Abstract
The potential benefit of technology to enhance recovery after central nervous system injuries is an area of increasing interest and exploration. The primary emphasis to date has been motor recovery/augmentation and communication. This paper introduces two original studies to demonstrate how advanced technology may be integrated into subacute rehabilitation. The first study addresses the feasibility of brain computer interface with patients on an inpatient spinal cord injury unit. The second study explores the validity of two virtual environments with acquired brain injury as part of an intensive outpatient neurorehabilitation program. These preliminary studies support the feasibility of advanced technologies in the subacute stage of neurorehabilitation. These modalities were well tolerated by participants and could be incorporated into patients' inpatient and outpatient rehabilitation regimens without schedule disruptions. This paper expands the limited literature base regarding the use of advanced technologies in the early stages of recovery for neurorehabilitation populations and speaks favorably to the potential integration of brain computer interface and virtual reality technologies as part of a multidisciplinary treatment program.
The yearly incidence of traumatic brain injury (TBI) (∼1.7 million), acquired brain injury (∼900,000), and spinal cord injury (SCI) (∼12,000) in the US fails to adequately reflect the long-term impact and annual societal cost, which may exceed $100 billion a year (1–5). As advances in medical care are improving survival rates in these populations, the need for a multidisciplinary approach focusing on long-term outcomes, secondary complications, and quality of life is magnified (3, 6). This multidisciplinary approach strongly aligns with key aspects of the World Health Organization's International Classification of Functioning, Disability, and Health Model, where the primary health conditions must be conceptualized in relation to environmental and contextual factors with emphasis upon improving function (7) (Figure 1). Advanced technologies such as brain computer interface (BCI), which uses brain patterns to help patients bypass injuries that impede motor or verbal responses, and virtual reality (VR) have shown potential as viable treatment tools in the rehabilitation setting (8–11); however, the application of advanced technologies in neurorehabilitation is not systematic, and studies to support their use in clinical settings remain limited (12–14). This prompted our group to begin exploratory studies into the feasibility and utility of off-the-shelf BCI and VR technologies with neurorehabilitation populations. This paper introduces two original studies to demonstrate how advanced technology may be integrated into the subacute phase of central nervous system recovery. Approval to complete the studies was obtained from the hospital's institutional review board.
Figure 1.
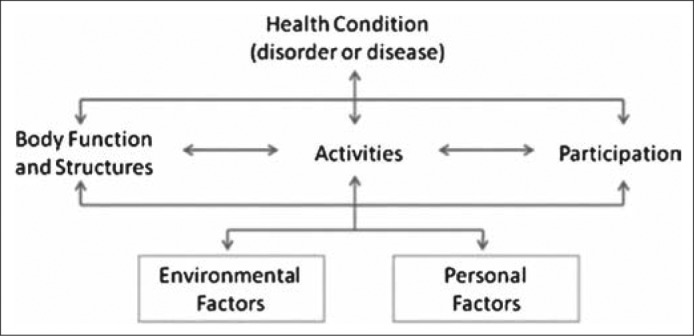
The International Classification of Functioning, Disability, and Health model. Source: World Health Organization (7).
FEASIBILITY STUDY AND PILOT STUDY
On the SCI rehabilitation treatment unit at the Baylor Institute for Rehabilitation, 25 medically stable patients without severe cognitive or psychiatric impairment were included in the first study. Most participants had sustained cervical-level (48%) or thoracic-level (44%) SCIs and had residual tetraplegia (52%). At initial contact, an extensive screening was completed, including neuropsychological tests, formal questionnaires of mood, pain, and physical status, and qualitative, study-specific questions. Select measures were repeated immediately before the off-the-shelf BCI paradigm and at the final contact. The BCI paradigm involved a cube rotation task using the EPOC headset (Emotiv, San Francisco, CA). This device was originally developed for gaming, but has been increasingly used in research studies (15–17). Although this off-the shelf BCI is less sensitive in its capture of electroencephalographic data when compared with traditional medical devices (18), its portability, ease of use, and cost made it an attractive option for an inpatient hospital setting. This device allows for wireless 14-channel electroencephalographic recording based on the international 10 to 20 locations (AF3, F7, F3, FC5, T7, P7, O1, O2, P8, T8, FC6, F4, F8, AF4) along with two reference electrodes (P3, P4).
After a brief training session for each increasingly complex BCI task (push cube, move left, move right, and cube disappearance), each participant performed three trials, lasting 8 seconds each. A MATLAB scoring program was employed for data acquisition, to log stimulus presentation, and for psychophysiological monitoring (19). The results of the feasibility study suggested that the technology was easily learned (92% of trials were successful) and mastery of the paradigm was not significantly related to prior technology proficiency, current cognitive functioning, pain level, or emotional distress. Equally important, the participants enjoyed the experience and had no reported adverse effects from the headset. The encouraging findings of the small feasibility study open the door for future work among inpatient SCI populations during rehabilitation. This is an ideal time to provide initial exposure and training for such technology if clinical paradigms can be developed. The daunting next step entails the development of paradigms specific to SCI treatment targets.
On our SCI treatment team, key psychological treatment goals revolve around psychological adjustment, pain management, and educational interventions that often incorporate aspects of social skills training. Future use of BCI paradigms will be dependent on the ability to integrate VR paradigms that are linked to this triad of clinical priorities. Of particular interest within the rehabilitation psychology field is programming based on frequent challenges and emotionally laden scenarios after SCI. These scenarios could touch upon addressing disability with family/friends, navigating public areas with limited access, and addressing intimacy concerns. One could envision a preventive approach using virtual social simulations to promote more adaptive skills in early stages of rehabilitation. BCI could also be linked to biofeedback-like paradigms to further address pain, anxiety, and emotional regulation, which can complicate outcomes after SCI.
The emphasis on clinically relevant and generalizable treatment environments may be in part addressed via immersive environments. A second pilot study was conducted to validate the cognitive rehabilitation efficacy of two virtual environments following central nervous system insult. Participants included individuals with acquired TBI, stroke, brain neoplasm, and anoxic injury. A key focus was treatment outcomes associated with VR training of specific executive functions: cognitive flexibility, working memory, complex attentional processes, and cognitive and motor inhibition, in addition to processing speed.
Individuals who consented to participate in this study were enrolled in a multidisciplinary outpatient day neurorehabilitation program at the Baylor Institute for Rehabilitation. The only deviation in programming was the introduction of the two VR programs as a supplementary cognitive rehabilitation intervention. The laptop-presented virtual apartment (ClinicaVR: Apartment Stroop [20]) and virtual classroom settings (VR Classroom [21–24]) were selected because they simulate demands and distractions found in real-world settings. While in the immersive environments, participants performed two conditions of a response inhibition task in the face of distractions. Task difficulty increased across sessions with respect to the quantity and type of distractions the participant was exposed to, with a total of 8 training sessions completed biweekly (4-week treatment duration). A Z800 3DVisor head-mounted display (HMD) was used to create a 3D-like effect, and the built in 3-axis head-tracker allowed patients to look 360 degrees around themselves by turning their head.
During baseline testing (session 1) and the final session (session 8), patients were additionally administered the Automated Neuropsychological Assessment Metrics Stroop and Go-No Go computerized tests, Woodcock-Johnson 3rd Edition Pair Cancellation subtest, and Delis-Kaplan Executive Functions System Color-Word Interference test (25–27). These tests were used to compare VR treatment outcomes with performance on unimodal Stroop/executive testing and paper-pencil tests. Patients also completed the Simulator Sickness Questionnaire upon conclusion of sessions 1 and 8 to document any symptoms associated with the HMD.
Twenty-one brain injury patients participated in the pilot study: 9 diagnosed with stroke (43%), 6 with TBI (29%), 2 with anoxic injury (10%), 3 with brain tumor (14%), and 1 with amyloid angiopathy (5%). Preliminary analyses were conducted using the performance of the group with stroke, which accounted for the largest diagnostic category. The smaller groups comprising patients with anoxic injury and brain tumor demonstrated such profound variability that a combined analysis would have been minimally informative. When comparing the stroke subgroup with 9 demographically matched healthy controls on the ClinicaVR: Apartment Stroop, there were no significant group differences in reaction time on conditions with distractions (F(1,16) 3.418, P = 0.062) or without distractions (F(1,16) 1.793, P = 0.200) employing analysis of covariance and adjusting for age. However, response time was significantly slower for stroke patients than for controls (F(1,16) 17.109, P < .01). The former may be due to the fact that the stroke subgroup included some relatively young patients, ranging in age from 22 to 65 (mean age = 47). It may also be that the stroke group was relatively higher functioning cognitively, given that patients with significantly impaired comprehension, bimanual apraxia, and attention (e.g., patients with attention span < 10 minutes) that could potentially confound cognitive performance outcomes on the VR programs were excluded from the study. However, two of the stroke patients were noted to respond with errors on all items of the incongruent word-color stimulus trial of the Stroop task, indicating variation in severity level within this group.
Qualitatively, across all acquired brain injury patient groups treated in this pilot study (TBI, stroke, anoxic injury, etc.), those exhibiting overt impulsivity or anxiety appeared to exhibit impulsive responding on the VR-based executive measures. Patients with reported or observable fatigue demonstrated reduced attention and self-monitoring, committing omission errors due to fluctuations in engagement. As additional quantitative error analysis is completed, it will be interesting to learn whether results parallel qualitative observations.
Six of the 21 patients initially endorsed slight or moderate fatigue, headache, eye strain, difficulty focusing, perspiring, and blurred vision on the Simulator Sickness Questionnaire, which assesses the occurrence, nature, and severity of sickness symptoms induced by virtual environments (28). By the fourth session, the number of patients reporting HMD-related symptoms declined to four. No adverse events occurred, and no patients volitionally withdrew from the study. Six of the 21 patients partially completed the study, but failed to complete all 8 intervention sessions. Two patients were medically withdrawn from the day neurorehabilitation program due to refractory medical complications, two patients self-discharged from the program against medical advice, and four patients' rehabilitation regimens were concluded prior to their projected discharge dates when insurance or state-assisted benefits were not extended.
With regard to feasibility, similar to the BCI apparatus described above, the portability, ease of use, and cost of the devices used to administer the VR programs made them amenable to this setting. Scheduling of the VR intervention sessions and space required constant and effective communication between the research team and the day neurorehabilitation teams, due to the variability in patient schedules, modifications in length of stay, and unplanned events (e.g., illness, external medical appointments, impact of payer source on rehabilitation days). The day neurorehabilitation team was positively responsive to integration of the VR intervention in the rehabilitation program. Due to built-in demonstrations paired with verbal instructions from the research team members administering the VR interventions, patients found the technology user-friendly. Some patients provided unsolicited feedback, stating that the virtual environments and internal distractions in the programs were realistic. In fact, patients spontaneously commented on the improvement in their performance from initial to later sessions. One patient specifically attributed an observable subjective improvement in reaction time to the VR intervention.
The efforts to replicate home and school settings using VR in the pilot study allow for potentially highly relevant information to guide discharge planning. It is hoped that findings from this pilot study will encourage ongoing study to validate VR technologies in neurological populations for the purpose of enhancing cognitive intervention and rehabilitation.
CHALLENGES IN TECHNOLOGY APPLICATION
The preliminary studies presented herein represent initial attempts to explore the feasibility and potential benefit of VR and BCI technologies. The ease of training and positive participant response with VR and BCI paradigms, along with the lack of adverse effects even with patients in the subacute stage of recovery, were quite encouraging. Still, the clear enthusiasm for technology must be tempered by an acknowledgment of potential barriers. The key concerns involve issues surrounding the utility of BCI and VR, management of technological problems, and financial feasibility. The virtual environments used in these pilot studies are not commercially available, and only a few research labs have access to them. Further, a number of VR systems use arrays of screens to allow for full-body interactions, costing many thousands of dollars. From a utility standpoint, our projects ranged from simple visual stimuli to more advanced depictions of real-world settings. Still, there may be a need for more realistic visual paradigms. Studies are needed to assess the impact and potential clinical efficacy of varying levels of stimulus fidelity and immersion.
Our studies involved collaboration with experts in the area of technology and psychology who could provide any needed assistance in a timely manner. The presence of an information technology support staff was also readily available as part of our hospital system. Still, occasions arose where technology did not work properly, resulting in delayed intervention or the need to reschedule. Such complications speak to the challenges of implementing interventions dependent upon technology within inpatient and outpatient rehabilitation settings. Any delays in these fast-paced settings, requiring the coordination of various disciplines, can be quite disruptive to the milieu.
Finally, the financial feasibility of VR and BCI will largely be determined by future outcomes research. Unless there is support for clinical gain in the form of improved outcomes, decreased complications, or secondary decline in medical costs (e.g., decreased length of stay, less use of future medical services), cost concerns may prohibit adoption of such technologies. Mainstream implementation in rehabilitation would be a financial challenge considering the trend of declining reimbursement for clinical services and emphasis on bundled services with recent health care changes. The initial cost must be coupled with the need for staff training and statistician support by individuals trained to analyze the data formats associated with this technology. Additionally, BCI and VR require a private space that limits distractions that are all too frequent in rehabilitation settings. Private rooms or dedicated areas for such interventions would be ideal, yet allocation of such space was a challenge in our studies.
Acknowledgments
The authors would like to thank Anne Carlew, BS, Erin Sullivan, MS, and Jesse Smotherman, BS, for their assistance with data collection and the rehabilitation therapy teams of Baylor Institute for Rehabilitation's spinal cord team and day neurorehabilitation program for their coordination efforts. We greatly appreciate Digital Media Works for use of its VR programs.
References
- 1.Brain Injury Association of America. Brain injury statistics. Available at http://www.biausa.org/LiteratureRetrieve.aspx?ID=104992; accessed January 14, 2016.
- 2.Centers for Disease Control and Prevention. Injury Prevention & Control: Traumatic Brain Injury. Available at http://www.cdc.gov/traumaticbraininjury/; accessed February 4, 2014.
- 3.Jackson D, McCrone P, Mosweu I, Siegert R, Turner-Stokes L. Service use and costs for people with long-term neurological conditions in the first year following discharge from in-patient neuro-rehabilitation: a longitudinal cohort study. PLoS One. 2014;9(11):e113056. doi: 10.1371/journal.pone.0113056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mahabaleshwarkar R, Khanna R. National hospitalization burden associated with spinal cord injuries in the United States. Spinal Cord. 2014;52(2):139–144. doi: 10.1038/sc.2013.144. [DOI] [PubMed] [Google Scholar]
- 5.Wyndaele M, Wyndaele JJ. Incidence, prevalence and epidemiology of spinal cord injury: what learns a worldwide literature survey? Spinal Cord. 2006;44(9):523–529. doi: 10.1038/sj.sc.3101893. [DOI] [PubMed] [Google Scholar]
- 6.Tate DG, Kalpakjian CZ, Forchheimer MB. Quality of life issues in individuals with spinal cord injury. Arch Phys Med Rehabil. 2002;83(12, Suppl 2):S18–S25. doi: 10.1053/apmr.2002.36835. [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization. How to Use the ICF: A Practical Manual for Using the International Classification of Functioning, Disability and Health (ICF) Geneva, Switzerland: WHO; 2013. pp. 1–127. [Google Scholar]
- 8.Astrand E, Wardak C, Ben Hamed S. Selective visual attention to drive cognitive brain-machine interfaces: from concepts to neurofeedback and rehabilitation applications. Front Syst Neurosci. 2014;8:144. doi: 10.3389/fnsys.2014.00144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Larson EB, Feigon M, Gagliardo P, Dvorkin AY. Virtual reality and cognitive rehabilitation: a review of current outcome research. NeuroRehabilitation. 2014;34(4):759–772. doi: 10.3233/NRE-141078. [DOI] [PubMed] [Google Scholar]
- 10.Rábago CA, Wilken JM. Application of a mild traumatic brain injury rehabilitation program in a virtual realty environment: a case study. J Neurol Phys Ther. 2011;35(4):185–193. doi: 10.1097/NPT.0b013e318235d7e6. [DOI] [PubMed] [Google Scholar]
- 11.Tankus A, Fried I, Shoham S. Cognitive-motor brain-machine interfaces. J Physiol Paris. 2014;108(1):38–44. doi: 10.1016/j.jphysparis.2013.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Enzinger C, Ropele S, Fazekas F, Loitfelder M, Gorani F, Seifert T, Reiter G, Neuper C, Pfurtscheller G, Muller-Putz G. Brain motor system function in a patient with complete spinal cord injury following extensive brain-computer interface training. Exp Brain Res. 2008;190(2):215–223. doi: 10.1007/s00221-008-1465-y. [DOI] [PubMed] [Google Scholar]
- 13.Kaufmann T, Holz EM, Kübler A. Comparison of tactile, auditory, and visual modality for brain-computer interface use: a case study with a patient in the locked-in state. Front Neurosci. 2013;7:129. doi: 10.3389/fnins.2013.00129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kiper P, Agostini M, Luque-Moreno C, Tonin P, Turolla A. Reinforced feedback in virtual environment for rehabilitation of upper extremity dysfunction after stroke: preliminary data from a randomized controlled trial. BioMed Res Int. 2014;2014:752128. doi: 10.1155/2014/752128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Badcock NA, Mousikou P, Mahajan Y, de Lissa P, Thie J, McArthur G. Validation of the Emotiv EPOCR EEG gaming system for measuring research quality auditory ERPs. Peer J. 2013;1:e38. doi: 10.7717/peerj.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dutta A, Kumar R, Malhotra S, Chugh S, Banerjee A, Dutta A. A low-cost point-of-care testing system for psychomotor symptoms of depression affecting standing balance: a preliminary study in India. Depress Res Treat. 2013;2013:640861. doi: 10.1155/2013/640861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pham T, Tran D. Emotional recognition using the Emotiv EPOC device. Neural Information Processing. 19th International Conference, ICONIP 2012, Doha, Qatar, November 12–15, 2012, Proceedings, Part V. 2012. pp. 394–399.
- 18.Duvinage M, Castermans T, Petieau M, Hoellinger T, Cheron G, Dutoit T. Performance of the Emotiv EPOC headset for P300-based applications. Biomed Eng Online. 2013;12(1):56. doi: 10.1186/1475-925X-12-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McMahan T, Parberry I, Parsons TD. Modality specific assessment of video game player's experience using the Emotiv entertainment computing. Entertain Comput. 2015;7:1–6. [Google Scholar]
- 20.Henry M, Joyal CC, Nolin P. Development and initial assessment of a new paradigm for assessing cognitive and motor inhibition: the bimodal virtual-reality Stroop. J Neurosci Methods. 2012;210(2):125–131. doi: 10.1016/j.jneumeth.2012.07.025. [DOI] [PubMed] [Google Scholar]
- 21.Adams R, Finn P, Moes E, Flannery K, Rizzo AS. Distractibility in attention deficit/hyperactivity disorder (ADHD): the virtual reality classroom. Child Neuropsychol. 2009;15(2):120–135. doi: 10.1080/09297040802169077. [DOI] [PubMed] [Google Scholar]
- 22.Nolin P, Stipanicic A, Henry M, Joyal CC, Allain P. Virtual reality as a screening tool for sports concussion in adolescents. Brain Inj. 2012;26(13–14):1564–1573. doi: 10.3109/02699052.2012.698359. [DOI] [PubMed] [Google Scholar]
- 23.Parsons TD, Bowerly T, Buckwalter JG, Rizzo AA. A controlled clinical comparison of attention performance in children with ADHD in a virtual reality classroom compared to standard neuropsychological methods. Child Neuropsychol. 2007;13(4):363–381. doi: 10.1080/13825580600943473. [DOI] [PubMed] [Google Scholar]
- 24.Pollak Y, Weiss PL, Rizzo AA, Weizer M, Shriki L, Shalev RS, Gross-Tsur V. The utility of a continuous performance test embedded in virtual reality in measuring ADHD-related deficits. J Dev Behav Pediatr. 2009;30(1):2–6. doi: 10.1097/DBP.0b013e3181969b22. [DOI] [PubMed] [Google Scholar]
- 25.Delis DC, Kaplan E, Kramer JH. Delis Kaplan Executive Function System (D-KEFS) San Antonio, TX: The Psychological Corporation; 2001. [Google Scholar]
- 26.Schrank FA, McGrew KS, Woodcock RW. Technical Abstract (Woodcock-Johnson III Assessment Service Bulletin No. 2) Itasca, IL: Riverside Publishing; 2001. [Google Scholar]
- 27.Woodhouse J, Heyanka DJ, Scott J, Vincent A, Roebuck-Spencer T, Domboski-Davidson K, O'Mahar K, Adams R. Efficacy of the ANAM General Neuropsychological Screening Battery (ANAM GNS) for detecting neurocognitive impairment in a mixed clinical sample. Clin Neuropsychol. 2013;27(3):376–385. doi: 10.1080/13854046.2012.762427. [DOI] [PubMed] [Google Scholar]
- 28.Kennedy RS, Lane NE, Berbaum KS, Lilienthal MG. An enhanced method for quantifying simulator sickness. Int J Aviat Psychol. 1993;3(3):203–220. [Google Scholar]


