Abstract
Background
Despite the effects of food insecurity on health are well documented, clear governmental policies to face food insecurity do not exist in western countries. In Canada, interventions to face food insecurity are developed at the community level and can be categorized into two basic strategies: those providing an immediate response to the need for food, defined “traditional” and those targeting the improvement of participants’ social cohesion, capabilities and management of their own nutrition, defined “alternative”.
Objective
The objective of this study was to evaluate the effects of food insecurity interventions on food security status and perceived health of participants.
Design
This was a longitudinal multilevel study implemented in Montreal, Quebec, Canada. Participants were recruited in a two-stage cluster sampling frame. Clustering units were community organizations working on food insecurity; units of analysis were participants in community food security interventions. A total of 450 participants were interviewed at the beginning and after 9 months of participation in traditional or alternative food security interventions. Food security and perceived health were investigated as dependent variables. Differences overtime were assessed through multilevel regression models.
Results
Participants in traditional interventions lowered their food insecurity at follow-up. Decreases among participants in alternative interventions were not statistically significant. Participants in traditional interventions also improved physical (B coefficient 3.00, CI 95% 0.42–5.59) and mental health (B coefficient 6.25, CI 95% 4.15–8.35).
Conclusions
Our results challenge the widely held view suggesting the ineffectiveness of traditional interventions in the short term. Although effects may be intervention-dependent, food banks decreased food insecurity and, in so doing, positively affected perceived health. Although study findings demonstrate that food banks offer short term reprise from the effects of food insecurity, the question as to whether food banks are the most appropriate solution to food insecurity still needs to be addressed.
Introduction
Food insecurity, defined as the “limited, inadequate, or insecure access of individuals and households to sufficient, safe, nutritious and personally acceptable food to meet their dietary requirements for a productive and healthy life” [1], represents a major public health concern [2]. The effects of food insecurity on type II diabetes [3, 4] hypertension [4, 5], cardiovascular diseases [4], mental distress [4, 6–9], depression [10] and poor health in general [6, 7, 11] are well documented.
Despite the well-known association between food insecurity and health, food insecurity is steadily increasing in developed countries such as Canada. In 2011–2012, 8.3% of households experienced food insecurity [12] and efforts to stop its growth are thus far unsuccessful [12, 13]. To date, interventions to tackle food insecurity have been developed at the community level and are sometimes institutionalized, but a clear governmental policy to address food insecurity does not exist in Canada nor in the majority of developed countries [14]. This is due to a profound shift in federal and provincial social policy from a welfare state with modest social rights established in the period 1966–73 to market-driven, neo-liberal approaches[15]. This shift first began in Canada and in many western countries in 1981 and intensified during the following two decades. Indeed, the influence of neoliberalism has marked a return to privatization and charitable or faith-based responses to basic human needs such as food and shelter [15]. Notwithstanding these efforts from community-based organizations they are described as insufficient and inadequate [16], although scientific evaluation of the effectiveness of such interventions has never been published. This research aimed to provide knowledge concerning the effectiveness of community-based food insecurity interventions.
Interventions in food insecurity implemented by community organizations can be categorized into two basic strategies: those facilitating access to food by providing an immediate response to the need for food and those targeting the improvement of participants’ social cohesion, capabilities and management of their own nutrition. The traditional type of intervention, represented by food banks, is oriented toward the satisfaction of immediate needs of people experiencing food insecurity through food supply. Food banks targeting routine food necessities are the most immediate response to food insecurity and are ideally short term solutions [17]. The second intervention strategy, providing an alternative to the traditional, are represented by community kitchens, community gardens and buying groups. These interventions have objectives related to empowerment, supporting the development of skills that allow participants to steadily improve their food insecurity status. The objective of alternative interventions reaches beyond food insecurity problem and involves aspects of social inclusion, social capital and participation in civic activities. Neither traditional nor alternative food security interventions pursue the objective of impacting the economic factors at the root of food insecurity, nor the broader systemic factors that shape food production and distribution. It has therefore been suggested that these interventions have limited potential to impact food insecurity status[18].
The role of community interventions in facing food insecurity is at the core of a long-standing debate. Some researchers argue that food banks exacerbate rather than alleviate food insecurity by masking it, undermining social justice and relieving governments of their duties [16, 19, 20]. In contrast, other researchers underline the importance of food banks, affirming the importance of their role in addressing hunger and health issues[21, 22]. In this respect, it is argued that the strategic position community organizations have in changing food insecurity intervention strategies may be strengthened.
Despite this important debate regarding how public policy and intervention may or may not eradicate food insecurity, there is a lack of empirical evidence about the effectiveness of the different intervention strategies commonly implemented by community organizations to address food insecurity. Indeed, in spite of the multitude of studies correlating food insecurity and health, there is a lack of data on the effectiveness of interventions on households’ food insecurity and their effects on participants’ health [23]. The rare studies analyzing the health of participants in food insecurity interventions were based on interviews during or at the end of the interventions, generally through retrospective accounts often based on a small number of respondents [24, 25]. The relationship between food insecurity and health is complex and recursive: food insecurity can cause ill-health and poor health can worsen food insecurity [26]. In addition, the mediating effect of participation in food insecurity interventions has not been addressed.
To our knowledge, this is the first study that selected and recruited new participants from community-based food insecurity interventions for a prospective effectiveness evaluation. The objective of this study is to evaluate the short-time effects of food insecurity interventions on food security and perceived health of participants. Identifying the effects of interventions on health and food insecurity is essential to advance knowledge regarding the effectiveness of food insecurity intervention overall, as well as with respect to traditional and alternative approaches.
Methods
Sample Selection
This is a longitudinal study of newly recruited participants in traditional and alternative interventions. Participants were recruited in a two-stage cluster sampling frame. Clustering units were community organizations working on food insecurity in the Montreal Metropolitan Region (MMR). The MMR includes 82 municipalities and a population of nearly four millions people [27]. The list of organizations involved in food insecurity interventions was validated through the confirmation of experts with in-depth knowledge of the food insecurity intervention network in the Montreal area. Organizations exclusively targeting children such as school lunch and breakfast programs were excluded. A total of 451 organizations were selected. We administered a phone survey to the directors of 30.1% (136 / 451) of these organizations, randomly selected, to identify the interventions each organization implemented and the number of new and overall participants. Of the 136 surveyed organizations, 61 uniquely offered traditional interventions and 75 offered a form of alternative intervention. Organizations offering both traditional and alternative interventions were classified as alternative. Participants selected from these organizations were uniquely participating in alternative interventions
Organizations were invited to participate in our study based upon their number of new participants each year. A minimum number of 30 and 50 participants having begun a food insecurity intervention in the past 6 months was set respectively for alternative and traditional interventions. This criteria for participation was determined first, by considering what could be expected in terms of participant recruitment and second, what was needed in terms of statistical analysis. Community partners’ expertise first informed our criteria for the minimum number of new participants. Namely, new participants in alternative interventions are less numerous than in traditional interventions whereas participation is stable and constant for longer periods of times. While the number of new participants in traditional interventions is higher, participation is more sporadic and related to temporary situations. Second, power calculations for the minimum number of participants required for statistical analysis, as further explained below, considered the hierarchical nature of the data.
Individuals between 18 and 65 years of age registered for the first time, and for less than 6 months in selected MMR food insecurity community organizations were invited to participate in our study. People older than 65 years of age were excluded from the study because, in Québec, they can benefit from income supplement and have preferential paths to fight food insecurity. Homeless people were also excluded for two reasons. First, homeless people represent a sub-population extremely vulnerable and their strategies to cope with food are different from the rest of the population [28]. Second, their inclusion in the study would have biased results because of the lack of long term strategies for food insecurity directed to this vulnerable population.
Multi-level modeling
Services and resources provided by organizations, although classified in the same category (i.e. food bank) could differ among organizations according to policies, quality of food or frequency of access. Participants in our study were nested within organizations. With nested data observations may not be independent and hierarchical multilevel modeling is recommended [29].
To account for these differences along with the longitudinal nature of the data, analysis accounted for data structured into three levels. The first level was the change overtime in dependent variables, the second level were individuals, the third corresponded to the organization where participants were recruited. With this hierarchical structure of data, and since the intraclass (among individuals) and interclass (among different organizations) coefficients for our outcome variables were unknown, we needed a large number of participants in each organization to detect a 10% difference in the variables measuring food security with an acceptable degree of precision (0.9) and at a statistically significant threshold (0.05). Among the 136 organizations, 16 organizations carrying out traditional interventions and 6 implementing alternative interventions met the criteria for a minimum number of new registered participants.
Measures and Variables
From October 2011 to May 2012 a questionnaire to investigate health, food insecurity and vulnerability was completed by participants with the support of research assistants specifically-trained to accompany participants through the completion of the questionnaire. The questionnaire took approximately 30–45 minutes and was administered face to face in French or in English, according to the preference of participants. Interviews took place in the organizations providing food insecurity interventions or in the nearby area. Participants were informed that they would be called back and invited to participate in the second part of the study and were asked to inform the research team in case of changes of address. Six months after the first interview, a postcard inviting participants to communicate possible changes of address was sent to each participant. Nine months after the first interview, participants were invited by phone to complete the follow up interview. A nine month follow-up was considered adequate to detect intervention effects on the level of food security and health status because according to community partners, sufficient time has passed such that participation in alternative food security interventions has become regular. Non respondents were contacted by mail and invited to contact project managers. The second interview took place in the same location as the first. In case of changes of address or impracticability of the first location, another place was chosen by mutual agreement. The same questionnaire was used for the first and the second survey.
The categorizing variable corresponded to participants’ enrollment in one of the two intervention strategies, traditional or alternative. Dependent variables were food security status and perceived physical and mental health. Control variables considered in the study were gender, age, country of birth, marital status and income.
Food security status
Food security status was measured using the food security module included in the Canadian Community Health Survey(CCHS)[30]. The food security module presents the same questions used in the United States Household Food Security Survey Module (HFSSM). The HFSSM was validated to measure change in food security status overtime [31]. The CCHS calculates three scores of food insecurity for the previous year: for the respondent, for dependent children (when applicable) and for the respondent’s household. The CCHS food security module is composed of 10 adult-related and 8 children-related questions investigating whether the respondent or other household members experienced indicators of food insecurity. Questions query the severity of the experiences associated with food, such as an anxiety that food will run out, a need to modify the amount of food consumed, experiencing hunger, and in the extreme, going a whole day without eating.
Each multiple choice answer is recoded scoring 0 or 1 point, where 0 corresponds to food security and 1 to food insecurity status. For example, if the question “You and other household members worried that food would run out before you got money to buy more. Was that often true, sometimes true, or never true in the past 12 months?” was answered “never true” the question was coded as 0 while responses of “often true” or “sometimes true” were coded 1. The answers “often” and “sometimes” are both considered affirmative responses because they indicate that the condition occurred at some time during the year [31].
The final score ranges between 0 to 10 for adults and 0 to 8 for children. The food security module defines three levels of food security: food security, with scores of 0 or 1, moderate insecurity with a score between 2 and 5 for adults and 2 and 4 for children, and severe insecurity with score respectively above 5 for adults and above 4 for children. Household food security status is dependent on both adult and child scores. In families with children, the household is food secure if both adults and children are food secure; the household is moderately food insecure if either adults or children are moderately food insecure but neither is severely food insecure; the household is severely food insecure if either adults or children are severely food insecure. In childless households, adults’ food security status corresponds to household food security status.
Health related quality of life
Generic health-related quality of life was measured using the SF-12-v2 questionnaire [32]. The SF-12-v2 is a shorter and validated version of SF-36, regularly used to assess perceived health [33]. The questionnaire tests physical and mental health in the last four weeks generating 8 subscales: 1- physical functioning (composed of 2 items: health limitations in accomplishing moderate activities such as moving a table, or pushing a vacuum cleaner; health limitations in climbing several flights of stairs); 2- role limitations due to physical problems (composed of 2 items: limitations accomplishing what one desires to accomplish; limitations in the kind of work or activities); 3- bodily pain (composed of 1 item: pain interference in the accomplishment of normal work); 4- general health perceptions (composed of 1 item: own health perception); 5- vitality (composed of 1 item: perceived energy); 6- social functioning (composed of 1 item: interference of physical health or emotional problems); 7- role limitations due to emotional problems (composed of 2 items: limitations in accomplishing what wanted as a result of feeling depressed or anxious; less attention in doing work or other activities); and 8- mental health (composed of 2 items: perception of calm and peace; perception of downhearted and depression). Based on these subscales, two summary scores were calculated: the physical (PCS) and the mental (MCS) component summary scores. PCS was built with the subscales 1 through 4 and MCS was built with subscales 5 through 8.PCS and MCS scores were transformed in a 0–100 score according to published regression weights and scoring rules (a higher score indicating better health-related quality of life) as suggested in the user manual.[34]
Household income and other control variables
Respondent’s gender, age, country of birth, being part of a visible minority, marital status and household income were self-reported. According to the Employment Equity Act of Canada, we defined visible minorities "persons, other than Aboriginal peoples, who are non-Caucasian in race or non-white in colour". Household income was grouped into 7 categories ranging from “no income” to “income superior to $40000”.
Statistical analysis
In our analysis, missing values were not imputed but excluded pair-wise. Since our data were repeated measures from individuals nested in organizations and categorized in two different interventions, the influence of dependent variables on the outcomes (food insecurity and health) was investigated with multilevel regression analyses.
We used multilevel models to account for the hierarchical structure of data and likewise, to avoid an underestimation of the group effect and incorrectly rejecting the null hypothesis of no difference (i.e. type I error)[29]. The analyses were executed separately for participants in traditional and alternative interventions. Generalized linear latent regression models (GLLAMM) were used. GLLAMM performs maximum likelihood estimation by using adaptive quadrature. Three-level random intercept regression models were constructed for food security for each intervention strategy. A first model was constructed using food insecurity as the dependent variable. Subsequently, a sequence of controlling variables (respondent’s gender, age, country of birth, marital status and income) were entered as covariates at the individual level of the model. No organization level factors were added to the models.
Six linear random intercept regression GLLAMM models were used to assess perceived health (three for physical health and three for mental health) in each intervention group. The first two models considered physical and mental health unadjusted, the following two models were adjusted for respondents’ gender, age, country of birth, marital status and income, while the last two models were also adjusted for adults’ food security status. Differences across time in the two intervention groups were also tested through GLAMM models. The STATA v11.2 software was used to perform statistical analysis.
Ethic statement
This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects/patients were approved by the health research ethics committee (CERES) of the University of Montreal. Written informed consent was obtained from all subjects/patients.
Results
In total, 824 new participants responded to the first questionnaire; 711 were participants in one of the 16 organizations classified as offering uniquely traditional interventions, and 113 were participants in one of the 6 organizations offering alternative interventions.
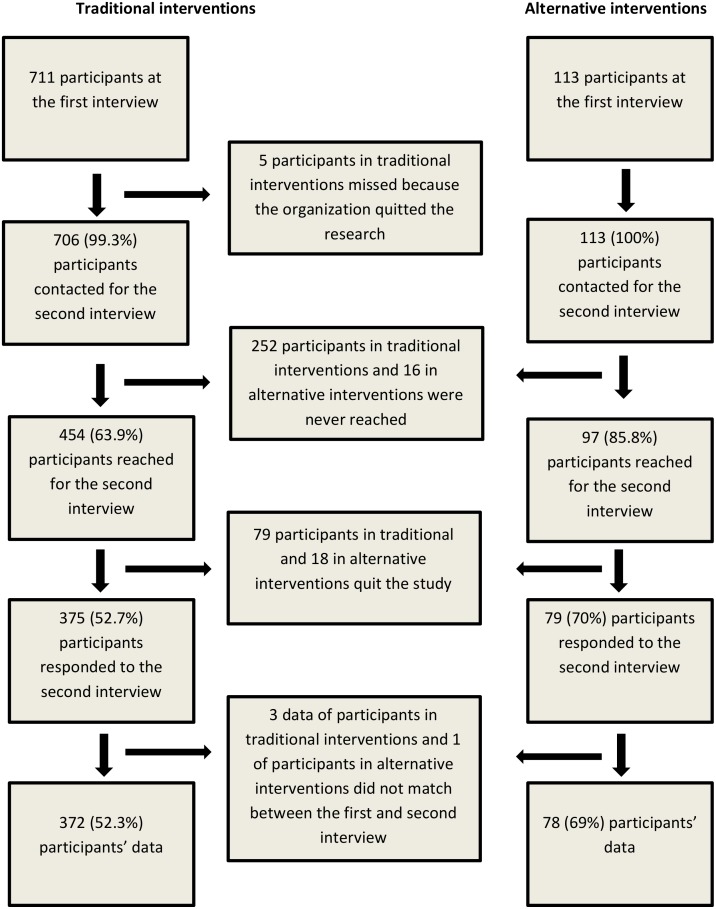
Among the 824 original respondents, 374 (45.4%) participants were missing at follow up (Fig 1).
Fig 1. Data on participation and missing at follow-up for traditional and alternative interventions.
The final sample size was composed of 450 people: 372 participants in traditional interventions (52.3% of initial participants) and 78 participants in alternative interventions (69% of initial participants). No statistical significant differences were found in the descriptive characteristics of participants according to loss to follow up (Table 1; Chi square tests were performed to assess differences). Statistically significant differences between the two intervention groups were found with respect to gender (p = 0.000), country of birth (p = 0.000), belonging to a visible minority (0.014) and marital status(p = 0.001). More in depth analysis of the differences between the two study populations have been described elsewhere. [35, 36]. Intra-group statistically significant differences were found in employment status and income when we compared the first and the second interview data: participants were more likely to be employed and to have a higher income at follow-up. These differences in employment status were evident in both groups (traditional interventions, p = 0.000; alternative interventions p = 0.010), while differences in income were evident only within traditional intervention participants (p = 0.001) (Table 2).
Table 1. Descriptive characteristics of new participants in traditional and alternative interventions.
| Participants in traditional interventions n. 372 (%) | Participants in alternative interventions n. 78 (%) | Total n. 450 (%) | |
|---|---|---|---|
| Gender* | |||
| Male | 171 (46.0) | 19 (24.4) | 190 (42.2) |
| Female | 201 (54.0) | 59 (75.6) | 260 (57.8) |
| Age | |||
| <30 years | 43 (11.6) | 13 (16.9) | 56 (12.5) |
| 30–49 years | 190 (51.2) | 40 (51.9) | 230 (51.3) |
| 50–65 years | 138 (37.2) | 24 (31.2) | 162 (36.2) |
| Country of birth* | |||
| Canada | 252 (67.3) | 36 (46.2) | 288 (64.1) |
| Others | 119 (32.1) | 42 (53.8) | 161 (35.9) |
| Visible minority* | |||
| Yes | 85 (23.7) | 29 (37.2) | 114 (26.1) |
| No | 274 (76.3) | 49 (62.8) | 323 (73.9) |
| Marital status* | |||
| Married/ common law spouse | 118 (32.2) | 30 (39.5) | 148 (33.4) |
| Single | 174 (47.4) | 22 (28.9) | 196 (44.2) |
| Other (separated, divorced, widowed) | 75 (20.4) | 24 (31.6) | 99 (22.3) |
Age and marital status refer to the first interview
* p value <0.05
Table 2. Descriptive characteristics of new participants in traditional and alternative interventions.
| Participants in traditional interventions n. 372 (%) | Participants in alternative interventions n. 78 (%) | |||
|---|---|---|---|---|
| T1 | T2 | T1 | T2 | |
| Employment status | ||||
| Working | 29 (7.8) | 73 (19.6) | 9 (11.5) | 19 (24.4) |
| Studying | 33 (8.9) | 29 (7.8) | 9 (11.5) | 11 (14.1) |
| Working and studying | 11 (3.0) | 16 (4.3) | 3 (3.8) | 3 (3.8) |
| At home | 245 (65.9) | 182 (48.9) | 51 (65.4) | 34 (43.6) |
| Other | 8 (2.2) | 69 (18.5) | 2 (2.6) | 11 (14.1) |
| Not respondent | 46 (12.4) | 3 (0.8) | 4 (5.1) | 0 |
| Education | ||||
| Less than a high school diploma | 98 (26.3) | 102 (27.4) | 19 (24.4) | 12 (15.4) |
| Secondary (high) school diploma or equivalent | 94 (25.3) | 97 (26.1) | 18 (23.1) | 17 (21.8) |
| Less than a bachelor degree | 105 (28.2) | 99 (26.6) | 19 (24.4) | 23 (29.5) |
| Bachelor’s degree or above | 62 (16.7) | 71 (19.1) | 21 (27.0) | 26 (33.3) |
| Not respondent | 13 (3.5) | 3 (0.8) | 1 (1.3) | 0 |
| Income | ||||
| <5000$ | 39 (10.5) | 16 (4.3) | 8 (10.3) | 6 (7.7) |
| 5000–9.999$ | 119 (32.0) | 118 (31.7) | 11 (14.1) | 13 (16.7) |
| 10000–14.999$ | 102 (27.4) | 111 (29.8) | 17 (21.8) | 21 (27.0) |
| 15000–19.999$ | 26 (7.0) | 42 (11.3) | 9 (11.5) | 8 (10.3) |
| 20000–29.999$ | 19 (5.1) | 41 (11.0) | 10 (12.8) | 11 (14.1) |
| 30000–39.999$ | 12 (3.2) | 16 (4.3) | 6 (7.7) | 5 (6.4) |
| ≥40000$ | 14 (10.8) | 10 (2.7) | 7 (9.0) | 6 (7.7) |
| Not respondent | 41 (11.0) | 18 (4.8) | 10 (12.8) | 8 (10.3) |
Participants in traditional interventions had lowered their food insecurity at follow-up. This was true for households with our without children. Decreases among participants in alternative interventions were not statistically significant (Table 3).
Table 3. Food security status traditional and alternative interventions participants distinguishing among adults, children and household.
| A | ||||
| Participants in traditional interventions n.372 | T1 | T2 | OR (CI) | Adjusted OR (CI) a |
| Adults | ||||
| Food secure | 41 (11.6) | 86 (23.4) | Ref | Ref |
| Moderate insecure | 138 (39.0) | 141 (38.3) | 0.23 (0.12;0.46) | 0.30 (0.14;0.62) |
| Severe insecure | 175 (49.4) | 141 (38.3) | 0.18 (0.09–0.36) | 0.22 (0.10;0.44) |
| Children | ||||
| Food secure | 33 (24.3) | 58 (40.3) | Ref | Ref |
| Moderate insecure | 79 (58.1) | 74 (51.4) | 0.37 (0.18;0.76) | 0.39 (0.17;0.89) |
| Severe insecure | 24 (17.6) | 12 (8.3) | 0.20 (0.08; 0.51) | 0.22 (0.08;0.64) |
| Household | ||||
| Food secure | 37 (10.4) | 77 (20.9) | Ref | Ref |
| Moderate insecure | 141 (39.8) | 148 (40.2) | 0.29 (0.15;0.55) | 0.39 (0.20;0.77) |
| Severe insecure | 176 (49.7) | 143(38.9) | 0.22 (0.12;0.42) | 0.27 (0.14;0.54) |
| B | ||||
| Participants in alternative interventions n.78 | T1 | T2 | OR (CI) | Adjusted OR (CI) a |
| Adults | ||||
| Food secure | 23 (32.4) | 30 (40) | Ref | Ref |
| Moderate insecure | 28 (39.4) | 28 (37.3) | 0.60 (0.23;1.54) | 0.36 (0.10;1.31) |
| Severe insecure | 20 (28.2) | 17 (22.7) | 0.51 (0.18; 1.41) | 0.32 (0.08;1.25) |
| Children | ||||
| Food secure | 16 (45.7) | 21 (60.0) | Ref | Ref |
| Moderate insecure | 15 (42.9) | 12 (34.2) | 0.33 (0.07;1.62) | 0.35 (0.07;1.70) |
| Severe insecure | 4 (11.4) | 2 (5.7) | 0.20 (0.02; 1.85) | 0.21 (0.01; 8.33) |
| Household | ||||
| Food secure | 23 (32.4) | 29 (38.7) | Ref | Ref |
| Moderate insecure | 26 (36.6) | 29 (38.7) | 0.70 (0.26;1.83) | 0.42 (0.11;1.53) |
| Severe insecure | 22 (31.0) | 17 (22.7) | 0.48 (0.17;1.35) | 0.32 (0.08;1.25) |
a OR is adjusted for respondent’s gender, age, country of birth, marital status and income.
Participants in traditional interventions reported improved physical (adjusted B coefficient 3.00, CI 95% 0.42–5.59) and mental health (adjusted B coefficient 6.25, CI 95% 4.15–8.35) at follow-up. However, improvement in physical health disappeared when adjusting for food security. No change in physical health at follow-up was found for participants in alternative interventions. Mental health improvement was found among participants in alternative interventions, however this effect disappeared in the adjusted model, which is likely due to the study’s lack of power (Table 4). No statistical significant differences were found between participants in traditional and in alternative interventions across time.
Table 4. Perception of physical and mental health traditional and alternative interventions participants.
Scores are in percentage scale.
| A | |||||
| Participants in traditional interventions n. 372 | T1 | T2 | β coefficient (CI) | Partially adjusted β coefficient (CI) a | Adjusted β coefficient (CI) b |
| Physical Components Score | 63.97 | 66.91 | 3.02 (0.63;5.40) | 3.00 (0.42;5.59) | 1.51 (-1.11;4.12) |
| Mental Components Score | 58.13 | 63.86 | 5.85 (3.92; 7.78) | 6.25 (4.15; 8.35) | 5.28 (3.13; 7.42) |
| B | |||||
| Participants in alternative interventions n. 78 | T1 | T2 | β coefficient (CI) | Partially adjusted β coefficient (CI) a | Adjusted β coefficient (CI) b |
| Physical Components Score | 70.62 | 70.59 | 0.11 (-4.93; 5.15) | -1.10 (-6.57; 4.36) | -0.89 (-6.66;4.89) |
| Mental Components Score | 66.06 | 71.1 | 4.66 (0.10; 9.23) | 4.51 (-0.39; 9.41) | 4.21 (-1.28;9.69) |
a β coefficient is adjusted for respondent’s gender, age, country of birth, marital status and income,
b β coefficient is adjusted for respondent’s gender, age, country of birth, marital status, income, and food security status
Discussion
The objective of this study was to evaluate the short term effects of two distinct food insecurity intervention approaches, traditional and alternative, on participants’ food security and perceived health. Study results found traditional, but not alternative food insecurity interventions to have short term effects on participants. Nevertheless, although not statistically significant, participants in alternative interventions also improved their food insecurity. Relative to their baseline measures, participants in traditional interventions reported a decrease in food insecurity and improvement in self-reported mental and physical health at nine-month follow-up. No such improvements were reported for participants in alternative interventions and while not statistically significant, an improvement was reported for mental health.
The absence of statistically significant effects on food insecurity and perceived health among alternative interventions is not surprising for several reasons. First, people who start participating in alternative interventions are generally more food secure and less vulnerable than those who start participating in traditional interventions. [35, 36] Moreover, collective kitchens and community gardens do not have short term objectives with regard to food insecurity and health. Rather, alternative interventions aim to decrease food insecurity through mutual collaboration, empowerment and social inclusion; they implement long term strategies building change over time [18]. Therefore, although they are often identified as food insecurity interventions, their potential effects go beyond food insecurity alone. Moreover, in our study, the sample of participants in alternative interventions may have been too small to allow enough power to detect significant effects. A small number of participants in alternative food insecurity interventions is associated with the hierarchical nature of our data and the need to employ strict inclusion criteria. Receiving 30 new participants in the 6 months that preceded baseline measurements did not occur for most organizations that offered alternative interventions and many could not guarantee the minimum number of participants.
The short-term impact of food banks on perceived health confirmed the already known association between food insecurity and health. [5–9, 11, 37] Nevertheless, this research adds important facets to this association.[35, 36] First, results show that 9 months of intervention are sufficient to show decreases in food insecurity and improvement in perceived mental and physical health. It appears thus, that improvements in food insecurity are concomitant with improvements in health. This finding underlines the importance of acting swiftly in facing food insecurity. Many households do not have access to food banks because of lack of information, perceptions of food aid, or feelings they are not in enough need [16]; a prompt participation in food banks may rapidly improve food insecurity and consequently their health. Secondly, the use of traditional interventions was found to have a positive association with mental health even after adjusting for food insecurity. Over and above any indirect effect from improving food insecurity status, participating in a traditional type of food insecurity intervention appears to have a direct and positive effect on mental health. The use of food banks may guarantee the family’s regular access to food and this may impact feelings of alienation characterizing people in food insecurity [38] and consequently improve mental health. Nevertheless, participants often have to overcome feelings of shame, embarrassment, degradation and humiliation before accessing food banks [39–41]. This finding of a positive association between the use of traditional intervention and mental health improvements provides an additional argument for why food banks need to be made easily accessible to any household in food insecurity and the importance of overcoming the resistance and inability that people in food insecurity have in accessing food banks [40, 41].
Some study limitations should be taken into account in the discussion of this study’s results. At first, we limited our selection criteria to organizations with at least 50 newly registered subjects within 6 months for traditional strategy, 30 for alternative strategy. This criterion excluded the smallest organizations. Participants in small organizations could present different characteristics relative to those participating in bigger organizations. Moreover, this criterion limited the number of organizations implementing alternative interventions that could be enrolled in the study. This limited the statistical power in data analysis, especially concerning alternative interventions. A second limitation is related due to the high rate of loss to follow-up; nevertheless, our retention rates are in line with other studies on vulnerable populations[42, 43].
Our results challenge the widely held view suggesting the ineffectiveness of traditional interventions, at least in the short term. Given the nature of traditional food insecurity interventions, effects are likely to disappear when participants are no longer exposed to the intervention. This is however congruent with the objectives of food banks, which is to provide first aid intervention and decrease participants’ food insecurity over a limited period of time.
Conclusions
Traditional interventions represent an effective food security intervention in short-term, improving both food insecurity status and health of participants. Nevertheless, these positive effects may be time-limited and disappear when access to traditional interventions ends. Although food banks may offer a short term reprise from the effects of food insecurity, the question as to whether food banks are an appropriate solution, socially and politically, to food insecurity should not be overlooked. As clearly stated in recent food banks reports, it is a mistake to think that food banks or other charitable food programs are able to adequately address household food insecurity over the long term [41, 44]. Further research is needed to identify how traditional interventions have an effect upon long term food insecurity and the potential that alternative interventions may offer longer term advantages.
Acknowledgments
The authors would like to acknowledge the members of the steering committee of the research on the “Effects of interventions in food insecurity” for their contribution and support in the research. All authors have read and approved the final manuscript.
Data Availability
Ethical and legal restrictions prevent public sharing of data. Data requests may be sent to Boyer Ginette, Chair on Community Approach and Health Inequality (CACIS) of the University of Montreal coordinator, http://chairecacis.org/nous-joindre.
Funding Statement
The project on food security was founded in 2010 by CIHR, Canadian Institute of Health Research with the grant n. GIR-112691. CIHR had no role in the design, analysis or writing of this article. Louise Potvin holds a Canada Research Chair (CIHR:950-228295) and Federico Roncarolo was funded through PHIRNET postdoctoral award (CIHR: TGF-96112) and FRQ-S postdoctoral research award (28518).
References
- 1.Tarasuk V. Household Food Insecurity in Canada. Topics in Clinical Nutrition. 2005;20(4):299–312. [Google Scholar]
- 2.Nord M. What have we learned from two decades of research on household food security? Public Health Nutr. 2014;17(01):2–4. 10.1017/S1368980013003091 [DOI] [Google Scholar]
- 3.Seligman H, Bindman A, Vittinghoff E, Kanaya A, Kushel M. Food Insecurity is Associated with Diabetes Mellitus: Results from the National Health Examination and Nutrition Examination Survey (NHANES) 1999–2002. J Gen Intern Med. 2007;22(7):1018–23. 10.1007/s11606-007-0192-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vozoris NT, Tarasuk VS. Household Food Insufficiency Is Associated with Poorer Health. J Nutr. 2003;133(1):120–6. [DOI] [PubMed] [Google Scholar]
- 5.Seligman HK, Laraia BA, Kushel MB. Food Insecurity Is Associated with Chronic Disease among Low-Income NHANES Participants. J Nutr. 2010;140(2):304–10. 10.3945/jn.109.112573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sharkey JR, Johnson CM, Dean WR. Relationship of Household Food Insecurity to Health-Related Quality of Life in a Large Sample of Rural and Urban Women. Women & Health. 2011;51(5):442–60. 10.1080/03630242.2011.584367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Che J, Chen J. Food insecurity in Canadian households. Health Rep. 2001;12(4):11–22. [PubMed] [Google Scholar]
- 8.Muldoon KA, Duff P, Fielden S, Anema A. Food insufficiency is associated with psychiatric morbidity in a nationally representative study of mental illness among food insecure Canadians. Soc Psychiatry Psychiatr Epidemiol. 2013;48(5):795–803. 10.1007/s00127-012-0597-3 [DOI] [PubMed] [Google Scholar]
- 9.Carter KN, Kruse K, Blakely T, Collings S. The association of food security with psychological distress in New Zealand and any gender differences. Soc Sci Med. 2011;72(9):1463–71. 10.1016/j.socscimed.2011.03.009 [DOI] [PubMed] [Google Scholar]
- 10.Leung CW, Epel ES, Willett WC, Rimm EB, Laraia BA. Household food insecurity is positively associated with depression among low-income supplemental nutrition assistance program participants and income-eligible nonparticipants. J Nutr. 2015;145(3):622–7. Epub 2015/03/04. 10.3945/jn.114.199414 . [DOI] [PubMed] [Google Scholar]
- 11.McLeod L, Veall M. The dynamics of food insecurity and overall health: evidence from the Canadian National Population Health Survey. Applied Economics. 2006;38(18):2131–46. 10.1080/00036840500427429 [DOI] [Google Scholar]
- 12.Tarasuk V, Mitchell A, Dachner N. Household food insecurity in Canada, 2012. Toronto, ON.: Research to identify policy options to reduce food insecurity (PROOF), 2014. [Google Scholar]
- 13.Food and Agriculture Organization of the United Nations, International Found for Agriculture Development, World Food Program. The State of Food Insecurity in the World 2013. The multiple dimensions of food security. Rome: 2013.
- 14.Tarasuk V, McIntyre L, Power E. Report to Olivier De Schutter, the United Nations Special Rapporteur on the Right to Food Mission to Canada. 2012.
- 15.Riches G. Food Banks and Food Security: Welfare Reform, Human Rights and Social Policy. Lessons from Canada? Social Policy & Administration. 2002;36(6):648–63. [Google Scholar]
- 16.Riches G. Thinking and acting outside the charitable food box: hunger and the right to food in rich societies. Development in Practice. 2011;21(4–5):768–75. 10.1080/09614524.2011.561295 [DOI] [Google Scholar]
- 17.Tarasuk V. A Critical Examination of Community-Based Responses to Household Food Insecurity in Canada. Health Educ Behav. 2001;28(4):487–99. 10.1177/109019810102800408 [DOI] [PubMed] [Google Scholar]
- 18.Tarasuk V, Reynolds R. A Qualitative Study of Community Kitchens as a Response to Income-Related Food Insecurity. Can J Diet Pract Res. 1999;60(1):11–6. Epub 2002/02/15. . [PubMed] [Google Scholar]
- 19.Poppendieck J. Dilemmas of emergency food: A guide for the perplexed. Agric Hum Values. 1994;11(4):69–76. 10.1007/BF01530418 [DOI] [Google Scholar]
- 20.Tarasuk V, Naomi D, Rachel L. Food banks, welfare, and food insecurity in Canada. British Food Journal. 2014;116(9):1405–17. 10.1108/BFJ-02-2014-0077 [DOI] [Google Scholar]
- 21.Wakefield S, Fleming J, Klassen C, Skinner A. Sweet Charity, revisited: Organizational responses to food insecurity in Hamilton and Toronto, Canada. Critical Social Policy. 2013;33(3):427–50. 10.1177/0261018312458487 [DOI] [Google Scholar]
- 22.Webb KL. Introduction–Food Banks of the Future: Organizations Dedicated to Improving Food Security and Protecting the Health of the People They Serve. Journal of Hunger & Environmental Nutrition. 2013;8(3):257–60. 10.1080/19320248.2013.817169 [DOI] [Google Scholar]
- 23.Collins PA, Power EM, Little MH. Municipal-level responses to household food insecurity in Canada: a call for critical, evaluative research. Can J Public Health. 2014;105(2):e138–41. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Engler-Stringer R, Berenbaum S. Exploring food security with collective kitchens participants in three Canadian cities. Qual Health Res. 2007;17(1):75–84. 10.1177/1049732306296451 WOS:000243072000008. [DOI] [PubMed] [Google Scholar]
- 25.Draper C, Freedman D. Review and Analysis of the Benefits, Purposes, and Motivations Associated with Community Gardening in the United States. Journal of Community Practice. 2010;18(4):458–92. 10.1080/10705422.2010.519682 [DOI] [Google Scholar]
- 26.Tarasuk V, Mitchell A, McLaren L, McIntyre L. Chronic physical and mental health conditions among adults may increase vulnerability to household food insecurity. J Nutr. 2013;143(11):1785–93. 10.3945/jn.113.178483 . [DOI] [PubMed] [Google Scholar]
- 27.Ministère des affaires municipales régions et occupation du territoire. Répertoire des municipalités: communauté métropolitaine de Montréal 2012 [updated 2015/march/15; cited 2012 2012/Nov/12]. Available: http://www.mamrot.gouv.qc.ca/repertoire-des-municipalites/fiche/mrc/663/.
- 28.Tarasuk V, Vogt J. Household food insecurity in Ontario. Can J Public Health. 2009;100(3):184(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Goldstein H. Multilevel Statistical Models London1999 [cited 2012 20th Dec]. Available: http://www.ats.ucla.edu/stat/examples/msm_goldstein/.
- 30.Office of Nutrition Policy and Promotion HC. Canadian Community Health Survey, Cycle 2.2, Nutrition (2004)—Income-Related Household Food Security in Canada: Health Canada; 2007 [updated 2008/01/07; cited 2012]. Available: http://www.hc-sc.gc.ca/fn-an/surveill/nutrition/commun/income_food_sec-sec_alim-eng.php.
- 31.Bickel G, Nord M, Price C, Hamilton W, Cook J. Guide to Measuring Household food Security, Revised 2000. In: Food and Nutrition Service USDoA, editor. Alaexandria, VA: 2000. [Google Scholar]
- 32.Ware JE, Kosinski M, Keller SD. How to Score the SF-12 Physical and Mental Health Summary Scale. Boston, MA: The Health Institute, New England Medical Center; 1995. [Google Scholar]
- 33.Ware JE, Kosinski M, Gandek B, Aaronson NK, Apolone G, Bech P, et al. The Factor Structure of the SF-36 Health Survey in 10 Countries: Results from the IQOLA Project. J Clin Epidemiol. 1998;51(11):1159–65. 10.1016/s0895-4356(98)00107-3 [DOI] [PubMed] [Google Scholar]
- 34.Ware J, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–33. Epub 1996/03/01. . [DOI] [PubMed] [Google Scholar]
- 35.Roncarolo F, Adam C, Bisset S, Potvin L. Traditional and alternative community food security interventions in montreal, Quebec: different practices, different people. J Community Health. 2015;40(2):199–207. Epub 2014/07/12. 10.1007/s10900-014-9917-8 . [DOI] [PubMed] [Google Scholar]
- 36.Roncarolo F, Adam C, Bisset S, Potvin L. Food capacities and satisfaction in participants in food security community interventions in Montreal, Canada. Health Promot Int. 2015. Epub 2015/08/15. 10.1093/heapro/dav085 . [DOI] [PubMed] [Google Scholar]
- 37.Stuff JE, Casey PH, Szeto KL, Gossett JM, Robbins JM, Simpson PM, et al. Household Food Insecurity Is Associated with Adult Health Status. J Nutr. 2004;134(9):2330–5. [DOI] [PubMed] [Google Scholar]
- 38.Hamelin A-M, Beaudry M, Habicht J-P. Characterization of household food insecurity in Québec: food and feelings. Soc Sci Med. 2002;54(1):119–32. 10.1016/s0277-9536(01)00013-2 [DOI] [PubMed] [Google Scholar]
- 39.Tarasuk V, Beaton GH. Household Food Insecurity and Hunger Among Families Using Food Banks. Can J Public Health. 1999;90(2):109–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Loopstra R, Tarasuk V. The Relationship between Food Banks and Household Food Insecurity among Low-Income Toronto Families. Canadian Public Policy. 2012;38(4):497–514. [Google Scholar]
- 41.Perry J, Williams M, Sefton T, Haddad M. Emergency Use Only Understanding and reducing the use of food banks in the UK. The Child Poverty Action Group, Church of England, Oxfam GB and The Trussell Trust, 2014. [Google Scholar]
- 42.Brannon EE, Kuhl ES, Boles RE, Aylward BS, Ratcliff MB, Valenzuela JM, et al. Strategies for Recruitment and Retention of Families from Low-Income, Ethnic Minority Backgrounds in a Longitudinal Study of Caregiver Feeding and Child Weight. Child Health Care. 2013;42(3):198–213. 10.1080/02739615.2013.816590 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nicholson LM, Schwirian PM, Klein EG, Skybo T, Murray-Johnson L, Eneli I, et al. Recruitment and retention strategies in longitudinal clinical studies with low-income populations. Contemp Clin Trials. 2011;32(3):353–62. 10.1016/j.cct.2011.01.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Food Banks Canada. Hunger Counts 2014. Mississauga, ON 2014.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Ethical and legal restrictions prevent public sharing of data. Data requests may be sent to Boyer Ginette, Chair on Community Approach and Health Inequality (CACIS) of the University of Montreal coordinator, http://chairecacis.org/nous-joindre.