.0046 | .0020 |
| Kentucky | Harrison | 15.38 | 1.92 | 45.45 | 0.0035 | .0021 |
| Kentucky | Breathitt | 28.07 | 16.97 | 41.54 | 0.0029 | .0021 |
| West Virginia | McDowell | 21.88 | 12.51 | 33.97 | 0.0040 | .0022 |
| Kentucky | Boyd | 25.14 | 19.03 | 32.07 | 0.0040 | .0023 |
| Texas | Orange | 18.18 | 5.19 | 40.28 | 0.0040 | .0024 |
| West Virginia | Putnam | 23.66 | 16.68 | 31.88 | 0.0040 | .0025 |
| Kentucky | Bourbon | 46.15 | 19.22 | 74.87 | 0.0040 | .0027 |
| Kentucky | Clay | 31.25 | 18.66 | 46.25 | 0.0040 | .0028 |
| Virginia | Russell | 42.22 | 27.66 | 57.85 | 0.0051 | .0028 |
| Missouri | Howell | 33.33 | 19.09 | 50.22 | 0.0024 | .0031 |
| Texas | Tyler | 26.32 | 9.15 | 51.20 | 0.0034 | .0035 |
| Kentucky | Carter | 28.74 | 19.54 | 39.43 | 0.0039 | .0036 |
| Tennessee | Lauderdale | 36.84 | 21.81 | 54.01 | 0.0040 | .0036 |
| West Virginia | Summers | 22.86 | 10.42 | 40.14 | 0.0045 | .0037 |
| Kentucky | Morgan | 28.21 | 20.28 | 37.27 | 0.0034 | .0042 |
| Texas | Burleson | 33.33 | 4.33 | 77.72 | 0.0039 | .0044 |
| Kentucky | Pulaski | 20.34 | 14.67 | 27.03 | 0.0050 | .0045 |
| Texas | Trinity | 28.57 | 3.67 | 70.96 | 0.0039 | .0045 |
| Georgia | Polk | 13.64 | 2.91 | 34.91 | 0.0044 | .0047 |
| Illinois | Mason | 25.00 | 5.49 | 57.19 | 0.0034 | .0047 |
| West Virginia | Fayette | 25.42 | 17.86 | 34.26 | 0.0038 | .0060 |
| Tennessee | Grainger | 50.00 | 18.71 | 81.29 | 0.0044 | .0068 |
| Tennessee | Jefferson | 12.90 | 3.63 | 29.83 | 0.0039 | .0069 |
| Tennessee | Haywood | 19.35 | 7.45 | 37.47 | 0.0043 | .0070 |
| West Virginia | Mason | 30.67 | 20.53 | 42.38 | 0.0039 | .0070 |
| West Virginia | Jackson | 21.95 | 13.56 | 32.46 | 0.0044 | .0073 |
| Alabama | Calhoun | 16.67 | 11.76 | 22.60 | 0.0038 | .0074 |
| Missouri | Cape Girardeau | 24.59 | 14.46 | 37.29 | 0.0033 | .0075 |
| Kentucky | Hardin | 19.49 | 14.17 | 25.75 | 0.0059 | .0076 |
| Missouri | Cedar | 25.00 | 3.19 | 65.09 | 0.0022 | .0079 |
| Missouri | Texas | 25.00 | 9.77 | 46.71 | 0.0049 | .0079 |
| Ohio | Ross | 25.81 | 11.86 | 44.61 | 0.0048 | .0082 |
| Ohio | Lawrence | 25.81 | 15.53 | 38.50 | 0.0048 | .0091 |
| Louisiana | Rapides | 20.50 | 16.82 | 24.58 | 0.0047 | .0099 |
Abbreviation: CI, confidence interval.
Fig. 2.
Hotspots and coldspots of insufficient sleep, represented by P values for both high (red) and low (blue) concentrations of insufficient sleep by county.
Fig. 3.
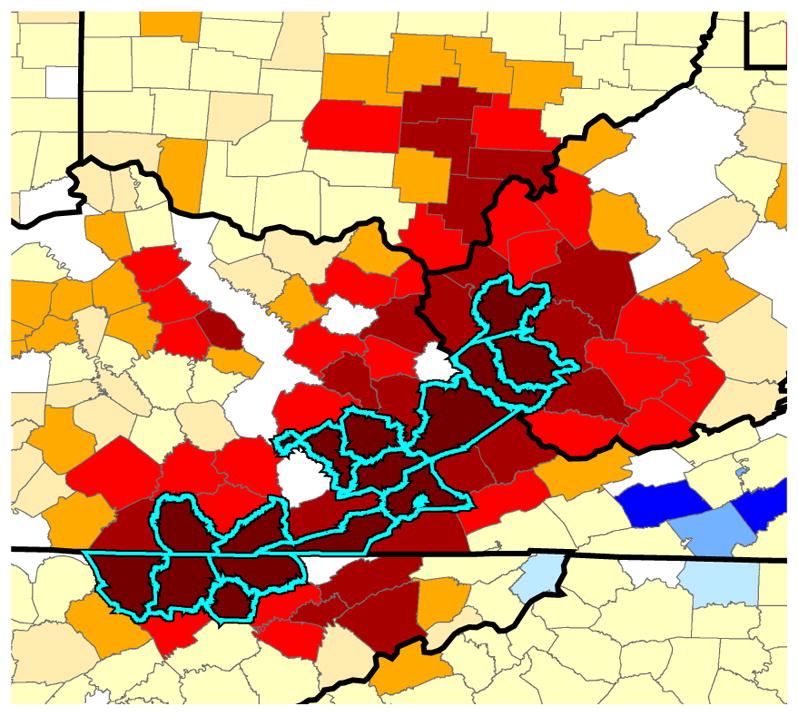
Map of the 15 counties that had the highest percentage of insufficient sleep, all with P < .0001.
Coldspots of insufficient sleep
Table 2 lists the 45 counties identified as reporting “coldspots” with significantly low levels of insufficient sleep (P < .01 level). Table 2 includes the state and name of each county, the percentage of insufficient sleep observed, 95% confidence interval, the value for each county i, and the P value . Unlike the large aggregation of hotspots identified above, there are no coldspots of comparable intensity. However, there were several regions that contained smaller aggregations of coldspots, including areas of Texas, Northern Virginia, and the Northern Midwest.
Table 2.
Counties identified as coldspots of low insufficient sleep.
| State | County | % Insufficient sleep | 95% CI | G* | P− | |
|---|---|---|---|---|---|---|
| Texas | Howard | 0.00 | 0.00 | 52.18 | 0.0000 | .0000 |
| Texas | Pecos | 0.00 | 0.00 | 45.93 | 0.0000 | .0000 |
| Texas | Erath | 33.33 | 11.82 | 61.62 | 0.0011 | .0000 |
| Virginia | Harrisonburg | 0.00 | 0.00 | 45.93 | 0.0002 | .0008 |
| Wisconsin | Iowa | 15.25 | 7.22 | 26.99 | 0.0017 | .0009 |
| Illinois | Christian | 20.00 | 4.33 | 48.09 | 0.0010 | .0009 |
| Michigan | Iosco | 3.23 | 0.08 | 16.70 | 0.0004 | .0011 |
| Illinois | Montgomery | 0.00 | 0.00 | 16.84 | 0.0022 | .0014 |
| Virginia | Chesterfield | 17.29 | 11.29 | 24.81 | 0.0033 | .0015 |
| Texas | Colorado | 18.18 | 2.28 | 51.78 | 0.0016 | .0015 |
| Wisconsin | Adams | 12.50 | 5.18 | 24.07 | 0.0022 | .0019 |
| Illinois | Madison | 18.87 | 13.11 | 25.83 | 0.0030 | .0019 |
| Wisconsin | Grant | 15.09 | 6.75 | 27.59 | 0.0023 | .0020 |
| Wisconsin | Brown | 14.29 | 8.39 | 22.16 | 0.0019 | .0021 |
| Virginia | Colonial Heights | 0.00 | 0.00 | 84.19 | 0.0006 | .0026 |
| Virginia | Rockingham | 6.52 | 1.37 | 17.90 | 0.0023 | .0026 |
| Michigan | Aremac | 0.00 | 0.00 | 19.51 | 0.0012 | .0027 |
| Georgia | Mitchell | 11.11 | 1.38 | 34.71 | 0.0020 | .0027 |
| Wisconsin | Buffalo | 15.56 | 6.49 | 29.46 | 0.0013 | .0031 |
| Alabama | Jackson | 11.11 | 2.35 | 29.16 | 0.0020 | .0032 |
| Texas | Dawson | 0.00 | 0.00 | 60.24 | 0.0006 | .0033 |
| Georgia | Toombs | 13.64 | 2.91 | 34.91 | 0.0009 | .0035 |
| Iowa | Carroll | 6.25 | 0.77 | 20.81 | 0.0003 | .0038 |
| Virginia | Greensville | 15.00 | 3.21 | 37.89 | 0.0017 | .0038 |
| Illinois | Shelby | 0.00 | 0.00 | 21.80 | 0.0024 | .0044 |
| Texas | Brown | 21.74 | 7.46 | 43.70 | 0.0010 | .0051 |
| Wisconsin | Richland | 7.55 | 2.09 | 18.21 | 0.0017 | .0052 |
| Virginia | Waynesboro | 0.00 | 0.00 | 97.50 | 0.0003 | .0060 |
| Virginia | Staunton | 0.00 | 0.00 | 84.19 | 0.0003 | .0061 |
| Texas | Austin | 5.00 | 0.13 | 24.87 | 0.0021 | .0063 |
| Virginia | Petersburg | 5.26 | 0.13 | 26.03 | 0.0013 | .0063 |
| North Carolina | Hertford | 11.11 | 0.28 | 48.25 | 0.0010 | .0068 |
| Iowa | O’Brien | 11.11 | 2.35 | 29.16 | 0.0017 | .0069 |
| Virginia | Floyd | 6.67 | 0.17 | 31.95 | 0.0021 | .0070 |
| Virginia | Goochland | 4.17 | 0.11 | 21.12 | 0.0021 | .0074 |
| Minnesota | Winona | 9.09 | 3.02 | 19.95 | 0.0025 | .0080 |
| Virginia | Wythe | 20.69 | 7.99 | 39.72 | 0.0013 | .0083 |
| Iowa | Clayton | 18.18 | 6.98 | 35.46 | 0.0029 | .0085 |
| Wisconsin | Dane | 16.67 | 10.98 | 23.78 | 0.0025 | .0087 |
| Iowa | Sioux | 11.24 | 5.52 | 19.69 | 0.0014 | .0088 |
| Iowa | Harrison | 14.29 | 4.81 | 30.26 | 0.0010 | .0088 |
| Illinois | Stephenson | 16.67 | 4.74 | 37.38 | 0.0021 | .0089 |
| Virginia | Henrico | 14.79 | 9.39 | 21.71 | 0.0021 | .0094 |
| Illinois | Jersey | 6.67 | 0.17 | 31.95 | 0.0014 | .0095 |
| Iowa | Crawford | 4.44 | 0.54 | 15.15 | 0.0010 | .0097 |
Differentiating hotspots and coldspots
Multinomial logistic regression analyses including age, sex, race/ ethnicity, household size, education, insurance access, employment, fruit and vegetable consumption, sedentary lifestyle, heavy drinking, smoking, obesity, overall health, and mental health, included n = 373,176 respondents with complete data for analysis. Results can be seen in Table 3. Overall, individuals in hotspot counties were more likely to be younger to middle-aged, White, living with only 1 other person, less educated, with health insurance, and unemployed. They are also more likely to be sedentary, smokers, obese, and in overall fair or poor health, and they are less likely to be heavy drinkers and less likely to report poor mental health only 1–7 days in the past month. Individuals in coldspot counties were more likely to be White and have only a high school education, and no individuals in coldspot counties lived in households with ≥10 people.
Table 3.
Multinomial logistic regression analyses examining demographic, socioeconomic, and health factors that differentiate individuals in hotspots and coldspots.
| Variable | Category | Hotspot (Vs neither)
|
Coldspot (Vs neither)
|
||||
|---|---|---|---|---|---|---|---|
| OR | 95% CI | P | OR | 95% CI | P | ||
| Age (y) | 18–24 | 1.65 | 1.23–2.23 | .001 | 1.16 | 0.73–1.82 | .532 |
| 25–29 | 2.81 | 2.08–3.81 | <.001 | 0.78 | 0.47–1.29 | .338 | |
| 30–34 | 2.39 | 1.82–3.15 | <.001 | 0.96 | 0.63–1.45 | .838 | |
| 35–39 | 2.06 | 1.58–2.69 | <.001 | 0.79 | 0.53–1.16 | .221 | |
| 40–44 | 2.21 | 1.70–2.87 | <.001 | 0.84 | 0.58–1.21 | .344 | |
| 45–49 | 1.91 | 1.51–2.41 | <.001 | 0.71 | 0.49–1.01 | .059 | |
| 50–54 | 1.89 | 1.52–2.35 | <.001 | 0.83 | 0.59–1.15 | .256 | |
| 55–59 | 1.82 | 1.48–2.24 | <.001 | 0.80 | 0.57–1.11 | .180 | |
| 60–64 | 1.58 | 1.30–1.93 | <.001 | 0.89 | 0.65–1.20 | .436 | |
| 65–69 | 1.54 | 1.27–1.86 | <.001 | 0.83 | 0.61–1.12 | .227 | |
| 70–74 | 1.41 | 1.16–1.72 | .001 | 0.82 | 0.60–1.12 | .214 | |
| 75–79 | 1.18 | 0.96–1.46 | .109 | 0.75 | 0.54–1.04 | .088 | |
| 80+ | 1.00 | Reference | 1.00 | Reference | |||
| Sex | Male | 1.04 | 0.93–1.16 | .500 | 0.94 | 0.80–1.11 | .487 |
| Female | 1.00 | Reference | 1.00 | Reference | |||
| Race/ethnicity | Non-Hispanic White | 1.00 | Reference | 1.00 | Reference | ||
| Black/African American | 0.30 | 0.24–0.38 | <.001 | 0.55 | 0.37–0.81 | .003 | |
| Hispanic/Latino | 0.10 | 0.06–0.18 | <.001 | 0.42 | 0.28–0.64 | <.001 | |
| Asian/other | 0.34 | 0.18–0.62 | <.001 | 0.46 | 0.27–0.79 | .005 | |
| Multiracial | 0.53 | 0.40–0.70 | <.001 | 0.86 | 0.36–2.04 | .732 | |
| Household size | 1 (Live alone) | 1.00 | Reference | 1.00 | Reference | ||
| 2 People | 1.15 | 1.04–1.28 | .007 | 1.21 | 1.02–1.43 | .0310 | |
| 3–5 People | 0.98 | 0.87–1.11 | .766 | 1.09 | 0.90–1.34 | .378 | |
| 6–9 People | 0.75 | 0.55–1.02 | .063 | 0.70 | 0.44–1.12 | .133 | |
| ≥10 People | 1.58 | 0.24–10.38 | .636 | 0.00 | 0.00–0.00 | <.001 | |
| Education | Less than high school | 3.11 | 2.58–3.73 | <.001 | 1.15 | 0.81–1.62 | .432 |
| High school | 2.22 | 1.93–2.56 | <.001 | 1.33 | 1.10–1.62 | .004 | |
| Some college | 1.63 | 1.39–1.92 | <.001 | 1.03 | 0.85–1.25 | .770 | |
| College graduate | 1.00 | Reference | 1.00 | Reference | |||
| Insurance | Yes | 1.00 | Reference | 1.00 | Reference | ||
| No | 1.39 | 1.17–1.659 | <.001 | 0.98 | 0.71–1.34 | .881 | |
| Employment | Low intensity | 1.00 | Reference | 1.00 | Reference | ||
| Moderate intensity | 1.01 | 0.84–1.213 | .931 | 1.07 | 0.82–1.40 | .607 | |
| Manual labor | 1.03 | 0.82–1.301 | .788 | 0.79 | 0.54–1.15 | .218 | |
| Unemployed | 1.22 | 1.06–1.397 | .006 | 0.83 | 0.67–1.04 | .106 | |
| Fruit/vegetable consumption | <1/d | 1.11 | 0.82–1.498 | .510 | 0.91 | 0.56–1.48 | .708 |
| 1–3/d | 1.08 | 0.94–1.247 | .265 | 1.12 | 0.89–1.41 | .350 | |
| 3–5/d | 1.07 | 0.93–1.221 | .368 | 0.99 | 0.81–1.22 | .942 | |
| ≥5/d | 1.00 | Reference | 1.00 | Reference | |||
| Sedentary lifestyle | No | 1.00 | Reference | 1.00 | Reference | ||
| Yes | 1.37 | 1.20–1.566 | <.001 | 0.78 | 0.62–0.97 | .024 | |
| Heavy drinking | No | 1.00 | Reference | 1.00 | Reference | ||
| Yes | 0.53 | 0.39–0.727 | <.001 | 1.04 | 0.77–1.41 | .792 | |
| Smoking | No | 1.00 | Reference | 1.00 | Reference | ||
| Yes | 1.17 | 1.02–1.343 | .027 | 0.98 | 0.78–1.23 | .867 | |
| Obesity | No | 1.00 | Reference | 1.00 | Reference | ||
| Yes | 1.17 | 1.03–1.314 | .012 | 1.18 | 0.96–1.44 | .110 | |
| Overall health | Excellent | 1.00 | Reference | 1.00 | Reference | ||
| Very good | 1.15 | 0.95–1.385 | .165 | 1.12 | 0.88–1.40 | .389 | |
| Good | 1.17 | 0.97–1.417 | .100 | 1.01 | 0.77–1.33 | .925 | |
| Fair | 1.53 | 1.22–1.912 | <.001 | 1.04 | 0.72–1.49 | .834 | |
| Poor | 2.00 | 1.57–2.555 | <.001 | 1.66 | 0.95–2.90 | .075 | |
| Mental health (d) | 0 | 1.00 | Reference | 1.00 | Reference | ||
| 1–7 | 0.76 | 0.64–0.916 | .004 | 0.92 | 0.75–1.13 | .435 | |
| 8–14 | 0.95 | 0.69–1.298 | .738 | 0.83 | 0.50–1.36 | .453 | |
| 15–21 | 1.02 | 0.82–1.274 | .845 | 0.77 | 0.51–1.17 | .217 | |
| ≥22 | 1.14 | 0.96–1.361 | .141 | 0.78 | 0.53–1.15 | .216 | |
Discussion
Insufficient sleep is an important health risk factor, but little is known about its geographic distribution. The present study evaluated, at the county level, whether self-reported insufficient sleep is disproportionately distributed across the United States. Overall, we found that there are several notable hotspots, particularly 1 very large concentration in the Appalachia region that connects Tennessee, Virginia, West Virginia, Kentucky, and Ohio. Other hotspots were identified, particularly in the Southeast and Midwest United States. A number of coldspots were also identified, primarily in the Midwest, Texas, and Northern Virginia.
The main finding of this study is that the region that represents the largest aggregation of hotspots lies in a region of Appalachia that traverses West Virginia, Kentucky, Tennessee, Virginia, and Ohio. There have been a number of studies of this region that have shown that Appalachia is a region that has one of the highest obesity rates in the nation.28,29 In addition, individuals living in this region are at greater risk for cardiovascular disease30,31, diabetes20,21, lung diseases32–34, and several types of cancer30,32,33,35, relative to individuals in other areas. Some reasons for this may be the general lack of education in this region, low socioeconomic status, unemployment, lack of access to care, and lack of infrastructure.36 It is unclear why this region, in particular, has such a high rate of insufficient sleep relative to other regions. It may be the case that so many of the risk factors that are particularly prevalent in this area are also commonly identified as either risk factors for poor sleep or potential effects of poor sleep.3,37,38
In examining differences between individuals in hotspot and coldspot counties relative to counties that were neither, no clear pattern emerged for predicting individuals in coldspot counties, suggesting that the examined factors may not be the most relevant predictors. Regarding hotspot counties, the general pattern emerged that relatively younger individuals of lower socioeconomic status and poorer health were more likely to live in hotspot counties. It is interesting to note that racial/ethnic minority status was negatively associated with living in either a hotspot or coldspot county.
Although no previous studies have examined geographic patterning of insufficient sleep at the county level, 2 previous studies have used BRFSS data to investigate geographic patterning of other sleep-related variables. McKnight-Eily et al39 assessed the prevalence of insufficient sleep using the 2008 BRFSS. The measure of insufficient sleep was the same survey item, although it was categorized as 0/30, 1–13/30, 14–29/30, or 30/30 days (instead of 15–30/30 Vs 0–14/30 days used in the present study). Their analysis showed that, among the 48 continental US states and Washington, DC, the states with the highest rates of insufficient sleep every night were (in order), West Virginia (19.3%), Tennessee (14.8%), Kentucky (14.4%), Oklahoma (14.3%), Florida (13.5%), Georgia (13.4%), Missouri (13.4%), Alabama (13.2%), Mississippi (13.1%), Louisiana (13.0%), and North Carolina (13.0%). In the present study, hotspots were identified in nearly all of these states, particularly the 3 with the highest rates: West Virginia, Tennessee, and Kentucky, replicating these findings. The findings from the present study also extend these findings by identifying which areas of these states are at heightened risk because hotspots were generally confined to specific areas and were not statewide.
One other previous study has examined geographic patterning of sleep. Using BRFSS 2006, our group20 examined state-level prevalence of general sleep disturbance (which included difficulty falling asleep, difficulty maintaining sleep, or sleeping too much) as well as daytime tiredness/fatigue. This analysis also found that the states with the highest concentrations of both sleep disturbance and daytime/fatigue included West Virginia, Alabama, Mississippi, Missouri, and Oklahoma. As with the previously described study by McKnight-Eily et al39, the present study replicates the finding that states in Appalachia and the Southeast United States are at high risk for unhealthy sleep, and it extends these findings by suggesting regions within those states at highest risk.
The present data suggest that there are several areas of the country, most notable Appalachia, which may experience disproportionately high rates of insufficient sleep. To the degree to which this represents undiagnosed or untreated sleep disorders, this suggests that the areas identified as hotspots might be good targets for intervention. Notably, there are relatively few sleep centers accredited by the American Academy of Sleep Medicine in the central Appalachia region. Perhaps resources could be directed to this region to screen for and treat sleep disorders at these centers. Furthermore, this area may be ideal for adding sleep to existing health education programs.
Limitations
The most important limitation of the current study is that we are unable to explore reasons for this geographic variation. The previous study by Grandner et al20 found that variation in sleep disturbance at the census region level was driven by regional differences in mental health, race/ethnicity, access to health care, socioeconomics, smoking, and weather patterns. The limitations of the county-level analyses preclude similar analyses in this context. For example, although several previous studies have identified Appalachia as a region that is particularly high risk of chronic disease and a number of other adverse outcomes (see above), the present study is unable to determine whether these factors mediate the geographic relationship, due to limitations in the ability of this survey to capture these factors and limitations to the statistical techniques to leverage covariates.
Another important limitation of this approach is that the G statistic can be somewhat unpredictable when a county exhibits prevalence of insufficient sleep that is very different from its neighbors. This could result in a county (such as Falls County, TX) where the estimated prevalence is 0%, yet it is identified as a hotspot because all of its neighbors have high prevalence. Clearly, it is at the center of a hotspot, although it could be a “donut hole,” or it could have been misclassified due to small sample size. Furthermore, counties may be classified as coldspots, despite relatively high prevalence. This could result in a county (such as Erath County, Texas), where observed prevalence is high, but it is classified as a coldspot due to all of its neighbors having very low prevalence. This is an inherent limitation to the clustering approach in that some of the counties identified may not meet all of the typical characteristics of the cluster. These relatively uncommon anomalies may be due to limited sample sizes or complex regional patterns that cannot be adequately captured with this approach.
Another important limitation of the present study is that it is unknown to what degree the county-level data are unreliable estimates. The BRFSS weighting variables do not apply at the county level, and samples at the county level cannot be assumed to be representative in all cases.
Other limitations of these analyses exist as well. For example, cross-sectional data collection precludes assessments of causality. Although it is likely that residence predates sleep disturbance, it is not possible to determine whether changing residence will alter sleep. Furthermore, the insufficient sleep survey item is limited in its clinical utility; as it is not diagnostic of any particular sleep disorder, it may or may not reflect sleep duration, and it assesses a construct that has not been thoroughly evaluated psychometrically. Therefore, conclusions should be interpreted with appropriate caution.
Conclusions
Overall, insufficient sleep was found to be differentially distributed among US counties, with several hotspots and coldspots identified. In particular, a prominent hotspot was found in an Appalachian region at the intersection of Kentucky, Tennessee, West Virginia, and Virginia, with that hotspot extending into parts of Ohio. These findings could be used by stakeholders, including members of the public and health authorities at the national, regional, and state levels, who could use these data to discern the public health burden of sleep disturbance relative to geography.
Acknowledgments
We also wish to thank the Centers for Disease Control and Prevention for collecting these data and making them available and the BRFSS participants.
Footnotes
Supported by the National Institute of Environmental Health Sciences (R21ES022931) and the Cartographic Modeling Lab at the University of Pennsylvania (Philadelphia, PA).
References
- 1.Colten HR, Altevogt BM Institute of Medicine Committee on Sleep Medicine and Research. Sleep disorders and sleep deprivation: an unmet public health problem. Washington, DC: Institute of Medicine: National Academies Press; 2006. [PubMed] [Google Scholar]
- 2.Grandner MA, Patel NP, Hale L, Moore M. Mortality associated with sleep duration: the evidence, the possible mechanisms, and the future. Sleep Med Rev. 2010;14:191–203. doi: 10.1016/j.smrv.2009.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grandner MA, Patel NP, Gehrman PR, Perlis ML, Pack AI. Problems associated with short sleep: bridging the gap between laboratory and epidemiological studies. Sleep Med Rev. 2010;14:239–247. doi: 10.1016/j.smrv.2009.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Knutson KL. Does inadequate sleep play a role in vulnerability to obesity? Am J Hum Biol. 2012;24(3):361–371. doi: 10.1002/ajhb.22219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Knutson KL. Sleep duration and cardiometabolic risk: a review of the epidemiologic evidence. Best Pract Res Clin Endocrinol Metab. 2010;24(5):731–743. doi: 10.1016/j.beem.2010.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Buxton OM, Marcelli E. Short and long sleep are positively associated with obesity, diabetes, hypertension, and cardiovascular disease among adults in the United States. Soc Sci Med. 2010;71(5):1027–1036. doi: 10.1016/j.socscimed.2010.05.041. [DOI] [PubMed] [Google Scholar]
- 7.Altman NG, Izci-Balserak B, Schopfer E, et al. Sleep duration versus sleep insufficiency as predictors of cardiometabolic health outcomes. Sleep Med. 2012;13(10):1261–1270. doi: 10.1016/j.sleep.2012.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Roth TC, II, Rattenborg NC, Pravosudov VV. The ecological relevance of sleep: the trade-off between sleep, memory and energy conservation. Philos Trans R Soc Lond B Biol Sci. 2010;365(1542):945–959. doi: 10.1098/rstb.2009.0209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grandner MA, Patel NP, Gehrman PR, et al. Who sleeps better? Socioeconomic differences in reports of sleep disturbance. Sleep. 2009;32:A422–A423. Abstract Supplement. [Google Scholar]
- 10.Park SE, Kim HM, Kim DH, Kim J, Cha BS, Kim DJ. The association between sleep duration and general and abdominal obesity in Koreans: data from the Korean National Health and Nutrition Examination Survey, 2001 and 2005. Obesity (Silver Spring) 2009;17(4):767–771. doi: 10.1038/oby.2008.586. [DOI] [PubMed] [Google Scholar]
- 11.Gangwisch JE, Heymsfield SB, Boden-Albala B, et al. Sleep duration as a risk factor for diabetes incidence in a large U.S. sample. Sleep. 2008;30(12):1667–1673. doi: 10.1093/sleep/30.12.1667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gangwisch JE, Malaspina D, Boden-Albala B, Heymsfield SB. Inadequate sleep as a risk factor for obesity: analyses of the NHANES I. Sleep. 2005;28(10):1289–1296. doi: 10.1093/sleep/28.10.1289. [DOI] [PubMed] [Google Scholar]
- 13.Hale L, Hill TD, Burdette AM. Does sleep quality mediate the association between neighborhood disorder and self-rated physical health? Prev Med. 2010;51(3–4):275–278. doi: 10.1016/j.ypmed.2010.06.017. [DOI] [PubMed] [Google Scholar]
- 14.Hill TD, Burdette AM, Hale L. Neighborhood disorder, sleep quality, and psychological distress: testing a model of structural amplification. Health Place. 2009;15(4):1006–1013. doi: 10.1016/j.healthplace.2009.04.001. [DOI] [PubMed] [Google Scholar]
- 15.Bird CE, Seeman T, Escarce JJ, et al. Neighbourhood socioeconomic status and biological “wear and tear” in a nationally representative sample of US adults. J Epidemiol Community Health. 2010;64(10):860–865. doi: 10.1136/jech.2008.084814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hale L, Do DP. Racial differences in self-reports of sleep duration in a population-based study. Sleep. 2007;30(9):1096–1103. doi: 10.1093/sleep/30.9.1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hale L, Do DP. Sleep and the inner city: how race and neighborhood context relate to sleep duration. Population Association of America Annual Meeting Program; 2006. [Google Scholar]
- 18.Centers for Disease Control. Overview: BRFSS 2009. Washington, DC: CDC; 2009. [Google Scholar]
- 19.Edinger JD, Wyatt JK, Stepanski EJ, et al. Testing the reliability and validity of DSM-IV-TR and ICSD-2 insomnia diagnoses. Results of a multitrait-multimethod analysis. Arch Gen Psychiatry. 2011;68(10):992–1002. doi: 10.1001/archgenpsychiatry.2011.64. [DOI] [PubMed] [Google Scholar]
- 20.Grandner MA, Jackson NJ, Pigeon WR, Gooneratne NS, Patel NP. State and regional prevalence of sleep disturbance and daytime fatigue. J Clin Sleep Med. 2012;8(1):77–86. doi: 10.5664/jcsm.1668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Grandner MA, Martin JL, Patel NP, et al. Age and sleep disturbances among american men and women: data from the U.S. behavioral risk factor surveillance system. Sleep. 2012;35(3):395–406. doi: 10.5665/sleep.1704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Grandner MA, Hale L, Jackson N, Patel NP, Gooneratne NS, Troxel WM. Perceived racial discrimination as an independent predictor of sleep disturbance and daytime fatigue. Behav Sleep Med. 2012;10(4):235–249. doi: 10.1080/15402002.2012.654548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Grandner MA, Patel NP, Perlis ML, et al. Obesity, diabetes, and exercise associated with sleep-related complaints in the American population. J Public Health. 2011;19(5):463–474. doi: 10.1007/s10389-011-0398-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Grandner MA, Patel NP, Gehrman PR, et al. Who gets the best sleep? Ethnic and socioeconomic factors related to sleep disturbance. Sleep Med. 2010;11:470–479. doi: 10.1016/j.sleep.2009.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Grandner MA, Jackson NJ, Pak VM, Gehrman PR. Sleep disturbance is associated with cardiovascular and metabolic disorders. J Sleep Res. 2012;21(4):427–433. doi: 10.1111/j.1365-2869.2011.00990.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Getis A, Ord JK. The analysis of spatial association by use of distance statistics. Geogr Anal. 1992;24(3):189–206. [Google Scholar]
- 27.Daly H. Simple SAS, macros for the calculation of exact binomial and poisson confidence limits. Comput Biol Med. 1992;22:351–361. doi: 10.1016/0010-4825(92)90023-g. [DOI] [PubMed] [Google Scholar]
- 28.Pancoska P, Buch S, Cecchetti A, et al. Family networks of obesity and type 2 diabetes in rural Appalachia. Clin Transl Sci. 2009;2(6):413–421. doi: 10.1111/j.1752-8062.2009.00162.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tessaro I, Smith SL, Rye S. Knowledge and perceptions of diabetes in an Appalachian population. Prev Chronic Dis. 2005;2(2):A13. [PMC free article] [PubMed] [Google Scholar]
- 30.Borak J, Salipante-Zaidel C, Slade MD, Fields CA. Mortality disparities in Appalachia: reassessment of major risk factors. J Occup Environ Med. 2012;54(2):146–156. doi: 10.1097/JOM.0b013e318246f395. [DOI] [PubMed] [Google Scholar]
- 31.Kariisa M, Seiber E. Distribution of cardiovascular disease and associated risk factors by county type and health insurance status: results from the 2008 Ohio Family Health Survey. Public Health Rep. 2015;130(1):87–95. doi: 10.1177/003335491513000111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Blackley D, Behringer B, Zheng S. Cancer mortality rates in Appalachia: descriptive epidemiology and an approach to explaining differences in outcomes. J Community Health. 2012;37(4):804–813. doi: 10.1007/s10900-011-9514-z. [DOI] [PubMed] [Google Scholar]
- 33.Hendryx M, O’Donnell K, Horn K. Lung cancer mortality is elevated in coal-mining areas of Appalachia. Lung Cancer. 2008;62(1):1–7. doi: 10.1016/j.lungcan.2008.02.004. [DOI] [PubMed] [Google Scholar]
- 34.Wade WA, Petsonk EL, Young B, Mogri I. Severe occupational pneumoconiosis among West Virginian coal miners: one hundred thirty-eight cases of progressive massive fibrosis compensated between 2000 and 2009. Chest. 2011;139(6):1458–1462. doi: 10.1378/chest.10-1326. [DOI] [PubMed] [Google Scholar]
- 35.Casto BC, Sharma S, Fisher JL, Knobloch TJ, Agrawal A, Weghorst CM. Oral cancer in Appalachia. J Health Care Poor Underserved. 2009;20(1):274–285. doi: 10.1353/hpu.0.0097. [DOI] [PubMed] [Google Scholar]
- 36.Halverson JA, Bischak G. Underlying socioeconomic factors influencing health disparities in the Appalachian region. Morgantown, WV: Mary Babb Randolph Cancer Center, West Virginia University; 2008. [Google Scholar]
- 37.Grandner MA, Chakravorty S, Perlis ML, Oliver L, Gurubhagavatula I. Habitual sleep duration associated with self-reported and objectively determined cardiometabolic risk factors. Sleep Med. 2014;15(1):42–50. doi: 10.1016/j.sleep.2013.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Grandner MA. Addressing sleep disturbances: an opportunity to prevent cardiometabolic disease? Int Rev Psychiatry. 2014;26(2):155–176. doi: 10.3109/09540261.2014.911148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.McKnight-Eily LR, Liu Y, Perry GS, et al. Perceived insufficient rest or sleep among adults—United States, 2008. MMWR Morb Mortal Wkly Rep. 2009;58(42):1175–1179. [PubMed] [Google Scholar]