Abstract
Background
Hospital Value-Based Purchasing (HVBP) incentivizes quality performance based healthcare by linking payments directly to patient satisfaction scores obtained from Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) surveys. Lower HCAHPS scores appear to cluster in heterogeneous population dense areas and could bias CMS reimbursement.
Objective
Assess nonrandom variation in patient satisfaction as determined by HCAHPS.
Design
Multivariate regression modeling was performed for individual dimensions of HCAHPS and aggregate scores. Standardized partial regression coefficients assessed strengths of predictors. Weighted Individual (hospital) Patient Satisfaction Adjusted Score (WIPSAS) utilized four highly predictive variables and hospitals were re-ranked accordingly.
Setting
3,907 HVBP-participating hospitals.
Patients
934,800 patient surveys, by most conservative estimate.
Measurements
3,144 county demographics (U.S. Census), and HCAHPS.
Results
Hospital size and primary language (‘non-English speaking’) most strongly predicted unfavorable HCAHPS scores while education and white ethnicity most strongly predicted favorable HCAHPS scores. The average adjusted patient satisfaction scores calculated by WIPSAS approximated the national average of HCAHPS scores. However, WIPSAS changed hospital rankings by variable amounts depending on the strength of the predictive variables in the hospitals’ locations. Structural and demographic characteristics that predict lower scores were accounted for by WIPSAS that also improved rankings of many safety-net hospitals and academic medical centers in diverse areas.
Conclusions
Demographic and structural factors (e.g., hospital beds) predict patient satisfaction scores even after CMS adjustments. CMS should consider WIPSAS or a similar adjustment to account for the severity of patient satisfaction inequities that hospitals could strive to correct.
Introduction
The Affordable Care Act of 2010 mandates that government payments to hospitals and physicians must depend, in part, on metrics that assess the quality and efficiency of health care being provided in order to encourage value-based health care1. Value in health care is defined by the delivery of high quality care at low cost2,3. To this end, Hospital Value-Based Purchasing (HVBP) and Physician Value-Based Payment Modifier programs have been developed by the Centers for Medicare & Medicaid Services (CMS). HVBP is currently being phased in and affects CMS payments for FY 2013 for over 3,000 hospitals across the United States (U.S) in order to incentivize healthcare delivery value. The final phase of implementation will be in FY 2017 and will then affect two percent of all CMS hospital reimbursement. HVBP is based on objective measures of hospital performance as well as a subjective measure of performance captured under the “Patient Experience of Care” domain. This subjective measure will remain at 30% of the aggregate score until FY2016 when it will then be 25% the aggregate score moving forward.4 The program rewards hospitals for both overall achievement and improvement in any domain so that hospitals have multiple ways to receive financial incentives for providing quality care.5 Even still, there appears to be a non-random pattern of patient satisfaction scores across the country with less favorable scores clustering in densely populated areas.6
Value-Based Purchasing and other incentive based programs have been criticized for increasing disparities in healthcare by penalizing larger hospitals (including academic medical centers, safety-net hospitals, and others that disproportionately serve lower socioeconomic communities) and favoring physician-based specialty hospitals7–9. Therefore, hospitals that serve indigent and elderly populations may be at a disadvantage9,10. HVBP portends significant economic consequences for the majority of hospitals that rely heavily on Medicare and Medicaid reimbursement as most hospitals have large revenues but low profit margins11. Higher HVBP scores are associated with for profit status, smaller size, and location in certain areas of the U.S.12. Jha et al6 described HCAHPS scores regional geographic variability but concluded that poor satisfaction was due to poor quality.
The ‘Patient Experience of Care’ domain quantifies patient satisfaction using the validated Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey which is provided to a random sample of patients continuously throughout the year at 48 hours to 6 weeks after discharge. It is a publically-available standardized survey instrument used to measure patients’ perspectives on hospital care. It assesses the following eight dimensions: Nurse Communication, Doctor Communication, Hospital Staff Responsiveness, Pain Management, Medicine Communication, Discharge Information, Hospital Cleanliness and Quietness, and Overall Hospital Rating of which the last two dimensions each have two measures (Cleanliness and Quietness) and (Rating 9 or 10 and Definitely Recommend) to give a total of 10 distinct measures.
The United States is a complex network of urban, suburban, and rural demographic areas. Hospitals exist within a unique contextual and compositional meshwork that determines its case load. The top population density ‘decile’ of the USA lives within 37 counties while half of the most populous parts of the USA occupy a total of 250 counties out of a total of 3,143 counties in the USA. If the ten measures of patient satisfaction (HCAHPS) scores were abstracted from hospitals and viewed according to county-level population density (separated into deciles across the USA), a trend is apparent (Fig 1). Greater population density is associated with lower patient satisfaction in nine of ten categories. On the state level, composite scores of overall patient satisfaction (amount of positive scores) of hospitals show a12 percent variability and a significant correlation with population density (r= −0.479, Fig 2). The lowest overall satisfaction scores are obtained from hospitals located in the population dense regions of Washington D.C., New York State, California, Maryland, and New Jersey (i.e., 63–65%), and the best scores are from Louisiana, South Dakota, Iowa, Maine, and Vermont (i.e. 74–75%). The average patient satisfaction score is 71% ± 2.9%. Lower patient satisfaction scores appear to cluster in population dense areas and may be associated with greater heterogeneous patient demographics and economic variability in addition to population density.
Fig 1. Overall Patient Satisfaction by Population Density Decile.
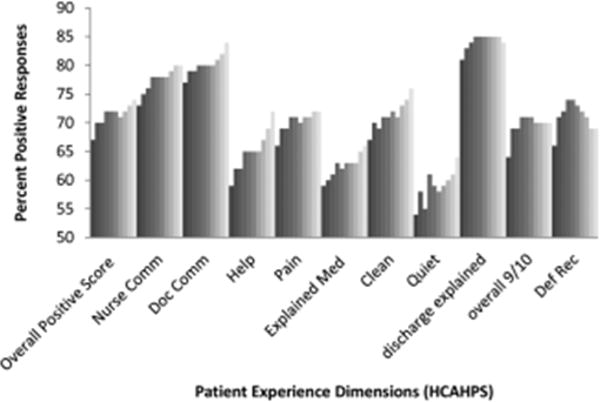
HCAHPS scores are segregated by population density deciles (representing 33 million people each). Population density increases along the grey scale. The composite score and nine out of ten HCAHPS dimensions demonstrate lower patient satisfaction as population density increases (darker shade).
Fig 2. Averaged Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) scores by state correlated with state population density.
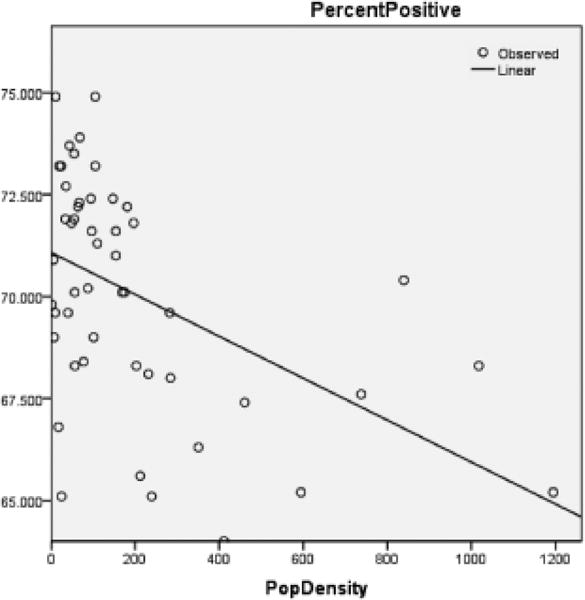
Bivariate correlation of composite HCAHPS scores predicted by state population density without District of Columbia, r = −0.479, p <.001 (2 –tailed). This observed correlation informed the hypothesis that population density could predict for lower patient satisfaction via HCAHPS scores.
These observations are surprising considering that CMS already adjusts HCAHPS scores based on ‘patient-mix’ coefficients and mode of collection13–18. Adjustments are updated multiple times per year and account for survey collection either by telephone, email, or paper survey since the populations that select survey forms will differ. Previous studies have shown that demographic features influence the patient evaluation process. For example, younger and more educated patients were found to provide less positive evaluations of health care19.
This study examined whether patients’ perceptions of healthcare (pattern of patient satisfaction) as quantified under the ‘patient experience domain’ of HVBP were affected and predicted by population density and other demographic factors that are outside the control of individual hospitals. In addition, hospital-level data (e.g., number of hospital beds) and county-level data such as race, age, gender, overall population, data, income, time spent commuting to work, primary language, and place of birth were analyzed for correlation with patient satisfaction scores. Our study demonstrates that demographic and hospital-level data can predict patient satisfaction scores and suggests that CMS may need to modify its adjustment formulas to eliminate bias in HVBP-based reimbursement.
Methods
Data Collection
Publically available data were obtained from Hospital Compare20, American Hospital Directory21, and the United States Census Bureau22 websites. Twenty relevant US census data categories were selected by their relevance for this study out of the 50 publically reported U.S Census categories and included the following: county population, county population density, percent of population change over one year, poverty level (percent), income level per capita, median household income, average household size, travel time to work, percentage of high school or college graduates, non-English primary language spoken at home, percentage of residents born outside of the United States, population percent in same residence for over one year, gender, race (White alone, White alone (not Hispanic or Latino), Black or African American alone), population over 65, and population under 18.
Hospital Consumer Assessment of Healthcare Providers and Systems Survey (HCAHPS) Development
The HCAHPS survey is 32 questions in length, comprised of 10 evaluative dimensions. All short-term, acute care, non-specialty hospitals are invited to participate in the HCAHPS survey.
Data Analysis
Statistical analyses used the Statistical Package for Social Sciences (SPSS; Chicago, IL) version 16.0 for Windows. Data were checked for statistical assumptions, including normality, linearity of relationships, and full range of scores. Categories in both the Hospital Compare (HCAHPS) and US Census data sets were analyzed to assess their distribution curves. The category of population densities (per county) was converted to a logarithmic scale to account for a skewed distribution and long tail in the area of low population density. Data were subsequently merged into one Excel spreadsheet using the VLookup Function such that relevant 2010 census county data were added to each hospital’s Hospital Compare data. Linear regression modeling was performed. Bivariate analysis was conducted (ENTER method) to determine the significant US Census data predictors for each of the 10 Hospital Compare dimensions including the composite overall satisfaction score. Significant predictors were then analyzed in a multivariate model (BACKWORDS method) for each Hospital Compare dimension and the composite average positive score. Models were assessed by determinates of correlation (adjusted R2) to assess for goodness of fit. Statistically significant predictor variables for overall patient satisfaction scores were then ranked according to their partial regression coefficients (standardized Beta).
A patient satisfaction predictive model was sought based upon significant predictors of aggregate percent positive HCAHPS scores. Various predictor combinations were formed based on their partial coefficients (i.e., standardized Beta coefficients); combinations were assessed based on their R2 values and assessed for co-linearity. Combinations of partial coefficients included the two, four, and eight most predictive variables, as well the two and single most positive and negative predictors. They were then incorporated into a multivariate analysis model (FORWARD method) and assessed based on their adjusted R2 values. A four variable combination (the two most predictive positive partial coefficients plus the two most predictive negative partial coefficients) was selected as a predictive model and a formula predictive of the composite overall satisfaction score was generated. This formula “Predicted Patient Satisfaction Formula” (PPSF) predicts hospital patient satisfaction HCAHPS scores based on the four predictive variables for particular county and hospital characteristics.
KMV= coefficient constant (70.9); B=unstandardized Beta coefficient (see Table 2 for values); HB=Number of hospital beds; NE= Proportion of non-English speakers; E=Education (proportion with bachelor’s degree); W= proportion identified as white race only
Table 2. Average Positive Score (i.e. HCAHPS composite score) Multivariate Regression by County & Hospital Demographics.
A multivariate linear regression model of statistically significant dimensions of patient satisfaction as determined by Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) scores is provided below. The dependent variable is the composite of Average Patient Satisfaction scores by hospital (3192 hospitals). Predictors (independent variables) were collected from U.S. census data for counties or county equivalents. All of the listed predictors (1st column) are statistically significant. They are placed in order of partial regression coefficient contribution to the model from most positive to most negative contribution. B = unstandardized beta coefficient, SE = standard error, β = standardized beta (partial coefficient), t = t statistic, p= statistical significance. Adjusted R Square (last row) is used to signify the goodness of fit.
| B | SE | β | t | p | |
|---|---|---|---|---|---|
| Educational attainment-Bachelor’s degree | 0.157 | 0.018 | 0.27 | 8.612 | <0.001 |
| White alone percent 2012 | 0.09 | 0.012 | 0.235 | 7.587 | <0.001 |
| resident population percent under 18 | 0.404 | 0.0444 | 0.209 | 9.085 | <0.001 |
| Black or African American alone percent 2012 | 0.083 | 0.014 | 0.191 | 5.936 | <0.001 |
| median household income 2007–2011 | −0.00003 | 0.00 | −0.062 | −2.027 | 0.043 |
| Population Density (Log) 2010 | −0.277 | 0.083 | −0.087 | −3.3333 | 0.001 |
| Average travel time to work | −0.107 | 0.024 | −0.088 | −4.366 | <0.001 |
| Educational attainment-high school | −0.082 | 0.026 | −0.088 | −3.147 | 0.002 |
| Average household size | −2.58 | 0.727 | −0.107 | −3.55 | <0.001 |
| Total Females percent 2012 | −0.423 | 0.067 | −0.107 | −6.296 | <0.001 |
| percent non-English at home 2007–2011 | −0.052 | 0.018 | −0.14 | −2.929 | 0.003 |
| Number of Hospital Beds | −0.006 | 0.00 | −0.213 | −12.901 | <0.001 |
| ADJUSTED R SQUARE | 0.222 |
The PPSF was then modified by weighting with the partial coefficient (β) in order to remove the bias in patient satisfaction generated by demographic and structural factors over which individual hospitals have limited or no control. This formula generated a Weighted Individual (hospital) Predicted Patient Satisfaction Score (WIPPSS). Application of this formula narrowed the predicted distribution of patient satisfaction for all hospitals across the country.
β=standardized Beta coefficient (see Table 2 for values)
To create an adjusted score with direct relevance to the reported patient satisfaction scores, the reported scores were multiplied by an adjustment factor that defines the difference between individual hospital weighted scores and the national mean HCAHPS score across the United States. This formula, the Weighted Individual (hospital) Patient Satisfaction Adjustment Score (WIPSAS), represents a patient satisfaction score adjusted for demographic and structural factors that can be utilized for inter-hospital comparisons across all areas of the country.
PSrep=Patient satisfaction reported score; PSUSA=Mean reported score for USA (71.84); WIPPSSX=WIPPSS for individual hospital
Application of Data Analysis
PPSF, WIPPSS and WIPSAS were calculated for all HCAHPS-participating hospitals and compared with averaged raw HCAHPS scores across the United States. WIPSAS and raw scores were specifically analyzed for New York State to demonstrate exactly how adjustments would change state level rankings.
Results
Complete HCAHPS scores were obtained from 3907 hospitals out of a total 4621 hospitals listed by the Hospital Compare website (85%). The majority of hospitals (2,884) collected over 300 surveys, fewer hospitals (696) collected 100–299 surveys and fewer still (333) collected less than 100 surveys. In total, results were available from at least 934,800 individual surveys, by the most conservative estimate. Missing HCAHPS hospital data averaged 13.4 (SD 12.2) hospitals per state. County level data were obtained from all 3,144 county or county equivalents across the USA (100%). Multivariate regression modeling across all HCAHPS dimensions found that between 10 and 16 of the 20 predictors (U.S. Census categories) were statistically significant and predictive of individual HCAHPS dimension scores and the aggregate percent positive score as demonstrated in Table 1. For example, county percentage of ‘bachelors’ degrees’ positively predicts for ‘positive MD communication’ scores and ‘hospital beds’ negatively predicts for ‘Quiet’ dimension. The strongest positive and negative predictive variables by model regression coefficients for each HCAHPS dimension are also listed in Table 1.
Table 1. Multivariate Regression of Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) by County & Hospital Demographics.
Linear regression modeling results of 10 dimensions of patient satisfaction (i.e., HCAHPS) and Average Positive Scores (top row) by county demographics and hospital size (left column) are shown. Adjusted R Square (last row) is used to signify the goodness of fit. All models are statistically significant with p=<0.001. Partial regression coefficients (Beta) are used to positively or negatively assess contribution to the individual models (i.e., each column). The dash (−) indicates non-significance and the asterisk (*) indicates a value that was statistically significant in univariate analysis but not in multivariate analysis. Independent variables (first column) are ordered top to bottom by the number of HCAHPS dimensions that each contributes to HCAHPS predictive scoring.
| Avg Positive Scores | RN Comm | MD Comm | Help | Pain | Explain Meds | Clean | Quiet | D/c explain | Rec 9/10 | Def Rec | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Educational-Bachelor’s | 0.27 | 0.19 | 0.45 | 0.10 | 0.10 | 0.05 | 0.08 | 0.33 | 0.15 | 0.27 | .416 |
| Hospital Beds | −0.21 | −0.16 | −0.19 | −0.26 | −0.16 | −0.17 | −0.27 | −0.26 | −0.06 | −0.11 | – |
| Pop. density 2010 | −0.09 | −0.07 | −0.28 | −0.20 | −0.08 | −0.23 | −0.14 | −0.19 | 0.22 | 0.07 | * |
| White alone percent | 0.24 | 0.25 | 0.09 | 0.16 | 0.23 | 0.07 | 0.16 | – | 0.17 | 0.31 | .317 |
| Total Females percent | −0.11 | −0.05 | −0.06 | −0.07 | −0.06 | −0.03 | −0.05 | −0.09 | −0.12 | −0.09 | – |
| African American alone | 0.19 | 0.19 | – | 0.09 | 0.23 | 0.09 | 0.07 | 0.34 | * | 0.09 | .084 |
| Avg travel time to work | −0.09 | −0.10 | * | −0.09 | −0.06 | −0.04 | −0.08 | * | −0.12 | −0.17 | −0.16 |
| Foreign-borne percent | * | −0.16 | 0.14 | −0.06 | −0.12 | −0.08 | 0.06 | −0.13 | −0.18 | * | * |
| Avg. household size | −0.11 | −0.05 | −0.15 | −0.07 | * | −0.07 | * | −0.01 | * | −0.07 | .076 |
| Non-English speaking | −0.14 | −0.12 | −0.50 | −0.07 | * | * | * | * | * | −0.34 | −0.28 |
| Education-high school | −0.09 | −0.09 | −0.40 | * | – | – | – | −0.27 | 0.06 | −0.08 | * |
| Household income | −0.06 | * | −0.35 | −0.08 | * | * | −0.16 | −0.41 | – | – | −.265 |
| Population 65 and over | * | −0.14 | −0.14 | −0.12 | * | −0.11 | −0.15 | – | – | * | −0.10 |
| White, not hisp/Latino | * | * | −0.20 | * | * | * | 0.09 | 0.13 | 0.09 | −0.22 | −0.25 |
| Population under 18 | 0.21 | – | 0.15 | – | 0.08 | – | – | – | 0.11 | 0.20 | – |
| Population (county) | * | −0.06 | −0.08 | * | −0.03 | −0.05 | * | * | −0.06 | * | * |
| All ages in poverty | – | – | −0.24 | – | – | – | −0.10 | −0.22 | −0.08 | * | −.281 |
| 1 year same residence | * | 0.13 | 0.12 | 0.11 | – | – | 0.10 | * | −0.04 | * | * |
| Per capita income | * | −0.07 | * | * | * | * | * | 0.09 | – | – | * |
| Population % change | * | * | * | * | * | * | −0.05 | – | – | * | * |
| ADJUSTED R SQUARE | 0.22 | 0.25 | 0.30 | 0.30 | 0.12 | 0.17 | 0.23 | 0.30 | 0.19 | 0.14 | 0.15 |
Table 2 highlights multivariate regression modeling of the composite ‘average positive score’ which produced an adjusted R square of .222, p=<0.001. All variables were significant and predicted change of the composite HCAHPS except for ‘place of birth-foreign born’. Table 2 ranks variables from most positive to most negative predictors.
Other HCAHPS domains demonstrated statistically significant models (p<0.001) and are listed by their coefficients of determination (i.e. adjusted R2); Table 1. The best fit dimensions were Help (adjusted R2=.304), Quiet (adjusted R2=.299), Doctor Communication (adjusted R2=.298), Nurse Communication (adjusted R2=.245), and Clean (adjusted R2=.232). Models that were not as strongly predictive as the composite score included Pain (adjusted R2=.124), Overall 9/10 (adjusted R2=.136), Definitely Recommend (adjusted R2=.150), and Explained Meds (adjusted R2=.169).
A predictive formula for average positive scores was created by determination of the most predictive partial coefficients and the best fit model. ‘Bachelor’s degree’ and ‘white only’ were the two greatest positive predictors and ‘number of hospital beds’ and ‘non-English speaking’ were the two greatest negative predictors. The PPSF’s (predictive formula) was chosen out of various combinations of predictors (see Table 2) because its coefficient of determination (adjusted R2=.155) was closest to the overall model’s coefficient of determination (adjusted R2=.222) without demonstrating co-linearity. Possible predictive formulas were based on the predictors’ standardized beta (β) and included the following combinations: the two greatest overall predictors (adjusted R2=0.051), the two greatest negative and positive predictors (adjusted R2=0.098), the four greatest overall predictors (adjusted R2=0.117), and the eight greatest overall predictors (adjusted R2=0.201), which suffered from co-linearity (‘household size’ plus ‘non-English speaking’ (Pearson=.624) and ‘under 18’ (Pearson=.708)). None of the correlated independent variables (e.g., ‘poverty’ and ‘median income’) were placed in the final model.
The mean WIPSAS scores closely corresponded with the national average of HCAHPS scores (71.6 versus 71.84) but compressed scores into a narrower distribution (SD 5.52 versus 5.92). The greatest positive and negative changes were by 8.51% and 2.25%, respectively. Essentially, a smaller number of hospitals in demographically challenged areas were more significantly impacted by the WIPSAS adjustment than the larger number of hospitals in demographically favorable areas. Large hospitals in demographically diverse counties saw the greatest positive change (e.g., Texas, California, and New York) while smaller hospitals in demographically non-diverse areas saw comparatively smaller decrements in the overall WIPSAS scores. The WIPSAS had the most beneficial effect on urban and rural safety net hospitals that serve diverse populations including many academic medical centers. This is illustrated by the re-ranking of the top 10 and bottom 10 hospitals in New York State by the WIPSAS (Table 3). For example, three academic medical centers in New York state, Montefiore Medical Center, New York Presbyterian Hospital, and Mount Sinai Hospital, were moved from the 46th, 43rd and 42nd (out of 167 hospitals) respectively into the top ten in patient satisfaction utilizing the WIPSAS methodology. Reported patient satisfaction scores, PPSF, WIPPSS and WIPSAS scores for each hospital in the United States is available online (supplemental Table S1).
Table 3. Top Ten Highest Ranked Hospitals in New York State by Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) Scores Compared to the Weighted Individual (hospital) Patient Satisfaction Adjustment Score (WIPSAS).
Top ten highest ranked hospitals in New York State by overall patient satisfaction out of 167 evaluable hospitals are shown. The left column represents the current top ten hospitals in 2013 by HCAHPS overall patient satisfaction scores and the right column represents the top ten hospitals after the WIPSAS adjustment. The four factors used to create the WIPSAS adjustment were the two most positive partial regression coefficients (Education-Bachelor’s degree, White alone percent 2012) and the two most negative partial regression coefficients (Number of Hospital Beds, non-English at Home). Three urban academic medical centers, Montefiore Medical Center, New York Presbyterian Hospital and Mount Sinai Hospital, were re-ranked from the 46th, 43rd and 42nd respectively into the top ten.
| Ten Highest Ranked Hospitals NYS by HCAHPS (#1–10) | Ten Highest Ranked NYS Hospitals After WIPSAS (#1–10) |
|---|---|
| 1) RIVER HOSPITAL, INC | 1) RIVER HOSPITAL, INC |
| 2) WESTFIELD MEMORIAL HOSPITAL, INC | 2) WESTFIELD MEMORIAL HOSPITAL, INC |
| 3) CLIFTON FINE HOSPITAL | 3) CLIFTON FINE HOSPITAL |
| 4) HOSPITAL FOR SPECIAL SURGERY | 4) HOSPITAL FOR SPECIAL SURGERY |
| 5) DELAWARE VALLEY HOSPITAL, INC | 5) NEW YORK-PRESBYTERIAN HOSPITAL |
| 6) PUTNAM HOSPITAL CENTER | 6) DELAWARE VALLEY HOSPITAL, INC |
| 7) MARGARETVILLE MEMORIAL HOSPITAL | 7) MONTEFIORE MEDICAL CENTER |
| 8) COMMUNITY MEMORIAL HOSPITAL, INC | 8) ST FRANCIS HOSPITAL, ROSLYN |
| 9) LEWIS COUNTY GENERAL HOSPITAL | 9) PUTNAM HOSPITAL CENTER |
| 10) ST FRANCIS HOSPITAL, ROSLYN | 10) MOUNT SINAI HOSPITAL |
Discussion
The HVBP program is an incentive program that is meant to enhance the quality of care. This study illustrates health care inequalities in patient satisfaction that are not accounted for by the current CMS adjustments and shows that education, ethnicity, primary language, and number of hospital beds are predictive of how patients evaluate their care via patient satisfaction scores. Hospitals that treat a disproportionate percentage of non-English speaking, non-White, non-educated patients in large facilities are not meeting patient satisfaction standards. This inequity is not ameliorated by the adjustments currently performed by CMS and has financial consequences for those hospitals that are not meeting national standards in patient satisfaction. These hospitals, which often include academic medical centers in urban areas, may therefore be penalized under the existing HVBP reimbursement models.
Using only four demographic and hospital-specific predictors (i.e. hospital beds, %non-English, %bachelors’ degrees, %white), it is possible to utilize a simple formula to predict patient satisfaction with a significant degree of correlation to the reported scores available through Hospital Compare.
Our initial hypothesis that population density predicted lower patient satisfaction scores was confirmed but these aforementioned demographic and hospital-based factors were stronger independent predictors of HCAHPS scores. The WIPSAS is a representation of patient satisfaction and quality of care delivery across the country that accounts for non-random variation in patient satisfaction scores.
For hospitals in New York State, WIPSAS resulted in the placement of three urban-based academic medical centers in the top-ten in patient satisfaction, when previously, based on the raw scores, their rankings were between 42nd and 46th, statewide. Prior studies have suggested that large, urban, teaching, and not-for-profit hospitals were disadvantaged based on their hospital characteristics and patient features10–12. Under the current CMS reimbursement methodologies, these institutions are more likely to receive financial penalties8. The WIPSAS is a simple method to assess hospitals’ performance in the area of patient satisfaction that accounts for the demographic and hospital-based factors (e.g., number of beds) of the hospital. Its incorporation into CMS reimbursement calculations, or incorporation of a similar adjustment formula, should be strongly considered in order to account for predictive factors in patient satisfaction that could be addressed to enhance their scores.
Limitations for this study are the approximation of county-level data for actual individual hospital demographic information and the exclusion of specialty hospitals, such as cancer centers and children’s hospitals, in HCAHPS surveys. Repeated multivariate analyses at different time points would also serve to identify how CMS –specific adjustments are recalibrated over time. While we have primarily reported on the composite percent positive score as a surrogate for all HCAHPS dimensions, an individual adjustment formula could be generated for each dimension of the ‘patient experience of care’ domain.
Although patient satisfaction is a component of how quality should be measured, further emphasis needs to be placed on non-random patient satisfaction variance so that HVBP can serve as an incentivizing program for at-risk hospitals. Regional variation in scoring is not altogether accounted for by the current CMS adjustment system. Since patient satisfaction scores are now directly linked to reimbursement, further evaluation is needed to enhance patient satisfaction scoring paradigms to account for demographic and hospital-specific factors.
Supplementary Material
Acknowledgments
All authors had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
Conflict of Interest: No conflict of interest reported by authors.
References
- 1.Florence CS, Atherly A, Thorpe KE. Will choice-based reform work for Medicare? Evidence from the Federal Employees Health Benefits Program. Health services research. 2006 Oct;41(5):1741–1761. doi: 10.1111/j.1475-6773.2006.00580.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.H.R. 3590 tC. Patient Protection and Affordable Care Act 2010. 2010 [Google Scholar]
- 3.Donabedian A. The quality of care. How can it be assessed? Jama. 1988 Sep 23–30;260(12):1743–1748. doi: 10.1001/jama.260.12.1743. [DOI] [PubMed] [Google Scholar]
- 4.Lake Superior Quality Innovation Network u, contract with the Centers for Medicare & Medicaid Services (CMS) aaot, Services USDoHaH. 2015 http://www.stratishealth.org/documents/VBP-FY2017.pdf. Accessed March 13th, 2015, 2015.
- 5.Hospital VBP Program. http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Hospital-Value-Based-Purchasing/
- 6.Jha AK, Orav EJ, Zheng J, Epstein AM. Patients’ perception of hospital care in the United States. The New England journal of medicine. 2008 Oct 30;359(18):1921–1931. doi: 10.1056/NEJMsa0804116. [DOI] [PubMed] [Google Scholar]
- 7.Porter ME, L T. Providers must lead the way in making value the overarching goal. Harvard Business Review. 2013 Oct;2013:3–19. [Google Scholar]
- 8.Jha AK, Orav EJ, Epstein AM. The effect of financial incentives on hospitals that serve poor patients. Annals of internal medicine. 2010 Sep 7;153(5):299–306. doi: 10.7326/0003-4819-153-5-201009070-00004. [DOI] [PubMed] [Google Scholar]
- 9.Joynt KE, Jha AK. Characteristics of hospitals receiving penalties under the Hospital Readmissions Reduction Program. Jama. 2013 Jan 23;309(4):342–343. doi: 10.1001/jama.2012.94856. [DOI] [PubMed] [Google Scholar]
- 10.Ryan AM. Will value-based purchasing increase disparities in care? The New England journal of medicine. 2013 Dec 26;369(26):2472–2474. doi: 10.1056/NEJMp1312654. [DOI] [PubMed] [Google Scholar]
- 11.Thorpe KE, Florence CS, Seiber EE. Hospital conversions, margins, and the provision of uncompensated care. Health affairs. 2000 Nov-Dec;19(6):187–194. doi: 10.1377/hlthaff.19.6.187. [DOI] [PubMed] [Google Scholar]
- 12.Borah BJ, Rock MG, Wood DL, Roellinger DL, Johnson MG, Naessens JM. Association between value-based purchasing score and hospital characteristics. BMC health services research. 2012;12:464. doi: 10.1186/1472-6963-12-464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Elliott MN, Zaslavsky AM, Goldstein E, et al. Effects of survey mode, patient mix, and nonresponse on CAHPS hospital survey scores. Health services research. 2009 Apr;44(2 Pt 1):501–518. doi: 10.1111/j.1475-6773.2008.00914.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Burroughs TE, Waterman BM, Cira JC, Desikan R, Claiborne Dunagan W. Patient satisfaction measurement strategies: a comparison of phone and mail methods. The Joint Commission journal on quality improvement. 2001 Jul;27(7):349–361. doi: 10.1016/s1070-3241(01)27030-8. [DOI] [PubMed] [Google Scholar]
- 15.Fowler FJ, Jr, Gallagher PM, Nederend S. Comparing telephone and mail responses to the CAHPS survey instrument. Consumer Assessment of Health Plans Study. Medical care. 1999 Mar;37(3 Suppl):MS41–49. doi: 10.1097/00005650-199903001-00005. [DOI] [PubMed] [Google Scholar]
- 16.Rodriguez HP, von Glahn T, Rogers WH, Chang H, Fanjiang G, Safran DG. Evaluating patients’ experiences with individual physicians: a randomized trial of mail, internet, and interactive voice response telephone administration of surveys. Medical care. 2006 Feb;44(2):167–174. doi: 10.1097/01.mlr.0000196961.00933.8e. [DOI] [PubMed] [Google Scholar]
- 17.O’Malley AJ, Zaslavsky AM, Elliott MN, Zaborski L, Cleary PD. Case-mix adjustment of the CAHPS Hospital Survey. Health services research. 2005 Dec;40(6 Pt 2):2162–2181. doi: 10.1111/j.1475-6773.2005.00470.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mode and Patient-Mix Adjustments of CAHPS Hospital Survey (HCAHPS) 2013 http://www.hcahpsonline.org/modeadjustment.aspx. Accessed December 1st, 2013.
- 19.Zaslavsky AM, Zaborski LB, Ding L, Shaul JA, Cioffi MJ, Clear PD. Adjusting Performance Measures to Ensure Equitable Plan Comparisons. Health Care Financing Review. 2001;22(3):109–126. [PMC free article] [PubMed] [Google Scholar]
- 20.Download, Explore, and Visualize Medicare.gov Data 2013. 2013 https://data.medicare.gov/data/hospital-compare/Patient%20Survey%20Results. Accessed December 1st 2013.
- 21.Directory AH. American Hospital Directory Hospital Statistics by State 2013. 2013 http://www.ahd.com/state_statistics.html. Accessed December 1st 2013.
- 22.US Census Download Center 2013. 2013 http://factfinder2.census.gov/help/en/download_options/downloading_overview.htm. Accessed December 1st, 2013.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


