Abstract
Pressure injuries are an accepted complication of prone positioning during the neurosurgical procedures. Horseshoe headrest are intended to reduce the incidence and severity of such injuries by allowing limited areas of contact between the skin of dependent areas of contact and the supporting surfaces. We report a case where a patient positioned prone over a horseshoe headrest developed inadvertent unilateral facial pressure injuries following a 6-h long craniovertebral junction (CVJ) surgery. We attempt to highlight this complication, analyze its causation, and briefly review the existing literature related to similar reported injuries.
Keywords: Craniovertebral junction (CVJ), dependent contact point, horseshoe headrest, pressure injuries, prone position
INTRODUCTION
Prone positioning aids in optimum exposure and access during craniovertebral junction (CVJ) surgeries. Consequently, complications, such as cardiovascular instability, raised airway pressures, neurovascular injuries, and pressure injuries, can occur.[1] A horseshoe headrest having cushioned pad base and multipositioning capabilities to support the forehead and cheeks is often employed. Focal pressure and consequent pressure necrosis is thus avoided.[2] We describe a case where a patient placed prone over horseshoe headrest developed unilateral facial injuries following CVJ surgery extending for a considerable duration and endeavor to explain the causation of these injuries. Written and informed consent was obtained from the patient prior to reporting this event.
CASE REPORT
A 40-year-old female patient [American Society of Anesthesiology Patient Classification (ASA) I] with atlantoaxial dislocation (AAD) was posted for posterior fixation. After administering general anesthesia, she was positioned prone on horseshoe headrest. The horseshoe headrest was further cushioned using two layers of cotton padding overlapped with gauze. Gardner–Wells cervical traction was applied to provide axial traction and maintain head neutrality. After positioning, the contact areas were confirmed to be appropriately padded and the eyes were verified to be pressure free. Following 6 h of uneventful surgery where occipitocervical fusion with occipital plate, C-2 transpedicle screws, and C-4 lateral mass screws were placed, the patient was turned supine for reversal and extubation. At this point, it was revealed that the patient had developed skin excoriation (1.5 × 1.5 cm) size over her left maxilla [Figure 1]. Hyperpigmented areas had developed over left infra and lateral orbital regions signifying deep tissue injury [Figure 1]. A significant headrest impression was found over the left forehead [Figure 1]. However, the right-sided dependent regions were free from any injuries. The injuries appeared pressure generated and were not due to chemical or cautery burns. Pupillary examination was done postextubation that showed bilaterally reacting and symmetrical pupils. Nevertheless, an urgent ophthalmology consultation was sought to rule out any ocular compromise that fortunately had not occurred. Antibiotic ointment was applied locally over maxillary abrasions. The injuries and especially their unilateral distribution, prompted us to identify their genesis and we reviewed the patient's radiographs. Minute analysis of the radiographs revealed that the along with atlantoaxial dislocation (AAD), the patient also had an asymmetrical joint between the first and second cervical vertebrae (C1-C2 joint). Due to axial asymmetry, a trivial lateral neck tilt was evident on the radiographs [Figures 2 and 3]. The manifestation of this tilt was however not apparent clinically. Although neck neutrality along the horizontal axis was sustained using axial traction following positioning, the lateral tilt was not negated and remained as such. Subsequently, the head had remained positioned with slight left-sided tilt throughout the procedure. The bony prominences on the left side therefore bore comparatively higher degrees of pressure for a significant period and the injuries resulted. Next day, significant periorbital edema had developed resulting from wounds leading to closure of the left eye [Figure 4]. She was prescribed oral serratiopeptidase, anti-inflammatory analgesics, and local antibiotic ointment. The periorbital swelling progressively resolved in 2 days, and the wounds healed in 2 weeks after which she was discharged.
Figure 1.

Skin excoriation over the maxilla, hyperpigmentation in the periorbital region, and headrest impression over the forehead (left sided) following supine positioning
Figure 2.
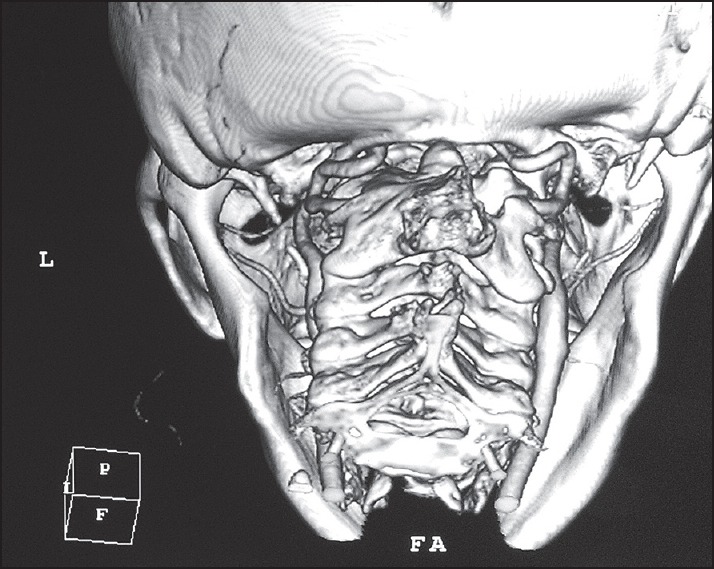
Coronal view MRI (T2 weighted) showing C1-C2 joint asymmetry with subaxial spine scoliosis
Figure 3.
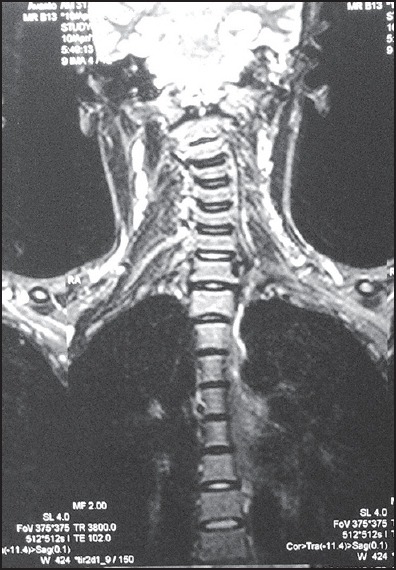
3D CT of craniovertebral junction showing joint asymmetry with mild lateral tilt
Figure 4.

Periorbital edema leading to the closure of the left eye
DISCUSSION
Prone positioning can injure skin of dependent contact points with severity of injuries rising proportionately with contact duration. The European Pressure Ulcer Advisory Panel (EUPAP) and the National Pressure Ulcer Advisory Panel (NPUAP) have defined pressure ulcers as localized injury to the skin and/or underlying tissue usually over a bony prominence, as a result of pressure, or pressure in combination with shear.[3] Factors implicated in generating pressure injuries are surgical duration, pressure intensity, shearing or frictional force, age, diabetes, peripheral vascular diseases, chronic low blood pressure (local tissue anoxia), and poor nutrition (reduced skin turgor).[4] Warming blankets (producing heat and moisture leading to skin breakdown) and inability to continuously check inaccessible dependent areas are additional reasons. In our patient, when the initial position check was undertaken, the alignment of the head was apparently neutral. However, due to the inherent left-sided lateral deviation of the CVJ, slight leftward tilt persisted. This disparity was not counterbalanced during the positioning with extra support beneath the deviated side. Subtle readjustments in the headrest's position were also made prior to sterile preparations. Probably these changes exaggerated the near neutral alignment of headrest to one where left side of face got placed slightly lower than the right side. Intermittent pressures transmitted during surgical opening and manipulation of the joint further aggravated the pressure over dependent contact regions. Due to higher weight (consequently higher pressures) that the bony prominences of left-sided dependent regions were subjected to for a significant period (6 h), the injuries occurred. Axial traction of patient's head possibly redistributed the gravity-induced (vertical) pressure between horseshoe and the facial skin increasing the surface shearing forces. Additionally, cotton pads overlapped with gauze could have contributed to the injury as compared to a uniform surface (gel pads, sponge, etc.), irregular surface of gauze is more likely to induce abrasions/pressure injuries. While exploring the literature for related complications, we came across a similar report where a patient developed pressure sores over both the malar and periorbital regions from horseshoe headrest.[5] Authors attributed these injuries to their preoccupation with avoiding pressure over eyeballs. Intermittent pressures transmitted during surgical manipulations were also blamed. A case of allergic “contact dermatitis” has been reported with the face placed over the PronePositioner™ (Voss Medical Products Inc., San Antonio, TX).[6] Alopecia in the shape of a horseshoe headrest has also been reported following the lengthy surgery.[7]
The frequency of reporting pressure injuries in prone position is low due to the theoretical likelihood of avoiding such complications by meticulous preparation or given that pressure injuries are regarded as a “recognized hazard,” documentations of such injuries is relatively meager.[1] Nonetheless, utmost care should be taken whenever prone positioning during surgical procedures is employed. Especially those cases where pathology lies in the CVJ, they merit meticulous review of radiographs to exclude any associated scoliosis prior to prone positioning. A previous investigation has reported a 35% incidence of associated kyphoscoliosis in patients with nonsyndromic AAD.[8] Higher concern is required in certain patients of CVJ anomalies particularly those with associated neck tilt, asymmetry at C1-C2, or in whom higher degree of manipulation is anticipated. If detected preoperatively, the contact zones of the affected side should be padded extra to compensate the lateral alignment imbalance. Slight modifications of horseshoe headrest may be done after proper explanation and communication with neurosurgeons. Manufacturers are also appealed to design improvised headrests with better compliance, adaptability according to the anatomic variations, and superior tissue compatibility.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflict of interest
There are no conflicts of interest.
REFERENCES
- 1.Edgcombe H, Carter K, Yarrow S. Anesthesia in the prone position. Br J Anaesth. 2008;100:165–83. doi: 10.1093/bja/aem380. [DOI] [PubMed] [Google Scholar]
- 2.Balakrishnan C, Pane TA. Use of the Mayfield horseshoe headrest for management of burns of the neck. Can J Plast Surg. 2005;13:83–4. doi: 10.1177/229255030501300204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Washington DC: National Pressure Ulcer Advisory Panel; 2009. European Pressure Ulcer Advisory Panel and National Pressure Ulcer Advisory Panel. Treatment of pressure ulcers: Quick Reference Guide; p. 5. [Google Scholar]
- 4.Woodward M. Risk factors for pressure ulcers — Can they withstand the pressure? Prim Intent. 1999:52–61. [Google Scholar]
- 5.Jain V, Bithal PK, Rath GP. Pressure sore on malar prominences by horseshoe headrest in prone position. Anaesth Intensive Care. 2007;35:304–5. [PubMed] [Google Scholar]
- 6.Jericho BG, Skaria GP. Contact dermatitis after the use of the PronePositioner. Anesth Analg. 2003;97:1706–8. doi: 10.1213/01.ANE.0000087061.76236.92. [DOI] [PubMed] [Google Scholar]
- 7.Bruce IA, Simmons MA, Hampal S. ‘Horseshoe-shaped’ post-operative alopecia following lengthy head and neck surgery. J Laryngol Otol. 2002;116:230–2. doi: 10.1258/0022215021910429. [DOI] [PubMed] [Google Scholar]
- 8.Sardhara J, Behari S, Jaiswal AK, Srivastava A, Sahu RN, Mehrotra A, et al. Syndromic versus nonsyndromic atlantoaxial dislocation: Do clinico-radiological differences have a bearing on management? Acta Neurochir (Wien) 2013;155:1157–67. doi: 10.1007/s00701-013-1717-x. [DOI] [PubMed] [Google Scholar]


