Abstract
We present a patient who had rheumatoid meningitis while on infliximab, a tumor necrosis factor alpha (TNF-α) inhibitor, which initially presented as transient ischemic attacks. Although our patient had been stable on infliximab for several years, her neurologic symptoms improved when her infliximab was held due to active infection and then recurred after reinitiation of therapy. Rheumatoid meningitis is exceedingly rare; however, there have been several other reports of rheumatoid meningitis developing in patients on TNF-α inhibitor therapy.
Rheumatoid meningitis is an exceedingly rare manifestation of rheumatoid arthritis (1). Though it is uncommon, there are several case reports of rheumatoid meningitis developing in patients on tumor necrosis alpha (TNF-α) inhibitor therapy (2–5). Our case is unique in that our patient's neurologic symptoms improved when infliximab, a TNF-α inhibitor, was held due to active infection and resumed following reinitiation of therapy.
CASE DESCRIPTION
A 66-year-old woman with hypertension, coronary artery disease, gastroesophageal reflux, and rheumatoid arthritis on infliximab for 12 years developed acute-onset expressive aphasia in late January 2014. The episode reportedly lasted around 30 minutes and resolved without intervention. She presented to her local emergency department at that time and was diagnosed with a transient ischemic attack after a noncontrast computed tomography scan of the head was negative. Three days later, she had another episode of expressive aphasia and was again diagnosed with a transient ischemic attack. Following her second episode, ultrasound disclosed left carotid stenosis prompting a left carotid endarterectomy.
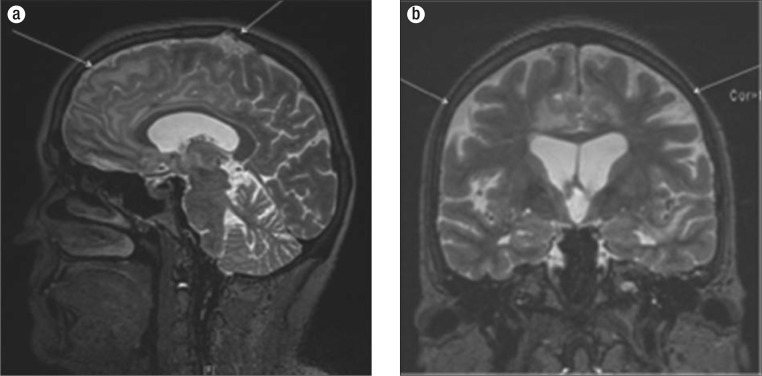
She also developed a right corneal abrasion which developed into dendritic keratitis followed by infections with Staphylococcus epidermidis and yeast. The infliximab was discontinued in February 2014 prior to having a deceased-donor corneal transplant in April 2014. Following her carotid endarterectomy and corneal transplant, her neurologic symptoms and right eye infection appeared to resolve, and she was started on infliximab and methotrexate in June 2014. After resuming infliximab, she noted intermittent episodes of lower-extremity numbness and tingling. Several months later, she developed a third episode of expressive aphasia, prompting hospitalization. On admission, her infliximab was held and magnetic resonance imaging (MRI) of the brain illustrated abnormal T2/FLAIR signal intensity in her bilateral frontal lobes and anterior temporal lobe with leptomeningeal enhancement (Figure 1). Notably, she was not taking nonsteroidal antiinflammatory medications or oral steroids prior to admission. A lumbar puncture illustrated 213 white blood cells, 86% lymphocytes, protein 85.9 g/dL, and glucose 41 mg/dL. She was started on empiric acyclovir for herpes simplex encephalitis.
Figure 1.
MRI of the brain with gadolinium T2/FLAIR. (a) Sagittal image illustrating enhancement of the leptomeninges and frontal lobe. (b) Coronal image illustrating abnormal enhancement.
Her clinical status continued to decline, and she developed headache, nausea, vomiting, altered mental status, urinary incontinence, and intermittent bilateral lower-extremity numbness and paralysis over the next several days. Herpes simplex polymerase chain reaction from her cerebrospinal fluid (CSF) was negative, and a repeat MRI of the brain illustrated interval worsening of her abnormal T2/FLAIR signal intensity.
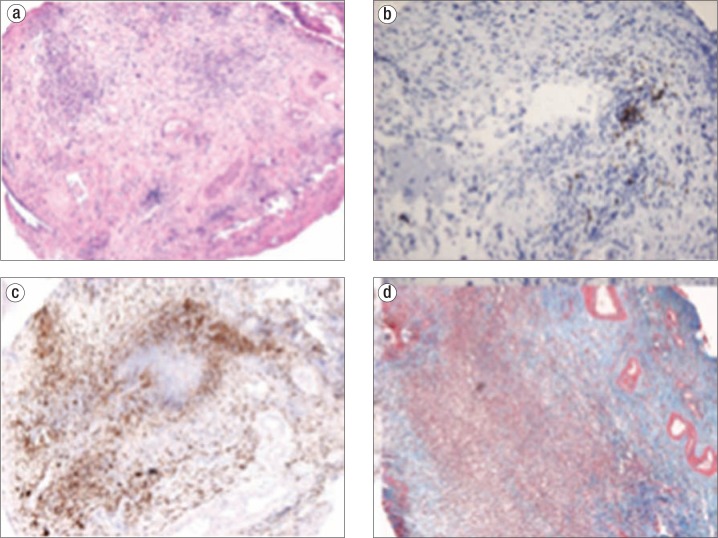
An electroencephalogram illustrated rare sharp waves over the left temporal region consistent with focal seizure disorder, and she was loaded on levetiracetam. Serologic studies illustrated a positive antinuclear antibody, rheumatoid factor, and anti-citrullinated protein antibody with negative double-stranded DNA antibody and normal serum complement levels. Repeat lumbar puncture again illustrated a lymphocytic pleocytosis, with 216 white blood cells, 87% lymphocytes, protein 44 g/dL, and glucose 63 mg/dL. An extensive infectious, neoplastic, and autoimmune analysis of her CSF was unremarkable apart from an elevated rheumatoid factor. Brain biopsy of the dura and cerebral cortex illustrated abundant T lymphocytes and macrophages, with a small number of B lymphocytes and IgG4-positive cells consistent with hypertrophic pachymeningitis (Figure 2). She was treated with 1000 mg intravenous methylprednisolone daily for 6 days with rapid improvement of her neurologic symptoms. She ultimately made a full neurologic recovery and was discharged on 50 mg prednisone daily.
Figure 2.
Brain biopsy findings suggesting a diagnosis of hypertrophic pachymeningitis. (a) Hematoxylin and eosin stain showing edematous cortex with attached chronically inflamed fibrous dura mater. (b) CD20 stain demonstrating scattered B lymphocytes. (c) CD68 stain demonstrating an abundance of macrophages. (d) Trichrome stain highlighting blue-staining dense fibrosis. Stains for organisms were negative, and IgG4 highlighted rare cells.
DISCUSSION
Although rheumatoid meningitis is rare, the number of biopsy-confirmed cases has increased greatly over the past several decades, due in part to improvements in imaging and increased access to MRI (6). The central nervous system manifestations of rheumatoid arthritis include vasculitis, rheumatoid nodules, and aseptic meningitis, most commonly in the form of lepto and pachymeningitis (2). Hypertrophic pachymeningitis results from chronic inflammation of the dura and has been illustrated on brain biopsy and MRI in patients with confirmed rheumatoid meningitis (3). Elevated CSF rheumatoid factor has been proven to be a highly specific marker of rheumatologic central nervous system disease (1). Our patient's negative infectious workup, elevated CSF rheumatoid factor, and brain biopsy illustrating hypertrophic pachymeningitis are all consistent with a diagnosis of rheumatoid meningitis. Although previous studies reported rheumatoid meningitis mortality rates as high as 70% (1), more recent case reports illustrate significant neurologic recovery following initiation of high-dose steroids, as seen in our patient (3–7).
Multiple studies illustrate a correlation between TNF-α inhibitors and both central and peripheral neuropathies. A double-blind clinical trial using lenercept, a soluble dimeric p55 TNF-IgG fusion protein, illustrated a statistically significant increase in episodes of multiple sclerosis compared with placebo (8). Another prospective study illustrated decreased conduction velocity on electromyography after 12 months of infliximab therapy (9). Several case reports illustrate the development of biopsy-confirmed aseptic, autoimmune meningitis soon after the initiation of TNF-α inhibitors (2–4). Of these reports, one case study illustrated the recurrence of neurologic symptoms upon repeated administration of adalimumab and complete resolution of symptoms following its withdrawal (5). A recent retrospective analysis also illustrated an increased incidence of aseptic meningitis in patients on TNF-α inhibitors compared to alternative disease-modifying antirheumatic drugs (7).
With the current trend towards early and long-term treatment with immunomodulating agents, over 2 million patients have been treated with TNF-α inhibitors worldwide. A recent pharmacologic review found 772 reports of neurologic side effects attributed to TNF-α inhibitors submitted to the US Food and Drug Administration between 2000 and 2009 (10). While the complete neurologic effects of TNF-α inhibitors are still unknown, our case report highlights a unique clinical presentation and encourages physicians to carefully consider autoimmune etiologies for neurologic symptoms in patients on TNF-α inhibitor therapy and promptly discontinue treatment when needed.
References
- 1.Kato T, Hoshi K, Sekijima Y, Matsuda M, Hashimoto T, Otani M, Suzuki A, Ikeda S. Rheumatoid meningitis: an autopsy report and review of the literature. Clin Rheumatol. 2003;22(6):475–480. doi: 10.1007/s10067-003-0788-0. [DOI] [PubMed] [Google Scholar]
- 2.Huys AC, Guerne PA, Horvath J. Rheumatoid meningitis occurring during adalimumab and methotrexate treatment. Joint Bone Spine. 2012;79(1):90–92. doi: 10.1016/j.jbspin.2011.07.008. [DOI] [PubMed] [Google Scholar]
- 3.Ahmed M, Luggen M, Herman JH, Weiss KL, Decourten-Myers G, Quinlan JG, Khanna D. Hypertrophic pachymeningitis in rheumatoid arthritis after adalimumab administration. J Rheumatol. 2006;33(11):2344–2346. [PubMed] [Google Scholar]
- 4.Booker MJ, Flint J, Saravana S. Aseptic meningitis in a patient taking etanercept for rheumatoid arthritis: a case report. Cases J. 2008;1(1):364–365. doi: 10.1186/1757-1626-1-364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jazeron A, Lallier JC, Rihn B, Thiercelin MC. Aseptic meningitis possibly induced by adalimumab. Joint Bone Spine. 2010;77(6):618–619. doi: 10.1016/j.jbspin.2010.06.001. [DOI] [PubMed] [Google Scholar]
- 6.Hayashi Y, Namekawa M, Ohtani K, Watanabe E, Nakano I. Parkinsonism as an initial manifestation of rheumatoid meningitis. Neurol Sci. 2014;35(7):1139–1141. doi: 10.1007/s10072-014-1699-3. [DOI] [PubMed] [Google Scholar]
- 7.Cavazzana I, Taraborelli M, Fredi M, Tincani A, Franceschini F. Aseptic meningitis occurring during anti-TNF-alpha therapy in rheumatoid arthritis and ankylosing spondylitis. Clin Exp Rheumatol. 2014;32(5):732–734. [PubMed] [Google Scholar]
- 8.The Lenercept Multiple Sclerosis Study Group and The University of British Columbia MS/MRI Analysis Group. TNF neutralization in MS: results of a randomized, placebo-controlled multicenter study. Neurology. 1999;53(3):457–465. [PubMed] [Google Scholar]
- 9.Kotyla PJ, Sliwinska-Kotyla B, Kucharz EJ. Treatment with infliximab may contribute to the development of peripheral neuropathy among the patients with rheumatoid arthritis. Clin Rheumatol. 2007;26(9):1595–1596. doi: 10.1007/s10067-007-0657-3. [DOI] [PubMed] [Google Scholar]
- 10.Deepak P, Stobaugh DJ, Sherid M, Sifuentes H, Ehrenpreis ED. Neurological events with tumour necrosis factor alpha inhibitors reported to the Food and Drug Administration Adverse Event Reporting System. Aliment Pharmacol Ther. 2013;38(4):388–396. doi: 10.1111/apt.12385. [DOI] [PubMed] [Google Scholar]